User login
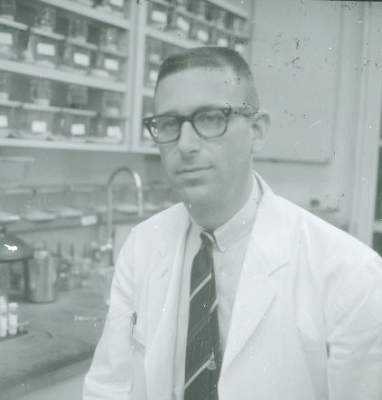
In 1966, Dr. Charles Hammond was wrapping up a 2-year stint at the National Institutes of Health where he served at the behest of the military draft board. He had graduated from medical school just 5 years prior, and was in the middle of his ob.gyn. residency training at Duke University in Durham, N.C. when he was called to serve.
His experience wasn’t unusual for the time.
“When the draft board called, you went,” he said in an interview.
When he returned, he picked up where he left off. Residencies at that time were an “open-ended thing,” sometimes lasting 5 or 6 years, depending on staffing needs and other considerations.
Dr. Hammond, now an emeritus professor at Duke, regards his public service commission as an opportunity that advanced his academic career – despite the interruption of his residency training.
Such draft-related interruptions ended in the wake of the Vietnam War, of course, but the late 1960s and the 1970s ushered in a whole new era of changes in ob.gyn. residency training programs.
By 1968, residencies lasted 4 years, and fellowships were for 2 years. Ob.gyn. subspecialties hadn’t yet been introduced, explained Dr. Sandra A. Carson, vice president for education at the American College of Obstetricians and Gynecologists.
“That is essentially how things worked for a long time,” she said in an interview.
That’s not to say there weren’t numerous other changes taking place in the specialty. In a series of interviews with physicians and educators who discussed the myriad ways that residency training has evolved over the last 50 years, a number of themes emerged.
Women in medicine
A striking change over the past 5 decades has been the increasing number of women in medicine. Nowhere has that been in greater evidence than in obstetrics and gynecology.
“There were a few – but very few,” Dr. Hammond said of women in medicine in the 1960s.
There was “a philosophy that men did it better,” he said, adding, “That has been nicely shown to be inaccurate.”
Currently, about 80% of first-year ob.gyn. residents are women, compared with 15% in 1975.
“Maybe even 83% now,” Dr. Carson said, noting that even in the early 1980s when she was in training, women were “few and far between.”
According to a 2011 workforce report by Dr. William F. Rayburn, obstetrics and gynecology has the highest percentage of women residents of any medical specialty – 80% in 2009 versus an average of 46% for other specialties combined, and that figure has remained fairly constant.
Dr. Kasandra Scales, a fourth-year resident at the State University of New York, Syracuse, said she is glad to be part of this era of the specialty where women play an integral role in the advancement of women’s health care.
“I believe our voice and unique perspective to relate with common experiences, such as the physical birth of a child or personal choices in contraception... has enhanced our specialty,” she said.
That said, the fact that men are noticeably absent from the pool of ob.gyn. applicants and residents concerns her. “There should be a balance, she said. “I think it is important to have diversity of all types in the healthcare system.”
Dr. Hammond looked back on his days in residency training and recalled pockets of resistance to the increasing number of women in medicine, but the ultimate effect was good for the specialty, he said, explaining that the quality of the resident pool improved steadily, because the number of qualified candidates increased.
“It has been an interesting interval to watch,” he said, specifically mentioning the demands that women faced in terms of family obligations, childbirth, and childrearing.
Restrictions on work hours instituted in residency programs in more recent years may have played an important role in opening the door to more women, he said.
Work hours down, learning curve up
Dr. Carson agreed that work-hour restrictions instituted in 2003 and updated in 2011, which cap the work week at 80 hours and also apply limits on shift hours, likely encouraged more women to enter the field. One constant over the last 50 years is the biological clock, she said, explaining that the pressures and demands of residency before limits were put in place may have steered women away.
Work-hour restrictions provide more flexibility, but they aren’t without controversy.
Dr. Hammond said he sees the value in work hour restrictions, but working long hours as a resident – sometimes as many as 110 hours per week – had its benefits, too.
“I remember one time when I’d been on call for about 2 and a half days, and up and working the whole time,” Dr. Hammond said. “I left the hospital, walked out to a bench, sat down, and fell asleep. I woke up and distinctly remember thinking, ‘Why am I doing this?’ But I did do it, and that fatigue helped me with learning to endure. You learned from it.”
Not only have long hours been viewed as a rite of passage in medicine, he said, but there were concerns initially that the level of education would diminish and that the risk of patient errors would increase as patients were handed off from one shift to the next, he said.
Data on the effects of work-hour rules have been conflicting. In one study, Dr. Roger P. Smith found little overall effect on total technical experience among residents before and after the restrictions were put in place (there was no statistically significant difference in the average of median total cases in the 3 years before and after). Previous studies had documented increased costs and reduced faculty job satisfaction, while still others had shown no significant changes in 30-day readmission rates, in-hospital mortality, patient length of stay, or resident performance, he noted. “What is emerging is that both the great hopes and the great fears surrounding resident work-hour restrictions have not come to pass,” Dr. Smith wrote (Obstet Gynecol. 2010 Jun;115[6]:1166-71).
Dr. Scales, who is currently chair of the Junior Fellow District II Advisory Council for ACOG, comes down on the side of wishing for more hours.
“[The restrictions] do limit the things we can do and the exposure we may otherwise have,” she said, noting that it’s frustrating to have to leave when she’d rather stay and “see a cool case.”
“It’s a nice idea in principle, but the same amount of work has to be done. It’s not real life,” she said of work-hour restrictions. “It’s hard, at least for me, to want to give up my patients. Our job is to take in as much as you can before you leave to go out into the big bad world.”
It may be difficult to determine the actual impact of work hour limits on patient outcomes because the field of obstetrics and gynecology has changed so much over time.
Dr. David Forstein, vice chair of clinical operations in the department of obstetrics and gynecology at the University of South Carolina, Greenville, and a member of the Accreditation Council for Graduate Medical Education’s task force on work hours said that, for one thing, patients are generally sicker now than ever before, due in part to the obesity epidemic.
Further, changing trends mean that residents are getting less exposure to some procedures like operative vaginal deliveries, while also having to learn more ways to perform hysterectomy. Residents aren’t necessarily less prepared. They’re just having to work very hard because of the depth and breadth of the required knowledge has increased, Dr. Forstein said. “There’s a lot more to learn.”
Dr. Carson agreed that the approach to education has changed, and that those changes are largely a reflection of overall shifts in education and technology.
Technology trends
Every physician interviewed for this article cited laparoscopy and robotic surgery as key technological advances. Fifty years ago, the surgical tools were simpler, Dr. Carson said. Now residents must learn four approaches to hysterectomy: vaginal, abdominal, laparoscopic, and robotic-assisted laparoscopic hysterectomy.
From ultrasound and birth control to genetic screening and robotic surgery, the evolution of the field has been astounding during this time period. The effects of the birth control pill on family planning alone forced an expansion of curriculum not only to the physiology of these things, but also to the treatment of women as a whole person and often as part of a family unit, she said.
Many of the technologies have dramatically changed the landscape, both in terms of how learning is accomplished (for example, simulation), and how physicians interact with patients, Dr. Hammond agreed. With ultrasound, for example, there was a sense that part of the physician-patient relationship was lost.
“To a point, some of us old guys felt like they were doing ultrasound assessment of patients rather than the tried-and-true ‘talk to them and examine them’ [approach],” he said. “I guess whichever generation you are in seems to be the right one, but it’s probably somewhere in between.”
Residency in 2016
If Dr. Scales is any indication, concerns about the loss of a personal touch are unfounded. She says that for her, that’s what it’s all about.
“We were exposed to [technology] since we were 5 or 6 – it’s all we know,” she said of herself and her fellow residents. “It’s not a disadvantage. It’s about efficiency.”
“We have to get things done as quickly as possible and technology helps us with that,” said Dr. Scales, the daughter of a teacher and blue collar worker, who spent most of her life “surrounded by the underprivileged.”
She always desired to help lift that population up, and while she didn’t have a draft board directing her toward public service, she had her own calling of sorts. As a premed major in college, she worked with a nonprofit organization, and later she worked with Hurricane Katrina survivors.
“I liked that aspect of medicine. I wanted to be able to identify with people on an individual level,” she said.
Technology, work-hour restrictions, gender distribution – they’re just part of the journey.
“I’m glad I chose ob.gyn.,” she said. “Sometimes you go through ... reflection ... Am I ready? My answer is yes. I’m excited about the next step, I’m comfortable in the skill I learned in my residency program, I’m excited about the work I do every day, and I’m very excited about the next chapters.”
In 1966, Dr. Charles Hammond was wrapping up a 2-year stint at the National Institutes of Health where he served at the behest of the military draft board. He had graduated from medical school just 5 years prior, and was in the middle of his ob.gyn. residency training at Duke University in Durham, N.C. when he was called to serve.
His experience wasn’t unusual for the time.
“When the draft board called, you went,” he said in an interview.
When he returned, he picked up where he left off. Residencies at that time were an “open-ended thing,” sometimes lasting 5 or 6 years, depending on staffing needs and other considerations.
Dr. Hammond, now an emeritus professor at Duke, regards his public service commission as an opportunity that advanced his academic career – despite the interruption of his residency training.
Such draft-related interruptions ended in the wake of the Vietnam War, of course, but the late 1960s and the 1970s ushered in a whole new era of changes in ob.gyn. residency training programs.
By 1968, residencies lasted 4 years, and fellowships were for 2 years. Ob.gyn. subspecialties hadn’t yet been introduced, explained Dr. Sandra A. Carson, vice president for education at the American College of Obstetricians and Gynecologists.
“That is essentially how things worked for a long time,” she said in an interview.
That’s not to say there weren’t numerous other changes taking place in the specialty. In a series of interviews with physicians and educators who discussed the myriad ways that residency training has evolved over the last 50 years, a number of themes emerged.
Women in medicine
A striking change over the past 5 decades has been the increasing number of women in medicine. Nowhere has that been in greater evidence than in obstetrics and gynecology.
“There were a few – but very few,” Dr. Hammond said of women in medicine in the 1960s.
There was “a philosophy that men did it better,” he said, adding, “That has been nicely shown to be inaccurate.”
Currently, about 80% of first-year ob.gyn. residents are women, compared with 15% in 1975.
“Maybe even 83% now,” Dr. Carson said, noting that even in the early 1980s when she was in training, women were “few and far between.”
According to a 2011 workforce report by Dr. William F. Rayburn, obstetrics and gynecology has the highest percentage of women residents of any medical specialty – 80% in 2009 versus an average of 46% for other specialties combined, and that figure has remained fairly constant.
Dr. Kasandra Scales, a fourth-year resident at the State University of New York, Syracuse, said she is glad to be part of this era of the specialty where women play an integral role in the advancement of women’s health care.
“I believe our voice and unique perspective to relate with common experiences, such as the physical birth of a child or personal choices in contraception... has enhanced our specialty,” she said.
That said, the fact that men are noticeably absent from the pool of ob.gyn. applicants and residents concerns her. “There should be a balance, she said. “I think it is important to have diversity of all types in the healthcare system.”
Dr. Hammond looked back on his days in residency training and recalled pockets of resistance to the increasing number of women in medicine, but the ultimate effect was good for the specialty, he said, explaining that the quality of the resident pool improved steadily, because the number of qualified candidates increased.
“It has been an interesting interval to watch,” he said, specifically mentioning the demands that women faced in terms of family obligations, childbirth, and childrearing.
Restrictions on work hours instituted in residency programs in more recent years may have played an important role in opening the door to more women, he said.
Work hours down, learning curve up
Dr. Carson agreed that work-hour restrictions instituted in 2003 and updated in 2011, which cap the work week at 80 hours and also apply limits on shift hours, likely encouraged more women to enter the field. One constant over the last 50 years is the biological clock, she said, explaining that the pressures and demands of residency before limits were put in place may have steered women away.
Work-hour restrictions provide more flexibility, but they aren’t without controversy.
Dr. Hammond said he sees the value in work hour restrictions, but working long hours as a resident – sometimes as many as 110 hours per week – had its benefits, too.
“I remember one time when I’d been on call for about 2 and a half days, and up and working the whole time,” Dr. Hammond said. “I left the hospital, walked out to a bench, sat down, and fell asleep. I woke up and distinctly remember thinking, ‘Why am I doing this?’ But I did do it, and that fatigue helped me with learning to endure. You learned from it.”
Not only have long hours been viewed as a rite of passage in medicine, he said, but there were concerns initially that the level of education would diminish and that the risk of patient errors would increase as patients were handed off from one shift to the next, he said.
Data on the effects of work-hour rules have been conflicting. In one study, Dr. Roger P. Smith found little overall effect on total technical experience among residents before and after the restrictions were put in place (there was no statistically significant difference in the average of median total cases in the 3 years before and after). Previous studies had documented increased costs and reduced faculty job satisfaction, while still others had shown no significant changes in 30-day readmission rates, in-hospital mortality, patient length of stay, or resident performance, he noted. “What is emerging is that both the great hopes and the great fears surrounding resident work-hour restrictions have not come to pass,” Dr. Smith wrote (Obstet Gynecol. 2010 Jun;115[6]:1166-71).
Dr. Scales, who is currently chair of the Junior Fellow District II Advisory Council for ACOG, comes down on the side of wishing for more hours.
“[The restrictions] do limit the things we can do and the exposure we may otherwise have,” she said, noting that it’s frustrating to have to leave when she’d rather stay and “see a cool case.”
“It’s a nice idea in principle, but the same amount of work has to be done. It’s not real life,” she said of work-hour restrictions. “It’s hard, at least for me, to want to give up my patients. Our job is to take in as much as you can before you leave to go out into the big bad world.”
It may be difficult to determine the actual impact of work hour limits on patient outcomes because the field of obstetrics and gynecology has changed so much over time.
Dr. David Forstein, vice chair of clinical operations in the department of obstetrics and gynecology at the University of South Carolina, Greenville, and a member of the Accreditation Council for Graduate Medical Education’s task force on work hours said that, for one thing, patients are generally sicker now than ever before, due in part to the obesity epidemic.
Further, changing trends mean that residents are getting less exposure to some procedures like operative vaginal deliveries, while also having to learn more ways to perform hysterectomy. Residents aren’t necessarily less prepared. They’re just having to work very hard because of the depth and breadth of the required knowledge has increased, Dr. Forstein said. “There’s a lot more to learn.”
Dr. Carson agreed that the approach to education has changed, and that those changes are largely a reflection of overall shifts in education and technology.
Technology trends
Every physician interviewed for this article cited laparoscopy and robotic surgery as key technological advances. Fifty years ago, the surgical tools were simpler, Dr. Carson said. Now residents must learn four approaches to hysterectomy: vaginal, abdominal, laparoscopic, and robotic-assisted laparoscopic hysterectomy.
From ultrasound and birth control to genetic screening and robotic surgery, the evolution of the field has been astounding during this time period. The effects of the birth control pill on family planning alone forced an expansion of curriculum not only to the physiology of these things, but also to the treatment of women as a whole person and often as part of a family unit, she said.
Many of the technologies have dramatically changed the landscape, both in terms of how learning is accomplished (for example, simulation), and how physicians interact with patients, Dr. Hammond agreed. With ultrasound, for example, there was a sense that part of the physician-patient relationship was lost.
“To a point, some of us old guys felt like they were doing ultrasound assessment of patients rather than the tried-and-true ‘talk to them and examine them’ [approach],” he said. “I guess whichever generation you are in seems to be the right one, but it’s probably somewhere in between.”
Residency in 2016
If Dr. Scales is any indication, concerns about the loss of a personal touch are unfounded. She says that for her, that’s what it’s all about.
“We were exposed to [technology] since we were 5 or 6 – it’s all we know,” she said of herself and her fellow residents. “It’s not a disadvantage. It’s about efficiency.”
“We have to get things done as quickly as possible and technology helps us with that,” said Dr. Scales, the daughter of a teacher and blue collar worker, who spent most of her life “surrounded by the underprivileged.”
She always desired to help lift that population up, and while she didn’t have a draft board directing her toward public service, she had her own calling of sorts. As a premed major in college, she worked with a nonprofit organization, and later she worked with Hurricane Katrina survivors.
“I liked that aspect of medicine. I wanted to be able to identify with people on an individual level,” she said.
Technology, work-hour restrictions, gender distribution – they’re just part of the journey.
“I’m glad I chose ob.gyn.,” she said. “Sometimes you go through ... reflection ... Am I ready? My answer is yes. I’m excited about the next step, I’m comfortable in the skill I learned in my residency program, I’m excited about the work I do every day, and I’m very excited about the next chapters.”
In 1966, Dr. Charles Hammond was wrapping up a 2-year stint at the National Institutes of Health where he served at the behest of the military draft board. He had graduated from medical school just 5 years prior, and was in the middle of his ob.gyn. residency training at Duke University in Durham, N.C. when he was called to serve.
His experience wasn’t unusual for the time.
“When the draft board called, you went,” he said in an interview.
When he returned, he picked up where he left off. Residencies at that time were an “open-ended thing,” sometimes lasting 5 or 6 years, depending on staffing needs and other considerations.
Dr. Hammond, now an emeritus professor at Duke, regards his public service commission as an opportunity that advanced his academic career – despite the interruption of his residency training.
Such draft-related interruptions ended in the wake of the Vietnam War, of course, but the late 1960s and the 1970s ushered in a whole new era of changes in ob.gyn. residency training programs.
By 1968, residencies lasted 4 years, and fellowships were for 2 years. Ob.gyn. subspecialties hadn’t yet been introduced, explained Dr. Sandra A. Carson, vice president for education at the American College of Obstetricians and Gynecologists.
“That is essentially how things worked for a long time,” she said in an interview.
That’s not to say there weren’t numerous other changes taking place in the specialty. In a series of interviews with physicians and educators who discussed the myriad ways that residency training has evolved over the last 50 years, a number of themes emerged.
Women in medicine
A striking change over the past 5 decades has been the increasing number of women in medicine. Nowhere has that been in greater evidence than in obstetrics and gynecology.
“There were a few – but very few,” Dr. Hammond said of women in medicine in the 1960s.
There was “a philosophy that men did it better,” he said, adding, “That has been nicely shown to be inaccurate.”
Currently, about 80% of first-year ob.gyn. residents are women, compared with 15% in 1975.
“Maybe even 83% now,” Dr. Carson said, noting that even in the early 1980s when she was in training, women were “few and far between.”
According to a 2011 workforce report by Dr. William F. Rayburn, obstetrics and gynecology has the highest percentage of women residents of any medical specialty – 80% in 2009 versus an average of 46% for other specialties combined, and that figure has remained fairly constant.
Dr. Kasandra Scales, a fourth-year resident at the State University of New York, Syracuse, said she is glad to be part of this era of the specialty where women play an integral role in the advancement of women’s health care.
“I believe our voice and unique perspective to relate with common experiences, such as the physical birth of a child or personal choices in contraception... has enhanced our specialty,” she said.
That said, the fact that men are noticeably absent from the pool of ob.gyn. applicants and residents concerns her. “There should be a balance, she said. “I think it is important to have diversity of all types in the healthcare system.”
Dr. Hammond looked back on his days in residency training and recalled pockets of resistance to the increasing number of women in medicine, but the ultimate effect was good for the specialty, he said, explaining that the quality of the resident pool improved steadily, because the number of qualified candidates increased.
“It has been an interesting interval to watch,” he said, specifically mentioning the demands that women faced in terms of family obligations, childbirth, and childrearing.
Restrictions on work hours instituted in residency programs in more recent years may have played an important role in opening the door to more women, he said.
Work hours down, learning curve up
Dr. Carson agreed that work-hour restrictions instituted in 2003 and updated in 2011, which cap the work week at 80 hours and also apply limits on shift hours, likely encouraged more women to enter the field. One constant over the last 50 years is the biological clock, she said, explaining that the pressures and demands of residency before limits were put in place may have steered women away.
Work-hour restrictions provide more flexibility, but they aren’t without controversy.
Dr. Hammond said he sees the value in work hour restrictions, but working long hours as a resident – sometimes as many as 110 hours per week – had its benefits, too.
“I remember one time when I’d been on call for about 2 and a half days, and up and working the whole time,” Dr. Hammond said. “I left the hospital, walked out to a bench, sat down, and fell asleep. I woke up and distinctly remember thinking, ‘Why am I doing this?’ But I did do it, and that fatigue helped me with learning to endure. You learned from it.”
Not only have long hours been viewed as a rite of passage in medicine, he said, but there were concerns initially that the level of education would diminish and that the risk of patient errors would increase as patients were handed off from one shift to the next, he said.
Data on the effects of work-hour rules have been conflicting. In one study, Dr. Roger P. Smith found little overall effect on total technical experience among residents before and after the restrictions were put in place (there was no statistically significant difference in the average of median total cases in the 3 years before and after). Previous studies had documented increased costs and reduced faculty job satisfaction, while still others had shown no significant changes in 30-day readmission rates, in-hospital mortality, patient length of stay, or resident performance, he noted. “What is emerging is that both the great hopes and the great fears surrounding resident work-hour restrictions have not come to pass,” Dr. Smith wrote (Obstet Gynecol. 2010 Jun;115[6]:1166-71).
Dr. Scales, who is currently chair of the Junior Fellow District II Advisory Council for ACOG, comes down on the side of wishing for more hours.
“[The restrictions] do limit the things we can do and the exposure we may otherwise have,” she said, noting that it’s frustrating to have to leave when she’d rather stay and “see a cool case.”
“It’s a nice idea in principle, but the same amount of work has to be done. It’s not real life,” she said of work-hour restrictions. “It’s hard, at least for me, to want to give up my patients. Our job is to take in as much as you can before you leave to go out into the big bad world.”
It may be difficult to determine the actual impact of work hour limits on patient outcomes because the field of obstetrics and gynecology has changed so much over time.
Dr. David Forstein, vice chair of clinical operations in the department of obstetrics and gynecology at the University of South Carolina, Greenville, and a member of the Accreditation Council for Graduate Medical Education’s task force on work hours said that, for one thing, patients are generally sicker now than ever before, due in part to the obesity epidemic.
Further, changing trends mean that residents are getting less exposure to some procedures like operative vaginal deliveries, while also having to learn more ways to perform hysterectomy. Residents aren’t necessarily less prepared. They’re just having to work very hard because of the depth and breadth of the required knowledge has increased, Dr. Forstein said. “There’s a lot more to learn.”
Dr. Carson agreed that the approach to education has changed, and that those changes are largely a reflection of overall shifts in education and technology.
Technology trends
Every physician interviewed for this article cited laparoscopy and robotic surgery as key technological advances. Fifty years ago, the surgical tools were simpler, Dr. Carson said. Now residents must learn four approaches to hysterectomy: vaginal, abdominal, laparoscopic, and robotic-assisted laparoscopic hysterectomy.
From ultrasound and birth control to genetic screening and robotic surgery, the evolution of the field has been astounding during this time period. The effects of the birth control pill on family planning alone forced an expansion of curriculum not only to the physiology of these things, but also to the treatment of women as a whole person and often as part of a family unit, she said.
Many of the technologies have dramatically changed the landscape, both in terms of how learning is accomplished (for example, simulation), and how physicians interact with patients, Dr. Hammond agreed. With ultrasound, for example, there was a sense that part of the physician-patient relationship was lost.
“To a point, some of us old guys felt like they were doing ultrasound assessment of patients rather than the tried-and-true ‘talk to them and examine them’ [approach],” he said. “I guess whichever generation you are in seems to be the right one, but it’s probably somewhere in between.”
Residency in 2016
If Dr. Scales is any indication, concerns about the loss of a personal touch are unfounded. She says that for her, that’s what it’s all about.
“We were exposed to [technology] since we were 5 or 6 – it’s all we know,” she said of herself and her fellow residents. “It’s not a disadvantage. It’s about efficiency.”
“We have to get things done as quickly as possible and technology helps us with that,” said Dr. Scales, the daughter of a teacher and blue collar worker, who spent most of her life “surrounded by the underprivileged.”
She always desired to help lift that population up, and while she didn’t have a draft board directing her toward public service, she had her own calling of sorts. As a premed major in college, she worked with a nonprofit organization, and later she worked with Hurricane Katrina survivors.
“I liked that aspect of medicine. I wanted to be able to identify with people on an individual level,” she said.
Technology, work-hour restrictions, gender distribution – they’re just part of the journey.
“I’m glad I chose ob.gyn.,” she said. “Sometimes you go through ... reflection ... Am I ready? My answer is yes. I’m excited about the next step, I’m comfortable in the skill I learned in my residency program, I’m excited about the work I do every day, and I’m very excited about the next chapters.”