User login
PARIS – The writing is on the wall: 2-year results of the NOTION* trial suggest that transcatheter aortic valve replacement is the future – and already in selected cases, the present – preferred therapy for aortic stenosis in patients at low surgical risk.
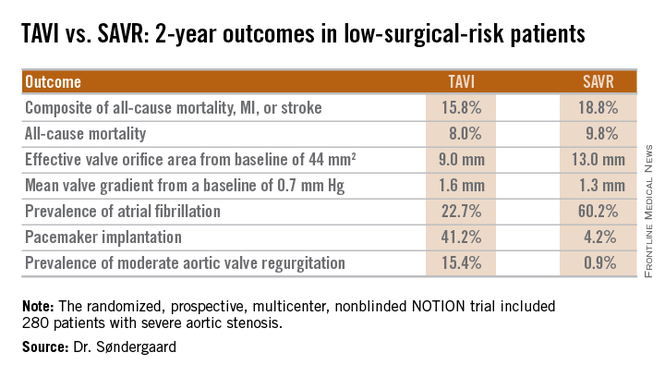
NOTION was a multicenter, prospective, nonblinded, randomized trial, the first-ever study to compare less-invasive transcatheter aortic valve implantation (TAVI, also called transcatheter aortic valve replacement, or TAVR) and traditional surgical aortic valve replacement (SAVR) in a truly low-surgical-risk population. The 280 participants had a median Society of Thoracic Surgeons score of 3 and no major comorbid conditions.
At 2 years’ follow-up, the TAVI group had significantly larger valve orifice areas and lower gradients, along with lower rates of life-threatening bleeding, cardiogenic stroke, and severe kidney injury than did the SAVR group. Moreover, the TAVI group showed a strong favorable trend in terms of the primary composite endpoint comprising all-cause mortality, MI, or stroke, although the advantage didn’t achieve statistical significance because of the relatively small study size, Dr. Lars Søndergaard said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Longer-term data on durability and more randomized controlled trials are needed before we adopt routine use of TAVI in low-risk patients, but I think it’s reasonable to offer TAVI in selected low-risk patients today,” concluded Dr. Søndergaard of the University of Copenhagen.
Session cochair Dr. William Wijns noted that NOTION, which utilized Medtronics’ self-expanding CoreValve for TAVI, began in 2009 and thus used an early iteration of the device. One might reasonably expect that the study results would be substantially more strongly in favor of TAVI had the contemporary version of the CoreValve been employed, observed Dr. Wijns, codirector of the cardiovascular center in Aalst, Belgium.
Dr. Søndergaard concurred. While the prevalence of moderate aortic regurgitation at 2 years in the TAVI arm of NOTION was 15.4%, in part because the valves were routinely placed under echocardiographic guidance, current-generation TAVI valves placed under CT guidance have a 1%-5% rate of moderate regurgitation. And while 41% of the TAVI group in NOTION had a pacemaker at 2 years, other studies show the rate drops to roughly 10% with the newest version of the CoreValve.
Dr. Søndergaard and coinvestigators plan to follow the NOTION participants for 10 years, issuing periodic updates. That’s a welcome development because patients at low surgical risk constitute the largest portion of those with significant aortic stenosis. Many of them are young enough that they should have a substantial remaining lifespan after aortic valve replacement, so it will be important to establish TAVI’s long-term durability.
The NOTION trial was funded by the Danish Heart Foundation. Dr. Søndergaard reported having no financial conflicts.
*Correction, 6/1/2015: An earlier version of this article misstated the name of the NOTION trial.
PARIS – The writing is on the wall: 2-year results of the NOTION* trial suggest that transcatheter aortic valve replacement is the future – and already in selected cases, the present – preferred therapy for aortic stenosis in patients at low surgical risk.
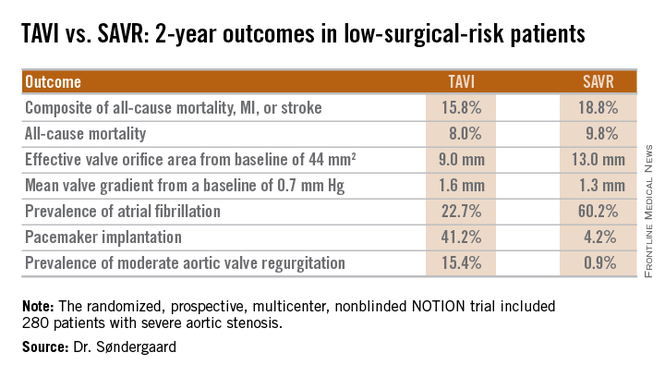
NOTION was a multicenter, prospective, nonblinded, randomized trial, the first-ever study to compare less-invasive transcatheter aortic valve implantation (TAVI, also called transcatheter aortic valve replacement, or TAVR) and traditional surgical aortic valve replacement (SAVR) in a truly low-surgical-risk population. The 280 participants had a median Society of Thoracic Surgeons score of 3 and no major comorbid conditions.
At 2 years’ follow-up, the TAVI group had significantly larger valve orifice areas and lower gradients, along with lower rates of life-threatening bleeding, cardiogenic stroke, and severe kidney injury than did the SAVR group. Moreover, the TAVI group showed a strong favorable trend in terms of the primary composite endpoint comprising all-cause mortality, MI, or stroke, although the advantage didn’t achieve statistical significance because of the relatively small study size, Dr. Lars Søndergaard said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Longer-term data on durability and more randomized controlled trials are needed before we adopt routine use of TAVI in low-risk patients, but I think it’s reasonable to offer TAVI in selected low-risk patients today,” concluded Dr. Søndergaard of the University of Copenhagen.
Session cochair Dr. William Wijns noted that NOTION, which utilized Medtronics’ self-expanding CoreValve for TAVI, began in 2009 and thus used an early iteration of the device. One might reasonably expect that the study results would be substantially more strongly in favor of TAVI had the contemporary version of the CoreValve been employed, observed Dr. Wijns, codirector of the cardiovascular center in Aalst, Belgium.
Dr. Søndergaard concurred. While the prevalence of moderate aortic regurgitation at 2 years in the TAVI arm of NOTION was 15.4%, in part because the valves were routinely placed under echocardiographic guidance, current-generation TAVI valves placed under CT guidance have a 1%-5% rate of moderate regurgitation. And while 41% of the TAVI group in NOTION had a pacemaker at 2 years, other studies show the rate drops to roughly 10% with the newest version of the CoreValve.
Dr. Søndergaard and coinvestigators plan to follow the NOTION participants for 10 years, issuing periodic updates. That’s a welcome development because patients at low surgical risk constitute the largest portion of those with significant aortic stenosis. Many of them are young enough that they should have a substantial remaining lifespan after aortic valve replacement, so it will be important to establish TAVI’s long-term durability.
The NOTION trial was funded by the Danish Heart Foundation. Dr. Søndergaard reported having no financial conflicts.
*Correction, 6/1/2015: An earlier version of this article misstated the name of the NOTION trial.
PARIS – The writing is on the wall: 2-year results of the NOTION* trial suggest that transcatheter aortic valve replacement is the future – and already in selected cases, the present – preferred therapy for aortic stenosis in patients at low surgical risk.
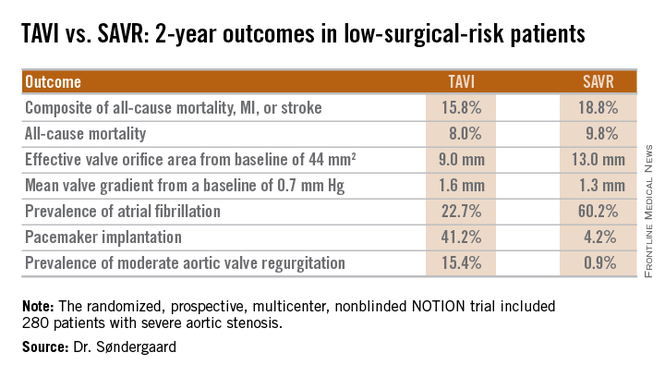
NOTION was a multicenter, prospective, nonblinded, randomized trial, the first-ever study to compare less-invasive transcatheter aortic valve implantation (TAVI, also called transcatheter aortic valve replacement, or TAVR) and traditional surgical aortic valve replacement (SAVR) in a truly low-surgical-risk population. The 280 participants had a median Society of Thoracic Surgeons score of 3 and no major comorbid conditions.
At 2 years’ follow-up, the TAVI group had significantly larger valve orifice areas and lower gradients, along with lower rates of life-threatening bleeding, cardiogenic stroke, and severe kidney injury than did the SAVR group. Moreover, the TAVI group showed a strong favorable trend in terms of the primary composite endpoint comprising all-cause mortality, MI, or stroke, although the advantage didn’t achieve statistical significance because of the relatively small study size, Dr. Lars Søndergaard said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Longer-term data on durability and more randomized controlled trials are needed before we adopt routine use of TAVI in low-risk patients, but I think it’s reasonable to offer TAVI in selected low-risk patients today,” concluded Dr. Søndergaard of the University of Copenhagen.
Session cochair Dr. William Wijns noted that NOTION, which utilized Medtronics’ self-expanding CoreValve for TAVI, began in 2009 and thus used an early iteration of the device. One might reasonably expect that the study results would be substantially more strongly in favor of TAVI had the contemporary version of the CoreValve been employed, observed Dr. Wijns, codirector of the cardiovascular center in Aalst, Belgium.
Dr. Søndergaard concurred. While the prevalence of moderate aortic regurgitation at 2 years in the TAVI arm of NOTION was 15.4%, in part because the valves were routinely placed under echocardiographic guidance, current-generation TAVI valves placed under CT guidance have a 1%-5% rate of moderate regurgitation. And while 41% of the TAVI group in NOTION had a pacemaker at 2 years, other studies show the rate drops to roughly 10% with the newest version of the CoreValve.
Dr. Søndergaard and coinvestigators plan to follow the NOTION participants for 10 years, issuing periodic updates. That’s a welcome development because patients at low surgical risk constitute the largest portion of those with significant aortic stenosis. Many of them are young enough that they should have a substantial remaining lifespan after aortic valve replacement, so it will be important to establish TAVI’s long-term durability.
The NOTION trial was funded by the Danish Heart Foundation. Dr. Søndergaard reported having no financial conflicts.
*Correction, 6/1/2015: An earlier version of this article misstated the name of the NOTION trial.
AT EUROPCR
Key clinical point: At 2 years, outcomes of TAVI look as good as and in some domains better than outcomes of surgical aortic valve replacement in low-surgical-risk patients.
Major finding: The 2-year composite outcome of all-cause mortality, MI, or stroke occurred in 15.8% of the TAVI group compared with 18.8% of surgically treated patients.
Data source: The randomized, prospective, multicenter, nonblinded NOTION trial includes 280 low-surgical-risk patients with severe aortic stenosis.
Disclosures: The NOTION trial was sponsored by the Danish Heart Foundation. The presenter reported having no financial conflicts.

