User login
This Photo Rounds aims to help you hone your visual diagnostic skills to recognize the 3 most common types of skin cancer (in order of prevalence): basal cell carcinoma, squamous cell carcinoma, and melanoma. (See also “Diagnosis of skin malignancy,”.)
Pattern recognition informs us about the initial differential diagnosis and the appropriate biopsy method.
Basal cell carcinoma
The most common basal cell carcinoma is nodular. Figure 1 shows nodular basal cell carcinoma with a raised pearly pink and white nodule with a smooth, shiny, translucent surface. The smooth surface reflects a loss of the normal pore pattern. Telangiectasias can be seen within the lesion, and the border may appear to be rolled.
Figure 2 shows a nodular basal cell carcinoma that is both pigmented and has some central ulceration. This figure demonstrates how difficult it is to distinguish a melanoma from a pigmented basal cell carcinoma.
Figure 3 shows the next most frequently seen basal cell carcinoma, the superficial basal cell carcinoma. These lesions are found most often on the trunk and extremities rather than the face, and may appear as a pink scaling plaque. Sometimes shallow crusts or erosions may be seen within the lesion. Note the thready border present around this scaling plaque. This slightly elevated border is the best tip-off to recognizing this scaling plaque as a skin cancer rather than a plaque of psoriasis or nummular eczema.
Figure 4 shows the least prevalent basal cell carcinoma, the sclerosing type. These lesions are often ivory-colored or colorless. The skin may be appear atrophic and feel indurated. A sclerosing basal cell carcinoma may resemble a scar and can be easily overlooked. These carcinomas are often called morpheaform because of the resemblance to localized scleroderma (morphea). They are also called infiltrating basal cell carcinoma because they infiltrate into the surrounding normal skin in a way not easily visible to the naked eye.
FIGURE 1
Squamous cell carcinoma
The next most common type of skin cancer is squamous cell carcinoma. These cancers are most often found on the lips, ears, and scalp. Figure 5 shows a squamous cell carcinoma on the lower lip. The lower lip catches more ultraviolet rays from the sun than the upper lip, and therefore is the more prevalent site for this carcinoma.
Figure 6 shows a squamous cell carcinoma on the face in an area of sun exposure. This carcinoma looks very much like the superficial basal cell carcinoma in Figure 3, except that the squamous cell carcinoma has one area of crusting. The only way to make a definitive diagnosis is to perform biopsy and get a pathologic reading.
FIGURE 5
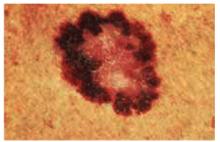
There are many different types of melanomas. Figure 7 shows one version of the most common melanoma, the superficial spreading melanoma. The dark pigmentation around the outside of this melanoma is where the lesion is superficially spreading away from the center (which has lost its pigmentation). This lesion meets all of the ABCDE criteria for malignant melanoma.
Figure 8 shows a melanoma arising in a lentigo maligna on the face of an older patient. It is not necessary to know the type of melanoma before the biopsy, but you should recognize that the lesion may be melanoma and perform a full-thickness biopsy. What may have started off as a simple age spot in this patient has become a malignant melanoma (see page 214).
Figure 9 shows a very thick and deadly nodular melanoma. One can recognize a nodular melanoma by the increased thickness and its darker pigmentation.
Figure 10 shows an uncommon type of melanoma but one of the deadliest—the acrallentiginous melanoma. This melanoma is often not detected until it has metastasized. Any pigmented lesion on the hands, feet, or under the fingernails that looks like melanoma should be biopsied early before it gets to this deadly stage.
FIGURE 7
Choice of biopsy technique
Choice of biopsy technique depends on the type of skin lesion. Most basal cell and squamous cell carcinomas can be adequately biopsied by the shave technique because the pathology is superficial and the prognosis is not determined by thickness. Exceptions include sclerosing basal cell carcinomas and very flat superficial basal cell carcinomas, which are best biopsied with a full-thickness specimen in the form of a punch biopsy or excisional biopsy.
All lesions you suspect may be melanoma should be biopsied with a full-thickness specimen. Very small and very large lesions can initially be biopsied using a punch instrument. The excisional biopsy is preferred when the lesion can be removed with one surgical procedure. Depending upon the depth of the melanoma, you may need to perform a second surgery to get adequate margins.
This Photo Rounds aims to help you hone your visual diagnostic skills to recognize the 3 most common types of skin cancer (in order of prevalence): basal cell carcinoma, squamous cell carcinoma, and melanoma. (See also “Diagnosis of skin malignancy,”.)
Pattern recognition informs us about the initial differential diagnosis and the appropriate biopsy method.
Basal cell carcinoma
The most common basal cell carcinoma is nodular. Figure 1 shows nodular basal cell carcinoma with a raised pearly pink and white nodule with a smooth, shiny, translucent surface. The smooth surface reflects a loss of the normal pore pattern. Telangiectasias can be seen within the lesion, and the border may appear to be rolled.
Figure 2 shows a nodular basal cell carcinoma that is both pigmented and has some central ulceration. This figure demonstrates how difficult it is to distinguish a melanoma from a pigmented basal cell carcinoma.
Figure 3 shows the next most frequently seen basal cell carcinoma, the superficial basal cell carcinoma. These lesions are found most often on the trunk and extremities rather than the face, and may appear as a pink scaling plaque. Sometimes shallow crusts or erosions may be seen within the lesion. Note the thready border present around this scaling plaque. This slightly elevated border is the best tip-off to recognizing this scaling plaque as a skin cancer rather than a plaque of psoriasis or nummular eczema.
Figure 4 shows the least prevalent basal cell carcinoma, the sclerosing type. These lesions are often ivory-colored or colorless. The skin may be appear atrophic and feel indurated. A sclerosing basal cell carcinoma may resemble a scar and can be easily overlooked. These carcinomas are often called morpheaform because of the resemblance to localized scleroderma (morphea). They are also called infiltrating basal cell carcinoma because they infiltrate into the surrounding normal skin in a way not easily visible to the naked eye.
FIGURE 1
Squamous cell carcinoma
The next most common type of skin cancer is squamous cell carcinoma. These cancers are most often found on the lips, ears, and scalp. Figure 5 shows a squamous cell carcinoma on the lower lip. The lower lip catches more ultraviolet rays from the sun than the upper lip, and therefore is the more prevalent site for this carcinoma.
Figure 6 shows a squamous cell carcinoma on the face in an area of sun exposure. This carcinoma looks very much like the superficial basal cell carcinoma in Figure 3, except that the squamous cell carcinoma has one area of crusting. The only way to make a definitive diagnosis is to perform biopsy and get a pathologic reading.
FIGURE 5
There are many different types of melanomas. Figure 7 shows one version of the most common melanoma, the superficial spreading melanoma. The dark pigmentation around the outside of this melanoma is where the lesion is superficially spreading away from the center (which has lost its pigmentation). This lesion meets all of the ABCDE criteria for malignant melanoma.
Figure 8 shows a melanoma arising in a lentigo maligna on the face of an older patient. It is not necessary to know the type of melanoma before the biopsy, but you should recognize that the lesion may be melanoma and perform a full-thickness biopsy. What may have started off as a simple age spot in this patient has become a malignant melanoma (see page 214).
Figure 9 shows a very thick and deadly nodular melanoma. One can recognize a nodular melanoma by the increased thickness and its darker pigmentation.
Figure 10 shows an uncommon type of melanoma but one of the deadliest—the acrallentiginous melanoma. This melanoma is often not detected until it has metastasized. Any pigmented lesion on the hands, feet, or under the fingernails that looks like melanoma should be biopsied early before it gets to this deadly stage.
FIGURE 7
Choice of biopsy technique
Choice of biopsy technique depends on the type of skin lesion. Most basal cell and squamous cell carcinomas can be adequately biopsied by the shave technique because the pathology is superficial and the prognosis is not determined by thickness. Exceptions include sclerosing basal cell carcinomas and very flat superficial basal cell carcinomas, which are best biopsied with a full-thickness specimen in the form of a punch biopsy or excisional biopsy.
All lesions you suspect may be melanoma should be biopsied with a full-thickness specimen. Very small and very large lesions can initially be biopsied using a punch instrument. The excisional biopsy is preferred when the lesion can be removed with one surgical procedure. Depending upon the depth of the melanoma, you may need to perform a second surgery to get adequate margins.
This Photo Rounds aims to help you hone your visual diagnostic skills to recognize the 3 most common types of skin cancer (in order of prevalence): basal cell carcinoma, squamous cell carcinoma, and melanoma. (See also “Diagnosis of skin malignancy,”.)
Pattern recognition informs us about the initial differential diagnosis and the appropriate biopsy method.
Basal cell carcinoma
The most common basal cell carcinoma is nodular. Figure 1 shows nodular basal cell carcinoma with a raised pearly pink and white nodule with a smooth, shiny, translucent surface. The smooth surface reflects a loss of the normal pore pattern. Telangiectasias can be seen within the lesion, and the border may appear to be rolled.
Figure 2 shows a nodular basal cell carcinoma that is both pigmented and has some central ulceration. This figure demonstrates how difficult it is to distinguish a melanoma from a pigmented basal cell carcinoma.
Figure 3 shows the next most frequently seen basal cell carcinoma, the superficial basal cell carcinoma. These lesions are found most often on the trunk and extremities rather than the face, and may appear as a pink scaling plaque. Sometimes shallow crusts or erosions may be seen within the lesion. Note the thready border present around this scaling plaque. This slightly elevated border is the best tip-off to recognizing this scaling plaque as a skin cancer rather than a plaque of psoriasis or nummular eczema.
Figure 4 shows the least prevalent basal cell carcinoma, the sclerosing type. These lesions are often ivory-colored or colorless. The skin may be appear atrophic and feel indurated. A sclerosing basal cell carcinoma may resemble a scar and can be easily overlooked. These carcinomas are often called morpheaform because of the resemblance to localized scleroderma (morphea). They are also called infiltrating basal cell carcinoma because they infiltrate into the surrounding normal skin in a way not easily visible to the naked eye.
FIGURE 1
Squamous cell carcinoma
The next most common type of skin cancer is squamous cell carcinoma. These cancers are most often found on the lips, ears, and scalp. Figure 5 shows a squamous cell carcinoma on the lower lip. The lower lip catches more ultraviolet rays from the sun than the upper lip, and therefore is the more prevalent site for this carcinoma.
Figure 6 shows a squamous cell carcinoma on the face in an area of sun exposure. This carcinoma looks very much like the superficial basal cell carcinoma in Figure 3, except that the squamous cell carcinoma has one area of crusting. The only way to make a definitive diagnosis is to perform biopsy and get a pathologic reading.
FIGURE 5
There are many different types of melanomas. Figure 7 shows one version of the most common melanoma, the superficial spreading melanoma. The dark pigmentation around the outside of this melanoma is where the lesion is superficially spreading away from the center (which has lost its pigmentation). This lesion meets all of the ABCDE criteria for malignant melanoma.
Figure 8 shows a melanoma arising in a lentigo maligna on the face of an older patient. It is not necessary to know the type of melanoma before the biopsy, but you should recognize that the lesion may be melanoma and perform a full-thickness biopsy. What may have started off as a simple age spot in this patient has become a malignant melanoma (see page 214).
Figure 9 shows a very thick and deadly nodular melanoma. One can recognize a nodular melanoma by the increased thickness and its darker pigmentation.
Figure 10 shows an uncommon type of melanoma but one of the deadliest—the acrallentiginous melanoma. This melanoma is often not detected until it has metastasized. Any pigmented lesion on the hands, feet, or under the fingernails that looks like melanoma should be biopsied early before it gets to this deadly stage.
FIGURE 7
Choice of biopsy technique
Choice of biopsy technique depends on the type of skin lesion. Most basal cell and squamous cell carcinomas can be adequately biopsied by the shave technique because the pathology is superficial and the prognosis is not determined by thickness. Exceptions include sclerosing basal cell carcinomas and very flat superficial basal cell carcinomas, which are best biopsied with a full-thickness specimen in the form of a punch biopsy or excisional biopsy.
All lesions you suspect may be melanoma should be biopsied with a full-thickness specimen. Very small and very large lesions can initially be biopsied using a punch instrument. The excisional biopsy is preferred when the lesion can be removed with one surgical procedure. Depending upon the depth of the melanoma, you may need to perform a second surgery to get adequate margins.