User login
Moreover, fracture risk appears to be higher among IBD patients using steroids, according to a report published in the Journal of Clinical Gastroenterology by Yuga Komaki, MD, of the Inflammatory Bowel Disease Center, University of Chicago, and coauthors.
“Further studies addressing the differential risk among Crohn’s disease and ulcerative colitis are needed, but strict surveillance and prevention of spine fractures are indicated in IBD,” wrote Dr. Komaki and associates.
The systematic review and meta-analysis by Dr. Komaki and colleagues was based on 10 studies comprising 470,541 patients with IBD for whom the risk of fracture was reported.
“It is of importance to identify the risk of fractures, as it will increase patient morbidity, disability, and mortality,” the authors wrote. “However, it is often overlooked in the management of IBD.”
Results of the analysis by this group of researchers showed that there was no significant difference in fracture risk overall between IBD patients and controls (odds ratio, 1.08; 95% confidence interval, 0.72-1.62; P = .70).
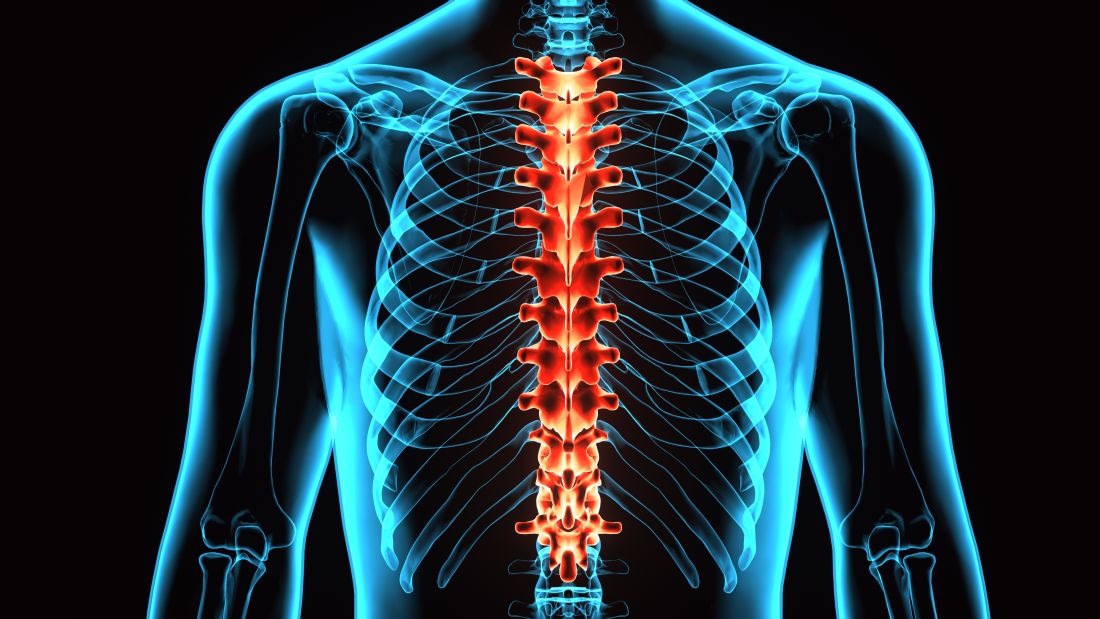
By contrast, the OR for spine fractures was significantly elevated (OR, 2.21; 95% CI, 1.39-3.50; P less than .0001), while risk of hip, rib, and wrist fractures were not, Dr. Komaki and coauthors said in their report.
Steroids were more often being used in the treatment of IBD patients who had fractures than in patients with no fractures, though the finding did not quite reach statistical significance (OR, 1.47; 95% CI, 0.99-2.20; P = .057).
Prior studies of fracture risk in IBD have shown “controversial results,” according to Dr. Komaki and colleagues. Some of those studies suggest an increased risk of fractures, whereas others suggest the risk is not different from what is seen in the general population.
“Individual studies may be underpowered to detect any risk,” they said in the report.
Steroids have been shown to increase risk of spine and rib fracture, but whether those earlier studies apply in IBD is unclear, they noted.
While the present meta-analysis sheds light on fracture risk in IBD patients, further meta-analyses may be needed to specifically look at cohorts of patients with Crohn’s disease and ulcerative colitis.
In this study, the investigators did find that spine fracture risk was significantly elevated in patients with Crohn’s disease, and was trending toward significance for ulcerative colitis patients. They cautioned that those results were based on a limited amount of patient data.
Dr. Komaki reported that he had no disclosures related to the reported study. One study coauthor reported disclosures related to AbbVie and Celltrion.
SOURCE: Komaki Y et al. J Clin Gastroenterol. 2018 Apr 18. 2018 Apr 18. doi: 10.1097/MCG.0000000000001031.
Moreover, fracture risk appears to be higher among IBD patients using steroids, according to a report published in the Journal of Clinical Gastroenterology by Yuga Komaki, MD, of the Inflammatory Bowel Disease Center, University of Chicago, and coauthors.
“Further studies addressing the differential risk among Crohn’s disease and ulcerative colitis are needed, but strict surveillance and prevention of spine fractures are indicated in IBD,” wrote Dr. Komaki and associates.
The systematic review and meta-analysis by Dr. Komaki and colleagues was based on 10 studies comprising 470,541 patients with IBD for whom the risk of fracture was reported.
“It is of importance to identify the risk of fractures, as it will increase patient morbidity, disability, and mortality,” the authors wrote. “However, it is often overlooked in the management of IBD.”
Results of the analysis by this group of researchers showed that there was no significant difference in fracture risk overall between IBD patients and controls (odds ratio, 1.08; 95% confidence interval, 0.72-1.62; P = .70).
By contrast, the OR for spine fractures was significantly elevated (OR, 2.21; 95% CI, 1.39-3.50; P less than .0001), while risk of hip, rib, and wrist fractures were not, Dr. Komaki and coauthors said in their report.
Steroids were more often being used in the treatment of IBD patients who had fractures than in patients with no fractures, though the finding did not quite reach statistical significance (OR, 1.47; 95% CI, 0.99-2.20; P = .057).
Prior studies of fracture risk in IBD have shown “controversial results,” according to Dr. Komaki and colleagues. Some of those studies suggest an increased risk of fractures, whereas others suggest the risk is not different from what is seen in the general population.
“Individual studies may be underpowered to detect any risk,” they said in the report.
Steroids have been shown to increase risk of spine and rib fracture, but whether those earlier studies apply in IBD is unclear, they noted.
While the present meta-analysis sheds light on fracture risk in IBD patients, further meta-analyses may be needed to specifically look at cohorts of patients with Crohn’s disease and ulcerative colitis.
In this study, the investigators did find that spine fracture risk was significantly elevated in patients with Crohn’s disease, and was trending toward significance for ulcerative colitis patients. They cautioned that those results were based on a limited amount of patient data.
Dr. Komaki reported that he had no disclosures related to the reported study. One study coauthor reported disclosures related to AbbVie and Celltrion.
SOURCE: Komaki Y et al. J Clin Gastroenterol. 2018 Apr 18. 2018 Apr 18. doi: 10.1097/MCG.0000000000001031.
Moreover, fracture risk appears to be higher among IBD patients using steroids, according to a report published in the Journal of Clinical Gastroenterology by Yuga Komaki, MD, of the Inflammatory Bowel Disease Center, University of Chicago, and coauthors.
“Further studies addressing the differential risk among Crohn’s disease and ulcerative colitis are needed, but strict surveillance and prevention of spine fractures are indicated in IBD,” wrote Dr. Komaki and associates.
The systematic review and meta-analysis by Dr. Komaki and colleagues was based on 10 studies comprising 470,541 patients with IBD for whom the risk of fracture was reported.
“It is of importance to identify the risk of fractures, as it will increase patient morbidity, disability, and mortality,” the authors wrote. “However, it is often overlooked in the management of IBD.”
Results of the analysis by this group of researchers showed that there was no significant difference in fracture risk overall between IBD patients and controls (odds ratio, 1.08; 95% confidence interval, 0.72-1.62; P = .70).
By contrast, the OR for spine fractures was significantly elevated (OR, 2.21; 95% CI, 1.39-3.50; P less than .0001), while risk of hip, rib, and wrist fractures were not, Dr. Komaki and coauthors said in their report.
Steroids were more often being used in the treatment of IBD patients who had fractures than in patients with no fractures, though the finding did not quite reach statistical significance (OR, 1.47; 95% CI, 0.99-2.20; P = .057).
Prior studies of fracture risk in IBD have shown “controversial results,” according to Dr. Komaki and colleagues. Some of those studies suggest an increased risk of fractures, whereas others suggest the risk is not different from what is seen in the general population.
“Individual studies may be underpowered to detect any risk,” they said in the report.
Steroids have been shown to increase risk of spine and rib fracture, but whether those earlier studies apply in IBD is unclear, they noted.
While the present meta-analysis sheds light on fracture risk in IBD patients, further meta-analyses may be needed to specifically look at cohorts of patients with Crohn’s disease and ulcerative colitis.
In this study, the investigators did find that spine fracture risk was significantly elevated in patients with Crohn’s disease, and was trending toward significance for ulcerative colitis patients. They cautioned that those results were based on a limited amount of patient data.
Dr. Komaki reported that he had no disclosures related to the reported study. One study coauthor reported disclosures related to AbbVie and Celltrion.
SOURCE: Komaki Y et al. J Clin Gastroenterol. 2018 Apr 18. 2018 Apr 18. doi: 10.1097/MCG.0000000000001031.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
Key clinical point: Patients with inflammatory bowel disease may be at increased risk of fractures in the spine.
Major finding: The odds ratio for spine fractures was 2.21 (95% CI, 1.39-3.50; P less than .0001).
Study details: A systematic review and meta-analysis of 10 studies including 470,541 patients.
Disclosures: One study author reported disclosures related to AbbVie and Celltrion.
Source: Komaki Y et al. J Clin Gastroenterol. 2018 Apr 18. doi: 10.1097/MCG.0000000000001031.