User login
Four days after delivering a boy by cesarean section, a 24-year-old woman sought care at our gynecology emergency room for a diffuse skin eruption. She said that one day after delivery, she developed several pruritic lesions near the site of the surgical incision. She attributed this to the surgical tape, but within the next 24 hours, blisters began to develop elsewhere on her body.
On exam, we noted light pink papules and plaques—some with overlying tense bullae—in and around her umbilicus (FIGURE 1), as well as on her abdomen, lower extremities, and within the left third and fourth web space of her toes. There were no lesions in the oral mucosa or near the groin or genitalia.
Aside from this blistering skin eruption, our patient was recovering well after the C-section. Her postoperative medications included simethicone, prenatal vitamins with iron, ibuprofen, ferrous sulfate, stool softeners, and acetaminophen with codeine. She indicated that her newborn son didn’t have any health problems—skin or otherwise—and her 2 other sons were healthy. She had no significant medical or dermatologic history. We performed a skin biopsy.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Pemphigoid gestationis
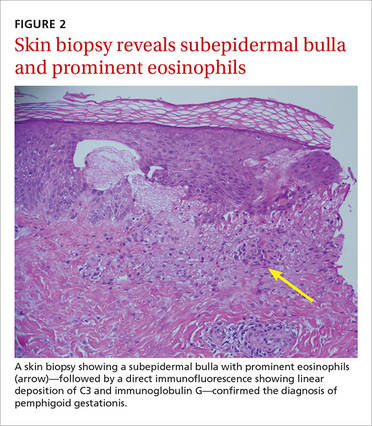
Based on the appearance of the lesions and the lab findings, we diagnosed our patient with pemphigoid gestationis (PG). The pathology demonstrated a subepidermal blister with prominent eosinophils, which supported the diagnosis (FIGURE 2). Direct immunofluorescence further supported the diagnosis, as it showed a thick, dense, and linear C3 deposition and weak immunoglobulin G deposition along the epidermal basement membrane zone.
PG, previously referred to as herpes gestationis, is a rare autoimmune dermatosis of pregnancy that usually presents with intense, pruritic, erythematous papules and blisters that surround the umbilicus. PG lesions spread rapidly throughout the body, but tend to spare the face and oral mucosa. The incidence is approximately 1 in 50,000 pregnancies.1
Although the exact pathogenesis of PG is unknown, it is hypothesized that major histocompatibility complex class II antigens within the placenta may play a role through cross-reaction with maternal skin.2
PG usually develops weeks to months before delivery
The onset of PG is usually during the second or third trimester; it typically manifests earlier and with greater severity in subsequent pregnancies.2 That said, postpartum cases and cases where PG “skipped” pregnancies have been reported.2 PG can impact the fetus—about 5% to 10% of infants born to affected mothers have a diffuse bullous eruption similar to that of PG.3 One study found a fetal mortality rate of up to 30% and high rates of prematurity.1
This case represents an interesting variation because the patient hadn’t developed any dermatologic conditions during her previous 2 pregnancies, and it was only after she delivered her third child that she developed PG. While there is a wide range of possible presentations of PG, all mothers who have it should be monitored by an obstetrician and should follow up with a dermatologist during their prenatal periods due to the small but significant risks of prematurity and fetal growth restriction.4
Reactivation of symptoms. Although PG symptoms typically resolve several weeks before delivery, 75% of patients experience reactivation of their symptoms at delivery.4 Progestin has immunosuppressive properties, and variations in progestin levels near delivery are thought to be responsible for the relapsing-remitting course of PG symptoms.4
Rule out other diagnoses with patch testing, skin biopsy
Pruritic and erythematous bullae and vesicles, particularly around the umbilicus, should raise clinical suspicion for PG in a pregnant patient. A skin biopsy showing a subepidermal bulla with prominent eosinophils, as well as direct immunofluorescence showing linear deposition of C3 and IgG at the dermo-epidermal junction, indicates a diagnosis of PG.
The differential diagnosis of PG includes urticarial/bullous drug eruptions, viral exanthems, allergic contact dermatitis, and pruritic urticarial papules and plaques of pregnancy (PUPPP). Clinical correlation and a careful review of the patient’s medications, symptoms, and exposure to viruses can aid in ruling out a drug eruption or viral exanthema. Patch testing can be performed to rule out allergic contact dermatitis, and serum testing or indirect immunofluorescence or enzyme-linked immunosorbent assay is recommended to rule out PUPPP.
Treat with topical corticosteroids and systemic antihistamines
The goal of treatment for PG is to provide relief from the pruritus and to decrease and suppress blister formation. Topical corticosteroids, such as clobetasol or betamethasone, and systemic antihistamines, such as cetirizine, can be used to treat mild cases of PG. First-generation antihistamines are favored over second-generation antihistamines because of their increased safety when used during pregnancy.
Severe cases. Oral steroids are used for patients with more severe cases of PG. The preferred corticosteroid is prednisolone, typically starting at 20 to 40 mg/d or 0.5 to 1 mg/kg/d and adjusting as needed.5 For patients who do not respond to corticosteroids or for whom corticosteroids are contraindicated, intravenous immunoglobulins or plasmapheresis may be beneficial.5 If a patient requires postpartum treatment, the possibility of medications being passed through breast milk needs to be considered.
Our patient. We prescribed clobetasol 0.05% ointment for our patient and told her to apply it twice daily to the affected areas. We discussed the possibility of using a systemic corticosteroid, but she opted to use the topical medication exclusively because she was breastfeeding. Although our patient still gets an occasional blister when she is stressed, they go away 1 to 2 days after she applies the clobetasol ointment.
CORRESPONDENCE
Sarah Groff, MD, University of Texas Health Science Center at San Antonio, 7979 Wurzbach Road, San Antonio, TX 78229; [email protected].
1. Lawley TJ, Stingl G, Katz SI. Fetal and maternal risk factors in herpes gestationis. Arch Dermatol. 1978;114:552-555.
2. Engineer L, Bhol K, Ahmed AR. Pemphigoid gestationis: a review. Am J Obstet Gynecol. 2000;183:483-491.
3. Katz A, Minto JO, Toole JW, et al. Immunopathologic study of herpes gestationis in mother and infant. Arch Dermatol. 1977;113:1069-1072.
4. Huilaja L, Mäkikallio K, Tasanen K. Gestational pemphigoid. Orphanet J Rare Dis. 2014;9:136.
5. Jurecka W. Pregnancy dermatoses. In: Lebwohl MG, Berth-Jones J, Heymann WR, et al, eds. Treatment of Skin Disease: Comprehensive Therapeutic Strategies. 4th ed. Philadelphia, PA: Elsevier Saunders; 2014:606-611.
Four days after delivering a boy by cesarean section, a 24-year-old woman sought care at our gynecology emergency room for a diffuse skin eruption. She said that one day after delivery, she developed several pruritic lesions near the site of the surgical incision. She attributed this to the surgical tape, but within the next 24 hours, blisters began to develop elsewhere on her body.
On exam, we noted light pink papules and plaques—some with overlying tense bullae—in and around her umbilicus (FIGURE 1), as well as on her abdomen, lower extremities, and within the left third and fourth web space of her toes. There were no lesions in the oral mucosa or near the groin or genitalia.
Aside from this blistering skin eruption, our patient was recovering well after the C-section. Her postoperative medications included simethicone, prenatal vitamins with iron, ibuprofen, ferrous sulfate, stool softeners, and acetaminophen with codeine. She indicated that her newborn son didn’t have any health problems—skin or otherwise—and her 2 other sons were healthy. She had no significant medical or dermatologic history. We performed a skin biopsy.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Pemphigoid gestationis
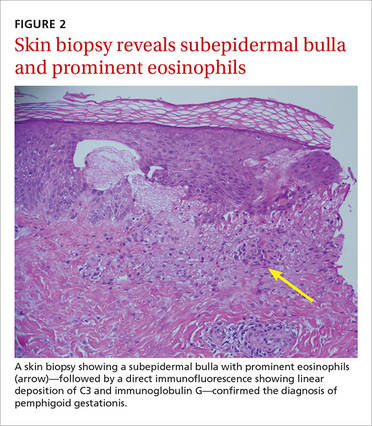
Based on the appearance of the lesions and the lab findings, we diagnosed our patient with pemphigoid gestationis (PG). The pathology demonstrated a subepidermal blister with prominent eosinophils, which supported the diagnosis (FIGURE 2). Direct immunofluorescence further supported the diagnosis, as it showed a thick, dense, and linear C3 deposition and weak immunoglobulin G deposition along the epidermal basement membrane zone.
PG, previously referred to as herpes gestationis, is a rare autoimmune dermatosis of pregnancy that usually presents with intense, pruritic, erythematous papules and blisters that surround the umbilicus. PG lesions spread rapidly throughout the body, but tend to spare the face and oral mucosa. The incidence is approximately 1 in 50,000 pregnancies.1
Although the exact pathogenesis of PG is unknown, it is hypothesized that major histocompatibility complex class II antigens within the placenta may play a role through cross-reaction with maternal skin.2
PG usually develops weeks to months before delivery
The onset of PG is usually during the second or third trimester; it typically manifests earlier and with greater severity in subsequent pregnancies.2 That said, postpartum cases and cases where PG “skipped” pregnancies have been reported.2 PG can impact the fetus—about 5% to 10% of infants born to affected mothers have a diffuse bullous eruption similar to that of PG.3 One study found a fetal mortality rate of up to 30% and high rates of prematurity.1
This case represents an interesting variation because the patient hadn’t developed any dermatologic conditions during her previous 2 pregnancies, and it was only after she delivered her third child that she developed PG. While there is a wide range of possible presentations of PG, all mothers who have it should be monitored by an obstetrician and should follow up with a dermatologist during their prenatal periods due to the small but significant risks of prematurity and fetal growth restriction.4
Reactivation of symptoms. Although PG symptoms typically resolve several weeks before delivery, 75% of patients experience reactivation of their symptoms at delivery.4 Progestin has immunosuppressive properties, and variations in progestin levels near delivery are thought to be responsible for the relapsing-remitting course of PG symptoms.4
Rule out other diagnoses with patch testing, skin biopsy
Pruritic and erythematous bullae and vesicles, particularly around the umbilicus, should raise clinical suspicion for PG in a pregnant patient. A skin biopsy showing a subepidermal bulla with prominent eosinophils, as well as direct immunofluorescence showing linear deposition of C3 and IgG at the dermo-epidermal junction, indicates a diagnosis of PG.
The differential diagnosis of PG includes urticarial/bullous drug eruptions, viral exanthems, allergic contact dermatitis, and pruritic urticarial papules and plaques of pregnancy (PUPPP). Clinical correlation and a careful review of the patient’s medications, symptoms, and exposure to viruses can aid in ruling out a drug eruption or viral exanthema. Patch testing can be performed to rule out allergic contact dermatitis, and serum testing or indirect immunofluorescence or enzyme-linked immunosorbent assay is recommended to rule out PUPPP.
Treat with topical corticosteroids and systemic antihistamines
The goal of treatment for PG is to provide relief from the pruritus and to decrease and suppress blister formation. Topical corticosteroids, such as clobetasol or betamethasone, and systemic antihistamines, such as cetirizine, can be used to treat mild cases of PG. First-generation antihistamines are favored over second-generation antihistamines because of their increased safety when used during pregnancy.
Severe cases. Oral steroids are used for patients with more severe cases of PG. The preferred corticosteroid is prednisolone, typically starting at 20 to 40 mg/d or 0.5 to 1 mg/kg/d and adjusting as needed.5 For patients who do not respond to corticosteroids or for whom corticosteroids are contraindicated, intravenous immunoglobulins or plasmapheresis may be beneficial.5 If a patient requires postpartum treatment, the possibility of medications being passed through breast milk needs to be considered.
Our patient. We prescribed clobetasol 0.05% ointment for our patient and told her to apply it twice daily to the affected areas. We discussed the possibility of using a systemic corticosteroid, but she opted to use the topical medication exclusively because she was breastfeeding. Although our patient still gets an occasional blister when she is stressed, they go away 1 to 2 days after she applies the clobetasol ointment.
CORRESPONDENCE
Sarah Groff, MD, University of Texas Health Science Center at San Antonio, 7979 Wurzbach Road, San Antonio, TX 78229; [email protected].
Four days after delivering a boy by cesarean section, a 24-year-old woman sought care at our gynecology emergency room for a diffuse skin eruption. She said that one day after delivery, she developed several pruritic lesions near the site of the surgical incision. She attributed this to the surgical tape, but within the next 24 hours, blisters began to develop elsewhere on her body.
On exam, we noted light pink papules and plaques—some with overlying tense bullae—in and around her umbilicus (FIGURE 1), as well as on her abdomen, lower extremities, and within the left third and fourth web space of her toes. There were no lesions in the oral mucosa or near the groin or genitalia.
Aside from this blistering skin eruption, our patient was recovering well after the C-section. Her postoperative medications included simethicone, prenatal vitamins with iron, ibuprofen, ferrous sulfate, stool softeners, and acetaminophen with codeine. She indicated that her newborn son didn’t have any health problems—skin or otherwise—and her 2 other sons were healthy. She had no significant medical or dermatologic history. We performed a skin biopsy.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Pemphigoid gestationis
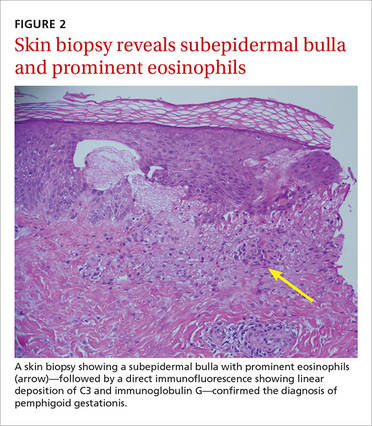
Based on the appearance of the lesions and the lab findings, we diagnosed our patient with pemphigoid gestationis (PG). The pathology demonstrated a subepidermal blister with prominent eosinophils, which supported the diagnosis (FIGURE 2). Direct immunofluorescence further supported the diagnosis, as it showed a thick, dense, and linear C3 deposition and weak immunoglobulin G deposition along the epidermal basement membrane zone.
PG, previously referred to as herpes gestationis, is a rare autoimmune dermatosis of pregnancy that usually presents with intense, pruritic, erythematous papules and blisters that surround the umbilicus. PG lesions spread rapidly throughout the body, but tend to spare the face and oral mucosa. The incidence is approximately 1 in 50,000 pregnancies.1
Although the exact pathogenesis of PG is unknown, it is hypothesized that major histocompatibility complex class II antigens within the placenta may play a role through cross-reaction with maternal skin.2
PG usually develops weeks to months before delivery
The onset of PG is usually during the second or third trimester; it typically manifests earlier and with greater severity in subsequent pregnancies.2 That said, postpartum cases and cases where PG “skipped” pregnancies have been reported.2 PG can impact the fetus—about 5% to 10% of infants born to affected mothers have a diffuse bullous eruption similar to that of PG.3 One study found a fetal mortality rate of up to 30% and high rates of prematurity.1
This case represents an interesting variation because the patient hadn’t developed any dermatologic conditions during her previous 2 pregnancies, and it was only after she delivered her third child that she developed PG. While there is a wide range of possible presentations of PG, all mothers who have it should be monitored by an obstetrician and should follow up with a dermatologist during their prenatal periods due to the small but significant risks of prematurity and fetal growth restriction.4
Reactivation of symptoms. Although PG symptoms typically resolve several weeks before delivery, 75% of patients experience reactivation of their symptoms at delivery.4 Progestin has immunosuppressive properties, and variations in progestin levels near delivery are thought to be responsible for the relapsing-remitting course of PG symptoms.4
Rule out other diagnoses with patch testing, skin biopsy
Pruritic and erythematous bullae and vesicles, particularly around the umbilicus, should raise clinical suspicion for PG in a pregnant patient. A skin biopsy showing a subepidermal bulla with prominent eosinophils, as well as direct immunofluorescence showing linear deposition of C3 and IgG at the dermo-epidermal junction, indicates a diagnosis of PG.
The differential diagnosis of PG includes urticarial/bullous drug eruptions, viral exanthems, allergic contact dermatitis, and pruritic urticarial papules and plaques of pregnancy (PUPPP). Clinical correlation and a careful review of the patient’s medications, symptoms, and exposure to viruses can aid in ruling out a drug eruption or viral exanthema. Patch testing can be performed to rule out allergic contact dermatitis, and serum testing or indirect immunofluorescence or enzyme-linked immunosorbent assay is recommended to rule out PUPPP.
Treat with topical corticosteroids and systemic antihistamines
The goal of treatment for PG is to provide relief from the pruritus and to decrease and suppress blister formation. Topical corticosteroids, such as clobetasol or betamethasone, and systemic antihistamines, such as cetirizine, can be used to treat mild cases of PG. First-generation antihistamines are favored over second-generation antihistamines because of their increased safety when used during pregnancy.
Severe cases. Oral steroids are used for patients with more severe cases of PG. The preferred corticosteroid is prednisolone, typically starting at 20 to 40 mg/d or 0.5 to 1 mg/kg/d and adjusting as needed.5 For patients who do not respond to corticosteroids or for whom corticosteroids are contraindicated, intravenous immunoglobulins or plasmapheresis may be beneficial.5 If a patient requires postpartum treatment, the possibility of medications being passed through breast milk needs to be considered.
Our patient. We prescribed clobetasol 0.05% ointment for our patient and told her to apply it twice daily to the affected areas. We discussed the possibility of using a systemic corticosteroid, but she opted to use the topical medication exclusively because she was breastfeeding. Although our patient still gets an occasional blister when she is stressed, they go away 1 to 2 days after she applies the clobetasol ointment.
CORRESPONDENCE
Sarah Groff, MD, University of Texas Health Science Center at San Antonio, 7979 Wurzbach Road, San Antonio, TX 78229; [email protected].
1. Lawley TJ, Stingl G, Katz SI. Fetal and maternal risk factors in herpes gestationis. Arch Dermatol. 1978;114:552-555.
2. Engineer L, Bhol K, Ahmed AR. Pemphigoid gestationis: a review. Am J Obstet Gynecol. 2000;183:483-491.
3. Katz A, Minto JO, Toole JW, et al. Immunopathologic study of herpes gestationis in mother and infant. Arch Dermatol. 1977;113:1069-1072.
4. Huilaja L, Mäkikallio K, Tasanen K. Gestational pemphigoid. Orphanet J Rare Dis. 2014;9:136.
5. Jurecka W. Pregnancy dermatoses. In: Lebwohl MG, Berth-Jones J, Heymann WR, et al, eds. Treatment of Skin Disease: Comprehensive Therapeutic Strategies. 4th ed. Philadelphia, PA: Elsevier Saunders; 2014:606-611.
1. Lawley TJ, Stingl G, Katz SI. Fetal and maternal risk factors in herpes gestationis. Arch Dermatol. 1978;114:552-555.
2. Engineer L, Bhol K, Ahmed AR. Pemphigoid gestationis: a review. Am J Obstet Gynecol. 2000;183:483-491.
3. Katz A, Minto JO, Toole JW, et al. Immunopathologic study of herpes gestationis in mother and infant. Arch Dermatol. 1977;113:1069-1072.
4. Huilaja L, Mäkikallio K, Tasanen K. Gestational pemphigoid. Orphanet J Rare Dis. 2014;9:136.
5. Jurecka W. Pregnancy dermatoses. In: Lebwohl MG, Berth-Jones J, Heymann WR, et al, eds. Treatment of Skin Disease: Comprehensive Therapeutic Strategies. 4th ed. Philadelphia, PA: Elsevier Saunders; 2014:606-611.
