User login
A recent explosion of interest in robotic surgery for routine hysterectomies and treatment of other nononcologic gynecologic conditions is raising concern about the cost and comparative value of the robot over conventional laparoscopy, as well as the future of vaginal hysterectomy and current and future training needs.
In 2010, for the first time, more hysterectomies were performed with the da Vinci Surgical System than any other procedure, including prostatectomy. The number of robotic-assisted hysterectomies performed worldwide grew to 110,000 in 2010, from approximately 69,000 the year before.
Approximately 32,000 of these hysterectomies were for treatment of cancer, and the remaining 78,000 were related to benign conditions, according to Chris Simmonds, senior director of marketing for Intuitive Surgical, which makes the da Vinci, the only such system currently on the market.
Gynecologic oncologists swiftly embraced the robotic surgical system after it was approved in 2005 for gynecologic surgical procedures because it enabled them to perform minimally invasive endometrial cancer staging – something most surgeons found too technically challenging with pure laparoscopy.
While issues of cost and training have been part of an ongoing debate in gynecologic oncology, such issues have taken on new meaning – and more urgency – with the more recent rise in robotically-assisted routine hysterectomy. It can be argued, some experts explain, that an advantage exists for robotics in gynecologic oncology that, overall, does not exist for benign disease.
"Robotics will probably be the future of surgery," said Dr. Resad P. Pasic, professor of obstetrics and gynecology and director of operative gynecologic endoscopy at the University of Louisville (Ky.). "We need to [better understand] what the real advantages are, however, especially for routine laparoscopic hysterectomies, because the cost is higher than traditional laparoscopy and vaginal surgery."
Robotic assistance "is great for some procedures, like myomectomies, where there is more suturing. But I really don’t see a huge benefit overall for less complex, benign cases," he said in an interview. "We’re even seeing supracervical hysterectomies being done [robotically] – that doesn’t make any sense."
A study published last year, which Dr. Pasic coauthored, found higher per-case hospital costs with robotic-assisted hysterectomies, compared with conventional laparoscopic hysterectomies, without any significant differences in complications, postsurgical infections, or frequency of hemorrhage.
Robot-assisted hysterectomies were associated with longer surgical times and cost an average of $2,600 more, the investigators reported (J. Minim. Invasive Gynecol. 2010;17:730-8).
Using the Premier hospital database, they analyzed patient records and billing and insurance data for more than 36,000 women who received minimally invasive hysterectomy during 2007-2008 in more than 350 hospitals. Their cost analysis reflected the cost of the robotic procedure to the hospital but did not include the acquisition or maintenance costs of the robotic device over time.
The robotic unit costs between $1 million and $2.3 million and is associated with annual maintenance costs of $100,000-$170,000 a year, and instrumentation/accessories costs of $1,300-$2,200 per procedure, according to Intuitive Surgical.
"Further decisions regarding the diffusion of robot technology in routine laparoscopic hysterectomy," they concluded, must be informed by randomized controlled studies of comparative effectiveness.
At the annual meeting of the American Association of Gynecologic Laparoscopists last month, the paper won the organization’s Robert Hunt Award for the "best article" published in the Journal of Minimally Invasive Gynecology in the past year. The study may cause some to pause, however, in that it was funded by Ethicon Endo-Surgery, and because three of the six coauthors have notable ties with Ethicon – one is employed by the company, one is a consultant, and Dr. Pasic is a speaker for the company.
Dr. Pasic, who said he uses the da Vinci for about 10% of his procedures, dismissed any suggestions of bias. "We’re not the only paper concluding there is a high cost to robotics, and we made every effort to be as impartial as possible," he said.
Authors of a broader recently-published analysis of robotic-assisted surgery and health care costs drew similar conclusions about comparative value. The investigators examined all the cost studies of robot-assisted procedures published since 2005 and reported that, on average, "across the full range of 20 types of surgery for which studies exist," the additional cost of using a robot-assisted procedure was about $1,600, or about 6% of the cost of the procedure in 2007 (N. Eng. J. Med. 2010;363:701-4).
There have not been any large-scale randomized trials of robot-assisted surgery, and the "limited observational evidence fails to show that the long-term outcomes of robot-assisted surgery are superior to those of conventional procedures," said Dr. Gabriel I. Barbash of the medical school at Tel Aviv (Israel) University and Sherry A. Glied, Ph.D., of the school of public health at Columbia University, New York.
With hysterectomy, a pure vaginal approach has long been viewed by many experts as the preferable approach whenever possible – the most cost-effective minimally invasive method – and some experts are concerned that the growing popularity of robotics may chip away at its use.
"Vaginal hysterectomy is an art, so the question is, are we killing the art with the new technology we’re using for laparoscopy and now robotics? Maybe ... there are some studies suggesting [this], but we have no definitive data," Dr. Pasic said.
Dr. Javier Magrina, a professor of obstetrics and gynecology and director of gynecologic oncology at the Mayo Clinic in Scottsdale, Ariz., who has written and lectured extensively on robotic surgery from the standpoint of both benign and malignant disease, said that so far, vaginal hysterectomy rates appear to be "stable in spite of robotics," comprising about 20%-25% of all hysterectomies. "The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good," he said in an interview.
Dr. Jed Delmore and his colleagues at the University of Kansas in Wichita found just this when they compared the types of hysterectomy performed at their teaching hospital and two outpatient surgery centers during two periods of time: before robotic surgery became locally available (2006-2007) and 2 years after it arrived (2009-2010).
Using electronic medical record and billing data to identify hysterectomies, they found that the number of abdominal hysterectomies decreased significantly, while the number of vaginal hysterectomies remained relatively constant. The unpublished findings were presented at the American Congress of Obstetricians and Gynecologists District VII meeting in Kansas City in September.
"At least in our community of 400,000 women, there was a positive shift," Dr. Delmore said in an interview.
Still, he said, the potential longer-term impact of robotics on vaginal hysterectomy is a concern. "If there’s a big shift from abdominal surgery to robotic surgery, that will be cost-effective. ... But if it turns out that over time fewer women end up having vaginal hysterectomies, and have robotic hysterectomies instead, there will be greater expense to individuals and society," said Dr. Delmore, professor of obstetrics and gynecology and director of gynecologic oncology at the university.
An even larger concern, he noted, is "whether robotic surgery, as it becomes more and more available, will increase the total volume of hysterectomies – in women who would have previously been treated with hormone therapy or [other modalities]."
Such a trend may be occurring with prostatectomy, note the authors of the New England Journal of Medicine cost analysis, with robotic technology possibly contributing to the substitution of surgical for non-surgical treatments for prostate cancer.
This does not appear to be happening with hysterectomy in the Kansas City area thus far, Dr. Delmore said.
The undercurrents may already exist, however. Gynecology is one of Intuitive Surgical’s five main "target markets," according to a company investor presentation, and hysterectomy is one of four "target" gynecologic procedures, along with sacral colpopexy, myomectomy, and endometrial resection.
With an estimated 600,000 hysterectomies being performed each year in the United States, Intuitive sees potential for growth. As of this fall, the 2011 surgical volume with the da Vinci had increased 30% over 2010 volume across all types of procedures, said Intuitive Surgical’s Mr. Simmonds.
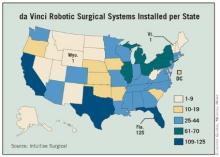
Having a surgical robot has become a status symbol of sorts for hospitals in many urban areas – as of September, Intuitive had installed 1,478 da Vinci surgical systems in the United States – and ob.gyns. may feel compelled to keep up with market demands.
"General ob.gyns. don’t want to be the only physicians in the community not offering it," said Dr. Delmore, who teaches robotic surgery as a proctor for Intuitive Surgical.
Many ob.gyns., moreover, find robotic-assisted laparoscopy much easier than conventional laparoscopy to learn and adopt. Suturing is easier, and Dr. Magrina and other proponents of robotics maintain that the advantages of instrument articulation and steady three-dimensional vision have proven even higher than expected – for hysterectomies as well as more complex gynecologic procedures.
While the learning curve for robotics is said to be relatively short, Dr. Pasic and his coauthors caution that robotic assistance should not be used by physicians who are unwilling to invest time and effort into laparoscopic training. Exuberance for the da Vinci could have an "unintended negative effect on resident and fellow training as it relates to overall laparoscopic competencies," they said.
Institutions, in the meantime, are individually attempting to determine how best to train residents in robotic-assisted surgery. The University of Kansas is implementing a training model for ob.gyn. residents that includes an online tutorial, training with inanimate objects, animal lab training, and bedside assistance in real robotic-assisted hysterectomies.
Dr. Delmore and his colleagues have a study underway to look at how graduate ob.gyns. utilize this training. "What if residents go somewhere afterward where there isn’t a robot, for instance? Will [they have learned enough] to safely operate?" he said.
Dr. Magrina said he had no relevant financial disclosures. Dr. Delmore teaches robotic surgery as a proctor for Intuitive Surgical. Dr. Pasic is a speaker for Ethicon Endo-Surgery.
A recent explosion of interest in robotic surgery for routine hysterectomies and treatment of other nononcologic gynecologic conditions is raising concern about the cost and comparative value of the robot over conventional laparoscopy, as well as the future of vaginal hysterectomy and current and future training needs.
In 2010, for the first time, more hysterectomies were performed with the da Vinci Surgical System than any other procedure, including prostatectomy. The number of robotic-assisted hysterectomies performed worldwide grew to 110,000 in 2010, from approximately 69,000 the year before.
Approximately 32,000 of these hysterectomies were for treatment of cancer, and the remaining 78,000 were related to benign conditions, according to Chris Simmonds, senior director of marketing for Intuitive Surgical, which makes the da Vinci, the only such system currently on the market.
Gynecologic oncologists swiftly embraced the robotic surgical system after it was approved in 2005 for gynecologic surgical procedures because it enabled them to perform minimally invasive endometrial cancer staging – something most surgeons found too technically challenging with pure laparoscopy.
While issues of cost and training have been part of an ongoing debate in gynecologic oncology, such issues have taken on new meaning – and more urgency – with the more recent rise in robotically-assisted routine hysterectomy. It can be argued, some experts explain, that an advantage exists for robotics in gynecologic oncology that, overall, does not exist for benign disease.
"Robotics will probably be the future of surgery," said Dr. Resad P. Pasic, professor of obstetrics and gynecology and director of operative gynecologic endoscopy at the University of Louisville (Ky.). "We need to [better understand] what the real advantages are, however, especially for routine laparoscopic hysterectomies, because the cost is higher than traditional laparoscopy and vaginal surgery."
Robotic assistance "is great for some procedures, like myomectomies, where there is more suturing. But I really don’t see a huge benefit overall for less complex, benign cases," he said in an interview. "We’re even seeing supracervical hysterectomies being done [robotically] – that doesn’t make any sense."
A study published last year, which Dr. Pasic coauthored, found higher per-case hospital costs with robotic-assisted hysterectomies, compared with conventional laparoscopic hysterectomies, without any significant differences in complications, postsurgical infections, or frequency of hemorrhage.
Robot-assisted hysterectomies were associated with longer surgical times and cost an average of $2,600 more, the investigators reported (J. Minim. Invasive Gynecol. 2010;17:730-8).
Using the Premier hospital database, they analyzed patient records and billing and insurance data for more than 36,000 women who received minimally invasive hysterectomy during 2007-2008 in more than 350 hospitals. Their cost analysis reflected the cost of the robotic procedure to the hospital but did not include the acquisition or maintenance costs of the robotic device over time.
The robotic unit costs between $1 million and $2.3 million and is associated with annual maintenance costs of $100,000-$170,000 a year, and instrumentation/accessories costs of $1,300-$2,200 per procedure, according to Intuitive Surgical.
"Further decisions regarding the diffusion of robot technology in routine laparoscopic hysterectomy," they concluded, must be informed by randomized controlled studies of comparative effectiveness.
At the annual meeting of the American Association of Gynecologic Laparoscopists last month, the paper won the organization’s Robert Hunt Award for the "best article" published in the Journal of Minimally Invasive Gynecology in the past year. The study may cause some to pause, however, in that it was funded by Ethicon Endo-Surgery, and because three of the six coauthors have notable ties with Ethicon – one is employed by the company, one is a consultant, and Dr. Pasic is a speaker for the company.
Dr. Pasic, who said he uses the da Vinci for about 10% of his procedures, dismissed any suggestions of bias. "We’re not the only paper concluding there is a high cost to robotics, and we made every effort to be as impartial as possible," he said.
Authors of a broader recently-published analysis of robotic-assisted surgery and health care costs drew similar conclusions about comparative value. The investigators examined all the cost studies of robot-assisted procedures published since 2005 and reported that, on average, "across the full range of 20 types of surgery for which studies exist," the additional cost of using a robot-assisted procedure was about $1,600, or about 6% of the cost of the procedure in 2007 (N. Eng. J. Med. 2010;363:701-4).
There have not been any large-scale randomized trials of robot-assisted surgery, and the "limited observational evidence fails to show that the long-term outcomes of robot-assisted surgery are superior to those of conventional procedures," said Dr. Gabriel I. Barbash of the medical school at Tel Aviv (Israel) University and Sherry A. Glied, Ph.D., of the school of public health at Columbia University, New York.
With hysterectomy, a pure vaginal approach has long been viewed by many experts as the preferable approach whenever possible – the most cost-effective minimally invasive method – and some experts are concerned that the growing popularity of robotics may chip away at its use.
"Vaginal hysterectomy is an art, so the question is, are we killing the art with the new technology we’re using for laparoscopy and now robotics? Maybe ... there are some studies suggesting [this], but we have no definitive data," Dr. Pasic said.
Dr. Javier Magrina, a professor of obstetrics and gynecology and director of gynecologic oncology at the Mayo Clinic in Scottsdale, Ariz., who has written and lectured extensively on robotic surgery from the standpoint of both benign and malignant disease, said that so far, vaginal hysterectomy rates appear to be "stable in spite of robotics," comprising about 20%-25% of all hysterectomies. "The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good," he said in an interview.
Dr. Jed Delmore and his colleagues at the University of Kansas in Wichita found just this when they compared the types of hysterectomy performed at their teaching hospital and two outpatient surgery centers during two periods of time: before robotic surgery became locally available (2006-2007) and 2 years after it arrived (2009-2010).
Using electronic medical record and billing data to identify hysterectomies, they found that the number of abdominal hysterectomies decreased significantly, while the number of vaginal hysterectomies remained relatively constant. The unpublished findings were presented at the American Congress of Obstetricians and Gynecologists District VII meeting in Kansas City in September.
"At least in our community of 400,000 women, there was a positive shift," Dr. Delmore said in an interview.
Still, he said, the potential longer-term impact of robotics on vaginal hysterectomy is a concern. "If there’s a big shift from abdominal surgery to robotic surgery, that will be cost-effective. ... But if it turns out that over time fewer women end up having vaginal hysterectomies, and have robotic hysterectomies instead, there will be greater expense to individuals and society," said Dr. Delmore, professor of obstetrics and gynecology and director of gynecologic oncology at the university.
An even larger concern, he noted, is "whether robotic surgery, as it becomes more and more available, will increase the total volume of hysterectomies – in women who would have previously been treated with hormone therapy or [other modalities]."
Such a trend may be occurring with prostatectomy, note the authors of the New England Journal of Medicine cost analysis, with robotic technology possibly contributing to the substitution of surgical for non-surgical treatments for prostate cancer.
This does not appear to be happening with hysterectomy in the Kansas City area thus far, Dr. Delmore said.
The undercurrents may already exist, however. Gynecology is one of Intuitive Surgical’s five main "target markets," according to a company investor presentation, and hysterectomy is one of four "target" gynecologic procedures, along with sacral colpopexy, myomectomy, and endometrial resection.
With an estimated 600,000 hysterectomies being performed each year in the United States, Intuitive sees potential for growth. As of this fall, the 2011 surgical volume with the da Vinci had increased 30% over 2010 volume across all types of procedures, said Intuitive Surgical’s Mr. Simmonds.
Having a surgical robot has become a status symbol of sorts for hospitals in many urban areas – as of September, Intuitive had installed 1,478 da Vinci surgical systems in the United States – and ob.gyns. may feel compelled to keep up with market demands.
"General ob.gyns. don’t want to be the only physicians in the community not offering it," said Dr. Delmore, who teaches robotic surgery as a proctor for Intuitive Surgical.
Many ob.gyns., moreover, find robotic-assisted laparoscopy much easier than conventional laparoscopy to learn and adopt. Suturing is easier, and Dr. Magrina and other proponents of robotics maintain that the advantages of instrument articulation and steady three-dimensional vision have proven even higher than expected – for hysterectomies as well as more complex gynecologic procedures.
While the learning curve for robotics is said to be relatively short, Dr. Pasic and his coauthors caution that robotic assistance should not be used by physicians who are unwilling to invest time and effort into laparoscopic training. Exuberance for the da Vinci could have an "unintended negative effect on resident and fellow training as it relates to overall laparoscopic competencies," they said.
Institutions, in the meantime, are individually attempting to determine how best to train residents in robotic-assisted surgery. The University of Kansas is implementing a training model for ob.gyn. residents that includes an online tutorial, training with inanimate objects, animal lab training, and bedside assistance in real robotic-assisted hysterectomies.
Dr. Delmore and his colleagues have a study underway to look at how graduate ob.gyns. utilize this training. "What if residents go somewhere afterward where there isn’t a robot, for instance? Will [they have learned enough] to safely operate?" he said.
Dr. Magrina said he had no relevant financial disclosures. Dr. Delmore teaches robotic surgery as a proctor for Intuitive Surgical. Dr. Pasic is a speaker for Ethicon Endo-Surgery.
A recent explosion of interest in robotic surgery for routine hysterectomies and treatment of other nononcologic gynecologic conditions is raising concern about the cost and comparative value of the robot over conventional laparoscopy, as well as the future of vaginal hysterectomy and current and future training needs.
In 2010, for the first time, more hysterectomies were performed with the da Vinci Surgical System than any other procedure, including prostatectomy. The number of robotic-assisted hysterectomies performed worldwide grew to 110,000 in 2010, from approximately 69,000 the year before.
Approximately 32,000 of these hysterectomies were for treatment of cancer, and the remaining 78,000 were related to benign conditions, according to Chris Simmonds, senior director of marketing for Intuitive Surgical, which makes the da Vinci, the only such system currently on the market.
Gynecologic oncologists swiftly embraced the robotic surgical system after it was approved in 2005 for gynecologic surgical procedures because it enabled them to perform minimally invasive endometrial cancer staging – something most surgeons found too technically challenging with pure laparoscopy.
While issues of cost and training have been part of an ongoing debate in gynecologic oncology, such issues have taken on new meaning – and more urgency – with the more recent rise in robotically-assisted routine hysterectomy. It can be argued, some experts explain, that an advantage exists for robotics in gynecologic oncology that, overall, does not exist for benign disease.
"Robotics will probably be the future of surgery," said Dr. Resad P. Pasic, professor of obstetrics and gynecology and director of operative gynecologic endoscopy at the University of Louisville (Ky.). "We need to [better understand] what the real advantages are, however, especially for routine laparoscopic hysterectomies, because the cost is higher than traditional laparoscopy and vaginal surgery."
Robotic assistance "is great for some procedures, like myomectomies, where there is more suturing. But I really don’t see a huge benefit overall for less complex, benign cases," he said in an interview. "We’re even seeing supracervical hysterectomies being done [robotically] – that doesn’t make any sense."
A study published last year, which Dr. Pasic coauthored, found higher per-case hospital costs with robotic-assisted hysterectomies, compared with conventional laparoscopic hysterectomies, without any significant differences in complications, postsurgical infections, or frequency of hemorrhage.
Robot-assisted hysterectomies were associated with longer surgical times and cost an average of $2,600 more, the investigators reported (J. Minim. Invasive Gynecol. 2010;17:730-8).
Using the Premier hospital database, they analyzed patient records and billing and insurance data for more than 36,000 women who received minimally invasive hysterectomy during 2007-2008 in more than 350 hospitals. Their cost analysis reflected the cost of the robotic procedure to the hospital but did not include the acquisition or maintenance costs of the robotic device over time.
The robotic unit costs between $1 million and $2.3 million and is associated with annual maintenance costs of $100,000-$170,000 a year, and instrumentation/accessories costs of $1,300-$2,200 per procedure, according to Intuitive Surgical.
"Further decisions regarding the diffusion of robot technology in routine laparoscopic hysterectomy," they concluded, must be informed by randomized controlled studies of comparative effectiveness.
At the annual meeting of the American Association of Gynecologic Laparoscopists last month, the paper won the organization’s Robert Hunt Award for the "best article" published in the Journal of Minimally Invasive Gynecology in the past year. The study may cause some to pause, however, in that it was funded by Ethicon Endo-Surgery, and because three of the six coauthors have notable ties with Ethicon – one is employed by the company, one is a consultant, and Dr. Pasic is a speaker for the company.
Dr. Pasic, who said he uses the da Vinci for about 10% of his procedures, dismissed any suggestions of bias. "We’re not the only paper concluding there is a high cost to robotics, and we made every effort to be as impartial as possible," he said.
Authors of a broader recently-published analysis of robotic-assisted surgery and health care costs drew similar conclusions about comparative value. The investigators examined all the cost studies of robot-assisted procedures published since 2005 and reported that, on average, "across the full range of 20 types of surgery for which studies exist," the additional cost of using a robot-assisted procedure was about $1,600, or about 6% of the cost of the procedure in 2007 (N. Eng. J. Med. 2010;363:701-4).
There have not been any large-scale randomized trials of robot-assisted surgery, and the "limited observational evidence fails to show that the long-term outcomes of robot-assisted surgery are superior to those of conventional procedures," said Dr. Gabriel I. Barbash of the medical school at Tel Aviv (Israel) University and Sherry A. Glied, Ph.D., of the school of public health at Columbia University, New York.
With hysterectomy, a pure vaginal approach has long been viewed by many experts as the preferable approach whenever possible – the most cost-effective minimally invasive method – and some experts are concerned that the growing popularity of robotics may chip away at its use.
"Vaginal hysterectomy is an art, so the question is, are we killing the art with the new technology we’re using for laparoscopy and now robotics? Maybe ... there are some studies suggesting [this], but we have no definitive data," Dr. Pasic said.
Dr. Javier Magrina, a professor of obstetrics and gynecology and director of gynecologic oncology at the Mayo Clinic in Scottsdale, Ariz., who has written and lectured extensively on robotic surgery from the standpoint of both benign and malignant disease, said that so far, vaginal hysterectomy rates appear to be "stable in spite of robotics," comprising about 20%-25% of all hysterectomies. "The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good," he said in an interview.
Dr. Jed Delmore and his colleagues at the University of Kansas in Wichita found just this when they compared the types of hysterectomy performed at their teaching hospital and two outpatient surgery centers during two periods of time: before robotic surgery became locally available (2006-2007) and 2 years after it arrived (2009-2010).
Using electronic medical record and billing data to identify hysterectomies, they found that the number of abdominal hysterectomies decreased significantly, while the number of vaginal hysterectomies remained relatively constant. The unpublished findings were presented at the American Congress of Obstetricians and Gynecologists District VII meeting in Kansas City in September.
"At least in our community of 400,000 women, there was a positive shift," Dr. Delmore said in an interview.
Still, he said, the potential longer-term impact of robotics on vaginal hysterectomy is a concern. "If there’s a big shift from abdominal surgery to robotic surgery, that will be cost-effective. ... But if it turns out that over time fewer women end up having vaginal hysterectomies, and have robotic hysterectomies instead, there will be greater expense to individuals and society," said Dr. Delmore, professor of obstetrics and gynecology and director of gynecologic oncology at the university.
An even larger concern, he noted, is "whether robotic surgery, as it becomes more and more available, will increase the total volume of hysterectomies – in women who would have previously been treated with hormone therapy or [other modalities]."
Such a trend may be occurring with prostatectomy, note the authors of the New England Journal of Medicine cost analysis, with robotic technology possibly contributing to the substitution of surgical for non-surgical treatments for prostate cancer.
This does not appear to be happening with hysterectomy in the Kansas City area thus far, Dr. Delmore said.
The undercurrents may already exist, however. Gynecology is one of Intuitive Surgical’s five main "target markets," according to a company investor presentation, and hysterectomy is one of four "target" gynecologic procedures, along with sacral colpopexy, myomectomy, and endometrial resection.
With an estimated 600,000 hysterectomies being performed each year in the United States, Intuitive sees potential for growth. As of this fall, the 2011 surgical volume with the da Vinci had increased 30% over 2010 volume across all types of procedures, said Intuitive Surgical’s Mr. Simmonds.
Having a surgical robot has become a status symbol of sorts for hospitals in many urban areas – as of September, Intuitive had installed 1,478 da Vinci surgical systems in the United States – and ob.gyns. may feel compelled to keep up with market demands.
"General ob.gyns. don’t want to be the only physicians in the community not offering it," said Dr. Delmore, who teaches robotic surgery as a proctor for Intuitive Surgical.
Many ob.gyns., moreover, find robotic-assisted laparoscopy much easier than conventional laparoscopy to learn and adopt. Suturing is easier, and Dr. Magrina and other proponents of robotics maintain that the advantages of instrument articulation and steady three-dimensional vision have proven even higher than expected – for hysterectomies as well as more complex gynecologic procedures.
While the learning curve for robotics is said to be relatively short, Dr. Pasic and his coauthors caution that robotic assistance should not be used by physicians who are unwilling to invest time and effort into laparoscopic training. Exuberance for the da Vinci could have an "unintended negative effect on resident and fellow training as it relates to overall laparoscopic competencies," they said.
Institutions, in the meantime, are individually attempting to determine how best to train residents in robotic-assisted surgery. The University of Kansas is implementing a training model for ob.gyn. residents that includes an online tutorial, training with inanimate objects, animal lab training, and bedside assistance in real robotic-assisted hysterectomies.
Dr. Delmore and his colleagues have a study underway to look at how graduate ob.gyns. utilize this training. "What if residents go somewhere afterward where there isn’t a robot, for instance? Will [they have learned enough] to safely operate?" he said.
Dr. Magrina said he had no relevant financial disclosures. Dr. Delmore teaches robotic surgery as a proctor for Intuitive Surgical. Dr. Pasic is a speaker for Ethicon Endo-Surgery.