User login
As the men and women who graciously serve our country return home, often times we can easily recognize the associated morbidity that resulted from their service. The physical injuries that can occur are obvious. But people have become more sensitive toward the injuries that are not so easily apparent, such as traumatic brain injury and posttraumatic stress disorder (PTSD). These injuries have been the targets of campaigns to increase awareness not only among practitioners, but also the lay population, particularly as they relate to concussive sports injuries.
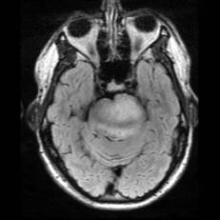
Because these issues are on the forefront of our minds, it’s not hard to understand the misdiagnosis of PTSD in a young marine, Corporal Jordan Mills, who started having difficulty with left ptosis and episodic diplopia in 2008. It wasn’t until he became dysarthric and clumsy on the opposite side that he was transferred out of Afghanistan to a military facility in Germany, where an MRI of the brain revealed a mass raising concern for a brainstem glioma.
Brainstem glioma is a rare brain tumor that occurs mainly in the pediatric population and in young adults. Tissue diagnosis of brainstem glioma often is avoided in an attempt to first do no harm because of the tumor’s diffusely infiltrative nature and the distortion and expansion of the brainstem and its valuable inhabitants. Brainstem glioma is one of the rare instances in oncology when it has been accepted as appropriate to treat based on imaging alone without a tissue diagnosis. Conventional therapy includes radiation with or without the addition of chemotherapy. In spite of aggressive treatment strategies, this fulminating tumor is often fatal within months to years of diagnosis.
Colleagues at the Children’s National Medical Center have developed a protocol to collect serum, cerebrospinal fluid, urine, and tumor tissue of affected patients in an attempt to identify unique molecular abnormalities that would allow practitioners to target therapy more accurately to improve treatment efficacy. Brainstem glioma has been elusive given the lack of tissue to study up to this point, based on only tumor location and biopsy, as opposed to resection options.
In 2010, researchers at the Armed Forces Health Surveillance Center reviewed cancer data from 2000-2010 and found that service members have higher rates of melanoma, brain, non-Hodgkin’s lymphoma, and breast, prostate, and testicular cancers than civilians do. The strongest risk factor was associated with age. Interestingly, marines were found to have the lowest rate of cancer overall. Over the time period studied, 904 service members died of cancer, with 101 soldiers succumbing to brain or other nervous system types of cancer.
At the age of 22 years, it was accepted that this was Corp. Mills’s diagnosis and he was honorably discharged from his third and final tour with the marines. He was treated aggressively and went on to receive chemotherapy during his radiation phase and then received an additional 12 months of oral chemotherapy thereafter.
In addition to Jordan’s remarkable physical strength, his mental and emotional strength persevered. His attitude all the while was to continue to live life to the fullest and trust through his faith and his medical team that his tumor would be taken care of.
Jordan went on to marry, start a family, and enroll in the local community college where he graduated with an associate’s degree in accounting with honors. He was accepted into a prestigious school of business and is working to receive his bachelor’s degree in accounting.
Jordan’s tumor progressed in November 2011 and Jordan has reinitiated chemotherapy. His resolve is stronger than ever and he’s working to develop a foundation for marines with brain tumors. The goals of the foundation are to not only provide financial support to the marines and their immediate family, but also to support the education of military personnel on early detection of CNS disorders.
Dr. Porter is a neuro-oncologist in the department of neurology at the Mayo Clinic in Phoenix.
As the men and women who graciously serve our country return home, often times we can easily recognize the associated morbidity that resulted from their service. The physical injuries that can occur are obvious. But people have become more sensitive toward the injuries that are not so easily apparent, such as traumatic brain injury and posttraumatic stress disorder (PTSD). These injuries have been the targets of campaigns to increase awareness not only among practitioners, but also the lay population, particularly as they relate to concussive sports injuries.
Because these issues are on the forefront of our minds, it’s not hard to understand the misdiagnosis of PTSD in a young marine, Corporal Jordan Mills, who started having difficulty with left ptosis and episodic diplopia in 2008. It wasn’t until he became dysarthric and clumsy on the opposite side that he was transferred out of Afghanistan to a military facility in Germany, where an MRI of the brain revealed a mass raising concern for a brainstem glioma.
Brainstem glioma is a rare brain tumor that occurs mainly in the pediatric population and in young adults. Tissue diagnosis of brainstem glioma often is avoided in an attempt to first do no harm because of the tumor’s diffusely infiltrative nature and the distortion and expansion of the brainstem and its valuable inhabitants. Brainstem glioma is one of the rare instances in oncology when it has been accepted as appropriate to treat based on imaging alone without a tissue diagnosis. Conventional therapy includes radiation with or without the addition of chemotherapy. In spite of aggressive treatment strategies, this fulminating tumor is often fatal within months to years of diagnosis.
Colleagues at the Children’s National Medical Center have developed a protocol to collect serum, cerebrospinal fluid, urine, and tumor tissue of affected patients in an attempt to identify unique molecular abnormalities that would allow practitioners to target therapy more accurately to improve treatment efficacy. Brainstem glioma has been elusive given the lack of tissue to study up to this point, based on only tumor location and biopsy, as opposed to resection options.
In 2010, researchers at the Armed Forces Health Surveillance Center reviewed cancer data from 2000-2010 and found that service members have higher rates of melanoma, brain, non-Hodgkin’s lymphoma, and breast, prostate, and testicular cancers than civilians do. The strongest risk factor was associated with age. Interestingly, marines were found to have the lowest rate of cancer overall. Over the time period studied, 904 service members died of cancer, with 101 soldiers succumbing to brain or other nervous system types of cancer.
At the age of 22 years, it was accepted that this was Corp. Mills’s diagnosis and he was honorably discharged from his third and final tour with the marines. He was treated aggressively and went on to receive chemotherapy during his radiation phase and then received an additional 12 months of oral chemotherapy thereafter.
In addition to Jordan’s remarkable physical strength, his mental and emotional strength persevered. His attitude all the while was to continue to live life to the fullest and trust through his faith and his medical team that his tumor would be taken care of.
Jordan went on to marry, start a family, and enroll in the local community college where he graduated with an associate’s degree in accounting with honors. He was accepted into a prestigious school of business and is working to receive his bachelor’s degree in accounting.
Jordan’s tumor progressed in November 2011 and Jordan has reinitiated chemotherapy. His resolve is stronger than ever and he’s working to develop a foundation for marines with brain tumors. The goals of the foundation are to not only provide financial support to the marines and their immediate family, but also to support the education of military personnel on early detection of CNS disorders.
Dr. Porter is a neuro-oncologist in the department of neurology at the Mayo Clinic in Phoenix.
As the men and women who graciously serve our country return home, often times we can easily recognize the associated morbidity that resulted from their service. The physical injuries that can occur are obvious. But people have become more sensitive toward the injuries that are not so easily apparent, such as traumatic brain injury and posttraumatic stress disorder (PTSD). These injuries have been the targets of campaigns to increase awareness not only among practitioners, but also the lay population, particularly as they relate to concussive sports injuries.
Because these issues are on the forefront of our minds, it’s not hard to understand the misdiagnosis of PTSD in a young marine, Corporal Jordan Mills, who started having difficulty with left ptosis and episodic diplopia in 2008. It wasn’t until he became dysarthric and clumsy on the opposite side that he was transferred out of Afghanistan to a military facility in Germany, where an MRI of the brain revealed a mass raising concern for a brainstem glioma.
Brainstem glioma is a rare brain tumor that occurs mainly in the pediatric population and in young adults. Tissue diagnosis of brainstem glioma often is avoided in an attempt to first do no harm because of the tumor’s diffusely infiltrative nature and the distortion and expansion of the brainstem and its valuable inhabitants. Brainstem glioma is one of the rare instances in oncology when it has been accepted as appropriate to treat based on imaging alone without a tissue diagnosis. Conventional therapy includes radiation with or without the addition of chemotherapy. In spite of aggressive treatment strategies, this fulminating tumor is often fatal within months to years of diagnosis.
Colleagues at the Children’s National Medical Center have developed a protocol to collect serum, cerebrospinal fluid, urine, and tumor tissue of affected patients in an attempt to identify unique molecular abnormalities that would allow practitioners to target therapy more accurately to improve treatment efficacy. Brainstem glioma has been elusive given the lack of tissue to study up to this point, based on only tumor location and biopsy, as opposed to resection options.
In 2010, researchers at the Armed Forces Health Surveillance Center reviewed cancer data from 2000-2010 and found that service members have higher rates of melanoma, brain, non-Hodgkin’s lymphoma, and breast, prostate, and testicular cancers than civilians do. The strongest risk factor was associated with age. Interestingly, marines were found to have the lowest rate of cancer overall. Over the time period studied, 904 service members died of cancer, with 101 soldiers succumbing to brain or other nervous system types of cancer.
At the age of 22 years, it was accepted that this was Corp. Mills’s diagnosis and he was honorably discharged from his third and final tour with the marines. He was treated aggressively and went on to receive chemotherapy during his radiation phase and then received an additional 12 months of oral chemotherapy thereafter.
In addition to Jordan’s remarkable physical strength, his mental and emotional strength persevered. His attitude all the while was to continue to live life to the fullest and trust through his faith and his medical team that his tumor would be taken care of.
Jordan went on to marry, start a family, and enroll in the local community college where he graduated with an associate’s degree in accounting with honors. He was accepted into a prestigious school of business and is working to receive his bachelor’s degree in accounting.
Jordan’s tumor progressed in November 2011 and Jordan has reinitiated chemotherapy. His resolve is stronger than ever and he’s working to develop a foundation for marines with brain tumors. The goals of the foundation are to not only provide financial support to the marines and their immediate family, but also to support the education of military personnel on early detection of CNS disorders.
Dr. Porter is a neuro-oncologist in the department of neurology at the Mayo Clinic in Phoenix.