User login
Researchers are attempting to develop new models to deal with patient privacy issues, including profound levels of patient participation in the dissemination of personal data, in the new era of genomic medicine, according to an article in the January issue of Science written by Jennifer Couzin-Frankel, based on interviews with participants and investigators in the RUDY trial and other projects.
The RUDY rheumatology registry in London is an example of such a new approach. RUDY, a registry used for research into rare bone diseases and vasculitis, has an emphasis on patients’ self-reported outcomes. In order to alleviate patients’ fears of loss of privacy because of data sharing, the study offers patients various controls over dissemination, according to one of the study’s principal investigators, Dr. Kassim Javaid, a University of Oxford (England) rheumatologist, wrote Ms. Couzin-Frankel (Science 2015;347:501-3).
Patients in the study can determine whether their blood, scans, and medical histories can be shared with other researchers. In addition, they will have access to a clinical trial Web page where they can find out whether their tissues samples are being used by other research groups.
This model is thought to not only increase the sense of patient participation and authority in the study, but also to provide transparency and accountability as to how their information is being used. Dr. Javaid refers to this strategy as “dynamic consent,” because patients can choose which portions of the study to participate in and whether to restrict their data and samples to RUDY investigators or to allow others to study them.
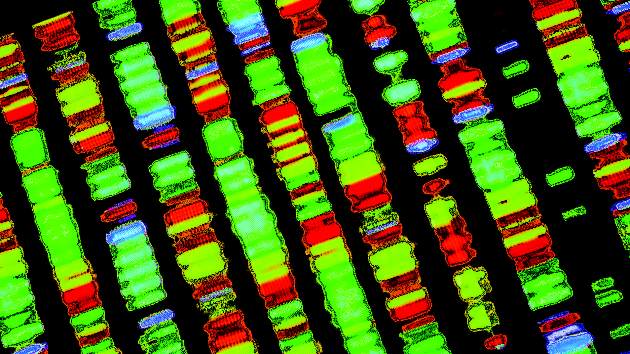
The problem of maintaining privacy is profound, because DNA sequencing provides such a potent means of individual identification. Ms. Couzin-Frankel cites in particular a case published in Science (2013;339:321-4), in which a group working with Dr. Yaniv Erlich showed that a man could be uniquely identified based on a partial DNA sequence of his Y chromosome, age, and U.S. state of residence, which is the type of information commonly posted in DNA databases widely accessible to the research community. By combining this information with data he found for others in the same family on popular genealogy databases, where more than 100,000 people already have posted DNA markers, Dr. Erlich could not only identify the donors of the DNA but also could identify their family members as far as second cousins once removed.
Although such data can be encrypted, reported Ms. Couzin-Frankel, Dr. Erlich pointed out that this can render the information largely useless for research and doesn’t even always protect the donor.
In contrast, however, many participants in trials and databases, such as the database/Web group PatientsLikeMe, see patient altruism as key. PatientsLikeMe has recruited more 300,000 people with more than 2,300 different diseases, who are sharing their health data, how they’re faring in clinical trials, and acting as a support group to one another in order to help medical scientists and drug companies further research their conditions. Patients voluntarily agree to this free flow of information, even though it decreases their privacy.
In another example in which patients cite altruistic reasons for giving up their privacy, the Personal Genome Project at Harvard Medical School in Boston, founded by geneticist George M. Church, Ph.D., has nearly 4,000 participants sharing their DNA sequences and health histories online for anyone to view. The Personal Genome Project even has a “real name” option, which allows participants to post their identity, Ms. Couzin-Frankel reports.
The Science article author, Ms. Couzin-Frankel, is a science journalist with no relevant financial conflicts. The RUDY study is funded by the University of Oxford and the U.K. National Institute for Health Research.
The article in Science raises important ethical questions, re: the deidentification of data and obtaining [of] informed consent when data or tissue or DNA alone can actually be used to identify the patient.

|
Dr. Jennifer S. Lawton |
When we obtain informed consent for participation in clinical trials, we ask our patients to take a “leap of faith” and trust us to maintain their privacy. Our patients personally gain little or nothing for participation, yet they altruistically allow their data or tissue to be used to improve the lives of others. Just as we do not want our Social Security number, bank account information, and credit card numbers to be public knowledge, we also do not want our genetic information – with potential risks of developing or predispositions for life-threatening diseases – public knowledge (or accessible to employers and insurance companies). These questions will be the topic of many ethical discussions in the future, and will provide an opportunity for innovative and advanced technology and methods to protect personal information.
Dr. Jennifer S. Lawton is the Acquired Cardiovascular Disease section editor for Thoracic Surgery News.
The article in Science raises important ethical questions, re: the deidentification of data and obtaining [of] informed consent when data or tissue or DNA alone can actually be used to identify the patient.

|
Dr. Jennifer S. Lawton |
When we obtain informed consent for participation in clinical trials, we ask our patients to take a “leap of faith” and trust us to maintain their privacy. Our patients personally gain little or nothing for participation, yet they altruistically allow their data or tissue to be used to improve the lives of others. Just as we do not want our Social Security number, bank account information, and credit card numbers to be public knowledge, we also do not want our genetic information – with potential risks of developing or predispositions for life-threatening diseases – public knowledge (or accessible to employers and insurance companies). These questions will be the topic of many ethical discussions in the future, and will provide an opportunity for innovative and advanced technology and methods to protect personal information.
Dr. Jennifer S. Lawton is the Acquired Cardiovascular Disease section editor for Thoracic Surgery News.
The article in Science raises important ethical questions, re: the deidentification of data and obtaining [of] informed consent when data or tissue or DNA alone can actually be used to identify the patient.

|
Dr. Jennifer S. Lawton |
When we obtain informed consent for participation in clinical trials, we ask our patients to take a “leap of faith” and trust us to maintain their privacy. Our patients personally gain little or nothing for participation, yet they altruistically allow their data or tissue to be used to improve the lives of others. Just as we do not want our Social Security number, bank account information, and credit card numbers to be public knowledge, we also do not want our genetic information – with potential risks of developing or predispositions for life-threatening diseases – public knowledge (or accessible to employers and insurance companies). These questions will be the topic of many ethical discussions in the future, and will provide an opportunity for innovative and advanced technology and methods to protect personal information.
Dr. Jennifer S. Lawton is the Acquired Cardiovascular Disease section editor for Thoracic Surgery News.
Researchers are attempting to develop new models to deal with patient privacy issues, including profound levels of patient participation in the dissemination of personal data, in the new era of genomic medicine, according to an article in the January issue of Science written by Jennifer Couzin-Frankel, based on interviews with participants and investigators in the RUDY trial and other projects.
The RUDY rheumatology registry in London is an example of such a new approach. RUDY, a registry used for research into rare bone diseases and vasculitis, has an emphasis on patients’ self-reported outcomes. In order to alleviate patients’ fears of loss of privacy because of data sharing, the study offers patients various controls over dissemination, according to one of the study’s principal investigators, Dr. Kassim Javaid, a University of Oxford (England) rheumatologist, wrote Ms. Couzin-Frankel (Science 2015;347:501-3).
Patients in the study can determine whether their blood, scans, and medical histories can be shared with other researchers. In addition, they will have access to a clinical trial Web page where they can find out whether their tissues samples are being used by other research groups.
This model is thought to not only increase the sense of patient participation and authority in the study, but also to provide transparency and accountability as to how their information is being used. Dr. Javaid refers to this strategy as “dynamic consent,” because patients can choose which portions of the study to participate in and whether to restrict their data and samples to RUDY investigators or to allow others to study them.
The problem of maintaining privacy is profound, because DNA sequencing provides such a potent means of individual identification. Ms. Couzin-Frankel cites in particular a case published in Science (2013;339:321-4), in which a group working with Dr. Yaniv Erlich showed that a man could be uniquely identified based on a partial DNA sequence of his Y chromosome, age, and U.S. state of residence, which is the type of information commonly posted in DNA databases widely accessible to the research community. By combining this information with data he found for others in the same family on popular genealogy databases, where more than 100,000 people already have posted DNA markers, Dr. Erlich could not only identify the donors of the DNA but also could identify their family members as far as second cousins once removed.
Although such data can be encrypted, reported Ms. Couzin-Frankel, Dr. Erlich pointed out that this can render the information largely useless for research and doesn’t even always protect the donor.
In contrast, however, many participants in trials and databases, such as the database/Web group PatientsLikeMe, see patient altruism as key. PatientsLikeMe has recruited more 300,000 people with more than 2,300 different diseases, who are sharing their health data, how they’re faring in clinical trials, and acting as a support group to one another in order to help medical scientists and drug companies further research their conditions. Patients voluntarily agree to this free flow of information, even though it decreases their privacy.
In another example in which patients cite altruistic reasons for giving up their privacy, the Personal Genome Project at Harvard Medical School in Boston, founded by geneticist George M. Church, Ph.D., has nearly 4,000 participants sharing their DNA sequences and health histories online for anyone to view. The Personal Genome Project even has a “real name” option, which allows participants to post their identity, Ms. Couzin-Frankel reports.
The Science article author, Ms. Couzin-Frankel, is a science journalist with no relevant financial conflicts. The RUDY study is funded by the University of Oxford and the U.K. National Institute for Health Research.
Researchers are attempting to develop new models to deal with patient privacy issues, including profound levels of patient participation in the dissemination of personal data, in the new era of genomic medicine, according to an article in the January issue of Science written by Jennifer Couzin-Frankel, based on interviews with participants and investigators in the RUDY trial and other projects.
The RUDY rheumatology registry in London is an example of such a new approach. RUDY, a registry used for research into rare bone diseases and vasculitis, has an emphasis on patients’ self-reported outcomes. In order to alleviate patients’ fears of loss of privacy because of data sharing, the study offers patients various controls over dissemination, according to one of the study’s principal investigators, Dr. Kassim Javaid, a University of Oxford (England) rheumatologist, wrote Ms. Couzin-Frankel (Science 2015;347:501-3).
Patients in the study can determine whether their blood, scans, and medical histories can be shared with other researchers. In addition, they will have access to a clinical trial Web page where they can find out whether their tissues samples are being used by other research groups.
This model is thought to not only increase the sense of patient participation and authority in the study, but also to provide transparency and accountability as to how their information is being used. Dr. Javaid refers to this strategy as “dynamic consent,” because patients can choose which portions of the study to participate in and whether to restrict their data and samples to RUDY investigators or to allow others to study them.
The problem of maintaining privacy is profound, because DNA sequencing provides such a potent means of individual identification. Ms. Couzin-Frankel cites in particular a case published in Science (2013;339:321-4), in which a group working with Dr. Yaniv Erlich showed that a man could be uniquely identified based on a partial DNA sequence of his Y chromosome, age, and U.S. state of residence, which is the type of information commonly posted in DNA databases widely accessible to the research community. By combining this information with data he found for others in the same family on popular genealogy databases, where more than 100,000 people already have posted DNA markers, Dr. Erlich could not only identify the donors of the DNA but also could identify their family members as far as second cousins once removed.
Although such data can be encrypted, reported Ms. Couzin-Frankel, Dr. Erlich pointed out that this can render the information largely useless for research and doesn’t even always protect the donor.
In contrast, however, many participants in trials and databases, such as the database/Web group PatientsLikeMe, see patient altruism as key. PatientsLikeMe has recruited more 300,000 people with more than 2,300 different diseases, who are sharing their health data, how they’re faring in clinical trials, and acting as a support group to one another in order to help medical scientists and drug companies further research their conditions. Patients voluntarily agree to this free flow of information, even though it decreases their privacy.
In another example in which patients cite altruistic reasons for giving up their privacy, the Personal Genome Project at Harvard Medical School in Boston, founded by geneticist George M. Church, Ph.D., has nearly 4,000 participants sharing their DNA sequences and health histories online for anyone to view. The Personal Genome Project even has a “real name” option, which allows participants to post their identity, Ms. Couzin-Frankel reports.
The Science article author, Ms. Couzin-Frankel, is a science journalist with no relevant financial conflicts. The RUDY study is funded by the University of Oxford and the U.K. National Institute for Health Research.
FROM SCIENCE
Key clinical point: The RUDY rheumatology registry represents a new data-sharing model based on patient-researcher trust.
Major finding: Openness, full documentation, and reviews are the key to creating a community of trust that obviates the need for cryptographic protection of DNA sequences.
Data source: A review and interview-based summary of new modes of data-sharing in medical research, focusing on the RUDY trial.
Disclosures: Jennifer Couzin-Frankel, a science journalist, has no relevant financial conflicts. The RUDY study is funded by the University of Oxford (England) and the U.K. National Institute for Health Research.