User login
A 64-year-old woman came into our emergency department (ED) complaining of constipation and worsening rectal pain. In an attempt to promote her overall health, the patient had recently begun experimenting with healthy alternatives to her regular diet. Three days before her visit, she had ceased having stools and was experiencing intermittent abdominal cramping. She self-administered 2 bisacodyl suppositories, 2 sodium biphosphate enemas, one 10-ounce bottle of magnesium citrate, and 15 senna-containing laxative tablets without improvement.
She sought care at an urgent care clinic where she received 2 additional enemas and a trial of manual disimpaction—without results. She was sent home to rest and asked to return the next morning for another trial of disimpaction. When the patient’s efforts to manually disimpact herself at home were unsuccessful, she contacted her primary care physician, who arranged a house call. When his own protracted disimpaction procedure was unsuccessful, he referred her to our ED.
On presentation, the patient had lower abdominal and rectal discomfort. Her vital signs were normal except for a temperature of 38.8° C. Her abdomen was soft and nontender. Inspection of her perianal area revealed erythema and excoriations. On digital rectal exam (which was poorly tolerated because of pain), we noted a moderate amount of soft, clay-like feces in the rectal vault, with overflow liquid stool expulsion.
Computed tomography (CT) imaging of the abdomen was obtained to rule out rectal injury or colonic perforation (FIGURE 1).
FIGURE 1
CT scan reveals a speckled intraluminal mass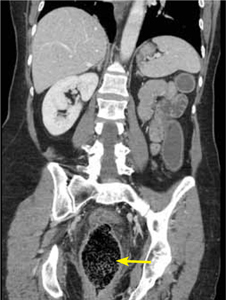
The patient had a markedly distended rectum and distal sigmoid colon caused by an intraluminal mass. Also present: circumferential wall thickening, perirectal edema without extraluminal gas, and generalized proximal colonic wall edema without a drainable collection.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Fecal impaction caused by a proctophytobezoar
CT imaging revealed a proctophytobezoar. On follow-up questioning, the patient recalled consuming approximately 10 ounces of cooked quinoa, a nutritious, gluten-free, high-protein seed, just prior to the onset of her constipation.
Constipation disproportionately affects the elderly and the young.1 Fecal impaction is a sequelae of constipation. Most commonly defined as hard, compacted feces in the rectum, fecal impaction can also include more proximal impactions due to fecal loading or retention.2
Causes of constipation and fecal impaction are similar and include low intake of dietary fiber, dehydration, immobility, alcohol ingestion, laxative abuse, medication adverse effects, depression, dementia, spinal cord dysfunction, diabetes, metabolic imbalances, and hypothyroidism.2,3 Insufficient hydration with consumption of a high-fiber food, as in this case, or with a bulk-forming laxative such as psyllium seed can result in fecal impaction.3
The many causes of a bezoar
A bezoar is a mass of poorly digested material that forms within the gastrointestinal tract—usually in the stomach—and less commonly in the small or large intestine.4 Trichobezoars (hair), lactobezoars (milk curd), phytobezoars (plant fiber), medication bezoars, and lithobezoars (small stones, pebbles, or gravel) are named after their contents. In keeping with this naming tradition, a gummi bear bezoar5 has also been described. Fecal impaction due to phytobezoars primarily composed of seeds has been associated with prickly pears, watermelons, sunflowers, pumpkins, pomegranates,6,7 and sesame seeds.4 Our patient’s experience adds quinoa seeds to this list.
Patients will complain of nausea and rectal urgency
Patients with fecal impaction may complain of nausea, rectal urgency, and rectalgia. A ball-valve effect of the fecal mass may allow paradoxical fecal incontinence and diarrhea.3 Digital rectal exam may demonstrate stool of any consistency, from rock hard pellets to soft clay-like stool.3 Absence of stool in the rectal vault does not rule out fecal impaction, and more proximal impactions may be revealed on plain abdominal radiography as bubbly, speckled masses of stool with associated signs of obstruction, such as colonic dilatation.
Fever, increased leukocyte count, and abdominal tenderness may indicate colonic perforation or ulceration. Signs of generalized peritonitis and free air on abdominal radiography warrant an immediate surgical consult.3
Complications from fecal impaction include bowel obstruction, sigmoid volvulus, and rectal prolapse.2 Stercoral ulceration and perforation due to pressure necrosis from a hard, inspissated fecal mass is an uncommon but life-threatening complication requiring resection of the affected colonic segment.8
What to look for on the CT. When the diagnosis is unclear or signs of complications are present, an abdominal CT is indicated. Concerning CT findings include ulceration, bowel wall enhancement and thickening (FIGURE 2), discontinuity of the bowel wall, presence of fecal material either protruding through the colonic wall or lying free within the intra-abdominal cavity, and extraluminal air.8
FIGURE 2
CT scan shows bowel wall thickening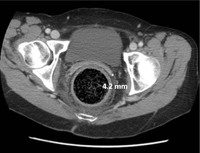
Treatment begins with a pharmacologic approach
By the time a patient with a fecal impaction gets to your office, it’s likely that he or she will have already tried over-the-counter laxatives, stool softeners, and perhaps an enema.
When such pharmacologic management has failed, you’ll need to perform a manual fragmentation and extraction of the fecal mass. Apply topical 2% lidocaine jelly for analgesia and lubrication, and then gently and progressively dilate the anal sphincter with one and then 2 fingers. A scissoring action will fragment the impaction.3
Once fragmentation and partial expulsion has been achieved, you may want to try a lubricating mineral oil enema, bisacodyl suppository, or rectal lavage. If the impaction extends beyond the reach of the fingers, sigmoidoscopic visualization and lavage are indicated.
Adding water-soluble contrast material (Gastrografin) in 20% to 50% solutions directed by fluoroscopy draws water into the lumen, thus lubricating the fecal mass3,9 and helping it to pass spontaneously.
Our patient’s case resolved with a trip to the OR
Since conservative and comprehensive management to improve our patient’s condition failed, she was taken to the operating room for a proctosigmoidoscopic disimpaction. A beveled metal proctoscope was used to disimpact the distal-most 10 cm and then a rigid sigmoidoscope was used to clear the colon of quinoa-laden fecal material to a total distance of 18 cm. Bowel walls were ecchymotic, yet viable and without laceration. She made an uneventful recovery and was discharged on hospital Day 3.
CORRESPONDENCE George L. Higgins, III, MD, Maine Medical Center, Department of Emergency Medicine, 47 Bramhall Street, Portland, ME 04102; [email protected]
1. Rao SS, Go JT. Update on the management of constipation in the elderly: new treatment options. Clin Interv Aging. 2010;5:163-171.
2. Creason N, Sparks D. Fecal impaction: a review. Nurs Diagn. 2000;11:15-23.
3. Wrenn K. Fecal impaction. N Engl J Med. 1989;321:658-662.
4. Shaw AG, Peacock O, Lund JN, et al. Large bowel obstruction due to sesame seed bezoar: a case report. J Med Case Reports. 2007;1:159.-
5. Barron MM, Steerman P. Gummi bear bezoar: a case report. J Emerg Med. 1989;7:143-144.
6. Eitan A, Bickel A, Katz IM. Fecal impaction in adults: report of 30 cases of seed bezoars in the rectum. Dis Colon Rectum. 2006;49:1768-1771.
7. Eitan A, Katz IM, Sweed Y, et al. Fecal impaction in children: report of 53 cases of rectal seed bezoars. J Pediatr Surg. 2007;42:1114-1117.
8. Kumar P, Pearce O, Higginson A. Imaging manifestations of faecal impaction and stercoral perforation. Clin Radiol. 2011;66:83-88.
9. Brenner BE, Simon RR. Anorectal emergencies. Ann Emerg Med. 1983;12:367-376.
A 64-year-old woman came into our emergency department (ED) complaining of constipation and worsening rectal pain. In an attempt to promote her overall health, the patient had recently begun experimenting with healthy alternatives to her regular diet. Three days before her visit, she had ceased having stools and was experiencing intermittent abdominal cramping. She self-administered 2 bisacodyl suppositories, 2 sodium biphosphate enemas, one 10-ounce bottle of magnesium citrate, and 15 senna-containing laxative tablets without improvement.
She sought care at an urgent care clinic where she received 2 additional enemas and a trial of manual disimpaction—without results. She was sent home to rest and asked to return the next morning for another trial of disimpaction. When the patient’s efforts to manually disimpact herself at home were unsuccessful, she contacted her primary care physician, who arranged a house call. When his own protracted disimpaction procedure was unsuccessful, he referred her to our ED.
On presentation, the patient had lower abdominal and rectal discomfort. Her vital signs were normal except for a temperature of 38.8° C. Her abdomen was soft and nontender. Inspection of her perianal area revealed erythema and excoriations. On digital rectal exam (which was poorly tolerated because of pain), we noted a moderate amount of soft, clay-like feces in the rectal vault, with overflow liquid stool expulsion.
Computed tomography (CT) imaging of the abdomen was obtained to rule out rectal injury or colonic perforation (FIGURE 1).
FIGURE 1
CT scan reveals a speckled intraluminal mass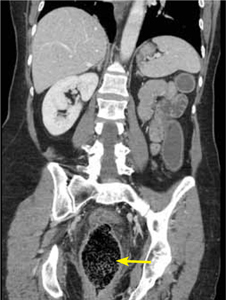
The patient had a markedly distended rectum and distal sigmoid colon caused by an intraluminal mass. Also present: circumferential wall thickening, perirectal edema without extraluminal gas, and generalized proximal colonic wall edema without a drainable collection.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Fecal impaction caused by a proctophytobezoar
CT imaging revealed a proctophytobezoar. On follow-up questioning, the patient recalled consuming approximately 10 ounces of cooked quinoa, a nutritious, gluten-free, high-protein seed, just prior to the onset of her constipation.
Constipation disproportionately affects the elderly and the young.1 Fecal impaction is a sequelae of constipation. Most commonly defined as hard, compacted feces in the rectum, fecal impaction can also include more proximal impactions due to fecal loading or retention.2
Causes of constipation and fecal impaction are similar and include low intake of dietary fiber, dehydration, immobility, alcohol ingestion, laxative abuse, medication adverse effects, depression, dementia, spinal cord dysfunction, diabetes, metabolic imbalances, and hypothyroidism.2,3 Insufficient hydration with consumption of a high-fiber food, as in this case, or with a bulk-forming laxative such as psyllium seed can result in fecal impaction.3
The many causes of a bezoar
A bezoar is a mass of poorly digested material that forms within the gastrointestinal tract—usually in the stomach—and less commonly in the small or large intestine.4 Trichobezoars (hair), lactobezoars (milk curd), phytobezoars (plant fiber), medication bezoars, and lithobezoars (small stones, pebbles, or gravel) are named after their contents. In keeping with this naming tradition, a gummi bear bezoar5 has also been described. Fecal impaction due to phytobezoars primarily composed of seeds has been associated with prickly pears, watermelons, sunflowers, pumpkins, pomegranates,6,7 and sesame seeds.4 Our patient’s experience adds quinoa seeds to this list.
Patients will complain of nausea and rectal urgency
Patients with fecal impaction may complain of nausea, rectal urgency, and rectalgia. A ball-valve effect of the fecal mass may allow paradoxical fecal incontinence and diarrhea.3 Digital rectal exam may demonstrate stool of any consistency, from rock hard pellets to soft clay-like stool.3 Absence of stool in the rectal vault does not rule out fecal impaction, and more proximal impactions may be revealed on plain abdominal radiography as bubbly, speckled masses of stool with associated signs of obstruction, such as colonic dilatation.
Fever, increased leukocyte count, and abdominal tenderness may indicate colonic perforation or ulceration. Signs of generalized peritonitis and free air on abdominal radiography warrant an immediate surgical consult.3
Complications from fecal impaction include bowel obstruction, sigmoid volvulus, and rectal prolapse.2 Stercoral ulceration and perforation due to pressure necrosis from a hard, inspissated fecal mass is an uncommon but life-threatening complication requiring resection of the affected colonic segment.8
What to look for on the CT. When the diagnosis is unclear or signs of complications are present, an abdominal CT is indicated. Concerning CT findings include ulceration, bowel wall enhancement and thickening (FIGURE 2), discontinuity of the bowel wall, presence of fecal material either protruding through the colonic wall or lying free within the intra-abdominal cavity, and extraluminal air.8
FIGURE 2
CT scan shows bowel wall thickening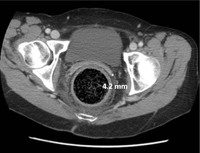
Treatment begins with a pharmacologic approach
By the time a patient with a fecal impaction gets to your office, it’s likely that he or she will have already tried over-the-counter laxatives, stool softeners, and perhaps an enema.
When such pharmacologic management has failed, you’ll need to perform a manual fragmentation and extraction of the fecal mass. Apply topical 2% lidocaine jelly for analgesia and lubrication, and then gently and progressively dilate the anal sphincter with one and then 2 fingers. A scissoring action will fragment the impaction.3
Once fragmentation and partial expulsion has been achieved, you may want to try a lubricating mineral oil enema, bisacodyl suppository, or rectal lavage. If the impaction extends beyond the reach of the fingers, sigmoidoscopic visualization and lavage are indicated.
Adding water-soluble contrast material (Gastrografin) in 20% to 50% solutions directed by fluoroscopy draws water into the lumen, thus lubricating the fecal mass3,9 and helping it to pass spontaneously.
Our patient’s case resolved with a trip to the OR
Since conservative and comprehensive management to improve our patient’s condition failed, she was taken to the operating room for a proctosigmoidoscopic disimpaction. A beveled metal proctoscope was used to disimpact the distal-most 10 cm and then a rigid sigmoidoscope was used to clear the colon of quinoa-laden fecal material to a total distance of 18 cm. Bowel walls were ecchymotic, yet viable and without laceration. She made an uneventful recovery and was discharged on hospital Day 3.
CORRESPONDENCE George L. Higgins, III, MD, Maine Medical Center, Department of Emergency Medicine, 47 Bramhall Street, Portland, ME 04102; [email protected]
A 64-year-old woman came into our emergency department (ED) complaining of constipation and worsening rectal pain. In an attempt to promote her overall health, the patient had recently begun experimenting with healthy alternatives to her regular diet. Three days before her visit, she had ceased having stools and was experiencing intermittent abdominal cramping. She self-administered 2 bisacodyl suppositories, 2 sodium biphosphate enemas, one 10-ounce bottle of magnesium citrate, and 15 senna-containing laxative tablets without improvement.
She sought care at an urgent care clinic where she received 2 additional enemas and a trial of manual disimpaction—without results. She was sent home to rest and asked to return the next morning for another trial of disimpaction. When the patient’s efforts to manually disimpact herself at home were unsuccessful, she contacted her primary care physician, who arranged a house call. When his own protracted disimpaction procedure was unsuccessful, he referred her to our ED.
On presentation, the patient had lower abdominal and rectal discomfort. Her vital signs were normal except for a temperature of 38.8° C. Her abdomen was soft and nontender. Inspection of her perianal area revealed erythema and excoriations. On digital rectal exam (which was poorly tolerated because of pain), we noted a moderate amount of soft, clay-like feces in the rectal vault, with overflow liquid stool expulsion.
Computed tomography (CT) imaging of the abdomen was obtained to rule out rectal injury or colonic perforation (FIGURE 1).
FIGURE 1
CT scan reveals a speckled intraluminal mass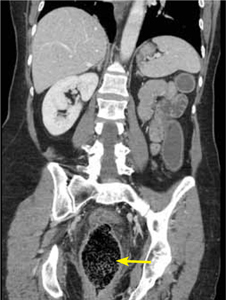
The patient had a markedly distended rectum and distal sigmoid colon caused by an intraluminal mass. Also present: circumferential wall thickening, perirectal edema without extraluminal gas, and generalized proximal colonic wall edema without a drainable collection.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Fecal impaction caused by a proctophytobezoar
CT imaging revealed a proctophytobezoar. On follow-up questioning, the patient recalled consuming approximately 10 ounces of cooked quinoa, a nutritious, gluten-free, high-protein seed, just prior to the onset of her constipation.
Constipation disproportionately affects the elderly and the young.1 Fecal impaction is a sequelae of constipation. Most commonly defined as hard, compacted feces in the rectum, fecal impaction can also include more proximal impactions due to fecal loading or retention.2
Causes of constipation and fecal impaction are similar and include low intake of dietary fiber, dehydration, immobility, alcohol ingestion, laxative abuse, medication adverse effects, depression, dementia, spinal cord dysfunction, diabetes, metabolic imbalances, and hypothyroidism.2,3 Insufficient hydration with consumption of a high-fiber food, as in this case, or with a bulk-forming laxative such as psyllium seed can result in fecal impaction.3
The many causes of a bezoar
A bezoar is a mass of poorly digested material that forms within the gastrointestinal tract—usually in the stomach—and less commonly in the small or large intestine.4 Trichobezoars (hair), lactobezoars (milk curd), phytobezoars (plant fiber), medication bezoars, and lithobezoars (small stones, pebbles, or gravel) are named after their contents. In keeping with this naming tradition, a gummi bear bezoar5 has also been described. Fecal impaction due to phytobezoars primarily composed of seeds has been associated with prickly pears, watermelons, sunflowers, pumpkins, pomegranates,6,7 and sesame seeds.4 Our patient’s experience adds quinoa seeds to this list.
Patients will complain of nausea and rectal urgency
Patients with fecal impaction may complain of nausea, rectal urgency, and rectalgia. A ball-valve effect of the fecal mass may allow paradoxical fecal incontinence and diarrhea.3 Digital rectal exam may demonstrate stool of any consistency, from rock hard pellets to soft clay-like stool.3 Absence of stool in the rectal vault does not rule out fecal impaction, and more proximal impactions may be revealed on plain abdominal radiography as bubbly, speckled masses of stool with associated signs of obstruction, such as colonic dilatation.
Fever, increased leukocyte count, and abdominal tenderness may indicate colonic perforation or ulceration. Signs of generalized peritonitis and free air on abdominal radiography warrant an immediate surgical consult.3
Complications from fecal impaction include bowel obstruction, sigmoid volvulus, and rectal prolapse.2 Stercoral ulceration and perforation due to pressure necrosis from a hard, inspissated fecal mass is an uncommon but life-threatening complication requiring resection of the affected colonic segment.8
What to look for on the CT. When the diagnosis is unclear or signs of complications are present, an abdominal CT is indicated. Concerning CT findings include ulceration, bowel wall enhancement and thickening (FIGURE 2), discontinuity of the bowel wall, presence of fecal material either protruding through the colonic wall or lying free within the intra-abdominal cavity, and extraluminal air.8
FIGURE 2
CT scan shows bowel wall thickening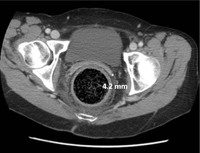
Treatment begins with a pharmacologic approach
By the time a patient with a fecal impaction gets to your office, it’s likely that he or she will have already tried over-the-counter laxatives, stool softeners, and perhaps an enema.
When such pharmacologic management has failed, you’ll need to perform a manual fragmentation and extraction of the fecal mass. Apply topical 2% lidocaine jelly for analgesia and lubrication, and then gently and progressively dilate the anal sphincter with one and then 2 fingers. A scissoring action will fragment the impaction.3
Once fragmentation and partial expulsion has been achieved, you may want to try a lubricating mineral oil enema, bisacodyl suppository, or rectal lavage. If the impaction extends beyond the reach of the fingers, sigmoidoscopic visualization and lavage are indicated.
Adding water-soluble contrast material (Gastrografin) in 20% to 50% solutions directed by fluoroscopy draws water into the lumen, thus lubricating the fecal mass3,9 and helping it to pass spontaneously.
Our patient’s case resolved with a trip to the OR
Since conservative and comprehensive management to improve our patient’s condition failed, she was taken to the operating room for a proctosigmoidoscopic disimpaction. A beveled metal proctoscope was used to disimpact the distal-most 10 cm and then a rigid sigmoidoscope was used to clear the colon of quinoa-laden fecal material to a total distance of 18 cm. Bowel walls were ecchymotic, yet viable and without laceration. She made an uneventful recovery and was discharged on hospital Day 3.
CORRESPONDENCE George L. Higgins, III, MD, Maine Medical Center, Department of Emergency Medicine, 47 Bramhall Street, Portland, ME 04102; [email protected]
1. Rao SS, Go JT. Update on the management of constipation in the elderly: new treatment options. Clin Interv Aging. 2010;5:163-171.
2. Creason N, Sparks D. Fecal impaction: a review. Nurs Diagn. 2000;11:15-23.
3. Wrenn K. Fecal impaction. N Engl J Med. 1989;321:658-662.
4. Shaw AG, Peacock O, Lund JN, et al. Large bowel obstruction due to sesame seed bezoar: a case report. J Med Case Reports. 2007;1:159.-
5. Barron MM, Steerman P. Gummi bear bezoar: a case report. J Emerg Med. 1989;7:143-144.
6. Eitan A, Bickel A, Katz IM. Fecal impaction in adults: report of 30 cases of seed bezoars in the rectum. Dis Colon Rectum. 2006;49:1768-1771.
7. Eitan A, Katz IM, Sweed Y, et al. Fecal impaction in children: report of 53 cases of rectal seed bezoars. J Pediatr Surg. 2007;42:1114-1117.
8. Kumar P, Pearce O, Higginson A. Imaging manifestations of faecal impaction and stercoral perforation. Clin Radiol. 2011;66:83-88.
9. Brenner BE, Simon RR. Anorectal emergencies. Ann Emerg Med. 1983;12:367-376.
1. Rao SS, Go JT. Update on the management of constipation in the elderly: new treatment options. Clin Interv Aging. 2010;5:163-171.
2. Creason N, Sparks D. Fecal impaction: a review. Nurs Diagn. 2000;11:15-23.
3. Wrenn K. Fecal impaction. N Engl J Med. 1989;321:658-662.
4. Shaw AG, Peacock O, Lund JN, et al. Large bowel obstruction due to sesame seed bezoar: a case report. J Med Case Reports. 2007;1:159.-
5. Barron MM, Steerman P. Gummi bear bezoar: a case report. J Emerg Med. 1989;7:143-144.
6. Eitan A, Bickel A, Katz IM. Fecal impaction in adults: report of 30 cases of seed bezoars in the rectum. Dis Colon Rectum. 2006;49:1768-1771.
7. Eitan A, Katz IM, Sweed Y, et al. Fecal impaction in children: report of 53 cases of rectal seed bezoars. J Pediatr Surg. 2007;42:1114-1117.
8. Kumar P, Pearce O, Higginson A. Imaging manifestations of faecal impaction and stercoral perforation. Clin Radiol. 2011;66:83-88.
9. Brenner BE, Simon RR. Anorectal emergencies. Ann Emerg Med. 1983;12:367-376.