User login
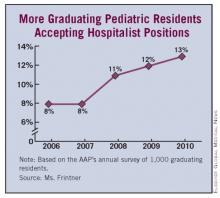
DENVER – Last year, roughly one in eight graduating pediatric residents accepted a hospitalist position.
These new pediatricians aren’t merely using the job as a stepping stone, either. Fully 84% of those who took a hospitalist position straight out of residency in 2010 say that being a hospitalist is their long-term career goal, Mary Pat Frintner said at the annual meeting of the Pediatric Academic Societies.
She presented highlights from the past 5 years of the American Academy of Pediatrics annual survey of graduating residents, administered to a random sample of 1,000 new graduates each year.
The proportion of graduating pediatric residents accepting a hospitalist position rose steadily from 8% in 2006 to 13% last year. Few of them reported any substantial difficulty in their job search: 45% indicated they experienced no difficulty at all in landing their position, and only 14% reported moderate and 3% considerable difficulty, according to Ms. Frintner of the department of research at AAP headquarters in Elk Grove Village, Ill.
Fifty-eight percent of the new pediatric hospitalists took a position in the same city as their residency. Two-thirds stayed in the same state.
The average full-time starting salary over the 5-year study period for residents taking a hospitalist position was $122,000 per year, with no significant increase over the years. Fifteen percent of 2010 grads who took a hospitalist position accepted a part-time, reduced-hours position.
Fifty-eight percent of the new pediatric hospitalists indicated that they will be working in a medical school or teaching hospital, and 36% in a community hospital. Community hospitals paid better.
Significant predictors of acceptance of a hospitalist position were having graduated from a residency training program with 60 or more residents, an educational debt of $120,000 or more, age less than 31 years, being nonmarried, and having gone to a U.S. medical school. Each of these predictors was only modest in power. Neither gender nor having children was significantly associated with taking a hospitalist position.
Across the full 5-year study span, 73% of those who took a pediatric hospitalist position upon graduation had hospitalist practice as their long-term goal. Twelve percent were aimed towards subspecialty practice, 10% had primary care pediatrics as their career goal, and 4% looked to a future involving a combined primary care/subspecialty practice.
Audience members commented that this AAP-funded study provides persuasive evidence in support of recognizing hospitalist practice as a pediatric subspecialty.
"With 13% of residents in 2010 going into it, if it were to be a pediatric subspecialty it would be the biggest subspecialty," one physician observed.
Of the roughly 30,000 hospitalists practicing today, only about 10% are believed to be pediatricians, Ms. Frintner noted.
Medical knowledge is too vast to be mastered by an individual. The location in which medical care is delivered, rather than the organ system involved, has become a common paradigm for delineating subspecialization.
The PICU, NICU and ED have all become boarded pediatric subspecialties. Pediatric inpatient medicine continues to evolve and has yet to determine whether to adopt a traditional board format (3-year fellowship with a research requirement), follow adult hospitalists with a focused practice certification (after 3 years of real-world and real-income experience), or to become a separate track within a 3-year pediatric residency program. As an already large and the fastest-growing subspecialty, hospitalists may break those molds and establish their own accreditation format. Committees are examining these options, each sparking debate at the annual Pediatric Hospital Medicine meeting.
Requiring less start up time than an outpatient practice, for the past decade hospital positions have been attractive to those seeking a temporary position after residency. But as these numbers show, the vast and growing majority of hospitalists are adopting inpatient medicine as an exciting career path. As a lifestyle choice, it is also more amenable to part-time positions, shift work such as nocturnists, and extended leaves of absence.
Intellectually, hospital medicine demands different knowledge and skills than outpatient medicine. These include the treatment of diseases in seriously ill children, coordinating care for technology-dependent children, and providing procedural sedation.
More recently, the emphasis of hospital medicine has focused on systemic issues, such as reducing errors and other quality improvement programs. In the near future, providing cost-effective care will gain importance.
KEVIN POWELL, M.D., PH.D., is associate professor of pediatrics at St. Louis University and a pediatric hospitalist at SSM Cardinal Glennon Children’s Medical Center in St. Louis. He has no relevant disclosures nor conflicts of interest to report.
Medical knowledge is too vast to be mastered by an individual. The location in which medical care is delivered, rather than the organ system involved, has become a common paradigm for delineating subspecialization.
The PICU, NICU and ED have all become boarded pediatric subspecialties. Pediatric inpatient medicine continues to evolve and has yet to determine whether to adopt a traditional board format (3-year fellowship with a research requirement), follow adult hospitalists with a focused practice certification (after 3 years of real-world and real-income experience), or to become a separate track within a 3-year pediatric residency program. As an already large and the fastest-growing subspecialty, hospitalists may break those molds and establish their own accreditation format. Committees are examining these options, each sparking debate at the annual Pediatric Hospital Medicine meeting.
Requiring less start up time than an outpatient practice, for the past decade hospital positions have been attractive to those seeking a temporary position after residency. But as these numbers show, the vast and growing majority of hospitalists are adopting inpatient medicine as an exciting career path. As a lifestyle choice, it is also more amenable to part-time positions, shift work such as nocturnists, and extended leaves of absence.
Intellectually, hospital medicine demands different knowledge and skills than outpatient medicine. These include the treatment of diseases in seriously ill children, coordinating care for technology-dependent children, and providing procedural sedation.
More recently, the emphasis of hospital medicine has focused on systemic issues, such as reducing errors and other quality improvement programs. In the near future, providing cost-effective care will gain importance.
KEVIN POWELL, M.D., PH.D., is associate professor of pediatrics at St. Louis University and a pediatric hospitalist at SSM Cardinal Glennon Children’s Medical Center in St. Louis. He has no relevant disclosures nor conflicts of interest to report.
Medical knowledge is too vast to be mastered by an individual. The location in which medical care is delivered, rather than the organ system involved, has become a common paradigm for delineating subspecialization.
The PICU, NICU and ED have all become boarded pediatric subspecialties. Pediatric inpatient medicine continues to evolve and has yet to determine whether to adopt a traditional board format (3-year fellowship with a research requirement), follow adult hospitalists with a focused practice certification (after 3 years of real-world and real-income experience), or to become a separate track within a 3-year pediatric residency program. As an already large and the fastest-growing subspecialty, hospitalists may break those molds and establish their own accreditation format. Committees are examining these options, each sparking debate at the annual Pediatric Hospital Medicine meeting.
Requiring less start up time than an outpatient practice, for the past decade hospital positions have been attractive to those seeking a temporary position after residency. But as these numbers show, the vast and growing majority of hospitalists are adopting inpatient medicine as an exciting career path. As a lifestyle choice, it is also more amenable to part-time positions, shift work such as nocturnists, and extended leaves of absence.
Intellectually, hospital medicine demands different knowledge and skills than outpatient medicine. These include the treatment of diseases in seriously ill children, coordinating care for technology-dependent children, and providing procedural sedation.
More recently, the emphasis of hospital medicine has focused on systemic issues, such as reducing errors and other quality improvement programs. In the near future, providing cost-effective care will gain importance.
KEVIN POWELL, M.D., PH.D., is associate professor of pediatrics at St. Louis University and a pediatric hospitalist at SSM Cardinal Glennon Children’s Medical Center in St. Louis. He has no relevant disclosures nor conflicts of interest to report.
DENVER – Last year, roughly one in eight graduating pediatric residents accepted a hospitalist position.
These new pediatricians aren’t merely using the job as a stepping stone, either. Fully 84% of those who took a hospitalist position straight out of residency in 2010 say that being a hospitalist is their long-term career goal, Mary Pat Frintner said at the annual meeting of the Pediatric Academic Societies.
She presented highlights from the past 5 years of the American Academy of Pediatrics annual survey of graduating residents, administered to a random sample of 1,000 new graduates each year.
The proportion of graduating pediatric residents accepting a hospitalist position rose steadily from 8% in 2006 to 13% last year. Few of them reported any substantial difficulty in their job search: 45% indicated they experienced no difficulty at all in landing their position, and only 14% reported moderate and 3% considerable difficulty, according to Ms. Frintner of the department of research at AAP headquarters in Elk Grove Village, Ill.
Fifty-eight percent of the new pediatric hospitalists took a position in the same city as their residency. Two-thirds stayed in the same state.
The average full-time starting salary over the 5-year study period for residents taking a hospitalist position was $122,000 per year, with no significant increase over the years. Fifteen percent of 2010 grads who took a hospitalist position accepted a part-time, reduced-hours position.
Fifty-eight percent of the new pediatric hospitalists indicated that they will be working in a medical school or teaching hospital, and 36% in a community hospital. Community hospitals paid better.
Significant predictors of acceptance of a hospitalist position were having graduated from a residency training program with 60 or more residents, an educational debt of $120,000 or more, age less than 31 years, being nonmarried, and having gone to a U.S. medical school. Each of these predictors was only modest in power. Neither gender nor having children was significantly associated with taking a hospitalist position.
Across the full 5-year study span, 73% of those who took a pediatric hospitalist position upon graduation had hospitalist practice as their long-term goal. Twelve percent were aimed towards subspecialty practice, 10% had primary care pediatrics as their career goal, and 4% looked to a future involving a combined primary care/subspecialty practice.
Audience members commented that this AAP-funded study provides persuasive evidence in support of recognizing hospitalist practice as a pediatric subspecialty.
"With 13% of residents in 2010 going into it, if it were to be a pediatric subspecialty it would be the biggest subspecialty," one physician observed.
Of the roughly 30,000 hospitalists practicing today, only about 10% are believed to be pediatricians, Ms. Frintner noted.
DENVER – Last year, roughly one in eight graduating pediatric residents accepted a hospitalist position.
These new pediatricians aren’t merely using the job as a stepping stone, either. Fully 84% of those who took a hospitalist position straight out of residency in 2010 say that being a hospitalist is their long-term career goal, Mary Pat Frintner said at the annual meeting of the Pediatric Academic Societies.
She presented highlights from the past 5 years of the American Academy of Pediatrics annual survey of graduating residents, administered to a random sample of 1,000 new graduates each year.
The proportion of graduating pediatric residents accepting a hospitalist position rose steadily from 8% in 2006 to 13% last year. Few of them reported any substantial difficulty in their job search: 45% indicated they experienced no difficulty at all in landing their position, and only 14% reported moderate and 3% considerable difficulty, according to Ms. Frintner of the department of research at AAP headquarters in Elk Grove Village, Ill.
Fifty-eight percent of the new pediatric hospitalists took a position in the same city as their residency. Two-thirds stayed in the same state.
The average full-time starting salary over the 5-year study period for residents taking a hospitalist position was $122,000 per year, with no significant increase over the years. Fifteen percent of 2010 grads who took a hospitalist position accepted a part-time, reduced-hours position.
Fifty-eight percent of the new pediatric hospitalists indicated that they will be working in a medical school or teaching hospital, and 36% in a community hospital. Community hospitals paid better.
Significant predictors of acceptance of a hospitalist position were having graduated from a residency training program with 60 or more residents, an educational debt of $120,000 or more, age less than 31 years, being nonmarried, and having gone to a U.S. medical school. Each of these predictors was only modest in power. Neither gender nor having children was significantly associated with taking a hospitalist position.
Across the full 5-year study span, 73% of those who took a pediatric hospitalist position upon graduation had hospitalist practice as their long-term goal. Twelve percent were aimed towards subspecialty practice, 10% had primary care pediatrics as their career goal, and 4% looked to a future involving a combined primary care/subspecialty practice.
Audience members commented that this AAP-funded study provides persuasive evidence in support of recognizing hospitalist practice as a pediatric subspecialty.
"With 13% of residents in 2010 going into it, if it were to be a pediatric subspecialty it would be the biggest subspecialty," one physician observed.
Of the roughly 30,000 hospitalists practicing today, only about 10% are believed to be pediatricians, Ms. Frintner noted.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES