User login
In older, frailer patients, limb revascularization appeared to preserve both limbs and ambulation longer ? and cost less ? than either amputation or a program of local wound care. Although these patients had worse clinical outcomes than did healthy patients who had revascularization, the benefits were still evident, Dr. Neal R. Barshes and his colleagues wrote in the January issue of Annals of Vascular Surgery.
"We believe that major amputation should be reserved for patients who develop life-threatening foot infections that cannot be controlled with foot drainage or minor amputations and subsequent palliative wound care," wrote Dr. Barshes of the Michael E. DeBakey Veterans Affairs Medical Center, Houston, and his coauthors.

They conducted a clinical outcomes and cost model that ran 1,000 simulated trials of 1,000 patients each. The parameters were drawn from the landmark MOVIE (Model to Optimize Healthcare Value in Ischemic Extremities) study. The study was modified to simulate a patient population older than 80 years, or who had undergone a prior major amputation of the contralateral lower limb, as these two groups have poorer postop outcomes than the usual population undergoing revascularization for lower limb ischemia. The analysis examined outcomes associated with six procedures:
? Primary amputation.
? Local wound care.
? Surgical revascularization followed if needed by surgical revision.
? Surgical revascularization followed if needed by endovascular revision.
? Initial endo revascularization followed if needed by surgical revision.
? Endo revascularization followed if needed by endovascular revision.
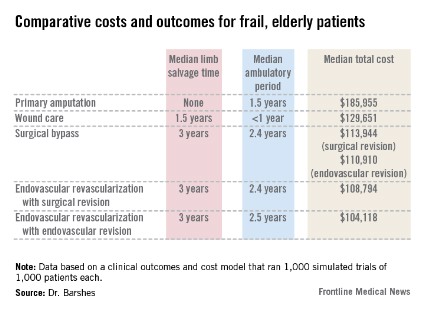
Primary amputation was the least clinically beneficial and the most expensive, with no limb salvage, a median ambulatory period of 1.5 years, and a total 10-year cost of $185,955. Much of the cost was for nursing and long-term care due to loss of independence.
Wound care also produced less desirable outcomes. The median 5-year limb salvage rate was 28%. See costs, salvage period, below.
Surgical bypass with either surgical or endo revision produced a limb salvage rate of 80%. Endo revascularization followed by surgical revision produced a 5-year limb salvage rate of 80%. Endo revascularization with endovascular revision produced a 5-year limb salvage rate of 80.5%, with a median salvage period of 3 years and a median ambulatory period of 2.5 years. This was the least expensive.
These outcomes were worse than those seen in the population of younger, healthier patients. The median 10-year cost for revascularization was up to $35,000 more. Clinical outcomes of the older population were also worse, with a 3-year period of limb preservation compared with more than 4 years in a healthier population, and about 2.5 ambulatory years compared with 4.6 years.
"In spite of these findings, revascularization still appears to be the most cost-effective alternative to wound care and primary amputation," the team noted.
The paper did not note any conflicts.
Dr. Barshes and colleagues suggest that an aggressive approach to limb revascularization, both endovascular and open bypass, may be appropriate and cost effective in older, frailer patients.
Certainly, in today?s era of cost-effective care, it is incumbent upon all of us, as health care providers, to further examine these types of issues. However, the studies necessary are not necessarily easy to perform. We must take into account not only the costs of the actual procedures and hospital stays, which are relatively easy to determine, but also the costs of rehabilitation, outpatient nursing care, wound care, and long-term care for those with loss of functional independence. Even this type of study does not assess all aspects that are important, including how much it is worth to maintain a limb and functional independence per year for each patient. What is not so easy to do is to put a value on limb salvage.
Hopefully we will be able to cull out the factors that may impact upon our decisions to re-intervene for critical limb ischemia, versus offering amputation when the patient presents with inadequate perfusion to the limb after initial attempts at limb salvage.
Dr. Linda Harris is an ACS Fellow and division chief, vascular surgery, State University of New York at Buffalo. She has no disclosures.
Dr. Barshes and colleagues suggest that an aggressive approach to limb revascularization, both endovascular and open bypass, may be appropriate and cost effective in older, frailer patients.
Certainly, in today?s era of cost-effective care, it is incumbent upon all of us, as health care providers, to further examine these types of issues. However, the studies necessary are not necessarily easy to perform. We must take into account not only the costs of the actual procedures and hospital stays, which are relatively easy to determine, but also the costs of rehabilitation, outpatient nursing care, wound care, and long-term care for those with loss of functional independence. Even this type of study does not assess all aspects that are important, including how much it is worth to maintain a limb and functional independence per year for each patient. What is not so easy to do is to put a value on limb salvage.
Hopefully we will be able to cull out the factors that may impact upon our decisions to re-intervene for critical limb ischemia, versus offering amputation when the patient presents with inadequate perfusion to the limb after initial attempts at limb salvage.
Dr. Linda Harris is an ACS Fellow and division chief, vascular surgery, State University of New York at Buffalo. She has no disclosures.
Dr. Barshes and colleagues suggest that an aggressive approach to limb revascularization, both endovascular and open bypass, may be appropriate and cost effective in older, frailer patients.
Certainly, in today?s era of cost-effective care, it is incumbent upon all of us, as health care providers, to further examine these types of issues. However, the studies necessary are not necessarily easy to perform. We must take into account not only the costs of the actual procedures and hospital stays, which are relatively easy to determine, but also the costs of rehabilitation, outpatient nursing care, wound care, and long-term care for those with loss of functional independence. Even this type of study does not assess all aspects that are important, including how much it is worth to maintain a limb and functional independence per year for each patient. What is not so easy to do is to put a value on limb salvage.
Hopefully we will be able to cull out the factors that may impact upon our decisions to re-intervene for critical limb ischemia, versus offering amputation when the patient presents with inadequate perfusion to the limb after initial attempts at limb salvage.
Dr. Linda Harris is an ACS Fellow and division chief, vascular surgery, State University of New York at Buffalo. She has no disclosures.
In older, frailer patients, limb revascularization appeared to preserve both limbs and ambulation longer ? and cost less ? than either amputation or a program of local wound care. Although these patients had worse clinical outcomes than did healthy patients who had revascularization, the benefits were still evident, Dr. Neal R. Barshes and his colleagues wrote in the January issue of Annals of Vascular Surgery.
"We believe that major amputation should be reserved for patients who develop life-threatening foot infections that cannot be controlled with foot drainage or minor amputations and subsequent palliative wound care," wrote Dr. Barshes of the Michael E. DeBakey Veterans Affairs Medical Center, Houston, and his coauthors.

They conducted a clinical outcomes and cost model that ran 1,000 simulated trials of 1,000 patients each. The parameters were drawn from the landmark MOVIE (Model to Optimize Healthcare Value in Ischemic Extremities) study. The study was modified to simulate a patient population older than 80 years, or who had undergone a prior major amputation of the contralateral lower limb, as these two groups have poorer postop outcomes than the usual population undergoing revascularization for lower limb ischemia. The analysis examined outcomes associated with six procedures:
? Primary amputation.
? Local wound care.
? Surgical revascularization followed if needed by surgical revision.
? Surgical revascularization followed if needed by endovascular revision.
? Initial endo revascularization followed if needed by surgical revision.
? Endo revascularization followed if needed by endovascular revision.
Primary amputation was the least clinically beneficial and the most expensive, with no limb salvage, a median ambulatory period of 1.5 years, and a total 10-year cost of $185,955. Much of the cost was for nursing and long-term care due to loss of independence.
Wound care also produced less desirable outcomes. The median 5-year limb salvage rate was 28%. See costs, salvage period, below.
Surgical bypass with either surgical or endo revision produced a limb salvage rate of 80%. Endo revascularization followed by surgical revision produced a 5-year limb salvage rate of 80%. Endo revascularization with endovascular revision produced a 5-year limb salvage rate of 80.5%, with a median salvage period of 3 years and a median ambulatory period of 2.5 years. This was the least expensive.
These outcomes were worse than those seen in the population of younger, healthier patients. The median 10-year cost for revascularization was up to $35,000 more. Clinical outcomes of the older population were also worse, with a 3-year period of limb preservation compared with more than 4 years in a healthier population, and about 2.5 ambulatory years compared with 4.6 years.
"In spite of these findings, revascularization still appears to be the most cost-effective alternative to wound care and primary amputation," the team noted.
The paper did not note any conflicts.
In older, frailer patients, limb revascularization appeared to preserve both limbs and ambulation longer ? and cost less ? than either amputation or a program of local wound care. Although these patients had worse clinical outcomes than did healthy patients who had revascularization, the benefits were still evident, Dr. Neal R. Barshes and his colleagues wrote in the January issue of Annals of Vascular Surgery.
"We believe that major amputation should be reserved for patients who develop life-threatening foot infections that cannot be controlled with foot drainage or minor amputations and subsequent palliative wound care," wrote Dr. Barshes of the Michael E. DeBakey Veterans Affairs Medical Center, Houston, and his coauthors.

They conducted a clinical outcomes and cost model that ran 1,000 simulated trials of 1,000 patients each. The parameters were drawn from the landmark MOVIE (Model to Optimize Healthcare Value in Ischemic Extremities) study. The study was modified to simulate a patient population older than 80 years, or who had undergone a prior major amputation of the contralateral lower limb, as these two groups have poorer postop outcomes than the usual population undergoing revascularization for lower limb ischemia. The analysis examined outcomes associated with six procedures:
? Primary amputation.
? Local wound care.
? Surgical revascularization followed if needed by surgical revision.
? Surgical revascularization followed if needed by endovascular revision.
? Initial endo revascularization followed if needed by surgical revision.
? Endo revascularization followed if needed by endovascular revision.
Primary amputation was the least clinically beneficial and the most expensive, with no limb salvage, a median ambulatory period of 1.5 years, and a total 10-year cost of $185,955. Much of the cost was for nursing and long-term care due to loss of independence.
Wound care also produced less desirable outcomes. The median 5-year limb salvage rate was 28%. See costs, salvage period, below.
Surgical bypass with either surgical or endo revision produced a limb salvage rate of 80%. Endo revascularization followed by surgical revision produced a 5-year limb salvage rate of 80%. Endo revascularization with endovascular revision produced a 5-year limb salvage rate of 80.5%, with a median salvage period of 3 years and a median ambulatory period of 2.5 years. This was the least expensive.
These outcomes were worse than those seen in the population of younger, healthier patients. The median 10-year cost for revascularization was up to $35,000 more. Clinical outcomes of the older population were also worse, with a 3-year period of limb preservation compared with more than 4 years in a healthier population, and about 2.5 ambulatory years compared with 4.6 years.
"In spite of these findings, revascularization still appears to be the most cost-effective alternative to wound care and primary amputation," the team noted.
The paper did not note any conflicts.
Major finding: In older, more frail patients, lower limb revascularization cost up to $90,000 less over 10 years, and yielded better clinical outcomes, than did primary amputation.
Data source: The clinical and cost outcomes model simulated 1,000 trials of 1,000 patients each.
Disclosures: The paper did not note any potential financial conflicts of interest or the study?s sponsor.