User login
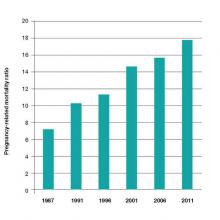
A mother’s untimely death in childbirth is a grave loss that sends shock waves of grief across generations of her family and community. As obstetricians practicing in the United States, we face a terrible problem. We have a continually rising rate of maternal death in a country with exceptional medical resources (FIGURE).1 Our national decentralized approach to dealing with maternal mortality is a factor contributing to the decades-long increase in the maternal mortality ratio. Let’s get organized to better respond to this public health crisis.
Medical education— Let’s get focused on maternal mortality
The 140-page Council on Resident Education in Obstetrics and Gynecology CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology provides a detailed enumeration of the key learning objectives for residents in obstetrics and gynecology.2 Surprisingly, the CREOG objectives do not mention reducing maternal mortality as an important curricular goal. Learning clinical processes and practices that decrease the risk of maternal mortality should be an important educational goal for all residents training in obstetrics and gynecology.
Nationwide action is needed to address the problem
Many countries have organized widespread efforts to reduce maternal mortality. In the United Kingdom and France there are nationwide reviews of maternal deaths with detailed analyses of clinical events and identification of areas for future improvement. These reviews result in the dissemination of countrywide clinical recommendations that change practice and hopefully reduce the risk of future maternal deaths. For example, following the identification of pulmonary embolism as a leading cause of maternal death in the United Kingdom there was a nationwide effort to increase the use of mechanical and pharmacologic prophylaxis to prevent deep venous thrombosis.
In the United States, experts have proposed that a national program of clinical review of severe maternal morbidity cases should be mandatory. (There are many more cases of “near misses” with severe maternal morbidity than there are maternal deaths.) The greater number of cases available for review should help institutions to quickly recognize potential areas for clinical improvement. One group of experts has recommended that all deliveries in which a pregnant woman received 4 or more units of blood or was admitted to an intensive care unit should be thoroughly reviewed to identify opportunities for clinical improvement.3
In the United Kingdom a contemporary clinical problem that is being addressed in an organized and systematic manner is how to respond to the rising rate of severe maternal morbidity caused by placenta accreta. Experts have concluded that women with a suspected placenta accreta should deliver in regional centers with advanced clinical resources—including an emergency surgical response team, interventional radiology, a high capacity blood bank, and an intensive care unit.
A similar approach has been proposed for managing placenta accreta in the United States.4 The American College of Obstetricians and Gynecologists (ACOG) and the Society of Maternal Fetal Medicine (SMFM) have proposed a tiered system of obstetric care with more complex cases being referred to regional perinatal centers.5 Regionalization of trauma services has been an important part of the US health care system for decades. Cases of severe trauma are brought to regional centers equipped to emergently treat complex injuries. A similar system of regulation and regionalization could be adapted for optimizing maternity care.
High-risk clinical events: Is your unit prepared?
In the United States the leading causes of maternal mortality, in descending order, are6−8:
- cardiovascular diseases
- infection
- hemorrhage
- cardiomyopathy
- pulmonary embolism
- hypertension
- amniotic fluid embolism
- stroke
- anesthesia complications.
Over the last decade, the Joint Commission has recommended that birthing centers develop standardized protocols and use simulation to improve the institution’s ability to respond in a timely manner to clinical events that may result in maternal morbidity or death.
The quality of published protocols dealing with hemorrhage, hypertension, and thromboembolism is continuously improving, and every birthing center should have written protocols that are updated on a regular timetable for these common high-risk events.9,10 Does your birthing unit have written protocols to deal with cardiac diseases, infection, obstetric hemorrhage, thromboembolism, and severe hypertension? Are simulation exercises used to strengthen familiarity with the protocols?
High-risk patients
An amazing fact of today’s medical care is that sexually active women of reproductive age who have high-risk medical problems often have not been counseled to use a highly effective contraceptive, resulting in an increased risk of unintended pregnancy and maternal death. For example, adult women with a history of congenital heart disease are known to be at increased risk of death if they become pregnant. In a recent study, women with a history of congenital heart disease had 178 maternal deaths per 100,000 deliveries—a rate approximately 10-fold higher than the US maternal mortality ratio.11 Yet, many of these women are not using a highly effective contraceptive, and this results in a high rate of unplanned pregnancy.12
In order to reduce the risk of unintended pregnancy in women with high-risk medical problems, health systems could make contraception an important “vital sign” for women with high-risk medical conditions.
Race and age matter greatly when it comes to maternal mortality risk
There are major racial differences in pregnancy-related mortality, with black women having much higher rates than white women. In the United States in 2011, the pregnancy-related mortality ratio for white, black, and women of other races was 12.5, 42.8, and 17.3 deaths per 100,000 live births, respectively. This represents a major racial disparity in pregnancy outcomes.1
The age of the mother is an important determinant of the risk of maternal death. Women younger than age 35 years have the lowest risk of maternal death. From 2006 to 2010, pregnant women older than age 40 had a risk of death approximately 3 times greater than women aged 34 or younger.2
References
- Pregnancy Mortality Surveillance System. Centers for Disease Control and Prevention Web site. http://www .cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html. Accessed August 20, 2015.
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol. 2015;125(1):5−12.
Let’s get organized
In a country with a history of embracing the “live free or die” ethic, it is often difficult for physicians to enthusiastically embrace the need for a higher level of organization and a potential reduction in individual freedom in order to improve health outcomes. And with a US maternal mortality ratio of 1 maternal death for every 5,400 births, many obstetricians will never have one of their patients die in childbirth. In fact, most obstetricians will have only 1 maternal death during their entire career. In this reality, when clinical events occur rarely, it is not possible for any single clinician, working alone, to impact the overall outcomes of those rare events. Therefore, teamwork and national efforts, such as the National Partnership for Maternal Safety,13 will be necessary to reverse our alarming trend of increasing maternal mortality. Let’s get organized to stop the rise of maternal deaths in the United States.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Chescheir NC. Enough already! Obstet Gynecol. 2015;125(1):2−4.
- Council on Resident Education in Obstetrics and Gynecology (CREOG) Educational Objectives: Core Curriculum in Obstetrics and Gynecology. 10th ed. Washington, DC: American College of Obstetricians and Gynecologists; 2013:140.
- Callaghan WM, Grobman WA, Kilpatrick SJ, Main EK, D’Alton M. Facility-based identification of women with severe maternal morbidity: it is time to start. Obstet Gynecol. 2014;123(5):978−981.
- Silver RM, Fox KA, Barton JR, et al. Center of excellence for placenta accreta. Am J Obstet Gynecol. 2015;212(5):561−568.
- American College of Obstetricians and Gynecologists and the Society of Maternal Fetal Medicine. Obstetric care consensus No 2: levels of maternal care. Obstet Gynecol. 2015;125(2):502−515.
- Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998−2005. Obstet Gynecol. 2010;116(6):1302−1309.
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006−2010. Obstet Gynecol. 2015;125(1):5−12.
- Pregnancy Mortality Surveillance System. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html. Accessed August 20, 2015.
- Shields LE, Wiesner S, Fulton J, Pelletreau B. Comprehensive maternal hemorrhage protocols reduce the use of blood products and improve patient safety. Am J Obstet Gynecol. 2015;212(3):272−280.
- James A. Committee on Practice Bulletins—Obstetrics. Practice bulletin No. 123: thromboembolism in pregnancy. ACOG. Obstet Gynecol. 2011;118(3):718−729.
- Thompson JL, Kuklina EV, Bateman BT, Callaghan WM, James AH, Grotegut CA. Medical and obstetrical outcomes among pregnant women with congenital heart disease. Obstet Gynecol. 2015;126(2):346−354.
- Lindley KJ, Madden T, Cahill AG, Ludbrook PA, Billadello JJ. Contraceptive use and unintended pregnancy in women with congenital heart disease. Obstet Gynecol. 2015;126(2):363−369.
- D’Alton ME, Main EK, Menard MK, Levy BS. The National Partnership for Maternal Safety. Obstet Gynecol. 2014;123(5):973−977.
A mother’s untimely death in childbirth is a grave loss that sends shock waves of grief across generations of her family and community. As obstetricians practicing in the United States, we face a terrible problem. We have a continually rising rate of maternal death in a country with exceptional medical resources (FIGURE).1 Our national decentralized approach to dealing with maternal mortality is a factor contributing to the decades-long increase in the maternal mortality ratio. Let’s get organized to better respond to this public health crisis.
Medical education— Let’s get focused on maternal mortality
The 140-page Council on Resident Education in Obstetrics and Gynecology CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology provides a detailed enumeration of the key learning objectives for residents in obstetrics and gynecology.2 Surprisingly, the CREOG objectives do not mention reducing maternal mortality as an important curricular goal. Learning clinical processes and practices that decrease the risk of maternal mortality should be an important educational goal for all residents training in obstetrics and gynecology.
Nationwide action is needed to address the problem
Many countries have organized widespread efforts to reduce maternal mortality. In the United Kingdom and France there are nationwide reviews of maternal deaths with detailed analyses of clinical events and identification of areas for future improvement. These reviews result in the dissemination of countrywide clinical recommendations that change practice and hopefully reduce the risk of future maternal deaths. For example, following the identification of pulmonary embolism as a leading cause of maternal death in the United Kingdom there was a nationwide effort to increase the use of mechanical and pharmacologic prophylaxis to prevent deep venous thrombosis.
In the United States, experts have proposed that a national program of clinical review of severe maternal morbidity cases should be mandatory. (There are many more cases of “near misses” with severe maternal morbidity than there are maternal deaths.) The greater number of cases available for review should help institutions to quickly recognize potential areas for clinical improvement. One group of experts has recommended that all deliveries in which a pregnant woman received 4 or more units of blood or was admitted to an intensive care unit should be thoroughly reviewed to identify opportunities for clinical improvement.3
In the United Kingdom a contemporary clinical problem that is being addressed in an organized and systematic manner is how to respond to the rising rate of severe maternal morbidity caused by placenta accreta. Experts have concluded that women with a suspected placenta accreta should deliver in regional centers with advanced clinical resources—including an emergency surgical response team, interventional radiology, a high capacity blood bank, and an intensive care unit.
A similar approach has been proposed for managing placenta accreta in the United States.4 The American College of Obstetricians and Gynecologists (ACOG) and the Society of Maternal Fetal Medicine (SMFM) have proposed a tiered system of obstetric care with more complex cases being referred to regional perinatal centers.5 Regionalization of trauma services has been an important part of the US health care system for decades. Cases of severe trauma are brought to regional centers equipped to emergently treat complex injuries. A similar system of regulation and regionalization could be adapted for optimizing maternity care.
High-risk clinical events: Is your unit prepared?
In the United States the leading causes of maternal mortality, in descending order, are6−8:
- cardiovascular diseases
- infection
- hemorrhage
- cardiomyopathy
- pulmonary embolism
- hypertension
- amniotic fluid embolism
- stroke
- anesthesia complications.
Over the last decade, the Joint Commission has recommended that birthing centers develop standardized protocols and use simulation to improve the institution’s ability to respond in a timely manner to clinical events that may result in maternal morbidity or death.
The quality of published protocols dealing with hemorrhage, hypertension, and thromboembolism is continuously improving, and every birthing center should have written protocols that are updated on a regular timetable for these common high-risk events.9,10 Does your birthing unit have written protocols to deal with cardiac diseases, infection, obstetric hemorrhage, thromboembolism, and severe hypertension? Are simulation exercises used to strengthen familiarity with the protocols?
High-risk patients
An amazing fact of today’s medical care is that sexually active women of reproductive age who have high-risk medical problems often have not been counseled to use a highly effective contraceptive, resulting in an increased risk of unintended pregnancy and maternal death. For example, adult women with a history of congenital heart disease are known to be at increased risk of death if they become pregnant. In a recent study, women with a history of congenital heart disease had 178 maternal deaths per 100,000 deliveries—a rate approximately 10-fold higher than the US maternal mortality ratio.11 Yet, many of these women are not using a highly effective contraceptive, and this results in a high rate of unplanned pregnancy.12
In order to reduce the risk of unintended pregnancy in women with high-risk medical problems, health systems could make contraception an important “vital sign” for women with high-risk medical conditions.
Race and age matter greatly when it comes to maternal mortality risk
There are major racial differences in pregnancy-related mortality, with black women having much higher rates than white women. In the United States in 2011, the pregnancy-related mortality ratio for white, black, and women of other races was 12.5, 42.8, and 17.3 deaths per 100,000 live births, respectively. This represents a major racial disparity in pregnancy outcomes.1
The age of the mother is an important determinant of the risk of maternal death. Women younger than age 35 years have the lowest risk of maternal death. From 2006 to 2010, pregnant women older than age 40 had a risk of death approximately 3 times greater than women aged 34 or younger.2
References
- Pregnancy Mortality Surveillance System. Centers for Disease Control and Prevention Web site. http://www .cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html. Accessed August 20, 2015.
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol. 2015;125(1):5−12.
Let’s get organized
In a country with a history of embracing the “live free or die” ethic, it is often difficult for physicians to enthusiastically embrace the need for a higher level of organization and a potential reduction in individual freedom in order to improve health outcomes. And with a US maternal mortality ratio of 1 maternal death for every 5,400 births, many obstetricians will never have one of their patients die in childbirth. In fact, most obstetricians will have only 1 maternal death during their entire career. In this reality, when clinical events occur rarely, it is not possible for any single clinician, working alone, to impact the overall outcomes of those rare events. Therefore, teamwork and national efforts, such as the National Partnership for Maternal Safety,13 will be necessary to reverse our alarming trend of increasing maternal mortality. Let’s get organized to stop the rise of maternal deaths in the United States.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
A mother’s untimely death in childbirth is a grave loss that sends shock waves of grief across generations of her family and community. As obstetricians practicing in the United States, we face a terrible problem. We have a continually rising rate of maternal death in a country with exceptional medical resources (FIGURE).1 Our national decentralized approach to dealing with maternal mortality is a factor contributing to the decades-long increase in the maternal mortality ratio. Let’s get organized to better respond to this public health crisis.
Medical education— Let’s get focused on maternal mortality
The 140-page Council on Resident Education in Obstetrics and Gynecology CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology provides a detailed enumeration of the key learning objectives for residents in obstetrics and gynecology.2 Surprisingly, the CREOG objectives do not mention reducing maternal mortality as an important curricular goal. Learning clinical processes and practices that decrease the risk of maternal mortality should be an important educational goal for all residents training in obstetrics and gynecology.
Nationwide action is needed to address the problem
Many countries have organized widespread efforts to reduce maternal mortality. In the United Kingdom and France there are nationwide reviews of maternal deaths with detailed analyses of clinical events and identification of areas for future improvement. These reviews result in the dissemination of countrywide clinical recommendations that change practice and hopefully reduce the risk of future maternal deaths. For example, following the identification of pulmonary embolism as a leading cause of maternal death in the United Kingdom there was a nationwide effort to increase the use of mechanical and pharmacologic prophylaxis to prevent deep venous thrombosis.
In the United States, experts have proposed that a national program of clinical review of severe maternal morbidity cases should be mandatory. (There are many more cases of “near misses” with severe maternal morbidity than there are maternal deaths.) The greater number of cases available for review should help institutions to quickly recognize potential areas for clinical improvement. One group of experts has recommended that all deliveries in which a pregnant woman received 4 or more units of blood or was admitted to an intensive care unit should be thoroughly reviewed to identify opportunities for clinical improvement.3
In the United Kingdom a contemporary clinical problem that is being addressed in an organized and systematic manner is how to respond to the rising rate of severe maternal morbidity caused by placenta accreta. Experts have concluded that women with a suspected placenta accreta should deliver in regional centers with advanced clinical resources—including an emergency surgical response team, interventional radiology, a high capacity blood bank, and an intensive care unit.
A similar approach has been proposed for managing placenta accreta in the United States.4 The American College of Obstetricians and Gynecologists (ACOG) and the Society of Maternal Fetal Medicine (SMFM) have proposed a tiered system of obstetric care with more complex cases being referred to regional perinatal centers.5 Regionalization of trauma services has been an important part of the US health care system for decades. Cases of severe trauma are brought to regional centers equipped to emergently treat complex injuries. A similar system of regulation and regionalization could be adapted for optimizing maternity care.
High-risk clinical events: Is your unit prepared?
In the United States the leading causes of maternal mortality, in descending order, are6−8:
- cardiovascular diseases
- infection
- hemorrhage
- cardiomyopathy
- pulmonary embolism
- hypertension
- amniotic fluid embolism
- stroke
- anesthesia complications.
Over the last decade, the Joint Commission has recommended that birthing centers develop standardized protocols and use simulation to improve the institution’s ability to respond in a timely manner to clinical events that may result in maternal morbidity or death.
The quality of published protocols dealing with hemorrhage, hypertension, and thromboembolism is continuously improving, and every birthing center should have written protocols that are updated on a regular timetable for these common high-risk events.9,10 Does your birthing unit have written protocols to deal with cardiac diseases, infection, obstetric hemorrhage, thromboembolism, and severe hypertension? Are simulation exercises used to strengthen familiarity with the protocols?
High-risk patients
An amazing fact of today’s medical care is that sexually active women of reproductive age who have high-risk medical problems often have not been counseled to use a highly effective contraceptive, resulting in an increased risk of unintended pregnancy and maternal death. For example, adult women with a history of congenital heart disease are known to be at increased risk of death if they become pregnant. In a recent study, women with a history of congenital heart disease had 178 maternal deaths per 100,000 deliveries—a rate approximately 10-fold higher than the US maternal mortality ratio.11 Yet, many of these women are not using a highly effective contraceptive, and this results in a high rate of unplanned pregnancy.12
In order to reduce the risk of unintended pregnancy in women with high-risk medical problems, health systems could make contraception an important “vital sign” for women with high-risk medical conditions.
Race and age matter greatly when it comes to maternal mortality risk
There are major racial differences in pregnancy-related mortality, with black women having much higher rates than white women. In the United States in 2011, the pregnancy-related mortality ratio for white, black, and women of other races was 12.5, 42.8, and 17.3 deaths per 100,000 live births, respectively. This represents a major racial disparity in pregnancy outcomes.1
The age of the mother is an important determinant of the risk of maternal death. Women younger than age 35 years have the lowest risk of maternal death. From 2006 to 2010, pregnant women older than age 40 had a risk of death approximately 3 times greater than women aged 34 or younger.2
References
- Pregnancy Mortality Surveillance System. Centers for Disease Control and Prevention Web site. http://www .cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html. Accessed August 20, 2015.
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol. 2015;125(1):5−12.
Let’s get organized
In a country with a history of embracing the “live free or die” ethic, it is often difficult for physicians to enthusiastically embrace the need for a higher level of organization and a potential reduction in individual freedom in order to improve health outcomes. And with a US maternal mortality ratio of 1 maternal death for every 5,400 births, many obstetricians will never have one of their patients die in childbirth. In fact, most obstetricians will have only 1 maternal death during their entire career. In this reality, when clinical events occur rarely, it is not possible for any single clinician, working alone, to impact the overall outcomes of those rare events. Therefore, teamwork and national efforts, such as the National Partnership for Maternal Safety,13 will be necessary to reverse our alarming trend of increasing maternal mortality. Let’s get organized to stop the rise of maternal deaths in the United States.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Chescheir NC. Enough already! Obstet Gynecol. 2015;125(1):2−4.
- Council on Resident Education in Obstetrics and Gynecology (CREOG) Educational Objectives: Core Curriculum in Obstetrics and Gynecology. 10th ed. Washington, DC: American College of Obstetricians and Gynecologists; 2013:140.
- Callaghan WM, Grobman WA, Kilpatrick SJ, Main EK, D’Alton M. Facility-based identification of women with severe maternal morbidity: it is time to start. Obstet Gynecol. 2014;123(5):978−981.
- Silver RM, Fox KA, Barton JR, et al. Center of excellence for placenta accreta. Am J Obstet Gynecol. 2015;212(5):561−568.
- American College of Obstetricians and Gynecologists and the Society of Maternal Fetal Medicine. Obstetric care consensus No 2: levels of maternal care. Obstet Gynecol. 2015;125(2):502−515.
- Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998−2005. Obstet Gynecol. 2010;116(6):1302−1309.
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006−2010. Obstet Gynecol. 2015;125(1):5−12.
- Pregnancy Mortality Surveillance System. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html. Accessed August 20, 2015.
- Shields LE, Wiesner S, Fulton J, Pelletreau B. Comprehensive maternal hemorrhage protocols reduce the use of blood products and improve patient safety. Am J Obstet Gynecol. 2015;212(3):272−280.
- James A. Committee on Practice Bulletins—Obstetrics. Practice bulletin No. 123: thromboembolism in pregnancy. ACOG. Obstet Gynecol. 2011;118(3):718−729.
- Thompson JL, Kuklina EV, Bateman BT, Callaghan WM, James AH, Grotegut CA. Medical and obstetrical outcomes among pregnant women with congenital heart disease. Obstet Gynecol. 2015;126(2):346−354.
- Lindley KJ, Madden T, Cahill AG, Ludbrook PA, Billadello JJ. Contraceptive use and unintended pregnancy in women with congenital heart disease. Obstet Gynecol. 2015;126(2):363−369.
- D’Alton ME, Main EK, Menard MK, Levy BS. The National Partnership for Maternal Safety. Obstet Gynecol. 2014;123(5):973−977.
- Chescheir NC. Enough already! Obstet Gynecol. 2015;125(1):2−4.
- Council on Resident Education in Obstetrics and Gynecology (CREOG) Educational Objectives: Core Curriculum in Obstetrics and Gynecology. 10th ed. Washington, DC: American College of Obstetricians and Gynecologists; 2013:140.
- Callaghan WM, Grobman WA, Kilpatrick SJ, Main EK, D’Alton M. Facility-based identification of women with severe maternal morbidity: it is time to start. Obstet Gynecol. 2014;123(5):978−981.
- Silver RM, Fox KA, Barton JR, et al. Center of excellence for placenta accreta. Am J Obstet Gynecol. 2015;212(5):561−568.
- American College of Obstetricians and Gynecologists and the Society of Maternal Fetal Medicine. Obstetric care consensus No 2: levels of maternal care. Obstet Gynecol. 2015;125(2):502−515.
- Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998−2005. Obstet Gynecol. 2010;116(6):1302−1309.
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006−2010. Obstet Gynecol. 2015;125(1):5−12.
- Pregnancy Mortality Surveillance System. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html. Accessed August 20, 2015.
- Shields LE, Wiesner S, Fulton J, Pelletreau B. Comprehensive maternal hemorrhage protocols reduce the use of blood products and improve patient safety. Am J Obstet Gynecol. 2015;212(3):272−280.
- James A. Committee on Practice Bulletins—Obstetrics. Practice bulletin No. 123: thromboembolism in pregnancy. ACOG. Obstet Gynecol. 2011;118(3):718−729.
- Thompson JL, Kuklina EV, Bateman BT, Callaghan WM, James AH, Grotegut CA. Medical and obstetrical outcomes among pregnant women with congenital heart disease. Obstet Gynecol. 2015;126(2):346−354.
- Lindley KJ, Madden T, Cahill AG, Ludbrook PA, Billadello JJ. Contraceptive use and unintended pregnancy in women with congenital heart disease. Obstet Gynecol. 2015;126(2):363−369.
- D’Alton ME, Main EK, Menard MK, Levy BS. The National Partnership for Maternal Safety. Obstet Gynecol. 2014;123(5):973−977.