User login
A 57-year-old retired farm worker came into the clinic with itchy pink rings all over his abdomen, legs, and arms. He said that the rash began 13 years ago, soon after he had retired from working in the fields. He said he had been exposed to pesticide chemicals but no other toxins. He’d never received a diagnosis of atopy or “sensitive skin.” He had sun damage on his lower arms, but none on the areas where the rash appeared.
Over the years, he had tried over-the-counter topical steroids, antifungals, and oral antihistamines, all with minimal relief. Furthermore, the lesions did not respond to 2 courses of oral antifungal medications. He said, “some days it itches more than others, but I just deal with it.” The patient was otherwise healthy and on no medications. He had been treated for active tuberculosis in the past but had no symptoms at this time. Out of his frustration, he recently began using paint thinner on the lesions. He thought the paint thinner “dried the rash out” and decreased the itching.
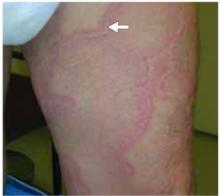
The distribution of the lesions can be seen in Figure 1. Erythematous rings can be seen on the abdomen and legs. These vary in size and shape. Figure 2 is a close-up of the left thigh showing the scale. There was no blanching erythema, no induration, no warmth, and no tenderness to palpation.
FIGURE 1
Rings on the trunk and legs
FIGURE 2
Close-up of thigh
What is the Diagnosis?
Diagnosis: Erythema Annulare Centrifugum
This patient has a rare skin condition called erythema annulare centrifugum (EAC). The primary lesion begins as a group of pink/erythematous papules that spread peripherally as they clear centrally, forming a “trailing scale” (Figure 3) They can enlarge at a rate of 2 to 5 mm/d, producing a plaque or patch of annular, arcuate, or polycyclic shape.1 The margin is indurated and can vary in width from 4 to 6 mm. Vesicles may also be present. Distribution is usually on the thighs and legs but can also appear on the upper extremities (Figure 4), trunk, or face.
Differential diagnosis
Other causes of similar erythematous itchy rings to consider include pityriasis rosea, tinea corporis, psoriasis, nummular eczema, atopic dermatitis, drug reaction, and erythema migrans. The physical exam is the most effective method to differentiate between the above diagnoses—specifically, the distribution and morphology of the lesions. The natural history of the lesions can further narrow the diagnosis.
Pityriasis rosea has erythematous patches distributed on the trunk and extremities. These patches have a distinctive collarette border. The “herald patch,” the first patch to appear, is often oval and about 1 to 3 inches in diameter. Lesions classically follow skin lines to create a “Christmas tree” pattern on the back. Unlike EAC, pityriasis only lasts 6 to 8 weeks.
Tinea corporis (ringworm) is a fungal infection that is often a single scaly annular patch. Like EAC, it can be erythematous and is distributed anywhere on the body. When it presents as multiple lesions, it more closely resembles EAC. Unlike EAC, however, it should show branched hyphae with septae on a KOH prep and fungal culture would show growth of dermatophytes. Furthermore, it responds well to 4 to 6 weeks of antifungal treatment.
Psoriasis may present as plaques on the extensor surfaces of extremities. “Guttate” psoriasis (meaning “like water drops”) appears like small drops on the back and abdomen. Psoriatic plaques do not have central clearing or the trailing scale characteristic of EAC. Psoriatic plaques are often more responsive to steroids than EAC.
FIGURE 3
“Trailing scale”on abdomen
FIGURE 4
Ring on inner arm
Epidemiology and Pathophysiology
EAC is an uncommon inflammatory skin condition of unknown cause. Histologically, it resembles pityriasis rosea, having a superficial perivascular lymphocytic infiltrate with moderate epidermal acanthosis.1,2 The primary lesions spread peripherally and clear centrally at a maximum rate of 2 to 5 mm/d. Pruritus is common but not always present.1
Although the cause and exact pathogenesis are unknown, EAC may in some cases be triggered by drugs, bacterial infections (like tuberculosis), fungi, viruses, parasites, autoimmune diseases, neoplasms, liver diseases, and dysproteinemias.1,3 Other hypotheses suggest that it may be a type IV hypersensitivity reaction.1 The mean duration is 11 months, but it can vary from as little as 4 weeks to 34 years.1
Diagnostic Tests
No specific tests are needed to make the diagnosis of EAC. However, it is a good idea to do a KOH prep to rule out tinea corporis or candidiasis. This technique has a sensitivity of 88% and a specificity of 95% for tinea.4 Thus, a positive result is sufficient for diagnosis. Fungal culture may be useful if you believe that the diagnosis is truly fungal but the KOH result is negative.
If physical exam leads to suspicion of underlying disease, it is important to order the appropriate diagnostic lab tests. A few case reports have described EAC as the presenting sign in patients diagnosed with cancer approximately 2 years later.1
Treatment
It is helpful if you can find an underlying disease process because most cases of EAC clear as the underlying disease is treated. Review the current drugs and consider replacing any drug reported to have been associated with EAC: chloroquine, hydroxychloroquine, estrogen, cimetidine, penicillin, salicylates, piroxicam, hydrochlorothiazide, and amitriptyline.1
If you have minimal suspicion for an underlying disease process and no causative drug agent is found, most cases of EAC require no treatment and resolve spontaneously.1 However, if pruritus is significant, treat symptomatically. One option is to start with a topical high-potency steroid ointment twice daily. Use this regimen for 2 weeks, then assess response. If the response is good, you may continue a mid-potency steroid as needed or pulse-dosing of a high-potency steroid on the weekends. The goal is to minimize the itching while also minimizing the side effects associated with long-term steroid treatment. Treat as needed and taper when possible. Steroids may cause resolution of lesions but do not prevent recurrence.
A second option is topical calcipotriol, a topical vitamin D derivative. A recent case report has shown this to be beneficial,2 but this is an off-label indication. To date, no randomized clinical trials have been done to demonstrate the efficacy of any other treatment.
Patient Outcome
A KOH prep and a fungal culture were obtained to confidently rule out tinea. Both results were negative. We decided to order a chest x-ray because of his past history of active tuberculosis; the test result was negative. To investigate for any underlying diseases, we ordered a complete blood count, chemistry panel, and erythrocyte sedimentation rate, which all showed normal results.
We explained the diagnosis of EAC as a chronic condition of unknown cause. Since steroids did not provide any relief for him in the past, we offered the option of using calcipotriol ointment, even though the evidence is only based on 1 case report.2 He chose to try the calcipotriol. We warned the patient to not use paint thinner because inhalation and skin exposure are harmful. The patient agreed to stop using it.
Corresponding author
Richard P. Usatine, MD, University of Texas Health Science Center at San Antonio, Department of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: [email protected].
1. Willard RJ, Montemarano AD. Erythema annulare centrifugum. eMedicine website. Available at: http://www.emedicine.com/derm/topic131.htm.
2. Gniadecki R. Case report: Calcipotriol for erythema annulare centrifugum. 2002 British Association of Dermatologists.British Journal of Dermatology 2002;146:317-319.
3. Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol 2003;25:451-462.
4. Bergus, GR, Johnson JS. Superficial tinea infections. Am Fam Physician 1993;48:259-268.
A 57-year-old retired farm worker came into the clinic with itchy pink rings all over his abdomen, legs, and arms. He said that the rash began 13 years ago, soon after he had retired from working in the fields. He said he had been exposed to pesticide chemicals but no other toxins. He’d never received a diagnosis of atopy or “sensitive skin.” He had sun damage on his lower arms, but none on the areas where the rash appeared.
Over the years, he had tried over-the-counter topical steroids, antifungals, and oral antihistamines, all with minimal relief. Furthermore, the lesions did not respond to 2 courses of oral antifungal medications. He said, “some days it itches more than others, but I just deal with it.” The patient was otherwise healthy and on no medications. He had been treated for active tuberculosis in the past but had no symptoms at this time. Out of his frustration, he recently began using paint thinner on the lesions. He thought the paint thinner “dried the rash out” and decreased the itching.
The distribution of the lesions can be seen in Figure 1. Erythematous rings can be seen on the abdomen and legs. These vary in size and shape. Figure 2 is a close-up of the left thigh showing the scale. There was no blanching erythema, no induration, no warmth, and no tenderness to palpation.
FIGURE 1
Rings on the trunk and legs
FIGURE 2
Close-up of thigh
What is the Diagnosis?
Diagnosis: Erythema Annulare Centrifugum
This patient has a rare skin condition called erythema annulare centrifugum (EAC). The primary lesion begins as a group of pink/erythematous papules that spread peripherally as they clear centrally, forming a “trailing scale” (Figure 3) They can enlarge at a rate of 2 to 5 mm/d, producing a plaque or patch of annular, arcuate, or polycyclic shape.1 The margin is indurated and can vary in width from 4 to 6 mm. Vesicles may also be present. Distribution is usually on the thighs and legs but can also appear on the upper extremities (Figure 4), trunk, or face.
Differential diagnosis
Other causes of similar erythematous itchy rings to consider include pityriasis rosea, tinea corporis, psoriasis, nummular eczema, atopic dermatitis, drug reaction, and erythema migrans. The physical exam is the most effective method to differentiate between the above diagnoses—specifically, the distribution and morphology of the lesions. The natural history of the lesions can further narrow the diagnosis.
Pityriasis rosea has erythematous patches distributed on the trunk and extremities. These patches have a distinctive collarette border. The “herald patch,” the first patch to appear, is often oval and about 1 to 3 inches in diameter. Lesions classically follow skin lines to create a “Christmas tree” pattern on the back. Unlike EAC, pityriasis only lasts 6 to 8 weeks.
Tinea corporis (ringworm) is a fungal infection that is often a single scaly annular patch. Like EAC, it can be erythematous and is distributed anywhere on the body. When it presents as multiple lesions, it more closely resembles EAC. Unlike EAC, however, it should show branched hyphae with septae on a KOH prep and fungal culture would show growth of dermatophytes. Furthermore, it responds well to 4 to 6 weeks of antifungal treatment.
Psoriasis may present as plaques on the extensor surfaces of extremities. “Guttate” psoriasis (meaning “like water drops”) appears like small drops on the back and abdomen. Psoriatic plaques do not have central clearing or the trailing scale characteristic of EAC. Psoriatic plaques are often more responsive to steroids than EAC.
FIGURE 3
“Trailing scale”on abdomen
FIGURE 4
Ring on inner arm
Epidemiology and Pathophysiology
EAC is an uncommon inflammatory skin condition of unknown cause. Histologically, it resembles pityriasis rosea, having a superficial perivascular lymphocytic infiltrate with moderate epidermal acanthosis.1,2 The primary lesions spread peripherally and clear centrally at a maximum rate of 2 to 5 mm/d. Pruritus is common but not always present.1
Although the cause and exact pathogenesis are unknown, EAC may in some cases be triggered by drugs, bacterial infections (like tuberculosis), fungi, viruses, parasites, autoimmune diseases, neoplasms, liver diseases, and dysproteinemias.1,3 Other hypotheses suggest that it may be a type IV hypersensitivity reaction.1 The mean duration is 11 months, but it can vary from as little as 4 weeks to 34 years.1
Diagnostic Tests
No specific tests are needed to make the diagnosis of EAC. However, it is a good idea to do a KOH prep to rule out tinea corporis or candidiasis. This technique has a sensitivity of 88% and a specificity of 95% for tinea.4 Thus, a positive result is sufficient for diagnosis. Fungal culture may be useful if you believe that the diagnosis is truly fungal but the KOH result is negative.
If physical exam leads to suspicion of underlying disease, it is important to order the appropriate diagnostic lab tests. A few case reports have described EAC as the presenting sign in patients diagnosed with cancer approximately 2 years later.1
Treatment
It is helpful if you can find an underlying disease process because most cases of EAC clear as the underlying disease is treated. Review the current drugs and consider replacing any drug reported to have been associated with EAC: chloroquine, hydroxychloroquine, estrogen, cimetidine, penicillin, salicylates, piroxicam, hydrochlorothiazide, and amitriptyline.1
If you have minimal suspicion for an underlying disease process and no causative drug agent is found, most cases of EAC require no treatment and resolve spontaneously.1 However, if pruritus is significant, treat symptomatically. One option is to start with a topical high-potency steroid ointment twice daily. Use this regimen for 2 weeks, then assess response. If the response is good, you may continue a mid-potency steroid as needed or pulse-dosing of a high-potency steroid on the weekends. The goal is to minimize the itching while also minimizing the side effects associated with long-term steroid treatment. Treat as needed and taper when possible. Steroids may cause resolution of lesions but do not prevent recurrence.
A second option is topical calcipotriol, a topical vitamin D derivative. A recent case report has shown this to be beneficial,2 but this is an off-label indication. To date, no randomized clinical trials have been done to demonstrate the efficacy of any other treatment.
Patient Outcome
A KOH prep and a fungal culture were obtained to confidently rule out tinea. Both results were negative. We decided to order a chest x-ray because of his past history of active tuberculosis; the test result was negative. To investigate for any underlying diseases, we ordered a complete blood count, chemistry panel, and erythrocyte sedimentation rate, which all showed normal results.
We explained the diagnosis of EAC as a chronic condition of unknown cause. Since steroids did not provide any relief for him in the past, we offered the option of using calcipotriol ointment, even though the evidence is only based on 1 case report.2 He chose to try the calcipotriol. We warned the patient to not use paint thinner because inhalation and skin exposure are harmful. The patient agreed to stop using it.
Corresponding author
Richard P. Usatine, MD, University of Texas Health Science Center at San Antonio, Department of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: [email protected].
A 57-year-old retired farm worker came into the clinic with itchy pink rings all over his abdomen, legs, and arms. He said that the rash began 13 years ago, soon after he had retired from working in the fields. He said he had been exposed to pesticide chemicals but no other toxins. He’d never received a diagnosis of atopy or “sensitive skin.” He had sun damage on his lower arms, but none on the areas where the rash appeared.
Over the years, he had tried over-the-counter topical steroids, antifungals, and oral antihistamines, all with minimal relief. Furthermore, the lesions did not respond to 2 courses of oral antifungal medications. He said, “some days it itches more than others, but I just deal with it.” The patient was otherwise healthy and on no medications. He had been treated for active tuberculosis in the past but had no symptoms at this time. Out of his frustration, he recently began using paint thinner on the lesions. He thought the paint thinner “dried the rash out” and decreased the itching.
The distribution of the lesions can be seen in Figure 1. Erythematous rings can be seen on the abdomen and legs. These vary in size and shape. Figure 2 is a close-up of the left thigh showing the scale. There was no blanching erythema, no induration, no warmth, and no tenderness to palpation.
FIGURE 1
Rings on the trunk and legs
FIGURE 2
Close-up of thigh
What is the Diagnosis?
Diagnosis: Erythema Annulare Centrifugum
This patient has a rare skin condition called erythema annulare centrifugum (EAC). The primary lesion begins as a group of pink/erythematous papules that spread peripherally as they clear centrally, forming a “trailing scale” (Figure 3) They can enlarge at a rate of 2 to 5 mm/d, producing a plaque or patch of annular, arcuate, or polycyclic shape.1 The margin is indurated and can vary in width from 4 to 6 mm. Vesicles may also be present. Distribution is usually on the thighs and legs but can also appear on the upper extremities (Figure 4), trunk, or face.
Differential diagnosis
Other causes of similar erythematous itchy rings to consider include pityriasis rosea, tinea corporis, psoriasis, nummular eczema, atopic dermatitis, drug reaction, and erythema migrans. The physical exam is the most effective method to differentiate between the above diagnoses—specifically, the distribution and morphology of the lesions. The natural history of the lesions can further narrow the diagnosis.
Pityriasis rosea has erythematous patches distributed on the trunk and extremities. These patches have a distinctive collarette border. The “herald patch,” the first patch to appear, is often oval and about 1 to 3 inches in diameter. Lesions classically follow skin lines to create a “Christmas tree” pattern on the back. Unlike EAC, pityriasis only lasts 6 to 8 weeks.
Tinea corporis (ringworm) is a fungal infection that is often a single scaly annular patch. Like EAC, it can be erythematous and is distributed anywhere on the body. When it presents as multiple lesions, it more closely resembles EAC. Unlike EAC, however, it should show branched hyphae with septae on a KOH prep and fungal culture would show growth of dermatophytes. Furthermore, it responds well to 4 to 6 weeks of antifungal treatment.
Psoriasis may present as plaques on the extensor surfaces of extremities. “Guttate” psoriasis (meaning “like water drops”) appears like small drops on the back and abdomen. Psoriatic plaques do not have central clearing or the trailing scale characteristic of EAC. Psoriatic plaques are often more responsive to steroids than EAC.
FIGURE 3
“Trailing scale”on abdomen
FIGURE 4
Ring on inner arm
Epidemiology and Pathophysiology
EAC is an uncommon inflammatory skin condition of unknown cause. Histologically, it resembles pityriasis rosea, having a superficial perivascular lymphocytic infiltrate with moderate epidermal acanthosis.1,2 The primary lesions spread peripherally and clear centrally at a maximum rate of 2 to 5 mm/d. Pruritus is common but not always present.1
Although the cause and exact pathogenesis are unknown, EAC may in some cases be triggered by drugs, bacterial infections (like tuberculosis), fungi, viruses, parasites, autoimmune diseases, neoplasms, liver diseases, and dysproteinemias.1,3 Other hypotheses suggest that it may be a type IV hypersensitivity reaction.1 The mean duration is 11 months, but it can vary from as little as 4 weeks to 34 years.1
Diagnostic Tests
No specific tests are needed to make the diagnosis of EAC. However, it is a good idea to do a KOH prep to rule out tinea corporis or candidiasis. This technique has a sensitivity of 88% and a specificity of 95% for tinea.4 Thus, a positive result is sufficient for diagnosis. Fungal culture may be useful if you believe that the diagnosis is truly fungal but the KOH result is negative.
If physical exam leads to suspicion of underlying disease, it is important to order the appropriate diagnostic lab tests. A few case reports have described EAC as the presenting sign in patients diagnosed with cancer approximately 2 years later.1
Treatment
It is helpful if you can find an underlying disease process because most cases of EAC clear as the underlying disease is treated. Review the current drugs and consider replacing any drug reported to have been associated with EAC: chloroquine, hydroxychloroquine, estrogen, cimetidine, penicillin, salicylates, piroxicam, hydrochlorothiazide, and amitriptyline.1
If you have minimal suspicion for an underlying disease process and no causative drug agent is found, most cases of EAC require no treatment and resolve spontaneously.1 However, if pruritus is significant, treat symptomatically. One option is to start with a topical high-potency steroid ointment twice daily. Use this regimen for 2 weeks, then assess response. If the response is good, you may continue a mid-potency steroid as needed or pulse-dosing of a high-potency steroid on the weekends. The goal is to minimize the itching while also minimizing the side effects associated with long-term steroid treatment. Treat as needed and taper when possible. Steroids may cause resolution of lesions but do not prevent recurrence.
A second option is topical calcipotriol, a topical vitamin D derivative. A recent case report has shown this to be beneficial,2 but this is an off-label indication. To date, no randomized clinical trials have been done to demonstrate the efficacy of any other treatment.
Patient Outcome
A KOH prep and a fungal culture were obtained to confidently rule out tinea. Both results were negative. We decided to order a chest x-ray because of his past history of active tuberculosis; the test result was negative. To investigate for any underlying diseases, we ordered a complete blood count, chemistry panel, and erythrocyte sedimentation rate, which all showed normal results.
We explained the diagnosis of EAC as a chronic condition of unknown cause. Since steroids did not provide any relief for him in the past, we offered the option of using calcipotriol ointment, even though the evidence is only based on 1 case report.2 He chose to try the calcipotriol. We warned the patient to not use paint thinner because inhalation and skin exposure are harmful. The patient agreed to stop using it.
Corresponding author
Richard P. Usatine, MD, University of Texas Health Science Center at San Antonio, Department of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: [email protected].
1. Willard RJ, Montemarano AD. Erythema annulare centrifugum. eMedicine website. Available at: http://www.emedicine.com/derm/topic131.htm.
2. Gniadecki R. Case report: Calcipotriol for erythema annulare centrifugum. 2002 British Association of Dermatologists.British Journal of Dermatology 2002;146:317-319.
3. Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol 2003;25:451-462.
4. Bergus, GR, Johnson JS. Superficial tinea infections. Am Fam Physician 1993;48:259-268.
1. Willard RJ, Montemarano AD. Erythema annulare centrifugum. eMedicine website. Available at: http://www.emedicine.com/derm/topic131.htm.
2. Gniadecki R. Case report: Calcipotriol for erythema annulare centrifugum. 2002 British Association of Dermatologists.British Journal of Dermatology 2002;146:317-319.
3. Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol 2003;25:451-462.
4. Bergus, GR, Johnson JS. Superficial tinea infections. Am Fam Physician 1993;48:259-268.