User login
SNOWMASS, COLO. – Patients with lumbar spinal stenosis display a distinctive gait and posture that are of great assistance in diagnosing this common low back/leg pain syndrome.
"I find that in the supermarket I can identify persons with symptomatic lumbar stenosis because they lean forward on the cart and have a characteristic wide-based gait. The gait reflects poor balance. In essence the feet are not communicating effectively with the brain because of compression of proprioceptive fibers," Dr. Jeffrey N. Katz explained at the meeting.
The clinical syndrome of lumbar spinal stenosis (LSS) requires both the appropriate clinical picture and the radiographic finding of lumbar spinal canal narrowing on cross-sectional imaging. The radiographic narrowing typically is caused by three pathoanatomic abnormalities occurring together: thickening of the normally paper-thin ligamentum flavum, facet joint osteoarthritis, and disc protrusion.
Radiographic evidence of lumbar spinal canal narrowing is necessary but not sufficient to diagnose the clinical syndrome of LSS. That’s because many individuals with anatomic stenosis don’t have the signs and symptoms of LSS, much as MRI studies have shown that a herniated lumbar disc is present in close to one-third of asymptomatic individuals, according to Dr. Katz, professor of medicine, orthopedic surgery, and epidemiology at Harvard Medical School, Boston.
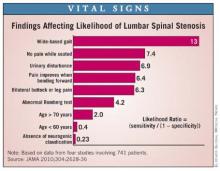
The clinical history and physical examination are invaluable in helping establish the diagnosis of LSS. Dr. Katz and coworkers analyzed data from four published studies involving 741 patients with radiographic evidence of anatomic stenosis to generate a list of predictors of increased likelihood of the syndrome of LSS in an individual patient (JAMA 2010;304:2628-36).
This analysis showed that among the most useful findings for ruling in the diagnosis are a wide-based gait, which confers a likelihood ratio of 13; lack of pain when seated, with an associated likelihood ratio of 7.4; and improvement of symptoms when bending forward, with a likelihood ratio of 6.4.
Patients with LSS typically have pain or discomfort with walking or prolonged standing. The pain radiates into the buttocks, often bilaterally, while extending below the knee far less often. Their polyradiculopathy is often at multiple levels, as distinguished from the monoradicular, well-demarcated pain affecting one of several key dermatomes that’s typical in patients with a herniated disc. Also characteristic of many patients with LSS is a pseudocerebellar syndrome marked by the wide-based gait, unsteadiness, and a positive Romberg test resulting from involvement of the posterior spinal column, he continued.
The differential diagnosis for LSS is lengthy. It includes hip osteoarthritis, trochanteric bursitis, iliopsoas bursitis, stenosis of the cervical spinal canal, pelvic or sacral insufficiency fracture, muscle strain or tears, vascular claudication, myofascial referred pain, and facet arthropathy without stenosis.
"The problem is not that any of the diagnoses on the differential list is particularly difficult to identify, but rather that they can often coexist. In the office, I do a lot of local injections into the trochanteric bursa to try to understand what’s really causing a patient’s symptoms," Dr. Katz said.
Accurate identification of patients who have LSS is paramount because the disorder’s natural history is distinctly different from other common causes of low back pain, including lumbago and a herniated lumbar disc. As a result of these divergent natural history trajectories, the preferred treatment of LSS differs from that for the other conditions. Indeed, LSS is the No.1 indication for spinal surgery beyond age 65 years (JAMA 2010; 303:1259-65).
Dr. Katz reported having no financial conflicts.
SNOWMASS, COLO. – Patients with lumbar spinal stenosis display a distinctive gait and posture that are of great assistance in diagnosing this common low back/leg pain syndrome.
"I find that in the supermarket I can identify persons with symptomatic lumbar stenosis because they lean forward on the cart and have a characteristic wide-based gait. The gait reflects poor balance. In essence the feet are not communicating effectively with the brain because of compression of proprioceptive fibers," Dr. Jeffrey N. Katz explained at the meeting.
The clinical syndrome of lumbar spinal stenosis (LSS) requires both the appropriate clinical picture and the radiographic finding of lumbar spinal canal narrowing on cross-sectional imaging. The radiographic narrowing typically is caused by three pathoanatomic abnormalities occurring together: thickening of the normally paper-thin ligamentum flavum, facet joint osteoarthritis, and disc protrusion.
Radiographic evidence of lumbar spinal canal narrowing is necessary but not sufficient to diagnose the clinical syndrome of LSS. That’s because many individuals with anatomic stenosis don’t have the signs and symptoms of LSS, much as MRI studies have shown that a herniated lumbar disc is present in close to one-third of asymptomatic individuals, according to Dr. Katz, professor of medicine, orthopedic surgery, and epidemiology at Harvard Medical School, Boston.
The clinical history and physical examination are invaluable in helping establish the diagnosis of LSS. Dr. Katz and coworkers analyzed data from four published studies involving 741 patients with radiographic evidence of anatomic stenosis to generate a list of predictors of increased likelihood of the syndrome of LSS in an individual patient (JAMA 2010;304:2628-36).
This analysis showed that among the most useful findings for ruling in the diagnosis are a wide-based gait, which confers a likelihood ratio of 13; lack of pain when seated, with an associated likelihood ratio of 7.4; and improvement of symptoms when bending forward, with a likelihood ratio of 6.4.
Patients with LSS typically have pain or discomfort with walking or prolonged standing. The pain radiates into the buttocks, often bilaterally, while extending below the knee far less often. Their polyradiculopathy is often at multiple levels, as distinguished from the monoradicular, well-demarcated pain affecting one of several key dermatomes that’s typical in patients with a herniated disc. Also characteristic of many patients with LSS is a pseudocerebellar syndrome marked by the wide-based gait, unsteadiness, and a positive Romberg test resulting from involvement of the posterior spinal column, he continued.
The differential diagnosis for LSS is lengthy. It includes hip osteoarthritis, trochanteric bursitis, iliopsoas bursitis, stenosis of the cervical spinal canal, pelvic or sacral insufficiency fracture, muscle strain or tears, vascular claudication, myofascial referred pain, and facet arthropathy without stenosis.
"The problem is not that any of the diagnoses on the differential list is particularly difficult to identify, but rather that they can often coexist. In the office, I do a lot of local injections into the trochanteric bursa to try to understand what’s really causing a patient’s symptoms," Dr. Katz said.
Accurate identification of patients who have LSS is paramount because the disorder’s natural history is distinctly different from other common causes of low back pain, including lumbago and a herniated lumbar disc. As a result of these divergent natural history trajectories, the preferred treatment of LSS differs from that for the other conditions. Indeed, LSS is the No.1 indication for spinal surgery beyond age 65 years (JAMA 2010; 303:1259-65).
Dr. Katz reported having no financial conflicts.
SNOWMASS, COLO. – Patients with lumbar spinal stenosis display a distinctive gait and posture that are of great assistance in diagnosing this common low back/leg pain syndrome.
"I find that in the supermarket I can identify persons with symptomatic lumbar stenosis because they lean forward on the cart and have a characteristic wide-based gait. The gait reflects poor balance. In essence the feet are not communicating effectively with the brain because of compression of proprioceptive fibers," Dr. Jeffrey N. Katz explained at the meeting.
The clinical syndrome of lumbar spinal stenosis (LSS) requires both the appropriate clinical picture and the radiographic finding of lumbar spinal canal narrowing on cross-sectional imaging. The radiographic narrowing typically is caused by three pathoanatomic abnormalities occurring together: thickening of the normally paper-thin ligamentum flavum, facet joint osteoarthritis, and disc protrusion.
Radiographic evidence of lumbar spinal canal narrowing is necessary but not sufficient to diagnose the clinical syndrome of LSS. That’s because many individuals with anatomic stenosis don’t have the signs and symptoms of LSS, much as MRI studies have shown that a herniated lumbar disc is present in close to one-third of asymptomatic individuals, according to Dr. Katz, professor of medicine, orthopedic surgery, and epidemiology at Harvard Medical School, Boston.
The clinical history and physical examination are invaluable in helping establish the diagnosis of LSS. Dr. Katz and coworkers analyzed data from four published studies involving 741 patients with radiographic evidence of anatomic stenosis to generate a list of predictors of increased likelihood of the syndrome of LSS in an individual patient (JAMA 2010;304:2628-36).
This analysis showed that among the most useful findings for ruling in the diagnosis are a wide-based gait, which confers a likelihood ratio of 13; lack of pain when seated, with an associated likelihood ratio of 7.4; and improvement of symptoms when bending forward, with a likelihood ratio of 6.4.
Patients with LSS typically have pain or discomfort with walking or prolonged standing. The pain radiates into the buttocks, often bilaterally, while extending below the knee far less often. Their polyradiculopathy is often at multiple levels, as distinguished from the monoradicular, well-demarcated pain affecting one of several key dermatomes that’s typical in patients with a herniated disc. Also characteristic of many patients with LSS is a pseudocerebellar syndrome marked by the wide-based gait, unsteadiness, and a positive Romberg test resulting from involvement of the posterior spinal column, he continued.
The differential diagnosis for LSS is lengthy. It includes hip osteoarthritis, trochanteric bursitis, iliopsoas bursitis, stenosis of the cervical spinal canal, pelvic or sacral insufficiency fracture, muscle strain or tears, vascular claudication, myofascial referred pain, and facet arthropathy without stenosis.
"The problem is not that any of the diagnoses on the differential list is particularly difficult to identify, but rather that they can often coexist. In the office, I do a lot of local injections into the trochanteric bursa to try to understand what’s really causing a patient’s symptoms," Dr. Katz said.
Accurate identification of patients who have LSS is paramount because the disorder’s natural history is distinctly different from other common causes of low back pain, including lumbago and a herniated lumbar disc. As a result of these divergent natural history trajectories, the preferred treatment of LSS differs from that for the other conditions. Indeed, LSS is the No.1 indication for spinal surgery beyond age 65 years (JAMA 2010; 303:1259-65).
Dr. Katz reported having no financial conflicts.
EXPERT ANALYSIS FROM A SYMPOSIUM SPONSORED BY THE AMERICAN COLLEGE OF RHEUMATOLOGY