User login
Neck and shoulder pain are common presenting symptoms in the general adult population with a 41.7% and 50.9% lifetime incidence in males and females, respectively.1 Generally, a single diagnosis is sought to explain a patient’s signs and symptoms, but occasionally 2 or more different causes are responsible. Only by conducting a thorough history and physical examination with proper follow-up will all contributing diseases be discovered. The following case illustrates 2 distinct etiologies responsible for the patient’s pain, one with an extremely unusual presentation.
Case Presentation
A 23-year-old male presented with a 3-month history of pain, spasm, and tightness of his right upper extremity along his posterior neck, shoulder, and triceps area. The patient reported no history of trauma, but he revealed increasing the amount of weight lifting, and his symptoms were especially worse when bench pressing or performing overhead exercises. No paresthesias were reported.
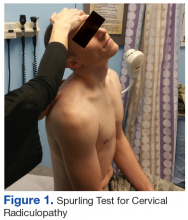
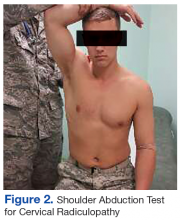
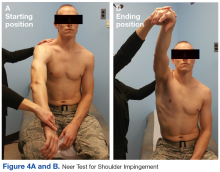
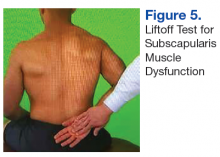
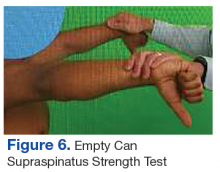
The initial examination revealed a well-developed muscular male with no visible atrophy or tenderness to palpation. He had full range of motion (ROM) of his neck, a normal motor and sensory examination of the C5-T1 nerve roots, and a negative Spurling maneuver. The patient had full ROM of both shoulders but had pain with right shoulder abduction starting at about 120° to 140°. He had pain with resisted supraspinatus muscle testing as well as pain with the liftoff test. The results of the patient’s Hawkins and Neer tests were negative (Table, Figures 1 to 6).2-4 A point-of-care shoulder ultrasound examination revealed no abnormalities.
The working diagnosis was external shoulder impingement with a differential diagnosis of internal impingement and/or cervical radiculopathy. A diagnostic/therapeutic injection of 40 mg of triamcinolone and 4 mL of 1% xylocaine without epinephrine was administered into the right subacromial bursa. The patient experienced immediate and complete relief of pain with repeat shoulder abduction, supraspinatus muscle testing, and the liftoff test. Although this procedure temporarily relieved the pain with movement, a sensation of tightness, pain, and spasm in the posterior shoulder and right posterior arm was still present. The patient was asked to perform therapeutic rotator cuff and scapular strengthening exercises, annotated on a patient information handout, for 15 minutes a day, every other day and to follow-up in 4 weeks.
At follow-up the external impingement symptoms (pain with shoulder abduction, resisted supraspinatus testing and the liftoff test) were fully resolved, but the patient reported persistent pain, spasm, and sensation of tightness in his right posterior shoulder and arm with intermittent extension into forearm and hand. A review of the history reminded the patient of a wrestling episode that caused neck pain months earlier. The patient reported that his current symptoms began after the wrestling episode.
Physical examination at this time revealed pain in the right posterior arm with left lateral neck movement but no neck pain with right lateral neck movement or flexion and extension. There was again a normal motor and sensory examination in the C5-T1 nerve distribution. Of note, there was full painless abduction in the right shoulder, which had improved from the previous examination, and there was no pain with resisted supraspinatus testing or the liftoff test, both of which had been abnormal at the initial encounter.
Due to the patient’s persistent posterior shoulder pain and exacerbation of symptoms with neck movement and the now revealed antecedent event of neck trauma, a higher concern for cervical disc pathology was entertained. A cervical magnetic resonance imaging examination (MRI) was ordered. A moderately sized left paracentral herniation of the disk at C5-C6 was found. The disk herniation was compressing the left ventral hemi-cord with narrowing of the left neuronal foramina. Additionally, there was a mild posterior disc osteophyte complex that caused mild left foraminal narrowing at C6-C7.
Neurosurgical consultation was obtained. Extensive discussion of nonsurgical vs surgical options were conducted, and a trial of nonsurgical therapy was agreed on. Physical therapy with cervical traction was prescribed with 2 sessions a week for 4 weeks. The patient also continued his therapeutic rotator cuff and scapular stabilizing exercises and decreased the amount and intensity of his weight lifting.
At the next 4-week follow-up, his symptoms were greatly reduced. He was discharged from supervised physical therapy and continued his at-home neck and shoulder strengthening regimen. At the 1-year follow-up, the patient reported that the radiating pain had essentially resolved—only occasionally being present with heavy upper-extremity weight lifting or grappling activities. He continues to be symptom free of his external impingement symptoms as well.
The final diagnosis was cervical radiculopathy of C5/6 nerve root due to left paracentral disc herniation with concomitant cord compression as well as external impingement (rotator cuff dysfunction) of the right shoulder. It is unclear whether the disc herniation contributed to the external shoulder impingement due to alterations in biomechanics or whether the 2 diseases were unrelated.
Discussion
The patient’s cervical disc herniation most likely was due to his earlier grappling episode when he had acute trauma to the neck or an exacerbation of an older asymptomatic herniation. His external shoulder impingement likely was due to overuse with heavy weight lifting, which also caused enough mechanical strain to exacerbate the patient’s cervical disc herniation symptoms. What is most unusual about this case is the right-sided cervical radicular symptoms due to a left-sided cervical disc herniation.
With an annual incidence of 107.3 in men and 63.5 in women per 100,000 patients, cervical radiculopathy is caused by compression or irritation of the cervical nerve roots as they exit the spine. The most common cause of cervical radiculopathy is spondylosis followed by disc herniation, but both can be present in the same patient. Spondylosis refers to degeneration of the discs and facet joints but generally without frank disc herniation.5
External shoulder impingement and cervical radiculopathy can have nearly identical symptoms of shoulder and upper arm pain as in this illustrated case. Patients with cervical radiculopathy generally present with neck, shoulder, and arm pain or neurologic deficits. These symptoms alone are very broad and present a wide differential diagnosis. One must determine whether the pain is from the neck or shoulder region.1 The Table and Figures 1 to 6 describe the physical examination maneuvers used to differentiate the etiology.
The decision to pursue imaging should be based on injury severity and patient treatment goals. Although plain radiographic imaging may reveal spondylotic changes, such as degenerative joint changes at the vertebral facets and uncovertebral joints as well as decreased disc space, MRI is the imaging modality of choice for viewing disc herniations.6Nonoperative management of cervical radiculopathy focuses on restoration of full pain-free neck ROM, cervical muscle strengthening, and consideration for cervical traction. The use of either topical or oral medications can be considered if needed to aid in sleep and/or participation in active rehabilitation. Complimentary methods, such as acupuncture, yoga, or therapeutic massage also should be considered. Additionally, corticosteroid epidural injections can be considered, but these have increased risk compared with lumbar epidural injections.7 Surgical indications include persistent symptoms after 6 to 12 weeks of conservative therapy with no improvement of symptoms or progressively worsening motor/neurologic deficits.8
Conclusion
This case illustrates how 2 different conditions can present similarly and lead to diagnostic uncertainty. In this case, both the shoulder impingement and cervical radiculopathy manifested as shoulder and upper arm pain and could be separated only once the impingement had been treated. In addition the left-sided disc herniation causing right-sided symptoms was very unusual. To the best of the authors’ knowledge, this is only the second report of cervical disc herniation causing contralateral symptoms. In the only other available case report on cervical disc herniation with contralateral symptoms, the symptoms occurred in both the contralateral arm and leg.9
1. Briggs AM, Straker LM, Bear NL, Smith AJ. Neck/shoulder pain in adolescents is not related to the level or nature of self-reported physical activity or type of sedentary activity in an Australian pregnancy cohort. BMC Musculoskelet Disord. 2009;10(1):87.
2. Hermans J, Luime JJ, Meuffels DE, Reijman M, Simel DL, Bierma-Zeinstra SM. Does this patient with shoulder pain have rotator cuff disease? JAMA. 2013;310(8):837-847.
3. Rubinstein SM, Pool JJ, van Tulder MW, Riphagen I, Riphagen II, de Vet HC. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J. 2007;16(3):307-319.
4. Ghasemi M, Golabchi K, Mousavi SA, et al. The value of provocative tests in diagnosis of cervical radiculopathy. J Res Med Sci. 2013;18(suppl 1):S35-S38.
5. Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech. 2015;28(5):E251-E259.
6. Green C, Butler J, Eustace S, Poynton A, O’Byrne JM. Imaging modalities for cervical spondylotic stenosis and myelopathy. Adv Orthop. 2012;2012:908324. [Epub July 20, 2011].
7. Childress MA, Beckers BA. Nonoperative management of cervical radiculopathy. Am Fam Physician. 2016;93(9):746-754.
8. Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005;353(4):392-399.
9. Yeung JT, Johnson JI, Karim AS. Cervical disc herniation presenting with neck pain and contralateral symptoms: a case report. J Med Case Rep. 2012;6:166.
Neck and shoulder pain are common presenting symptoms in the general adult population with a 41.7% and 50.9% lifetime incidence in males and females, respectively.1 Generally, a single diagnosis is sought to explain a patient’s signs and symptoms, but occasionally 2 or more different causes are responsible. Only by conducting a thorough history and physical examination with proper follow-up will all contributing diseases be discovered. The following case illustrates 2 distinct etiologies responsible for the patient’s pain, one with an extremely unusual presentation.
Case Presentation
A 23-year-old male presented with a 3-month history of pain, spasm, and tightness of his right upper extremity along his posterior neck, shoulder, and triceps area. The patient reported no history of trauma, but he revealed increasing the amount of weight lifting, and his symptoms were especially worse when bench pressing or performing overhead exercises. No paresthesias were reported.
The initial examination revealed a well-developed muscular male with no visible atrophy or tenderness to palpation. He had full range of motion (ROM) of his neck, a normal motor and sensory examination of the C5-T1 nerve roots, and a negative Spurling maneuver. The patient had full ROM of both shoulders but had pain with right shoulder abduction starting at about 120° to 140°. He had pain with resisted supraspinatus muscle testing as well as pain with the liftoff test. The results of the patient’s Hawkins and Neer tests were negative (Table, Figures 1 to 6).2-4 A point-of-care shoulder ultrasound examination revealed no abnormalities.
The working diagnosis was external shoulder impingement with a differential diagnosis of internal impingement and/or cervical radiculopathy. A diagnostic/therapeutic injection of 40 mg of triamcinolone and 4 mL of 1% xylocaine without epinephrine was administered into the right subacromial bursa. The patient experienced immediate and complete relief of pain with repeat shoulder abduction, supraspinatus muscle testing, and the liftoff test. Although this procedure temporarily relieved the pain with movement, a sensation of tightness, pain, and spasm in the posterior shoulder and right posterior arm was still present. The patient was asked to perform therapeutic rotator cuff and scapular strengthening exercises, annotated on a patient information handout, for 15 minutes a day, every other day and to follow-up in 4 weeks.
At follow-up the external impingement symptoms (pain with shoulder abduction, resisted supraspinatus testing and the liftoff test) were fully resolved, but the patient reported persistent pain, spasm, and sensation of tightness in his right posterior shoulder and arm with intermittent extension into forearm and hand. A review of the history reminded the patient of a wrestling episode that caused neck pain months earlier. The patient reported that his current symptoms began after the wrestling episode.
Physical examination at this time revealed pain in the right posterior arm with left lateral neck movement but no neck pain with right lateral neck movement or flexion and extension. There was again a normal motor and sensory examination in the C5-T1 nerve distribution. Of note, there was full painless abduction in the right shoulder, which had improved from the previous examination, and there was no pain with resisted supraspinatus testing or the liftoff test, both of which had been abnormal at the initial encounter.
Due to the patient’s persistent posterior shoulder pain and exacerbation of symptoms with neck movement and the now revealed antecedent event of neck trauma, a higher concern for cervical disc pathology was entertained. A cervical magnetic resonance imaging examination (MRI) was ordered. A moderately sized left paracentral herniation of the disk at C5-C6 was found. The disk herniation was compressing the left ventral hemi-cord with narrowing of the left neuronal foramina. Additionally, there was a mild posterior disc osteophyte complex that caused mild left foraminal narrowing at C6-C7.
Neurosurgical consultation was obtained. Extensive discussion of nonsurgical vs surgical options were conducted, and a trial of nonsurgical therapy was agreed on. Physical therapy with cervical traction was prescribed with 2 sessions a week for 4 weeks. The patient also continued his therapeutic rotator cuff and scapular stabilizing exercises and decreased the amount and intensity of his weight lifting.
At the next 4-week follow-up, his symptoms were greatly reduced. He was discharged from supervised physical therapy and continued his at-home neck and shoulder strengthening regimen. At the 1-year follow-up, the patient reported that the radiating pain had essentially resolved—only occasionally being present with heavy upper-extremity weight lifting or grappling activities. He continues to be symptom free of his external impingement symptoms as well.
The final diagnosis was cervical radiculopathy of C5/6 nerve root due to left paracentral disc herniation with concomitant cord compression as well as external impingement (rotator cuff dysfunction) of the right shoulder. It is unclear whether the disc herniation contributed to the external shoulder impingement due to alterations in biomechanics or whether the 2 diseases were unrelated.
Discussion
The patient’s cervical disc herniation most likely was due to his earlier grappling episode when he had acute trauma to the neck or an exacerbation of an older asymptomatic herniation. His external shoulder impingement likely was due to overuse with heavy weight lifting, which also caused enough mechanical strain to exacerbate the patient’s cervical disc herniation symptoms. What is most unusual about this case is the right-sided cervical radicular symptoms due to a left-sided cervical disc herniation.
With an annual incidence of 107.3 in men and 63.5 in women per 100,000 patients, cervical radiculopathy is caused by compression or irritation of the cervical nerve roots as they exit the spine. The most common cause of cervical radiculopathy is spondylosis followed by disc herniation, but both can be present in the same patient. Spondylosis refers to degeneration of the discs and facet joints but generally without frank disc herniation.5
External shoulder impingement and cervical radiculopathy can have nearly identical symptoms of shoulder and upper arm pain as in this illustrated case. Patients with cervical radiculopathy generally present with neck, shoulder, and arm pain or neurologic deficits. These symptoms alone are very broad and present a wide differential diagnosis. One must determine whether the pain is from the neck or shoulder region.1 The Table and Figures 1 to 6 describe the physical examination maneuvers used to differentiate the etiology.
The decision to pursue imaging should be based on injury severity and patient treatment goals. Although plain radiographic imaging may reveal spondylotic changes, such as degenerative joint changes at the vertebral facets and uncovertebral joints as well as decreased disc space, MRI is the imaging modality of choice for viewing disc herniations.6Nonoperative management of cervical radiculopathy focuses on restoration of full pain-free neck ROM, cervical muscle strengthening, and consideration for cervical traction. The use of either topical or oral medications can be considered if needed to aid in sleep and/or participation in active rehabilitation. Complimentary methods, such as acupuncture, yoga, or therapeutic massage also should be considered. Additionally, corticosteroid epidural injections can be considered, but these have increased risk compared with lumbar epidural injections.7 Surgical indications include persistent symptoms after 6 to 12 weeks of conservative therapy with no improvement of symptoms or progressively worsening motor/neurologic deficits.8
Conclusion
This case illustrates how 2 different conditions can present similarly and lead to diagnostic uncertainty. In this case, both the shoulder impingement and cervical radiculopathy manifested as shoulder and upper arm pain and could be separated only once the impingement had been treated. In addition the left-sided disc herniation causing right-sided symptoms was very unusual. To the best of the authors’ knowledge, this is only the second report of cervical disc herniation causing contralateral symptoms. In the only other available case report on cervical disc herniation with contralateral symptoms, the symptoms occurred in both the contralateral arm and leg.9
Neck and shoulder pain are common presenting symptoms in the general adult population with a 41.7% and 50.9% lifetime incidence in males and females, respectively.1 Generally, a single diagnosis is sought to explain a patient’s signs and symptoms, but occasionally 2 or more different causes are responsible. Only by conducting a thorough history and physical examination with proper follow-up will all contributing diseases be discovered. The following case illustrates 2 distinct etiologies responsible for the patient’s pain, one with an extremely unusual presentation.
Case Presentation
A 23-year-old male presented with a 3-month history of pain, spasm, and tightness of his right upper extremity along his posterior neck, shoulder, and triceps area. The patient reported no history of trauma, but he revealed increasing the amount of weight lifting, and his symptoms were especially worse when bench pressing or performing overhead exercises. No paresthesias were reported.
The initial examination revealed a well-developed muscular male with no visible atrophy or tenderness to palpation. He had full range of motion (ROM) of his neck, a normal motor and sensory examination of the C5-T1 nerve roots, and a negative Spurling maneuver. The patient had full ROM of both shoulders but had pain with right shoulder abduction starting at about 120° to 140°. He had pain with resisted supraspinatus muscle testing as well as pain with the liftoff test. The results of the patient’s Hawkins and Neer tests were negative (Table, Figures 1 to 6).2-4 A point-of-care shoulder ultrasound examination revealed no abnormalities.
The working diagnosis was external shoulder impingement with a differential diagnosis of internal impingement and/or cervical radiculopathy. A diagnostic/therapeutic injection of 40 mg of triamcinolone and 4 mL of 1% xylocaine without epinephrine was administered into the right subacromial bursa. The patient experienced immediate and complete relief of pain with repeat shoulder abduction, supraspinatus muscle testing, and the liftoff test. Although this procedure temporarily relieved the pain with movement, a sensation of tightness, pain, and spasm in the posterior shoulder and right posterior arm was still present. The patient was asked to perform therapeutic rotator cuff and scapular strengthening exercises, annotated on a patient information handout, for 15 minutes a day, every other day and to follow-up in 4 weeks.
At follow-up the external impingement symptoms (pain with shoulder abduction, resisted supraspinatus testing and the liftoff test) were fully resolved, but the patient reported persistent pain, spasm, and sensation of tightness in his right posterior shoulder and arm with intermittent extension into forearm and hand. A review of the history reminded the patient of a wrestling episode that caused neck pain months earlier. The patient reported that his current symptoms began after the wrestling episode.
Physical examination at this time revealed pain in the right posterior arm with left lateral neck movement but no neck pain with right lateral neck movement or flexion and extension. There was again a normal motor and sensory examination in the C5-T1 nerve distribution. Of note, there was full painless abduction in the right shoulder, which had improved from the previous examination, and there was no pain with resisted supraspinatus testing or the liftoff test, both of which had been abnormal at the initial encounter.
Due to the patient’s persistent posterior shoulder pain and exacerbation of symptoms with neck movement and the now revealed antecedent event of neck trauma, a higher concern for cervical disc pathology was entertained. A cervical magnetic resonance imaging examination (MRI) was ordered. A moderately sized left paracentral herniation of the disk at C5-C6 was found. The disk herniation was compressing the left ventral hemi-cord with narrowing of the left neuronal foramina. Additionally, there was a mild posterior disc osteophyte complex that caused mild left foraminal narrowing at C6-C7.
Neurosurgical consultation was obtained. Extensive discussion of nonsurgical vs surgical options were conducted, and a trial of nonsurgical therapy was agreed on. Physical therapy with cervical traction was prescribed with 2 sessions a week for 4 weeks. The patient also continued his therapeutic rotator cuff and scapular stabilizing exercises and decreased the amount and intensity of his weight lifting.
At the next 4-week follow-up, his symptoms were greatly reduced. He was discharged from supervised physical therapy and continued his at-home neck and shoulder strengthening regimen. At the 1-year follow-up, the patient reported that the radiating pain had essentially resolved—only occasionally being present with heavy upper-extremity weight lifting or grappling activities. He continues to be symptom free of his external impingement symptoms as well.
The final diagnosis was cervical radiculopathy of C5/6 nerve root due to left paracentral disc herniation with concomitant cord compression as well as external impingement (rotator cuff dysfunction) of the right shoulder. It is unclear whether the disc herniation contributed to the external shoulder impingement due to alterations in biomechanics or whether the 2 diseases were unrelated.
Discussion
The patient’s cervical disc herniation most likely was due to his earlier grappling episode when he had acute trauma to the neck or an exacerbation of an older asymptomatic herniation. His external shoulder impingement likely was due to overuse with heavy weight lifting, which also caused enough mechanical strain to exacerbate the patient’s cervical disc herniation symptoms. What is most unusual about this case is the right-sided cervical radicular symptoms due to a left-sided cervical disc herniation.
With an annual incidence of 107.3 in men and 63.5 in women per 100,000 patients, cervical radiculopathy is caused by compression or irritation of the cervical nerve roots as they exit the spine. The most common cause of cervical radiculopathy is spondylosis followed by disc herniation, but both can be present in the same patient. Spondylosis refers to degeneration of the discs and facet joints but generally without frank disc herniation.5
External shoulder impingement and cervical radiculopathy can have nearly identical symptoms of shoulder and upper arm pain as in this illustrated case. Patients with cervical radiculopathy generally present with neck, shoulder, and arm pain or neurologic deficits. These symptoms alone are very broad and present a wide differential diagnosis. One must determine whether the pain is from the neck or shoulder region.1 The Table and Figures 1 to 6 describe the physical examination maneuvers used to differentiate the etiology.
The decision to pursue imaging should be based on injury severity and patient treatment goals. Although plain radiographic imaging may reveal spondylotic changes, such as degenerative joint changes at the vertebral facets and uncovertebral joints as well as decreased disc space, MRI is the imaging modality of choice for viewing disc herniations.6Nonoperative management of cervical radiculopathy focuses on restoration of full pain-free neck ROM, cervical muscle strengthening, and consideration for cervical traction. The use of either topical or oral medications can be considered if needed to aid in sleep and/or participation in active rehabilitation. Complimentary methods, such as acupuncture, yoga, or therapeutic massage also should be considered. Additionally, corticosteroid epidural injections can be considered, but these have increased risk compared with lumbar epidural injections.7 Surgical indications include persistent symptoms after 6 to 12 weeks of conservative therapy with no improvement of symptoms or progressively worsening motor/neurologic deficits.8
Conclusion
This case illustrates how 2 different conditions can present similarly and lead to diagnostic uncertainty. In this case, both the shoulder impingement and cervical radiculopathy manifested as shoulder and upper arm pain and could be separated only once the impingement had been treated. In addition the left-sided disc herniation causing right-sided symptoms was very unusual. To the best of the authors’ knowledge, this is only the second report of cervical disc herniation causing contralateral symptoms. In the only other available case report on cervical disc herniation with contralateral symptoms, the symptoms occurred in both the contralateral arm and leg.9
1. Briggs AM, Straker LM, Bear NL, Smith AJ. Neck/shoulder pain in adolescents is not related to the level or nature of self-reported physical activity or type of sedentary activity in an Australian pregnancy cohort. BMC Musculoskelet Disord. 2009;10(1):87.
2. Hermans J, Luime JJ, Meuffels DE, Reijman M, Simel DL, Bierma-Zeinstra SM. Does this patient with shoulder pain have rotator cuff disease? JAMA. 2013;310(8):837-847.
3. Rubinstein SM, Pool JJ, van Tulder MW, Riphagen I, Riphagen II, de Vet HC. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J. 2007;16(3):307-319.
4. Ghasemi M, Golabchi K, Mousavi SA, et al. The value of provocative tests in diagnosis of cervical radiculopathy. J Res Med Sci. 2013;18(suppl 1):S35-S38.
5. Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech. 2015;28(5):E251-E259.
6. Green C, Butler J, Eustace S, Poynton A, O’Byrne JM. Imaging modalities for cervical spondylotic stenosis and myelopathy. Adv Orthop. 2012;2012:908324. [Epub July 20, 2011].
7. Childress MA, Beckers BA. Nonoperative management of cervical radiculopathy. Am Fam Physician. 2016;93(9):746-754.
8. Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005;353(4):392-399.
9. Yeung JT, Johnson JI, Karim AS. Cervical disc herniation presenting with neck pain and contralateral symptoms: a case report. J Med Case Rep. 2012;6:166.
1. Briggs AM, Straker LM, Bear NL, Smith AJ. Neck/shoulder pain in adolescents is not related to the level or nature of self-reported physical activity or type of sedentary activity in an Australian pregnancy cohort. BMC Musculoskelet Disord. 2009;10(1):87.
2. Hermans J, Luime JJ, Meuffels DE, Reijman M, Simel DL, Bierma-Zeinstra SM. Does this patient with shoulder pain have rotator cuff disease? JAMA. 2013;310(8):837-847.
3. Rubinstein SM, Pool JJ, van Tulder MW, Riphagen I, Riphagen II, de Vet HC. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J. 2007;16(3):307-319.
4. Ghasemi M, Golabchi K, Mousavi SA, et al. The value of provocative tests in diagnosis of cervical radiculopathy. J Res Med Sci. 2013;18(suppl 1):S35-S38.
5. Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech. 2015;28(5):E251-E259.
6. Green C, Butler J, Eustace S, Poynton A, O’Byrne JM. Imaging modalities for cervical spondylotic stenosis and myelopathy. Adv Orthop. 2012;2012:908324. [Epub July 20, 2011].
7. Childress MA, Beckers BA. Nonoperative management of cervical radiculopathy. Am Fam Physician. 2016;93(9):746-754.
8. Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005;353(4):392-399.
9. Yeung JT, Johnson JI, Karim AS. Cervical disc herniation presenting with neck pain and contralateral symptoms: a case report. J Med Case Rep. 2012;6:166.