User login
A 28-year-old man came to the office with a rash on his face. He reported he has had this rash on and off for 3 years. The rash sometimes itches around his moustache, and it gets worse with stress—he has been under increasing stress for the past 2 months. He is in good health and does not have any other symptoms, and he denies any risk factors for human immunodeficiency virus (HIV).
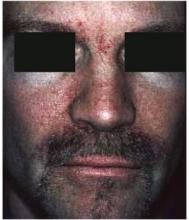
Physical examination reveals erythema and scale across his eyebrows, cheeks, and near his moustache. On close inspection, the scale is visible under his moustache and eyebrows as well.
FIGURE 1
Erythema on the face
FIGURE 2
Close-up of erythema
What is the diagnosis?
What are the management options?
DIAGNOSIS
This young man has seborrhea (seborrheic dermatitis), a superficial inflammatory dermatitis. It is a common condition characterized by patches of erythema and scaling, usually on the scalp (ie, dandruff), eyebrows, nasolabial creases, forehead, cheeks, around the nose, behind the ears, and under facial hair. Seborrhea can also occur over the sternum and in the axillae, submammary folds, umbilicus, groin, and gluteal creases. These areas are regions with a greater number of pilosebaceous units, which produce sebum.
Seborrhea is thought to be caused by an inflammatory hypersensitivity to epidermal, bacterial, or yeast antigens. Persons with seborrhea have a profusion of Pityrosporum yeast on the skin. This yeast can be a normal part of skin flora; seborrhea is an inflammatory reaction to its presence. Seborrhea is characterized by remissions and exacerbations. The most common precipitating factors are stress, immuno suppression, and cold weather. The treatment of seborrhea should be directed at the inflammation and the Pityrosporum.
Epidemiology
Seborrhea is most commonly seen in patients aged 20 and 50 years, and mostly in males. The prevalence of seborrhea is approximately 3% to 5% in young adults who are HIV-negative. The prevalence of seborrhea is as high as 36% in HIV-positive persons, although the vast majority of persons with seborrhea have a normal immune system. No lab tests are required to make the diagnosis.
Treatment: antifungals and topical steroids
Treat seborrhea with a 2-pronged plan: antifungal agents for the yeast and topical corticosteroids for the inflammation. The antifungals can also be used to prevent exacerbations; steroids should only be applied to active areas of inflammation.
Fortunately, seborrhea on the face responds well to low-potency topical corticosteroids, such as 1% hydrocortisone cream or lotion. Still, corticosteroids should not be used on the face for prolonged periods to avoid skin atrophy and other side effects. The lotion is better for hair-covered areas as it is less messy to apply than a cream.
Antifungal shampoos
Over-the-counter dandruff shampoos have been the mainstay of therapy for seborrhea of the scalp. These products often contain selenium (ie, Selsun Blue) or zinc (ie, Head and Shoulders), both of which are toxic to Pityrosporum. Often patients have both seborrhea on the scalp and the face, and using these shampoos can cut down the amount of Pityrosporumon both. Instruct patients with facial hair to lather their beards and moustache with shampoo as well.
Both ketoconazole (Nizoral) 2% shampoo and selenium sulfide 2.5% shampoo are effective in the treatment of moderate to severe dandruff (level of evidence [LOE]: 1b).1 Ketoconazole 2% shampoo is highly effective not only for clearing seborrheic dermatitis on the scalp but also for preventing relapse when used prophylactically once weekly (LOE: 1b).2 Ketoconazole has become available in a 1% over-the-counter dandruff shampoo, but the 2% shampoo still requires a prescription.
Treating severe cases
When seborrhea of the scalp becomes more severe, add a higher-potency steroid solution or lotion to the treatment until the exacerbation is under control. Ketoconazole cream is also a good treatment for seborrheic dermatitis in areas other than the scalp. Other antifungal creams such as miconazole can be used to treat seborrhea of the face.
One trial demonstrated the effectiveness of topical 1% metronidazole gel in seborrheic dermatitis (LOE: 1b). At the 8-week follow-up, 14 patients in the metronidazole group showed a marked to complete improvement compared with 2 in the placebo group (P<.001; number needed to treat=2).3 This is not an approved indication for metronidazole gel, but it may be considered when other topical medications fail. In a randomized controlled trial using crossover design, treatment with a low-dose homeopathic preparation provided significant improvement in seborrheic dermatitis and dandruff after 10 weeks of dosing (LOE: 2b).4
Most seborrheic dermatitis is fully treatable with topical agents. When topical medications are not providing adequate results, oral antifungal agents may be considered. In 1 study, oral terbinafine was found to be effective in the treatment of moderate to severe seborrheic dermatitis. Clinical improvement following 4 weeks treatment with terbinafine was maintained 8 weeks after completing treatment (LOE: 1b).5
Conclusion of visit
The patient was given a prescription for 1% hydrocortisone lotion and 2% ketoconazole cream, both to be applied twice daily to the affected areas. He also planned to investigate the homeopathy option for the future. It was explained to the patient that these treatments may not be curative, and seborrhea may come back when he is under stress.
1. Danby FW, Maddin WS, Margesson LJ, Rosenthal D. A randomized, double-blind, placebo-controlled trial of ketoconazole 2% shampoo versus selenium sulfide 2.5% shampoo in the treatment of moderate to severe dandruff. J Am Acad Dermatol 1993;29:1008-1012.
2. Peter RU, Richarz-Barthauer U. Successful treatment and prophylaxis of scalp seborrhoeic dermatitis and dandruff with 2% ketoconazole shampoo: results of a multicentre, double-blind, placebo-controlled trial. Br J Dermatol 1995;132:441-445.
3. Parsad D, Pandhi R, Negi KS, Kumar B. Topical metronidazole in seborrheic dermatitis—a double-blind study. Dermatology 2001;202:35-37.
4. Smith SA, Baker AE, Williams JH. Effective treatment of seborrheic dermatitis using a low dose, oral homeopathic medication consisting of potassium bromide, sodium bromide, nickel sulfate, and sodium chloride in a double-blind, placebo-controlled study. Altern Med Rev 2002;7:59-67.
5. Scaparro E, Quadri G, Virno G, Orifici C, Milani M. Evaluation of the efficacy and tolerability of oral terbinafine (Daskil) in patients with seborrhoeic dermatitis. A multicentre, randomized, investigator-blinded, placebo-controlled trial. Br J Dermatol 2001;144:854-857.
A 28-year-old man came to the office with a rash on his face. He reported he has had this rash on and off for 3 years. The rash sometimes itches around his moustache, and it gets worse with stress—he has been under increasing stress for the past 2 months. He is in good health and does not have any other symptoms, and he denies any risk factors for human immunodeficiency virus (HIV).
Physical examination reveals erythema and scale across his eyebrows, cheeks, and near his moustache. On close inspection, the scale is visible under his moustache and eyebrows as well.
FIGURE 1
Erythema on the face
FIGURE 2
Close-up of erythema
What is the diagnosis?
What are the management options?
DIAGNOSIS
This young man has seborrhea (seborrheic dermatitis), a superficial inflammatory dermatitis. It is a common condition characterized by patches of erythema and scaling, usually on the scalp (ie, dandruff), eyebrows, nasolabial creases, forehead, cheeks, around the nose, behind the ears, and under facial hair. Seborrhea can also occur over the sternum and in the axillae, submammary folds, umbilicus, groin, and gluteal creases. These areas are regions with a greater number of pilosebaceous units, which produce sebum.
Seborrhea is thought to be caused by an inflammatory hypersensitivity to epidermal, bacterial, or yeast antigens. Persons with seborrhea have a profusion of Pityrosporum yeast on the skin. This yeast can be a normal part of skin flora; seborrhea is an inflammatory reaction to its presence. Seborrhea is characterized by remissions and exacerbations. The most common precipitating factors are stress, immuno suppression, and cold weather. The treatment of seborrhea should be directed at the inflammation and the Pityrosporum.
Epidemiology
Seborrhea is most commonly seen in patients aged 20 and 50 years, and mostly in males. The prevalence of seborrhea is approximately 3% to 5% in young adults who are HIV-negative. The prevalence of seborrhea is as high as 36% in HIV-positive persons, although the vast majority of persons with seborrhea have a normal immune system. No lab tests are required to make the diagnosis.
Treatment: antifungals and topical steroids
Treat seborrhea with a 2-pronged plan: antifungal agents for the yeast and topical corticosteroids for the inflammation. The antifungals can also be used to prevent exacerbations; steroids should only be applied to active areas of inflammation.
Fortunately, seborrhea on the face responds well to low-potency topical corticosteroids, such as 1% hydrocortisone cream or lotion. Still, corticosteroids should not be used on the face for prolonged periods to avoid skin atrophy and other side effects. The lotion is better for hair-covered areas as it is less messy to apply than a cream.
Antifungal shampoos
Over-the-counter dandruff shampoos have been the mainstay of therapy for seborrhea of the scalp. These products often contain selenium (ie, Selsun Blue) or zinc (ie, Head and Shoulders), both of which are toxic to Pityrosporum. Often patients have both seborrhea on the scalp and the face, and using these shampoos can cut down the amount of Pityrosporumon both. Instruct patients with facial hair to lather their beards and moustache with shampoo as well.
Both ketoconazole (Nizoral) 2% shampoo and selenium sulfide 2.5% shampoo are effective in the treatment of moderate to severe dandruff (level of evidence [LOE]: 1b).1 Ketoconazole 2% shampoo is highly effective not only for clearing seborrheic dermatitis on the scalp but also for preventing relapse when used prophylactically once weekly (LOE: 1b).2 Ketoconazole has become available in a 1% over-the-counter dandruff shampoo, but the 2% shampoo still requires a prescription.
Treating severe cases
When seborrhea of the scalp becomes more severe, add a higher-potency steroid solution or lotion to the treatment until the exacerbation is under control. Ketoconazole cream is also a good treatment for seborrheic dermatitis in areas other than the scalp. Other antifungal creams such as miconazole can be used to treat seborrhea of the face.
One trial demonstrated the effectiveness of topical 1% metronidazole gel in seborrheic dermatitis (LOE: 1b). At the 8-week follow-up, 14 patients in the metronidazole group showed a marked to complete improvement compared with 2 in the placebo group (P<.001; number needed to treat=2).3 This is not an approved indication for metronidazole gel, but it may be considered when other topical medications fail. In a randomized controlled trial using crossover design, treatment with a low-dose homeopathic preparation provided significant improvement in seborrheic dermatitis and dandruff after 10 weeks of dosing (LOE: 2b).4
Most seborrheic dermatitis is fully treatable with topical agents. When topical medications are not providing adequate results, oral antifungal agents may be considered. In 1 study, oral terbinafine was found to be effective in the treatment of moderate to severe seborrheic dermatitis. Clinical improvement following 4 weeks treatment with terbinafine was maintained 8 weeks after completing treatment (LOE: 1b).5
Conclusion of visit
The patient was given a prescription for 1% hydrocortisone lotion and 2% ketoconazole cream, both to be applied twice daily to the affected areas. He also planned to investigate the homeopathy option for the future. It was explained to the patient that these treatments may not be curative, and seborrhea may come back when he is under stress.
A 28-year-old man came to the office with a rash on his face. He reported he has had this rash on and off for 3 years. The rash sometimes itches around his moustache, and it gets worse with stress—he has been under increasing stress for the past 2 months. He is in good health and does not have any other symptoms, and he denies any risk factors for human immunodeficiency virus (HIV).
Physical examination reveals erythema and scale across his eyebrows, cheeks, and near his moustache. On close inspection, the scale is visible under his moustache and eyebrows as well.
FIGURE 1
Erythema on the face
FIGURE 2
Close-up of erythema
What is the diagnosis?
What are the management options?
DIAGNOSIS
This young man has seborrhea (seborrheic dermatitis), a superficial inflammatory dermatitis. It is a common condition characterized by patches of erythema and scaling, usually on the scalp (ie, dandruff), eyebrows, nasolabial creases, forehead, cheeks, around the nose, behind the ears, and under facial hair. Seborrhea can also occur over the sternum and in the axillae, submammary folds, umbilicus, groin, and gluteal creases. These areas are regions with a greater number of pilosebaceous units, which produce sebum.
Seborrhea is thought to be caused by an inflammatory hypersensitivity to epidermal, bacterial, or yeast antigens. Persons with seborrhea have a profusion of Pityrosporum yeast on the skin. This yeast can be a normal part of skin flora; seborrhea is an inflammatory reaction to its presence. Seborrhea is characterized by remissions and exacerbations. The most common precipitating factors are stress, immuno suppression, and cold weather. The treatment of seborrhea should be directed at the inflammation and the Pityrosporum.
Epidemiology
Seborrhea is most commonly seen in patients aged 20 and 50 years, and mostly in males. The prevalence of seborrhea is approximately 3% to 5% in young adults who are HIV-negative. The prevalence of seborrhea is as high as 36% in HIV-positive persons, although the vast majority of persons with seborrhea have a normal immune system. No lab tests are required to make the diagnosis.
Treatment: antifungals and topical steroids
Treat seborrhea with a 2-pronged plan: antifungal agents for the yeast and topical corticosteroids for the inflammation. The antifungals can also be used to prevent exacerbations; steroids should only be applied to active areas of inflammation.
Fortunately, seborrhea on the face responds well to low-potency topical corticosteroids, such as 1% hydrocortisone cream or lotion. Still, corticosteroids should not be used on the face for prolonged periods to avoid skin atrophy and other side effects. The lotion is better for hair-covered areas as it is less messy to apply than a cream.
Antifungal shampoos
Over-the-counter dandruff shampoos have been the mainstay of therapy for seborrhea of the scalp. These products often contain selenium (ie, Selsun Blue) or zinc (ie, Head and Shoulders), both of which are toxic to Pityrosporum. Often patients have both seborrhea on the scalp and the face, and using these shampoos can cut down the amount of Pityrosporumon both. Instruct patients with facial hair to lather their beards and moustache with shampoo as well.
Both ketoconazole (Nizoral) 2% shampoo and selenium sulfide 2.5% shampoo are effective in the treatment of moderate to severe dandruff (level of evidence [LOE]: 1b).1 Ketoconazole 2% shampoo is highly effective not only for clearing seborrheic dermatitis on the scalp but also for preventing relapse when used prophylactically once weekly (LOE: 1b).2 Ketoconazole has become available in a 1% over-the-counter dandruff shampoo, but the 2% shampoo still requires a prescription.
Treating severe cases
When seborrhea of the scalp becomes more severe, add a higher-potency steroid solution or lotion to the treatment until the exacerbation is under control. Ketoconazole cream is also a good treatment for seborrheic dermatitis in areas other than the scalp. Other antifungal creams such as miconazole can be used to treat seborrhea of the face.
One trial demonstrated the effectiveness of topical 1% metronidazole gel in seborrheic dermatitis (LOE: 1b). At the 8-week follow-up, 14 patients in the metronidazole group showed a marked to complete improvement compared with 2 in the placebo group (P<.001; number needed to treat=2).3 This is not an approved indication for metronidazole gel, but it may be considered when other topical medications fail. In a randomized controlled trial using crossover design, treatment with a low-dose homeopathic preparation provided significant improvement in seborrheic dermatitis and dandruff after 10 weeks of dosing (LOE: 2b).4
Most seborrheic dermatitis is fully treatable with topical agents. When topical medications are not providing adequate results, oral antifungal agents may be considered. In 1 study, oral terbinafine was found to be effective in the treatment of moderate to severe seborrheic dermatitis. Clinical improvement following 4 weeks treatment with terbinafine was maintained 8 weeks after completing treatment (LOE: 1b).5
Conclusion of visit
The patient was given a prescription for 1% hydrocortisone lotion and 2% ketoconazole cream, both to be applied twice daily to the affected areas. He also planned to investigate the homeopathy option for the future. It was explained to the patient that these treatments may not be curative, and seborrhea may come back when he is under stress.
1. Danby FW, Maddin WS, Margesson LJ, Rosenthal D. A randomized, double-blind, placebo-controlled trial of ketoconazole 2% shampoo versus selenium sulfide 2.5% shampoo in the treatment of moderate to severe dandruff. J Am Acad Dermatol 1993;29:1008-1012.
2. Peter RU, Richarz-Barthauer U. Successful treatment and prophylaxis of scalp seborrhoeic dermatitis and dandruff with 2% ketoconazole shampoo: results of a multicentre, double-blind, placebo-controlled trial. Br J Dermatol 1995;132:441-445.
3. Parsad D, Pandhi R, Negi KS, Kumar B. Topical metronidazole in seborrheic dermatitis—a double-blind study. Dermatology 2001;202:35-37.
4. Smith SA, Baker AE, Williams JH. Effective treatment of seborrheic dermatitis using a low dose, oral homeopathic medication consisting of potassium bromide, sodium bromide, nickel sulfate, and sodium chloride in a double-blind, placebo-controlled study. Altern Med Rev 2002;7:59-67.
5. Scaparro E, Quadri G, Virno G, Orifici C, Milani M. Evaluation of the efficacy and tolerability of oral terbinafine (Daskil) in patients with seborrhoeic dermatitis. A multicentre, randomized, investigator-blinded, placebo-controlled trial. Br J Dermatol 2001;144:854-857.
1. Danby FW, Maddin WS, Margesson LJ, Rosenthal D. A randomized, double-blind, placebo-controlled trial of ketoconazole 2% shampoo versus selenium sulfide 2.5% shampoo in the treatment of moderate to severe dandruff. J Am Acad Dermatol 1993;29:1008-1012.
2. Peter RU, Richarz-Barthauer U. Successful treatment and prophylaxis of scalp seborrhoeic dermatitis and dandruff with 2% ketoconazole shampoo: results of a multicentre, double-blind, placebo-controlled trial. Br J Dermatol 1995;132:441-445.
3. Parsad D, Pandhi R, Negi KS, Kumar B. Topical metronidazole in seborrheic dermatitis—a double-blind study. Dermatology 2001;202:35-37.
4. Smith SA, Baker AE, Williams JH. Effective treatment of seborrheic dermatitis using a low dose, oral homeopathic medication consisting of potassium bromide, sodium bromide, nickel sulfate, and sodium chloride in a double-blind, placebo-controlled study. Altern Med Rev 2002;7:59-67.
5. Scaparro E, Quadri G, Virno G, Orifici C, Milani M. Evaluation of the efficacy and tolerability of oral terbinafine (Daskil) in patients with seborrhoeic dermatitis. A multicentre, randomized, investigator-blinded, placebo-controlled trial. Br J Dermatol 2001;144:854-857.