User login
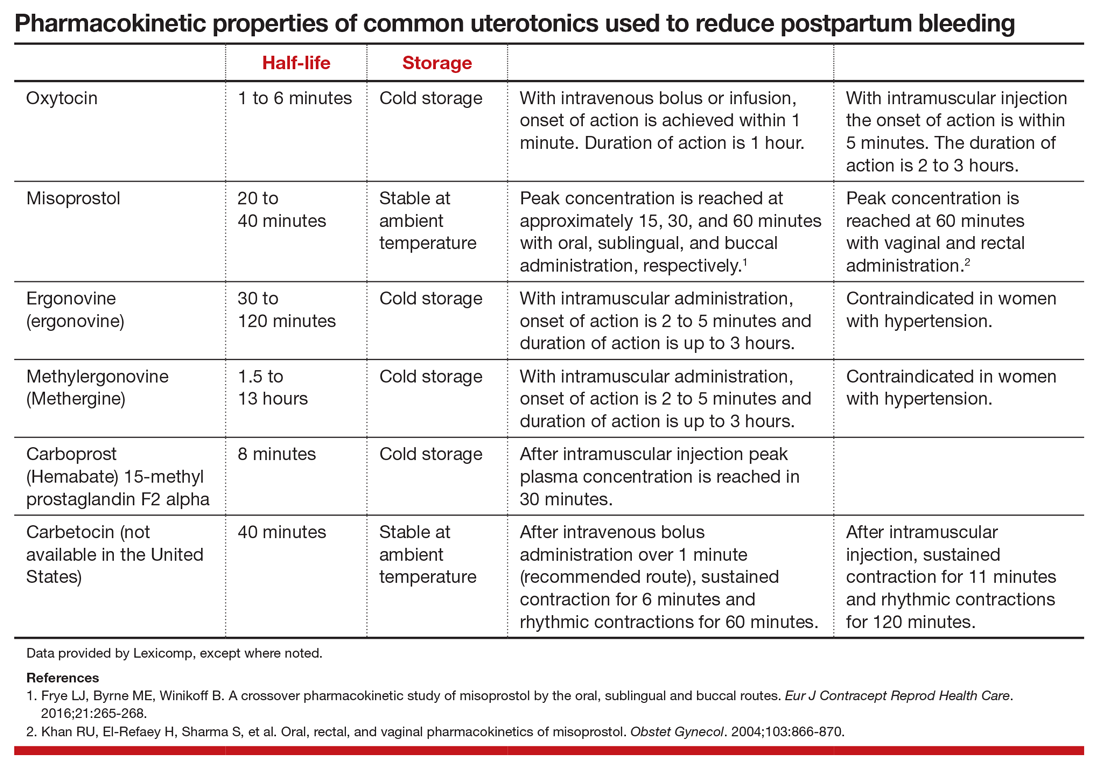
Excessive postpartum bleeding is a major cause of maternal morbidity and mortality. Worldwide, obstetric hemorrhage is the most common cause of maternal death.1,2 Medications reported to reduce postpartum bleeding include oxytocin, misoprostol, ergonovine, methylergonovine, carboprost, and tranexamic acid. A recent Cochrane network meta-analysis of 196 trials, including 135,559 women, distilled in 1,361 pages of analysis, reported on the medications associated with the greatest reduction in postpartum bleeding.3 Surprisingly, for preventing blood loss ≥ 500 mL, misoprostol plus oxytocin and ergonovine plus oxytocin were the highest ranked interventions. This evidence is summarized here.
Misoprostol plus oxytocin
After newborn delivery, active management of the third stage of labor, including uterotonic administration, is strongly recommended because it will reduce postpartum blood loss, decreasing the rate of postpartum hemorrhage (PPH).4 Both oxytocin and misoprostol are effective uterotonics. However, the combination of oxytocin plus misoprostol appears to be more effective than oxytocin alone in reducing the frequency of postpartum blood loss greater than 500 mL.3 To understand the clinical efficacy and adverse effects (AEs) of combined oxytocin plus misoprostol a meta-analysis was performed for both vaginal and cesarean deliveries (CDs).
Efficacy and AEs during vaginal delivery. In the meta-analysis, about 6,000 vaginal deliveries were analyzed, with no significant differences for misoprostol plus oxytocin versus oxytocin alone found for the following outcomes: maternal death, intensive care unit admissions, and rate of blood loss ≥ 1,000 mL (1.7% for both uterotonics vs 2.2% for oxytocin alone).3 Misoprostol plus oxytocin was significantly superior to oxytocin alone for the following outcomes: reduced risk of blood transfusion (0.95% vs 2.5%), reduced risk of blood loss ≥ 500 mL (5.9% vs 8.0%), reduced risk of requiring an additional uterotonic (3.6% vs 5.8%), and a smaller decrease in hemoglobin concentration from pre- to postdelivery (-0.89 g/L).3
In my opinion, the difference in hemoglobin concentration, although statistically significant, is not of clinical significance. However, compared with oxytocin alone, misoprostol plus oxytocin caused significantly more nausea (2.4% vs 0.66%), vomiting (3.1% vs 0.86%), and fever (21% vs 3.9%).3 A weakness of this meta-analysis is that the trials used a wide range of misoprostol dosages (200 to 600 µg) and multiple routes of administration, including sublingual (under the tongue), buccal, and rectal. This makes it impossible to identify a best misoprostol dosage and administration route.
Efficacy and AEs during CD. In the same meta-analysis about 2,000 CDs were analyzed, with no significant difference for misoprostol plus oxytocin versus oxytocin alone for the following outcomes: maternal death, intensive care unit admissions, and PPH ≥ 1,000 mL blood loss (6.2% vs 6.5%).3 Misoprostol plus oxytocin was significantly superior to oxytocin alone for the following outcomes: reduced risk of blood transfusion (2.6% vs 5.4%), reduced risk of blood loss ≥ 500 mL (32% vs 47%), reduced risk of requiring an additional uterotonic (14% vs 28%), and a smaller decrease in hemoglobin concentration from before to after delivery (-4.0 g/L).3 In my opinion, the statistically significant difference in hemoglobin concentration is not clinically significant. However, compared with oxytocin alone, misoprostol plus oxytocin caused significantly more nausea (12% vs 6.1%), vomiting (8.1% vs 5.4%), shivering (13% vs 7%), and fever (7.7% vs 4.0%).3
Continue to: Ergonovine plus oxytocin...
Ergonovine plus oxytocin
Ergonovine is an ergot derivative that causes uterine contractions and has been shown to effectively reduce blood loss at delivery. In the United States a methyl-derivative of ergonovine, methylergonovine, is widely available. In a meta-analysis with mostly vaginal deliveries, there were no significant differences for ergonovine plus oxytocin versus oxytocin alone for the following outcomes: death, intensive care unit admission, rate of blood loss ≥ 1,000 mL(2.0% vs 2.7%), blood transfusion, administration of an additional uterotonic, change in hemoglobin from pre- to postdelivery, nausea, hypertension, shivering, and fever.3 However, ergonovine plus oxytocin, compared with oxytocin alone, resulted in a significantly reduced rate of blood loss ≥ 500 mL (8.3% vs 10.2%) and an increased rate of vomiting (8.1% vs 1.6%).3 In these trials women with a blood pressure ≥ 150/100 mm Hg were generally excluded from receiving ergonovine because of its hypertensive effect.
Clinical practice options
Given the Cochrane meta-analysis results, ObGyns have two approaches for optimizing PPH reduction.
Option 1: Use a single uterotonic to reduce postpartum blood loss. If excess bleeding occurs, rapidly administer a second uterotonic agent. Currently, monotherapy with intravenous or intramuscular oxytocin is the standard for reducing postpartum blood loss.5,6 Advantages of this approach compared with dual agent therapy include simplification of care and minimization of AEs. However, oxytocin monotherapy for minimizing postpartum bleeding may be suboptimal. In the largest trial ever performed (involving 29,645 women) when oxytocin was administered postpartum, the rates of estimated blood loss ≥ 500 mL and ≥ 1,000 mL were 9.1% and 1.45%, respectively.5 Is 9% an optimal rate for blood loss ≥ 500 mL following a vaginal delivery? Or should we try to achieve a lower rate?
Given the “high” rate of blood loss ≥ 500 mL with oxytocin alone, it is important for clinicians using the one-uterotonic approach to promptly recognize patients who have excessive bleeding and transition rapidly from prevention to treatment. When PPH cases are reviewed, a common finding is that the clinicians did not timely recognize excess bleeding, delaying transition to treatment with additional uterotonics and other interventions. When routinely using oxytocin monotherapy, lowering the threshold for administering a second uterotonic (methylergonovine, carboprost, misoprostol, or tranexamic acid) may help decrease the frequency of excess postpartum blood loss.
Option 2: Administer two uterotonics to reduce postpartum blood loss at all deliveries. Given the “high” rate of excess postpartum blood loss with oxytocin monotherapy, an alternative is to administer two uterotonics at all births or at births with a high risk of excess blood loss. As discussed, administering two uterotonics, oxytocin plus misoprostol or oxytocin plus ergonovine, has been reported to be more effective than oxytocin alone for reducing postpartum bleeding ≥ 500 mL.3 In the Cochrane meta-analysis, per 1,000 women given oxytocin following a vaginal birth, 122 would have blood loss ≥ 500 mL, compared with 85 given oxytocin plus misoprostol or oxytocin plus ergonovine.3
Misoprostol is administered sublingually, buccally, or rectally, and methylergonovine is administered by intramuscular injection. Although dual uterotonic therapy is more effective than monotherapy, dual therapy is associated with more AEs. As noted, compared with oxytocin monotherapy, the combination of oxytocin plus misoprostol is associated with more nausea, vomiting, shivering, and fever. Oxytocin plus ergonovine is associated with a higher rate of vomiting than oxytocin monotherapy. In my practice I prefer using intramuscular methylergonovine as the second agent to avoid the high rate of fever associated with misoprostol.
For dual agent therapy, one approach is to administer misoprostol 200 µg or 400 µg through the buccal7,8 or sublingual9,10 routes. Higher dosages of misoprostol (600 µg to 800 µg) have been used11,12 but are likely associated with higher rates of nausea, vomiting,shivering, and fever than the lower dosages. Methylergonovine 0.2 mg is administered intramuscularly.
Continue to: The bottom line...
The bottom line
PPH is a major cause of maternal morbidity, and in low-resource settings, mortality. Oxytocin is the standard for reducing postpartum blood loss, but rates of blood loss ≥ 500 mL are high following this monotherapy. To reduce postpartum blood loss beyond what is possible with oxytocin alone, clinicians can more rapidly transition to administering a second uterotonic when they suspect blood loss is becoming excessive or they can use two uterotonic agents with all births or in those at high risk for excess bleeding. If blood loss does become excessive, clinicians need to pivot rapidly from prevention with oxytocin to treatment with our entire therapeutic armamentarium.
- Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2:e323-e333.
- Slomski A. Why do hundreds of US women die annually in childbirth? JAMA. 2019;321:1239-1241.
- Gallos ID, Papadopoulou A, Man R, et al. Uterotonic agents for preventing postpartum haemorrhage: a network meta-analysis. Cochrane Database Syst Rev. 2018;12:CD011689.
- American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 183: postpartum hemorrhage. Obstet Gynecol. 2017;130:e168-e186.
- Widmer M, Piaggio G, Nguyen TM, et al; WHO Champion Trial Group. Heat-stable carbetocin versus oxytocin to prevent hemorrhage after vaginal birth. N Engl J Med. 2018;379:743-752.
- Adnan N, Conlan-Trant R, McCormick C, et al. Intramuscular versus intravenous oxytocin to prevent postpartum haemorrhage at vaginal delivery: randomised controlled trial. BMJ. 2018;362:k3546.
- Hamm J, Russell Z, Botha T, et al. Buccal misoprostol to prevent hemorrhage at cesarean delivery: a randomized study. Am J Obstet Gynecol. 2005;192:1404-1406.
- Bhullar A, Carlan SJ, Hamm J, et al. Buccal misoprostol to decrease blood loss after vaginal delivery: a randomized trial. Obstet Gynecol. 2004;104:1282-1288.
- Hofmeyr GJ, Fawole B, Mugerwa K, et al. Administration of 400 µg of misoprostol to augment routine active management of the third stage of labor. Int J Gynaecol Obstet. 2011;112:98-102.
- Chaudhuri P, Majumdar A. A randomized trial of sublingual misoprostol to augment routine third-stage management among women at risk of postpartum hemorrhage. Int J Gynaecol Obstet. 2016;132:191-195.
- Winikoff B, Dabash R, Durocher J, et al. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women not exposed to oxytocin during labor: a double-blind, randomised, non-inferiority trial. Lancet. 2010;375:210-216.
- Blum J, Winikoff B, Raghavan S, et al. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women receiving prophylactic oxytocin: a double-blind, randomised, non-inferiority trial. Lancet. 2010;375:217-223.
Excessive postpartum bleeding is a major cause of maternal morbidity and mortality. Worldwide, obstetric hemorrhage is the most common cause of maternal death.1,2 Medications reported to reduce postpartum bleeding include oxytocin, misoprostol, ergonovine, methylergonovine, carboprost, and tranexamic acid. A recent Cochrane network meta-analysis of 196 trials, including 135,559 women, distilled in 1,361 pages of analysis, reported on the medications associated with the greatest reduction in postpartum bleeding.3 Surprisingly, for preventing blood loss ≥ 500 mL, misoprostol plus oxytocin and ergonovine plus oxytocin were the highest ranked interventions. This evidence is summarized here.
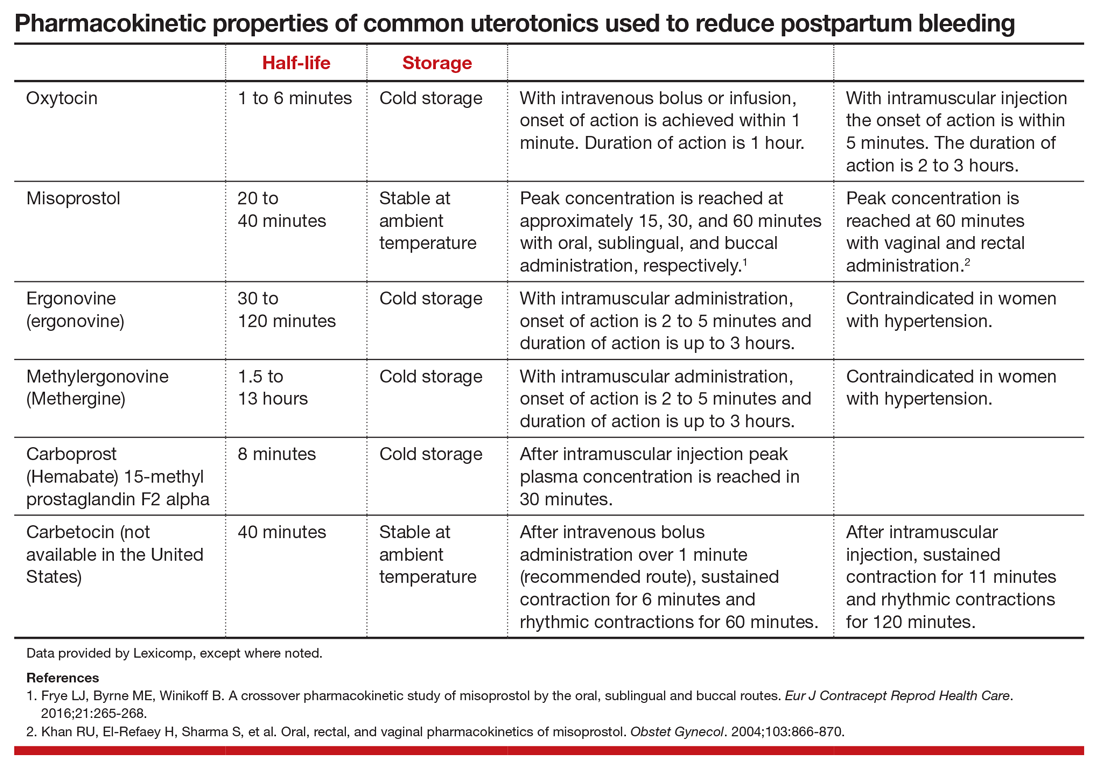
Misoprostol plus oxytocin
After newborn delivery, active management of the third stage of labor, including uterotonic administration, is strongly recommended because it will reduce postpartum blood loss, decreasing the rate of postpartum hemorrhage (PPH).4 Both oxytocin and misoprostol are effective uterotonics. However, the combination of oxytocin plus misoprostol appears to be more effective than oxytocin alone in reducing the frequency of postpartum blood loss greater than 500 mL.3 To understand the clinical efficacy and adverse effects (AEs) of combined oxytocin plus misoprostol a meta-analysis was performed for both vaginal and cesarean deliveries (CDs).
Efficacy and AEs during vaginal delivery. In the meta-analysis, about 6,000 vaginal deliveries were analyzed, with no significant differences for misoprostol plus oxytocin versus oxytocin alone found for the following outcomes: maternal death, intensive care unit admissions, and rate of blood loss ≥ 1,000 mL (1.7% for both uterotonics vs 2.2% for oxytocin alone).3 Misoprostol plus oxytocin was significantly superior to oxytocin alone for the following outcomes: reduced risk of blood transfusion (0.95% vs 2.5%), reduced risk of blood loss ≥ 500 mL (5.9% vs 8.0%), reduced risk of requiring an additional uterotonic (3.6% vs 5.8%), and a smaller decrease in hemoglobin concentration from pre- to postdelivery (-0.89 g/L).3
In my opinion, the difference in hemoglobin concentration, although statistically significant, is not of clinical significance. However, compared with oxytocin alone, misoprostol plus oxytocin caused significantly more nausea (2.4% vs 0.66%), vomiting (3.1% vs 0.86%), and fever (21% vs 3.9%).3 A weakness of this meta-analysis is that the trials used a wide range of misoprostol dosages (200 to 600 µg) and multiple routes of administration, including sublingual (under the tongue), buccal, and rectal. This makes it impossible to identify a best misoprostol dosage and administration route.
Efficacy and AEs during CD. In the same meta-analysis about 2,000 CDs were analyzed, with no significant difference for misoprostol plus oxytocin versus oxytocin alone for the following outcomes: maternal death, intensive care unit admissions, and PPH ≥ 1,000 mL blood loss (6.2% vs 6.5%).3 Misoprostol plus oxytocin was significantly superior to oxytocin alone for the following outcomes: reduced risk of blood transfusion (2.6% vs 5.4%), reduced risk of blood loss ≥ 500 mL (32% vs 47%), reduced risk of requiring an additional uterotonic (14% vs 28%), and a smaller decrease in hemoglobin concentration from before to after delivery (-4.0 g/L).3 In my opinion, the statistically significant difference in hemoglobin concentration is not clinically significant. However, compared with oxytocin alone, misoprostol plus oxytocin caused significantly more nausea (12% vs 6.1%), vomiting (8.1% vs 5.4%), shivering (13% vs 7%), and fever (7.7% vs 4.0%).3
Continue to: Ergonovine plus oxytocin...
Ergonovine plus oxytocin
Ergonovine is an ergot derivative that causes uterine contractions and has been shown to effectively reduce blood loss at delivery. In the United States a methyl-derivative of ergonovine, methylergonovine, is widely available. In a meta-analysis with mostly vaginal deliveries, there were no significant differences for ergonovine plus oxytocin versus oxytocin alone for the following outcomes: death, intensive care unit admission, rate of blood loss ≥ 1,000 mL(2.0% vs 2.7%), blood transfusion, administration of an additional uterotonic, change in hemoglobin from pre- to postdelivery, nausea, hypertension, shivering, and fever.3 However, ergonovine plus oxytocin, compared with oxytocin alone, resulted in a significantly reduced rate of blood loss ≥ 500 mL (8.3% vs 10.2%) and an increased rate of vomiting (8.1% vs 1.6%).3 In these trials women with a blood pressure ≥ 150/100 mm Hg were generally excluded from receiving ergonovine because of its hypertensive effect.
Clinical practice options
Given the Cochrane meta-analysis results, ObGyns have two approaches for optimizing PPH reduction.
Option 1: Use a single uterotonic to reduce postpartum blood loss. If excess bleeding occurs, rapidly administer a second uterotonic agent. Currently, monotherapy with intravenous or intramuscular oxytocin is the standard for reducing postpartum blood loss.5,6 Advantages of this approach compared with dual agent therapy include simplification of care and minimization of AEs. However, oxytocin monotherapy for minimizing postpartum bleeding may be suboptimal. In the largest trial ever performed (involving 29,645 women) when oxytocin was administered postpartum, the rates of estimated blood loss ≥ 500 mL and ≥ 1,000 mL were 9.1% and 1.45%, respectively.5 Is 9% an optimal rate for blood loss ≥ 500 mL following a vaginal delivery? Or should we try to achieve a lower rate?
Given the “high” rate of blood loss ≥ 500 mL with oxytocin alone, it is important for clinicians using the one-uterotonic approach to promptly recognize patients who have excessive bleeding and transition rapidly from prevention to treatment. When PPH cases are reviewed, a common finding is that the clinicians did not timely recognize excess bleeding, delaying transition to treatment with additional uterotonics and other interventions. When routinely using oxytocin monotherapy, lowering the threshold for administering a second uterotonic (methylergonovine, carboprost, misoprostol, or tranexamic acid) may help decrease the frequency of excess postpartum blood loss.
Option 2: Administer two uterotonics to reduce postpartum blood loss at all deliveries. Given the “high” rate of excess postpartum blood loss with oxytocin monotherapy, an alternative is to administer two uterotonics at all births or at births with a high risk of excess blood loss. As discussed, administering two uterotonics, oxytocin plus misoprostol or oxytocin plus ergonovine, has been reported to be more effective than oxytocin alone for reducing postpartum bleeding ≥ 500 mL.3 In the Cochrane meta-analysis, per 1,000 women given oxytocin following a vaginal birth, 122 would have blood loss ≥ 500 mL, compared with 85 given oxytocin plus misoprostol or oxytocin plus ergonovine.3
Misoprostol is administered sublingually, buccally, or rectally, and methylergonovine is administered by intramuscular injection. Although dual uterotonic therapy is more effective than monotherapy, dual therapy is associated with more AEs. As noted, compared with oxytocin monotherapy, the combination of oxytocin plus misoprostol is associated with more nausea, vomiting, shivering, and fever. Oxytocin plus ergonovine is associated with a higher rate of vomiting than oxytocin monotherapy. In my practice I prefer using intramuscular methylergonovine as the second agent to avoid the high rate of fever associated with misoprostol.
For dual agent therapy, one approach is to administer misoprostol 200 µg or 400 µg through the buccal7,8 or sublingual9,10 routes. Higher dosages of misoprostol (600 µg to 800 µg) have been used11,12 but are likely associated with higher rates of nausea, vomiting,shivering, and fever than the lower dosages. Methylergonovine 0.2 mg is administered intramuscularly.
Continue to: The bottom line...
The bottom line
PPH is a major cause of maternal morbidity, and in low-resource settings, mortality. Oxytocin is the standard for reducing postpartum blood loss, but rates of blood loss ≥ 500 mL are high following this monotherapy. To reduce postpartum blood loss beyond what is possible with oxytocin alone, clinicians can more rapidly transition to administering a second uterotonic when they suspect blood loss is becoming excessive or they can use two uterotonic agents with all births or in those at high risk for excess bleeding. If blood loss does become excessive, clinicians need to pivot rapidly from prevention with oxytocin to treatment with our entire therapeutic armamentarium.
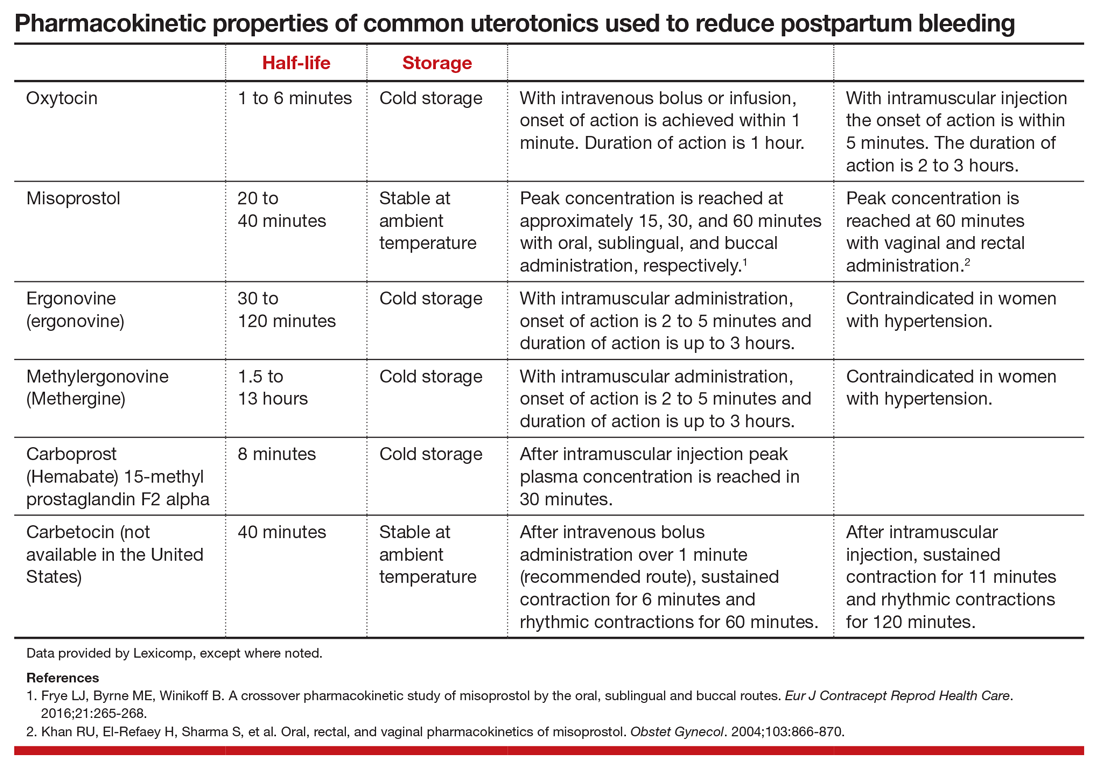
Excessive postpartum bleeding is a major cause of maternal morbidity and mortality. Worldwide, obstetric hemorrhage is the most common cause of maternal death.1,2 Medications reported to reduce postpartum bleeding include oxytocin, misoprostol, ergonovine, methylergonovine, carboprost, and tranexamic acid. A recent Cochrane network meta-analysis of 196 trials, including 135,559 women, distilled in 1,361 pages of analysis, reported on the medications associated with the greatest reduction in postpartum bleeding.3 Surprisingly, for preventing blood loss ≥ 500 mL, misoprostol plus oxytocin and ergonovine plus oxytocin were the highest ranked interventions. This evidence is summarized here.
Misoprostol plus oxytocin
After newborn delivery, active management of the third stage of labor, including uterotonic administration, is strongly recommended because it will reduce postpartum blood loss, decreasing the rate of postpartum hemorrhage (PPH).4 Both oxytocin and misoprostol are effective uterotonics. However, the combination of oxytocin plus misoprostol appears to be more effective than oxytocin alone in reducing the frequency of postpartum blood loss greater than 500 mL.3 To understand the clinical efficacy and adverse effects (AEs) of combined oxytocin plus misoprostol a meta-analysis was performed for both vaginal and cesarean deliveries (CDs).
Efficacy and AEs during vaginal delivery. In the meta-analysis, about 6,000 vaginal deliveries were analyzed, with no significant differences for misoprostol plus oxytocin versus oxytocin alone found for the following outcomes: maternal death, intensive care unit admissions, and rate of blood loss ≥ 1,000 mL (1.7% for both uterotonics vs 2.2% for oxytocin alone).3 Misoprostol plus oxytocin was significantly superior to oxytocin alone for the following outcomes: reduced risk of blood transfusion (0.95% vs 2.5%), reduced risk of blood loss ≥ 500 mL (5.9% vs 8.0%), reduced risk of requiring an additional uterotonic (3.6% vs 5.8%), and a smaller decrease in hemoglobin concentration from pre- to postdelivery (-0.89 g/L).3
In my opinion, the difference in hemoglobin concentration, although statistically significant, is not of clinical significance. However, compared with oxytocin alone, misoprostol plus oxytocin caused significantly more nausea (2.4% vs 0.66%), vomiting (3.1% vs 0.86%), and fever (21% vs 3.9%).3 A weakness of this meta-analysis is that the trials used a wide range of misoprostol dosages (200 to 600 µg) and multiple routes of administration, including sublingual (under the tongue), buccal, and rectal. This makes it impossible to identify a best misoprostol dosage and administration route.
Efficacy and AEs during CD. In the same meta-analysis about 2,000 CDs were analyzed, with no significant difference for misoprostol plus oxytocin versus oxytocin alone for the following outcomes: maternal death, intensive care unit admissions, and PPH ≥ 1,000 mL blood loss (6.2% vs 6.5%).3 Misoprostol plus oxytocin was significantly superior to oxytocin alone for the following outcomes: reduced risk of blood transfusion (2.6% vs 5.4%), reduced risk of blood loss ≥ 500 mL (32% vs 47%), reduced risk of requiring an additional uterotonic (14% vs 28%), and a smaller decrease in hemoglobin concentration from before to after delivery (-4.0 g/L).3 In my opinion, the statistically significant difference in hemoglobin concentration is not clinically significant. However, compared with oxytocin alone, misoprostol plus oxytocin caused significantly more nausea (12% vs 6.1%), vomiting (8.1% vs 5.4%), shivering (13% vs 7%), and fever (7.7% vs 4.0%).3
Continue to: Ergonovine plus oxytocin...
Ergonovine plus oxytocin
Ergonovine is an ergot derivative that causes uterine contractions and has been shown to effectively reduce blood loss at delivery. In the United States a methyl-derivative of ergonovine, methylergonovine, is widely available. In a meta-analysis with mostly vaginal deliveries, there were no significant differences for ergonovine plus oxytocin versus oxytocin alone for the following outcomes: death, intensive care unit admission, rate of blood loss ≥ 1,000 mL(2.0% vs 2.7%), blood transfusion, administration of an additional uterotonic, change in hemoglobin from pre- to postdelivery, nausea, hypertension, shivering, and fever.3 However, ergonovine plus oxytocin, compared with oxytocin alone, resulted in a significantly reduced rate of blood loss ≥ 500 mL (8.3% vs 10.2%) and an increased rate of vomiting (8.1% vs 1.6%).3 In these trials women with a blood pressure ≥ 150/100 mm Hg were generally excluded from receiving ergonovine because of its hypertensive effect.
Clinical practice options
Given the Cochrane meta-analysis results, ObGyns have two approaches for optimizing PPH reduction.
Option 1: Use a single uterotonic to reduce postpartum blood loss. If excess bleeding occurs, rapidly administer a second uterotonic agent. Currently, monotherapy with intravenous or intramuscular oxytocin is the standard for reducing postpartum blood loss.5,6 Advantages of this approach compared with dual agent therapy include simplification of care and minimization of AEs. However, oxytocin monotherapy for minimizing postpartum bleeding may be suboptimal. In the largest trial ever performed (involving 29,645 women) when oxytocin was administered postpartum, the rates of estimated blood loss ≥ 500 mL and ≥ 1,000 mL were 9.1% and 1.45%, respectively.5 Is 9% an optimal rate for blood loss ≥ 500 mL following a vaginal delivery? Or should we try to achieve a lower rate?
Given the “high” rate of blood loss ≥ 500 mL with oxytocin alone, it is important for clinicians using the one-uterotonic approach to promptly recognize patients who have excessive bleeding and transition rapidly from prevention to treatment. When PPH cases are reviewed, a common finding is that the clinicians did not timely recognize excess bleeding, delaying transition to treatment with additional uterotonics and other interventions. When routinely using oxytocin monotherapy, lowering the threshold for administering a second uterotonic (methylergonovine, carboprost, misoprostol, or tranexamic acid) may help decrease the frequency of excess postpartum blood loss.
Option 2: Administer two uterotonics to reduce postpartum blood loss at all deliveries. Given the “high” rate of excess postpartum blood loss with oxytocin monotherapy, an alternative is to administer two uterotonics at all births or at births with a high risk of excess blood loss. As discussed, administering two uterotonics, oxytocin plus misoprostol or oxytocin plus ergonovine, has been reported to be more effective than oxytocin alone for reducing postpartum bleeding ≥ 500 mL.3 In the Cochrane meta-analysis, per 1,000 women given oxytocin following a vaginal birth, 122 would have blood loss ≥ 500 mL, compared with 85 given oxytocin plus misoprostol or oxytocin plus ergonovine.3
Misoprostol is administered sublingually, buccally, or rectally, and methylergonovine is administered by intramuscular injection. Although dual uterotonic therapy is more effective than monotherapy, dual therapy is associated with more AEs. As noted, compared with oxytocin monotherapy, the combination of oxytocin plus misoprostol is associated with more nausea, vomiting, shivering, and fever. Oxytocin plus ergonovine is associated with a higher rate of vomiting than oxytocin monotherapy. In my practice I prefer using intramuscular methylergonovine as the second agent to avoid the high rate of fever associated with misoprostol.
For dual agent therapy, one approach is to administer misoprostol 200 µg or 400 µg through the buccal7,8 or sublingual9,10 routes. Higher dosages of misoprostol (600 µg to 800 µg) have been used11,12 but are likely associated with higher rates of nausea, vomiting,shivering, and fever than the lower dosages. Methylergonovine 0.2 mg is administered intramuscularly.
Continue to: The bottom line...
The bottom line
PPH is a major cause of maternal morbidity, and in low-resource settings, mortality. Oxytocin is the standard for reducing postpartum blood loss, but rates of blood loss ≥ 500 mL are high following this monotherapy. To reduce postpartum blood loss beyond what is possible with oxytocin alone, clinicians can more rapidly transition to administering a second uterotonic when they suspect blood loss is becoming excessive or they can use two uterotonic agents with all births or in those at high risk for excess bleeding. If blood loss does become excessive, clinicians need to pivot rapidly from prevention with oxytocin to treatment with our entire therapeutic armamentarium.
- Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2:e323-e333.
- Slomski A. Why do hundreds of US women die annually in childbirth? JAMA. 2019;321:1239-1241.
- Gallos ID, Papadopoulou A, Man R, et al. Uterotonic agents for preventing postpartum haemorrhage: a network meta-analysis. Cochrane Database Syst Rev. 2018;12:CD011689.
- American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 183: postpartum hemorrhage. Obstet Gynecol. 2017;130:e168-e186.
- Widmer M, Piaggio G, Nguyen TM, et al; WHO Champion Trial Group. Heat-stable carbetocin versus oxytocin to prevent hemorrhage after vaginal birth. N Engl J Med. 2018;379:743-752.
- Adnan N, Conlan-Trant R, McCormick C, et al. Intramuscular versus intravenous oxytocin to prevent postpartum haemorrhage at vaginal delivery: randomised controlled trial. BMJ. 2018;362:k3546.
- Hamm J, Russell Z, Botha T, et al. Buccal misoprostol to prevent hemorrhage at cesarean delivery: a randomized study. Am J Obstet Gynecol. 2005;192:1404-1406.
- Bhullar A, Carlan SJ, Hamm J, et al. Buccal misoprostol to decrease blood loss after vaginal delivery: a randomized trial. Obstet Gynecol. 2004;104:1282-1288.
- Hofmeyr GJ, Fawole B, Mugerwa K, et al. Administration of 400 µg of misoprostol to augment routine active management of the third stage of labor. Int J Gynaecol Obstet. 2011;112:98-102.
- Chaudhuri P, Majumdar A. A randomized trial of sublingual misoprostol to augment routine third-stage management among women at risk of postpartum hemorrhage. Int J Gynaecol Obstet. 2016;132:191-195.
- Winikoff B, Dabash R, Durocher J, et al. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women not exposed to oxytocin during labor: a double-blind, randomised, non-inferiority trial. Lancet. 2010;375:210-216.
- Blum J, Winikoff B, Raghavan S, et al. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women receiving prophylactic oxytocin: a double-blind, randomised, non-inferiority trial. Lancet. 2010;375:217-223.
- Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2:e323-e333.
- Slomski A. Why do hundreds of US women die annually in childbirth? JAMA. 2019;321:1239-1241.
- Gallos ID, Papadopoulou A, Man R, et al. Uterotonic agents for preventing postpartum haemorrhage: a network meta-analysis. Cochrane Database Syst Rev. 2018;12:CD011689.
- American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 183: postpartum hemorrhage. Obstet Gynecol. 2017;130:e168-e186.
- Widmer M, Piaggio G, Nguyen TM, et al; WHO Champion Trial Group. Heat-stable carbetocin versus oxytocin to prevent hemorrhage after vaginal birth. N Engl J Med. 2018;379:743-752.
- Adnan N, Conlan-Trant R, McCormick C, et al. Intramuscular versus intravenous oxytocin to prevent postpartum haemorrhage at vaginal delivery: randomised controlled trial. BMJ. 2018;362:k3546.
- Hamm J, Russell Z, Botha T, et al. Buccal misoprostol to prevent hemorrhage at cesarean delivery: a randomized study. Am J Obstet Gynecol. 2005;192:1404-1406.
- Bhullar A, Carlan SJ, Hamm J, et al. Buccal misoprostol to decrease blood loss after vaginal delivery: a randomized trial. Obstet Gynecol. 2004;104:1282-1288.
- Hofmeyr GJ, Fawole B, Mugerwa K, et al. Administration of 400 µg of misoprostol to augment routine active management of the third stage of labor. Int J Gynaecol Obstet. 2011;112:98-102.
- Chaudhuri P, Majumdar A. A randomized trial of sublingual misoprostol to augment routine third-stage management among women at risk of postpartum hemorrhage. Int J Gynaecol Obstet. 2016;132:191-195.
- Winikoff B, Dabash R, Durocher J, et al. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women not exposed to oxytocin during labor: a double-blind, randomised, non-inferiority trial. Lancet. 2010;375:210-216.
- Blum J, Winikoff B, Raghavan S, et al. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women receiving prophylactic oxytocin: a double-blind, randomised, non-inferiority trial. Lancet. 2010;375:217-223.

