User login
• Treat a nondisplaced shaft fracture of the fifth metatarsal conservatively, with 6 to 8 weeks of immobilization with a protective orthosis. B
• Suspect a navicular fracture in patients who describe a gradual onset of vague, dorsal midfoot pain associated with athletic activity. C
• Order magnetic resonance imaging when you suspect osteochondritis dissecans, as radiographs are insensitive for identifying these lesions. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Ankle sprain, one of the more common injuries that primary care physicians evaluate, is usually managed with conservative treatment. Not uncommonly, however, lateral ankle sprain is diagnosed without consideration of a broader differential diagnosis.
Contributing to the problem is the fact that the clinical presentation of some fractures and tendon injuries is similar to that of a routine sprain. In some cases, the mechanism of injury—sprains are usually caused by excessive inversion of the ankle on a plantar-flexed foot—is similar, as well. What’s more, radiographs are often omitted or misinterpreted.
In the pages that follow, we highlight 4 commonly misdiagnosed injuries: fifth metatarsal fractures, navicular fractures, talar dome lesions, and peroneal tendon injuries. These injuries should be included in the differential diagnosis of an acute ankle injury—or a subacute foot or ankle injury that fails to respond as expected. Prompt recognition and appropriate treatment result in optimal outcomes. When foot and ankle fractures and tendon injuries are misdiagnosed (or simply missed) and do not receive adequate treatment, long-term morbidity, including frequent reinjury and disability, may result.1
Are x-rays needed? Turn to the Ottawa rules
Ankle sprains represent a disruption in a ligament supporting a joint, and result in pain, edema, and ecchymosis, and often affect a patient’s ability to bear weight. While uncomplicated sprains generally heal with conservative treatment, other common foot and ankle injuries may require a different approach.

The Ottawa foot and ankle rules are an evidence-based guide to the use of initial radiographs after acute ankle injury (TABLE 1).2-4 Pain—near the malleoli (for the ankle) or in the midfoot—is the key criterion, but x-rays are recommended only if at least one other specified criterion is also met. With a sensitivity of nearly 100%, the rules have been shown to reliably exclude, and diagnose, ankle and midfoot fractures in children >5 years and adults.2,5
Table 1
Ottawa ankle and foot rules2-4
| Ankle |
X-rays are required only if the patient has pain near the malleolus and one or more of the following:
|
| Foot |
X-rays are required only if the patient has pain in the midfoot and one or more of the following:
|
Fifth metatarsal fractures are easily missed
The mechanism of injury for a fifth metatarsal fracture is often similar to that of a lateral ankle sprain. In addition, isolated ankle radiographs may not adequately evaluate the fifth metatarsal, which increases the risk of misdiagnosis.6
3 types of fifth metatarsal fractures
Fifth metatarsal fractures involve one of the following:
- an avulsion fracture, caused by the pull of the plantar aponeurosis and the peroneus brevis tendon at the tuberosity of the bone
- a Jones fracture, at the base of the fourth and fifth metatarsal (FIGURE 1)
- a shaft fracture, distal to the fifth metatarsal joint in the proximal diaphysis.6-8
FIGURE 1
Jones fractures heal slowly
This 50-year-old patient presented with pain and swelling in the ankle and lateral foot shortly after an inversion ankle injury. A radiograph (A) taken at that time reveals a Jones fracture. The second radiograph (B) was taken 6 weeks later, after continued immobilization with no weight-bearing. Three months after the injury (C), the patient was clinically asymptomatic.
While avulsion fractures are generally the result of an inversion ankle injury, Jones fractures are usually caused by a large adductive force applied to the forefoot on a plantar-flexed ankle.6 Shaft fractures, also known as diaphyseal stress fractures, are overuse injuries from chronic overload, usually after a sudden increase in running or walking.9
Patients with fifth metatarsal fractures typically have tenderness with palpation over the area of injury, with edema and ecchymosis when the injury is acute. Evidence-based guidelines recommend x-rays of the foot, including anteroposterior (AP), lateral, and oblique views.2-4 One study supports the use of an additional x-ray—an AP view of the ankle, including the base of the fifth metatarsal—if clinical suspicion is high and initial radiographs are negative or inconclusive.10
Shaft fractures may not be seen on x-rays in the first 3 weeks, but a periosteal reaction or linear lucency near the symptomatic area may be noticeable on radiographs taken at a later date.11 If this overuse injury seems likely but does not show up on the initial x-rays, however, magnetic resonance imaging (MRI) or a technetium bone scan can reliably identify a stress fracture.9
How to treat, when to refer
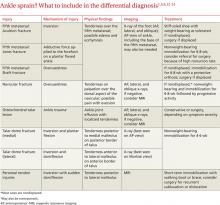
Treatment of fifth metatarsal fractures range from conservative to surgical, depending on the type (and extent) of injury (TABLE 2).1,5,6,12-14
TABLE 2
Nondisplaced avulsion fractures can be treated conservatively, with relative immobilization. In one prospective study, the use of a stiff-soled shoe, with weight-bearing as tolerated, was associated with excellent long-term outcomes.11 Orthopedic referral for probable reduction and fixation is indicated for avulsion fractures that are comminuted or >2 mm displaced, or have >30% involvement of the cubometatarsal joint.15,16
Jones fractures are known for prolonged healing and nonunion, as well as a high rate of complications. If the fracture is nondisplaced, start with conservative treatment, consisting of nonweight-bearing immobilization for 6 to 8 weeks, with additional immobilization dependent on radiographs. One randomized controlled trial of patients with Jones fractures showed a relatively high failure rate (44%) with casting; patients for whom casting was successful still had a median time to bony union of 15 weeks.17 Specialty consultation may be needed when there is fracture displacement, absence of bony union, or high clinical concern.6,17
Is your patient an athlete? Surgical fixation is favored for injured athletes with Jones fractures because failure rates are lower and both clinical union and return to play are shorter.18,19 In a case series involving 23 athletic patients with Jones fractures, the success rate for immediate surgical screw fixation approached 100% within 6 to 8 weeks.18
Nondisplaced shaft fractures may be treated conservatively, with 6 to 8 weeks of immobilization with a protective orthosis. An orthopedic referral is recommended for patients whose fractures have >3 mm displacement or >10 degree angulation.15
Navicular fractures are overuse injuries
The navicular is predisposed to stress injury because the central third of the bone is relatively avascular. In addition, the navicular is the area of greatest stress and impingement between the talus and cuneiform bones during repetitive foot strikes.12,20 Navicular fractures occur predominantly in track and field athletes.12
Patients presenting with a navicular stress fracture often report a gradual onset of vague dorsal midfoot pain associated with their workout.17 Examination typically reveals tenderness on palpation over the dorsal aspect of the navicular; passive eversion and active inversion may be painful, but edema and ecchymosis are usually absent.21
When pain is elicited by palpation of the navicular, radiographs are recommended.2,6 X-rays have a relatively low sensitivity (33%), however, for detecting acute navicular stress fractures. If initial radiographs are negative but there is a high clinical suspicion, advanced studies—with either MRI or a technetium bone scan—are recommended for a definitive diagnosis.12,22 While both are highly sensitive for navicular stress fractures, MRI provides greater specificity and anatomic detail.23
Most navicular fractures are nondisplaced
Nondisplaced navicular fractures can be treated conservatively, with nonweight-bearing immobilization for 6 to 8 weeks followed by progressive activity.24 Prospective studies have found that conservative treatment has a high success rate, with athletes usually able to return to play within 6 months.22,24,25 If tenderness remains after 6 to 8 weeks of immobilization, treatment choices are continued immobilization with no weight-bearing or orthopedic referral.26
Referral is indicated for navicular fractures that are comminuted or displaced, or involve more than one bone cortex.26 Surgical screw fixation may be recommended for navicular stress fractures in selected athletes because of its high success rate—and likelihood of an earlier return to play.27
Talar injuries are characterized by persistent pain
Injuries to the talus commonly occur at the same time as ankle sprains and may cause persistent pain, even after the sprain has healed.28 Evidence suggests that up to 90% of residual pain is related to an underlying cartilage injury.29,30 Most talar injuries are associated with the disruption of the cartilage overlaying the talar dome, which may lead to osteochondritis dissecans.29 Subtle talus fractures are also a concern after an acute ankle injury.
Osteochondral lesions are associated with a dull ankle pain deep in a location with a prior ankle injury; in some cases, the pain will become chronic.31 Physical exam findings typically include ankle joint effusion with localized tenderness around the joint.31
Ankle radiographs are insensitive for identifying osteochondral lesions, and MRI is recommended for evaluating suspected lesions.29,31 Treatment varies, depending on symptoms and severity. Patients with minimal symptoms may be treated conservatively; however, high failure rates have been reported.32 Surgical treatment depends on the size and site of the lesion and the degree of cartilage injury, and surgical consultation is recommended.31
Fractures of the talar dome (FIGURE 2) may be either medial or lateral and are often the result of inversion ankle injuries.14 History and clinical findings vary depending on the type of fracture.
FIGURE 2
Talar dome injuries often result from inversion ankle injuries
As with osteochondral lesions, ankle radiographs may fail to identify talus fractures. Computed tomography (CT) should be used to evaluate acute fractures of the talus, as CT scan is better able to define displacement, size, and intra-articular involvement.33 Talar fractures may be managed conservatively with immobilization and nonweight-bearing for 4 to 6 weeks, but specialty consultation should be considered.14,33
A tarsal coalition—an incomplete, congenital separation of the bones, occasionally involving the talus and the calcaneus—can also be a cause of persistent pain after a sprain.28 Physical exam typically demonstrates decreased range of motion in the subtalar or transverse tarsal joint. Radiographs may identify the coalition, but MRI or CT scan provides optimal visualization. Immobilization for 6 weeks is the recommended initial treatment, but if that fails, surgical excision or fusion may be necessary.
Peroneal tendon injuries may cause ankle instability
Peroneal tendon injuries, which include strains, subluxation, dislocation, and tears of one or both of the peroneal tendons, are often caused by ankle inversion similar to that of an uncomplicated sprain. Subsequent ankle instability may result from untreated peroneal tendon injuries.34 Peroneal tendon subluxation accounts for a very small number (0.3%-0.5%) of traumatic ankle injuries.35
Peroneal tendon injuries often occur during sports that involve frequent lateral movement or cutting—eg, football, basketball, and soccer—and are often caused by sudden dorsiflexion of the inverted foot, with coincident contraction of the peroneal muscles.36,37 This mechanism can disrupt the superior peroneal retinaculum, leading to recurrent subluxation or dislocation and subsequent ankle instability.36,38 Chronic subluxation can also result in longitudinal tears of the peroneal tendons, especially of the peroneus brevis.36,38,39
Patients with peroneal tendon injuries may report a “pop” at the time of injury. Pain is typically located posterior to the lateral malleolus, and recurrent subluxation is often described as a “snapping” around the lateral ankle during athletic activities.37,38 Instability is common in patients with subacute or chronic peroneal tendon injuries, especially on uneven surfaces.38
Acute peroneal tendon injuries cause posterolateral ankle pain, swelling, and weakness; exam findings include tenderness along the course of the peroneal tendons with associated edema.37 Subluxation or dislocation of the peroneal brevis tendon may be confirmed by placing the foot in plantar flexion and inversion and asking the patient to forcibly dorsiflex and evert the injured ankle.
Plain radiographs are usually normal in an isolated injury to the peroneal tendons. A fracture of the posterolateral margin of the fibula is a rare finding but indicates disruption of the peroneal retinaculum.36 MRI provides the best imaging for peroneal tendons and the stabilizing retinaculum, although a CT scan can provide detailed bony anatomy when subtle fractures are suspected or additional evaluation is needed.
Subluxation or dislocation indicate a need for surgery
Conservative management is recommended for peroneal tendon strains, but surgical treatment is increasingly recommended for subluxation or dislocation, especially if the problem is recurrent.36,37 Conservative treatment consists of short-term immobilization with a walking boot or brace, followed by physical therapy to improve strength and motion. Surgical treatment of subluxation and dislocation by stabilizing the peroneal tendons within the peroneal groove has been shown to provide lasting stability and improvement.37,38,40,41
CORRESPONDENCE Scott Hall, MD, University of Nevada-Reno, Brigham Building 316, Reno, NV 89557; [email protected]
1. van Rijn RM, van Os AG, Bernsen RM, et al. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008;121:324-331.
2. Nugent PJ. Ottawa ankle rules accurately assess injuries and reduce reliance on radiographs. J Fam Pract. 2004;53:785-788.
3. Stiell IG, McKnight RD, Greenberg GH, et al. Implementation of the Ottawa ankle rules. JAMA. 1994;271:827-832.
4. Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. JAMA. 1993;269:1127-1132.
5. Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002;66:785-795.
6. Den Hartog BD. Fracture of the proximal fifth metatarsal. J Am Acad Orthop Surg. 2009;17:458-464.
7. Torg JS, Balduini FC, Zelko RR, et al. Fractures of the base of the fifth metatarsal distal to the tuberosity. J Bone Joint Surg Am. 1984;66:209-214.
8. Dameron TB. Fractures and anatomical variations of the proximal portion of the fifth metatarsal. J Bone Joint Surg Am. 1975;57:788-792.
9. Boden BP, Oshbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29:100-113.
10. Pao DG. Avulsion fracture of the base of the fifth metatarsal not seen on conventional radiography of the foot: the need for an additional projection. Am J Roentgenol. 2000;175:549-552.
11. Egol K. Avulsion fractures of the fifth metatarsal base: a prospective outcome study. Foot Ankle Int. 2007;28:581-583.
12. Jones MH, Amendola AS. Navicular stress fractures. Clin Sports Med. 2006;25:151-158.
13. Fitch KD, Blackwell JB, Gilmour WN. Operation for non-union of stress fracture of the tarsal navicular. J Bone Joint Surg Br. 1989;71:105-110.
14. Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002;66:785-794.
15. Zwitser EW, Breederveld BS. Fractures of the fifth metatarsal; diagnosis and treatment. Injury. 2010;41:555-562.
16. Koslowsky TC, Gausepohl T, Mader K, et al. Treatment of displaced proximal fifth metatarsal fractures using a new one-step fixation technique. J Trauma. 2010;68:122-125.
17. Mologne TS. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 2005;33:970-975.
18. Porter DA, Duncan M, Meyer SJF. Fifth metatarsal Jones fracture fixation with a 4.5-mm cannulated stainless steel screw in the competitive and recreational athlete. Am J Sports Med. 2005;33:726-733.
19. Vu D, McDiarmid T, Brown M. What is the most effective management of acute fractures of the base of the fifth metatarsal? J Fam Pract. 2006;55:713-717.
20. Monteleone GP. Stress fractures in the athlete. Orthop Clin North Am. 1995;26:423-432.
21. Torg JS, Pavlov H, Cooley LH, et al. Stress fractures of the tarsal navicular. A retrospective review of twenty-one cases. J Bone Joint Surg Am. 1982;64:700-712.
22. Khan KM, Fuller PJ, Brukner PD, et al. Outcome of conservative and surgical management of navicular stress fracture in athletes. Eighty-six cases proven with computerized tomography. Am J Sports Med. 1992;20:657-666.
23. Sizensky JA, Marks RM. Imaging of the navicular. Foot Ankle Clin. 2004;9:181-209.
24. Torg JS, Moyer J, Gaughan JP, et al. Management of tarsal navicular stress fractures: conservative versus surgical treatment: a meta-analysis. Am J Sports Med. 2010;38:1048-1053.
25. Bojanic I. Conservative treatment of stress fractures of the tarsal navicular in athletes. Rev Chir Orthop Reparatrice Appar Mot. 1997;83:133-138.
26. Ostlie DK, Simons SM. Tarsal navicular stress fracture in a young athlete: case report with clinical, radiologic, and pathophysiologic correlations. J Am Board Fam Pract. 2001;14:381-385.
27. Towne LC, Blazina ME, Cozen LN. Fatigue fracture of the tarsal navicular. J Bone Joint Surg Am. 1970;52:376-378.
28. Strauss JE, Fornberg JA, Lippert FG. Chronic lateral ankle instability and associated conditions: a rationale for treatment. Foot Ankle Int. 2007;28:1041-1044.
29. Schachter AK, Chen AL, Reddy PD, et al. Osteochondral lesions of the talus. J Am Acad Orthop Surg. 2005;13:152-158.
30. Taga I, Shino K, Inoue M, et al. Articular cartilage lesion in ankles with lateral ligament injury. Am J Sport Med. 1993;21:120-127.
31. O’Loughlin PF, Heyworth BE, Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010;38:392-404.
32. Shearer C, Loomer R, Clement D. Nonoperatively managed stage 5 osteochondral talar lesions. Foot Ankle Int. 2002;23:651-654.
33. Haverstock BD. Foot and ankle imaging in the athlete. Clin Podiatr Med Surg. 2008;25:249-262.
34. Geppert M, Sobel M, Bohne W. Lateral ankle instability as a cause of superior peroneal retinacular laxity: an anatomic and biomechanical study of cadaveric feet. Foot Ankle. 1993;14:330-334.
35. Butler BW, Lanthier J, Wertheimer SJ. Subluxing peroneals: a review of the literature and case report. J Foot Ankle Surg. 1993;32:134-139.
36. Roth JA, Taylor WC, Whalen J. Peroneal tendon subluxation: the other lateral ankle injury. Br J Sports Med. 2010;44:1047-1053.
37. Maffulli N, Ferran NA, Oliva F, et al. Recurrent subluxation of the peroneal tendons. Am J Sports Med. 2006;34:986-992.
38. Mason RB, Henderson JP. Traumatic peroneal tendon instability. Am J Sports Med. 1996;24:652-658.
39. Brodsky J, Krause J. Peroneus brevis tendon tears: pathophysiology, surgical reconstruction, and clinical results. Foot Ankle Int. 1998;19:271-279.
40. Marten MA, Noyez JF, Mulier JC. Recurrent dislocation of the peroneal tendons. Results of rerouting the tendons under the calcaneofibular ligament. Am J Sports Med. 1986;14:148-150.
41. Escalas F, Figueras JM, Merino JA. Dislocation of the peroneal tendons. Long-term results of surgical treatment. J Bone Joint Surg Am. 1980;62:451-453.
• Treat a nondisplaced shaft fracture of the fifth metatarsal conservatively, with 6 to 8 weeks of immobilization with a protective orthosis. B
• Suspect a navicular fracture in patients who describe a gradual onset of vague, dorsal midfoot pain associated with athletic activity. C
• Order magnetic resonance imaging when you suspect osteochondritis dissecans, as radiographs are insensitive for identifying these lesions. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Ankle sprain, one of the more common injuries that primary care physicians evaluate, is usually managed with conservative treatment. Not uncommonly, however, lateral ankle sprain is diagnosed without consideration of a broader differential diagnosis.
Contributing to the problem is the fact that the clinical presentation of some fractures and tendon injuries is similar to that of a routine sprain. In some cases, the mechanism of injury—sprains are usually caused by excessive inversion of the ankle on a plantar-flexed foot—is similar, as well. What’s more, radiographs are often omitted or misinterpreted.
In the pages that follow, we highlight 4 commonly misdiagnosed injuries: fifth metatarsal fractures, navicular fractures, talar dome lesions, and peroneal tendon injuries. These injuries should be included in the differential diagnosis of an acute ankle injury—or a subacute foot or ankle injury that fails to respond as expected. Prompt recognition and appropriate treatment result in optimal outcomes. When foot and ankle fractures and tendon injuries are misdiagnosed (or simply missed) and do not receive adequate treatment, long-term morbidity, including frequent reinjury and disability, may result.1
Are x-rays needed? Turn to the Ottawa rules
Ankle sprains represent a disruption in a ligament supporting a joint, and result in pain, edema, and ecchymosis, and often affect a patient’s ability to bear weight. While uncomplicated sprains generally heal with conservative treatment, other common foot and ankle injuries may require a different approach.

The Ottawa foot and ankle rules are an evidence-based guide to the use of initial radiographs after acute ankle injury (TABLE 1).2-4 Pain—near the malleoli (for the ankle) or in the midfoot—is the key criterion, but x-rays are recommended only if at least one other specified criterion is also met. With a sensitivity of nearly 100%, the rules have been shown to reliably exclude, and diagnose, ankle and midfoot fractures in children >5 years and adults.2,5
Table 1
Ottawa ankle and foot rules2-4
| Ankle |
X-rays are required only if the patient has pain near the malleolus and one or more of the following:
|
| Foot |
X-rays are required only if the patient has pain in the midfoot and one or more of the following:
|
Fifth metatarsal fractures are easily missed
The mechanism of injury for a fifth metatarsal fracture is often similar to that of a lateral ankle sprain. In addition, isolated ankle radiographs may not adequately evaluate the fifth metatarsal, which increases the risk of misdiagnosis.6
3 types of fifth metatarsal fractures
Fifth metatarsal fractures involve one of the following:
- an avulsion fracture, caused by the pull of the plantar aponeurosis and the peroneus brevis tendon at the tuberosity of the bone
- a Jones fracture, at the base of the fourth and fifth metatarsal (FIGURE 1)
- a shaft fracture, distal to the fifth metatarsal joint in the proximal diaphysis.6-8
FIGURE 1
Jones fractures heal slowly
This 50-year-old patient presented with pain and swelling in the ankle and lateral foot shortly after an inversion ankle injury. A radiograph (A) taken at that time reveals a Jones fracture. The second radiograph (B) was taken 6 weeks later, after continued immobilization with no weight-bearing. Three months after the injury (C), the patient was clinically asymptomatic.
While avulsion fractures are generally the result of an inversion ankle injury, Jones fractures are usually caused by a large adductive force applied to the forefoot on a plantar-flexed ankle.6 Shaft fractures, also known as diaphyseal stress fractures, are overuse injuries from chronic overload, usually after a sudden increase in running or walking.9
Patients with fifth metatarsal fractures typically have tenderness with palpation over the area of injury, with edema and ecchymosis when the injury is acute. Evidence-based guidelines recommend x-rays of the foot, including anteroposterior (AP), lateral, and oblique views.2-4 One study supports the use of an additional x-ray—an AP view of the ankle, including the base of the fifth metatarsal—if clinical suspicion is high and initial radiographs are negative or inconclusive.10
Shaft fractures may not be seen on x-rays in the first 3 weeks, but a periosteal reaction or linear lucency near the symptomatic area may be noticeable on radiographs taken at a later date.11 If this overuse injury seems likely but does not show up on the initial x-rays, however, magnetic resonance imaging (MRI) or a technetium bone scan can reliably identify a stress fracture.9
How to treat, when to refer
Treatment of fifth metatarsal fractures range from conservative to surgical, depending on the type (and extent) of injury (TABLE 2).1,5,6,12-14
TABLE 2
Nondisplaced avulsion fractures can be treated conservatively, with relative immobilization. In one prospective study, the use of a stiff-soled shoe, with weight-bearing as tolerated, was associated with excellent long-term outcomes.11 Orthopedic referral for probable reduction and fixation is indicated for avulsion fractures that are comminuted or >2 mm displaced, or have >30% involvement of the cubometatarsal joint.15,16
Jones fractures are known for prolonged healing and nonunion, as well as a high rate of complications. If the fracture is nondisplaced, start with conservative treatment, consisting of nonweight-bearing immobilization for 6 to 8 weeks, with additional immobilization dependent on radiographs. One randomized controlled trial of patients with Jones fractures showed a relatively high failure rate (44%) with casting; patients for whom casting was successful still had a median time to bony union of 15 weeks.17 Specialty consultation may be needed when there is fracture displacement, absence of bony union, or high clinical concern.6,17
Is your patient an athlete? Surgical fixation is favored for injured athletes with Jones fractures because failure rates are lower and both clinical union and return to play are shorter.18,19 In a case series involving 23 athletic patients with Jones fractures, the success rate for immediate surgical screw fixation approached 100% within 6 to 8 weeks.18
Nondisplaced shaft fractures may be treated conservatively, with 6 to 8 weeks of immobilization with a protective orthosis. An orthopedic referral is recommended for patients whose fractures have >3 mm displacement or >10 degree angulation.15
Navicular fractures are overuse injuries
The navicular is predisposed to stress injury because the central third of the bone is relatively avascular. In addition, the navicular is the area of greatest stress and impingement between the talus and cuneiform bones during repetitive foot strikes.12,20 Navicular fractures occur predominantly in track and field athletes.12
Patients presenting with a navicular stress fracture often report a gradual onset of vague dorsal midfoot pain associated with their workout.17 Examination typically reveals tenderness on palpation over the dorsal aspect of the navicular; passive eversion and active inversion may be painful, but edema and ecchymosis are usually absent.21
When pain is elicited by palpation of the navicular, radiographs are recommended.2,6 X-rays have a relatively low sensitivity (33%), however, for detecting acute navicular stress fractures. If initial radiographs are negative but there is a high clinical suspicion, advanced studies—with either MRI or a technetium bone scan—are recommended for a definitive diagnosis.12,22 While both are highly sensitive for navicular stress fractures, MRI provides greater specificity and anatomic detail.23
Most navicular fractures are nondisplaced
Nondisplaced navicular fractures can be treated conservatively, with nonweight-bearing immobilization for 6 to 8 weeks followed by progressive activity.24 Prospective studies have found that conservative treatment has a high success rate, with athletes usually able to return to play within 6 months.22,24,25 If tenderness remains after 6 to 8 weeks of immobilization, treatment choices are continued immobilization with no weight-bearing or orthopedic referral.26
Referral is indicated for navicular fractures that are comminuted or displaced, or involve more than one bone cortex.26 Surgical screw fixation may be recommended for navicular stress fractures in selected athletes because of its high success rate—and likelihood of an earlier return to play.27
Talar injuries are characterized by persistent pain
Injuries to the talus commonly occur at the same time as ankle sprains and may cause persistent pain, even after the sprain has healed.28 Evidence suggests that up to 90% of residual pain is related to an underlying cartilage injury.29,30 Most talar injuries are associated with the disruption of the cartilage overlaying the talar dome, which may lead to osteochondritis dissecans.29 Subtle talus fractures are also a concern after an acute ankle injury.
Osteochondral lesions are associated with a dull ankle pain deep in a location with a prior ankle injury; in some cases, the pain will become chronic.31 Physical exam findings typically include ankle joint effusion with localized tenderness around the joint.31
Ankle radiographs are insensitive for identifying osteochondral lesions, and MRI is recommended for evaluating suspected lesions.29,31 Treatment varies, depending on symptoms and severity. Patients with minimal symptoms may be treated conservatively; however, high failure rates have been reported.32 Surgical treatment depends on the size and site of the lesion and the degree of cartilage injury, and surgical consultation is recommended.31
Fractures of the talar dome (FIGURE 2) may be either medial or lateral and are often the result of inversion ankle injuries.14 History and clinical findings vary depending on the type of fracture.
FIGURE 2
Talar dome injuries often result from inversion ankle injuries
As with osteochondral lesions, ankle radiographs may fail to identify talus fractures. Computed tomography (CT) should be used to evaluate acute fractures of the talus, as CT scan is better able to define displacement, size, and intra-articular involvement.33 Talar fractures may be managed conservatively with immobilization and nonweight-bearing for 4 to 6 weeks, but specialty consultation should be considered.14,33
A tarsal coalition—an incomplete, congenital separation of the bones, occasionally involving the talus and the calcaneus—can also be a cause of persistent pain after a sprain.28 Physical exam typically demonstrates decreased range of motion in the subtalar or transverse tarsal joint. Radiographs may identify the coalition, but MRI or CT scan provides optimal visualization. Immobilization for 6 weeks is the recommended initial treatment, but if that fails, surgical excision or fusion may be necessary.
Peroneal tendon injuries may cause ankle instability
Peroneal tendon injuries, which include strains, subluxation, dislocation, and tears of one or both of the peroneal tendons, are often caused by ankle inversion similar to that of an uncomplicated sprain. Subsequent ankle instability may result from untreated peroneal tendon injuries.34 Peroneal tendon subluxation accounts for a very small number (0.3%-0.5%) of traumatic ankle injuries.35
Peroneal tendon injuries often occur during sports that involve frequent lateral movement or cutting—eg, football, basketball, and soccer—and are often caused by sudden dorsiflexion of the inverted foot, with coincident contraction of the peroneal muscles.36,37 This mechanism can disrupt the superior peroneal retinaculum, leading to recurrent subluxation or dislocation and subsequent ankle instability.36,38 Chronic subluxation can also result in longitudinal tears of the peroneal tendons, especially of the peroneus brevis.36,38,39
Patients with peroneal tendon injuries may report a “pop” at the time of injury. Pain is typically located posterior to the lateral malleolus, and recurrent subluxation is often described as a “snapping” around the lateral ankle during athletic activities.37,38 Instability is common in patients with subacute or chronic peroneal tendon injuries, especially on uneven surfaces.38
Acute peroneal tendon injuries cause posterolateral ankle pain, swelling, and weakness; exam findings include tenderness along the course of the peroneal tendons with associated edema.37 Subluxation or dislocation of the peroneal brevis tendon may be confirmed by placing the foot in plantar flexion and inversion and asking the patient to forcibly dorsiflex and evert the injured ankle.
Plain radiographs are usually normal in an isolated injury to the peroneal tendons. A fracture of the posterolateral margin of the fibula is a rare finding but indicates disruption of the peroneal retinaculum.36 MRI provides the best imaging for peroneal tendons and the stabilizing retinaculum, although a CT scan can provide detailed bony anatomy when subtle fractures are suspected or additional evaluation is needed.
Subluxation or dislocation indicate a need for surgery
Conservative management is recommended for peroneal tendon strains, but surgical treatment is increasingly recommended for subluxation or dislocation, especially if the problem is recurrent.36,37 Conservative treatment consists of short-term immobilization with a walking boot or brace, followed by physical therapy to improve strength and motion. Surgical treatment of subluxation and dislocation by stabilizing the peroneal tendons within the peroneal groove has been shown to provide lasting stability and improvement.37,38,40,41
CORRESPONDENCE Scott Hall, MD, University of Nevada-Reno, Brigham Building 316, Reno, NV 89557; [email protected]
• Treat a nondisplaced shaft fracture of the fifth metatarsal conservatively, with 6 to 8 weeks of immobilization with a protective orthosis. B
• Suspect a navicular fracture in patients who describe a gradual onset of vague, dorsal midfoot pain associated with athletic activity. C
• Order magnetic resonance imaging when you suspect osteochondritis dissecans, as radiographs are insensitive for identifying these lesions. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Ankle sprain, one of the more common injuries that primary care physicians evaluate, is usually managed with conservative treatment. Not uncommonly, however, lateral ankle sprain is diagnosed without consideration of a broader differential diagnosis.
Contributing to the problem is the fact that the clinical presentation of some fractures and tendon injuries is similar to that of a routine sprain. In some cases, the mechanism of injury—sprains are usually caused by excessive inversion of the ankle on a plantar-flexed foot—is similar, as well. What’s more, radiographs are often omitted or misinterpreted.
In the pages that follow, we highlight 4 commonly misdiagnosed injuries: fifth metatarsal fractures, navicular fractures, talar dome lesions, and peroneal tendon injuries. These injuries should be included in the differential diagnosis of an acute ankle injury—or a subacute foot or ankle injury that fails to respond as expected. Prompt recognition and appropriate treatment result in optimal outcomes. When foot and ankle fractures and tendon injuries are misdiagnosed (or simply missed) and do not receive adequate treatment, long-term morbidity, including frequent reinjury and disability, may result.1
Are x-rays needed? Turn to the Ottawa rules
Ankle sprains represent a disruption in a ligament supporting a joint, and result in pain, edema, and ecchymosis, and often affect a patient’s ability to bear weight. While uncomplicated sprains generally heal with conservative treatment, other common foot and ankle injuries may require a different approach.

The Ottawa foot and ankle rules are an evidence-based guide to the use of initial radiographs after acute ankle injury (TABLE 1).2-4 Pain—near the malleoli (for the ankle) or in the midfoot—is the key criterion, but x-rays are recommended only if at least one other specified criterion is also met. With a sensitivity of nearly 100%, the rules have been shown to reliably exclude, and diagnose, ankle and midfoot fractures in children >5 years and adults.2,5
Table 1
Ottawa ankle and foot rules2-4
| Ankle |
X-rays are required only if the patient has pain near the malleolus and one or more of the following:
|
| Foot |
X-rays are required only if the patient has pain in the midfoot and one or more of the following:
|
Fifth metatarsal fractures are easily missed
The mechanism of injury for a fifth metatarsal fracture is often similar to that of a lateral ankle sprain. In addition, isolated ankle radiographs may not adequately evaluate the fifth metatarsal, which increases the risk of misdiagnosis.6
3 types of fifth metatarsal fractures
Fifth metatarsal fractures involve one of the following:
- an avulsion fracture, caused by the pull of the plantar aponeurosis and the peroneus brevis tendon at the tuberosity of the bone
- a Jones fracture, at the base of the fourth and fifth metatarsal (FIGURE 1)
- a shaft fracture, distal to the fifth metatarsal joint in the proximal diaphysis.6-8
FIGURE 1
Jones fractures heal slowly
This 50-year-old patient presented with pain and swelling in the ankle and lateral foot shortly after an inversion ankle injury. A radiograph (A) taken at that time reveals a Jones fracture. The second radiograph (B) was taken 6 weeks later, after continued immobilization with no weight-bearing. Three months after the injury (C), the patient was clinically asymptomatic.
While avulsion fractures are generally the result of an inversion ankle injury, Jones fractures are usually caused by a large adductive force applied to the forefoot on a plantar-flexed ankle.6 Shaft fractures, also known as diaphyseal stress fractures, are overuse injuries from chronic overload, usually after a sudden increase in running or walking.9
Patients with fifth metatarsal fractures typically have tenderness with palpation over the area of injury, with edema and ecchymosis when the injury is acute. Evidence-based guidelines recommend x-rays of the foot, including anteroposterior (AP), lateral, and oblique views.2-4 One study supports the use of an additional x-ray—an AP view of the ankle, including the base of the fifth metatarsal—if clinical suspicion is high and initial radiographs are negative or inconclusive.10
Shaft fractures may not be seen on x-rays in the first 3 weeks, but a periosteal reaction or linear lucency near the symptomatic area may be noticeable on radiographs taken at a later date.11 If this overuse injury seems likely but does not show up on the initial x-rays, however, magnetic resonance imaging (MRI) or a technetium bone scan can reliably identify a stress fracture.9
How to treat, when to refer
Treatment of fifth metatarsal fractures range from conservative to surgical, depending on the type (and extent) of injury (TABLE 2).1,5,6,12-14
TABLE 2
Nondisplaced avulsion fractures can be treated conservatively, with relative immobilization. In one prospective study, the use of a stiff-soled shoe, with weight-bearing as tolerated, was associated with excellent long-term outcomes.11 Orthopedic referral for probable reduction and fixation is indicated for avulsion fractures that are comminuted or >2 mm displaced, or have >30% involvement of the cubometatarsal joint.15,16
Jones fractures are known for prolonged healing and nonunion, as well as a high rate of complications. If the fracture is nondisplaced, start with conservative treatment, consisting of nonweight-bearing immobilization for 6 to 8 weeks, with additional immobilization dependent on radiographs. One randomized controlled trial of patients with Jones fractures showed a relatively high failure rate (44%) with casting; patients for whom casting was successful still had a median time to bony union of 15 weeks.17 Specialty consultation may be needed when there is fracture displacement, absence of bony union, or high clinical concern.6,17
Is your patient an athlete? Surgical fixation is favored for injured athletes with Jones fractures because failure rates are lower and both clinical union and return to play are shorter.18,19 In a case series involving 23 athletic patients with Jones fractures, the success rate for immediate surgical screw fixation approached 100% within 6 to 8 weeks.18
Nondisplaced shaft fractures may be treated conservatively, with 6 to 8 weeks of immobilization with a protective orthosis. An orthopedic referral is recommended for patients whose fractures have >3 mm displacement or >10 degree angulation.15
Navicular fractures are overuse injuries
The navicular is predisposed to stress injury because the central third of the bone is relatively avascular. In addition, the navicular is the area of greatest stress and impingement between the talus and cuneiform bones during repetitive foot strikes.12,20 Navicular fractures occur predominantly in track and field athletes.12
Patients presenting with a navicular stress fracture often report a gradual onset of vague dorsal midfoot pain associated with their workout.17 Examination typically reveals tenderness on palpation over the dorsal aspect of the navicular; passive eversion and active inversion may be painful, but edema and ecchymosis are usually absent.21
When pain is elicited by palpation of the navicular, radiographs are recommended.2,6 X-rays have a relatively low sensitivity (33%), however, for detecting acute navicular stress fractures. If initial radiographs are negative but there is a high clinical suspicion, advanced studies—with either MRI or a technetium bone scan—are recommended for a definitive diagnosis.12,22 While both are highly sensitive for navicular stress fractures, MRI provides greater specificity and anatomic detail.23
Most navicular fractures are nondisplaced
Nondisplaced navicular fractures can be treated conservatively, with nonweight-bearing immobilization for 6 to 8 weeks followed by progressive activity.24 Prospective studies have found that conservative treatment has a high success rate, with athletes usually able to return to play within 6 months.22,24,25 If tenderness remains after 6 to 8 weeks of immobilization, treatment choices are continued immobilization with no weight-bearing or orthopedic referral.26
Referral is indicated for navicular fractures that are comminuted or displaced, or involve more than one bone cortex.26 Surgical screw fixation may be recommended for navicular stress fractures in selected athletes because of its high success rate—and likelihood of an earlier return to play.27
Talar injuries are characterized by persistent pain
Injuries to the talus commonly occur at the same time as ankle sprains and may cause persistent pain, even after the sprain has healed.28 Evidence suggests that up to 90% of residual pain is related to an underlying cartilage injury.29,30 Most talar injuries are associated with the disruption of the cartilage overlaying the talar dome, which may lead to osteochondritis dissecans.29 Subtle talus fractures are also a concern after an acute ankle injury.
Osteochondral lesions are associated with a dull ankle pain deep in a location with a prior ankle injury; in some cases, the pain will become chronic.31 Physical exam findings typically include ankle joint effusion with localized tenderness around the joint.31
Ankle radiographs are insensitive for identifying osteochondral lesions, and MRI is recommended for evaluating suspected lesions.29,31 Treatment varies, depending on symptoms and severity. Patients with minimal symptoms may be treated conservatively; however, high failure rates have been reported.32 Surgical treatment depends on the size and site of the lesion and the degree of cartilage injury, and surgical consultation is recommended.31
Fractures of the talar dome (FIGURE 2) may be either medial or lateral and are often the result of inversion ankle injuries.14 History and clinical findings vary depending on the type of fracture.
FIGURE 2
Talar dome injuries often result from inversion ankle injuries
As with osteochondral lesions, ankle radiographs may fail to identify talus fractures. Computed tomography (CT) should be used to evaluate acute fractures of the talus, as CT scan is better able to define displacement, size, and intra-articular involvement.33 Talar fractures may be managed conservatively with immobilization and nonweight-bearing for 4 to 6 weeks, but specialty consultation should be considered.14,33
A tarsal coalition—an incomplete, congenital separation of the bones, occasionally involving the talus and the calcaneus—can also be a cause of persistent pain after a sprain.28 Physical exam typically demonstrates decreased range of motion in the subtalar or transverse tarsal joint. Radiographs may identify the coalition, but MRI or CT scan provides optimal visualization. Immobilization for 6 weeks is the recommended initial treatment, but if that fails, surgical excision or fusion may be necessary.
Peroneal tendon injuries may cause ankle instability
Peroneal tendon injuries, which include strains, subluxation, dislocation, and tears of one or both of the peroneal tendons, are often caused by ankle inversion similar to that of an uncomplicated sprain. Subsequent ankle instability may result from untreated peroneal tendon injuries.34 Peroneal tendon subluxation accounts for a very small number (0.3%-0.5%) of traumatic ankle injuries.35
Peroneal tendon injuries often occur during sports that involve frequent lateral movement or cutting—eg, football, basketball, and soccer—and are often caused by sudden dorsiflexion of the inverted foot, with coincident contraction of the peroneal muscles.36,37 This mechanism can disrupt the superior peroneal retinaculum, leading to recurrent subluxation or dislocation and subsequent ankle instability.36,38 Chronic subluxation can also result in longitudinal tears of the peroneal tendons, especially of the peroneus brevis.36,38,39
Patients with peroneal tendon injuries may report a “pop” at the time of injury. Pain is typically located posterior to the lateral malleolus, and recurrent subluxation is often described as a “snapping” around the lateral ankle during athletic activities.37,38 Instability is common in patients with subacute or chronic peroneal tendon injuries, especially on uneven surfaces.38
Acute peroneal tendon injuries cause posterolateral ankle pain, swelling, and weakness; exam findings include tenderness along the course of the peroneal tendons with associated edema.37 Subluxation or dislocation of the peroneal brevis tendon may be confirmed by placing the foot in plantar flexion and inversion and asking the patient to forcibly dorsiflex and evert the injured ankle.
Plain radiographs are usually normal in an isolated injury to the peroneal tendons. A fracture of the posterolateral margin of the fibula is a rare finding but indicates disruption of the peroneal retinaculum.36 MRI provides the best imaging for peroneal tendons and the stabilizing retinaculum, although a CT scan can provide detailed bony anatomy when subtle fractures are suspected or additional evaluation is needed.
Subluxation or dislocation indicate a need for surgery
Conservative management is recommended for peroneal tendon strains, but surgical treatment is increasingly recommended for subluxation or dislocation, especially if the problem is recurrent.36,37 Conservative treatment consists of short-term immobilization with a walking boot or brace, followed by physical therapy to improve strength and motion. Surgical treatment of subluxation and dislocation by stabilizing the peroneal tendons within the peroneal groove has been shown to provide lasting stability and improvement.37,38,40,41
CORRESPONDENCE Scott Hall, MD, University of Nevada-Reno, Brigham Building 316, Reno, NV 89557; [email protected]
1. van Rijn RM, van Os AG, Bernsen RM, et al. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008;121:324-331.
2. Nugent PJ. Ottawa ankle rules accurately assess injuries and reduce reliance on radiographs. J Fam Pract. 2004;53:785-788.
3. Stiell IG, McKnight RD, Greenberg GH, et al. Implementation of the Ottawa ankle rules. JAMA. 1994;271:827-832.
4. Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. JAMA. 1993;269:1127-1132.
5. Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002;66:785-795.
6. Den Hartog BD. Fracture of the proximal fifth metatarsal. J Am Acad Orthop Surg. 2009;17:458-464.
7. Torg JS, Balduini FC, Zelko RR, et al. Fractures of the base of the fifth metatarsal distal to the tuberosity. J Bone Joint Surg Am. 1984;66:209-214.
8. Dameron TB. Fractures and anatomical variations of the proximal portion of the fifth metatarsal. J Bone Joint Surg Am. 1975;57:788-792.
9. Boden BP, Oshbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29:100-113.
10. Pao DG. Avulsion fracture of the base of the fifth metatarsal not seen on conventional radiography of the foot: the need for an additional projection. Am J Roentgenol. 2000;175:549-552.
11. Egol K. Avulsion fractures of the fifth metatarsal base: a prospective outcome study. Foot Ankle Int. 2007;28:581-583.
12. Jones MH, Amendola AS. Navicular stress fractures. Clin Sports Med. 2006;25:151-158.
13. Fitch KD, Blackwell JB, Gilmour WN. Operation for non-union of stress fracture of the tarsal navicular. J Bone Joint Surg Br. 1989;71:105-110.
14. Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002;66:785-794.
15. Zwitser EW, Breederveld BS. Fractures of the fifth metatarsal; diagnosis and treatment. Injury. 2010;41:555-562.
16. Koslowsky TC, Gausepohl T, Mader K, et al. Treatment of displaced proximal fifth metatarsal fractures using a new one-step fixation technique. J Trauma. 2010;68:122-125.
17. Mologne TS. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 2005;33:970-975.
18. Porter DA, Duncan M, Meyer SJF. Fifth metatarsal Jones fracture fixation with a 4.5-mm cannulated stainless steel screw in the competitive and recreational athlete. Am J Sports Med. 2005;33:726-733.
19. Vu D, McDiarmid T, Brown M. What is the most effective management of acute fractures of the base of the fifth metatarsal? J Fam Pract. 2006;55:713-717.
20. Monteleone GP. Stress fractures in the athlete. Orthop Clin North Am. 1995;26:423-432.
21. Torg JS, Pavlov H, Cooley LH, et al. Stress fractures of the tarsal navicular. A retrospective review of twenty-one cases. J Bone Joint Surg Am. 1982;64:700-712.
22. Khan KM, Fuller PJ, Brukner PD, et al. Outcome of conservative and surgical management of navicular stress fracture in athletes. Eighty-six cases proven with computerized tomography. Am J Sports Med. 1992;20:657-666.
23. Sizensky JA, Marks RM. Imaging of the navicular. Foot Ankle Clin. 2004;9:181-209.
24. Torg JS, Moyer J, Gaughan JP, et al. Management of tarsal navicular stress fractures: conservative versus surgical treatment: a meta-analysis. Am J Sports Med. 2010;38:1048-1053.
25. Bojanic I. Conservative treatment of stress fractures of the tarsal navicular in athletes. Rev Chir Orthop Reparatrice Appar Mot. 1997;83:133-138.
26. Ostlie DK, Simons SM. Tarsal navicular stress fracture in a young athlete: case report with clinical, radiologic, and pathophysiologic correlations. J Am Board Fam Pract. 2001;14:381-385.
27. Towne LC, Blazina ME, Cozen LN. Fatigue fracture of the tarsal navicular. J Bone Joint Surg Am. 1970;52:376-378.
28. Strauss JE, Fornberg JA, Lippert FG. Chronic lateral ankle instability and associated conditions: a rationale for treatment. Foot Ankle Int. 2007;28:1041-1044.
29. Schachter AK, Chen AL, Reddy PD, et al. Osteochondral lesions of the talus. J Am Acad Orthop Surg. 2005;13:152-158.
30. Taga I, Shino K, Inoue M, et al. Articular cartilage lesion in ankles with lateral ligament injury. Am J Sport Med. 1993;21:120-127.
31. O’Loughlin PF, Heyworth BE, Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010;38:392-404.
32. Shearer C, Loomer R, Clement D. Nonoperatively managed stage 5 osteochondral talar lesions. Foot Ankle Int. 2002;23:651-654.
33. Haverstock BD. Foot and ankle imaging in the athlete. Clin Podiatr Med Surg. 2008;25:249-262.
34. Geppert M, Sobel M, Bohne W. Lateral ankle instability as a cause of superior peroneal retinacular laxity: an anatomic and biomechanical study of cadaveric feet. Foot Ankle. 1993;14:330-334.
35. Butler BW, Lanthier J, Wertheimer SJ. Subluxing peroneals: a review of the literature and case report. J Foot Ankle Surg. 1993;32:134-139.
36. Roth JA, Taylor WC, Whalen J. Peroneal tendon subluxation: the other lateral ankle injury. Br J Sports Med. 2010;44:1047-1053.
37. Maffulli N, Ferran NA, Oliva F, et al. Recurrent subluxation of the peroneal tendons. Am J Sports Med. 2006;34:986-992.
38. Mason RB, Henderson JP. Traumatic peroneal tendon instability. Am J Sports Med. 1996;24:652-658.
39. Brodsky J, Krause J. Peroneus brevis tendon tears: pathophysiology, surgical reconstruction, and clinical results. Foot Ankle Int. 1998;19:271-279.
40. Marten MA, Noyez JF, Mulier JC. Recurrent dislocation of the peroneal tendons. Results of rerouting the tendons under the calcaneofibular ligament. Am J Sports Med. 1986;14:148-150.
41. Escalas F, Figueras JM, Merino JA. Dislocation of the peroneal tendons. Long-term results of surgical treatment. J Bone Joint Surg Am. 1980;62:451-453.
1. van Rijn RM, van Os AG, Bernsen RM, et al. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008;121:324-331.
2. Nugent PJ. Ottawa ankle rules accurately assess injuries and reduce reliance on radiographs. J Fam Pract. 2004;53:785-788.
3. Stiell IG, McKnight RD, Greenberg GH, et al. Implementation of the Ottawa ankle rules. JAMA. 1994;271:827-832.
4. Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. JAMA. 1993;269:1127-1132.
5. Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002;66:785-795.
6. Den Hartog BD. Fracture of the proximal fifth metatarsal. J Am Acad Orthop Surg. 2009;17:458-464.
7. Torg JS, Balduini FC, Zelko RR, et al. Fractures of the base of the fifth metatarsal distal to the tuberosity. J Bone Joint Surg Am. 1984;66:209-214.
8. Dameron TB. Fractures and anatomical variations of the proximal portion of the fifth metatarsal. J Bone Joint Surg Am. 1975;57:788-792.
9. Boden BP, Oshbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29:100-113.
10. Pao DG. Avulsion fracture of the base of the fifth metatarsal not seen on conventional radiography of the foot: the need for an additional projection. Am J Roentgenol. 2000;175:549-552.
11. Egol K. Avulsion fractures of the fifth metatarsal base: a prospective outcome study. Foot Ankle Int. 2007;28:581-583.
12. Jones MH, Amendola AS. Navicular stress fractures. Clin Sports Med. 2006;25:151-158.
13. Fitch KD, Blackwell JB, Gilmour WN. Operation for non-union of stress fracture of the tarsal navicular. J Bone Joint Surg Br. 1989;71:105-110.
14. Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002;66:785-794.
15. Zwitser EW, Breederveld BS. Fractures of the fifth metatarsal; diagnosis and treatment. Injury. 2010;41:555-562.
16. Koslowsky TC, Gausepohl T, Mader K, et al. Treatment of displaced proximal fifth metatarsal fractures using a new one-step fixation technique. J Trauma. 2010;68:122-125.
17. Mologne TS. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 2005;33:970-975.
18. Porter DA, Duncan M, Meyer SJF. Fifth metatarsal Jones fracture fixation with a 4.5-mm cannulated stainless steel screw in the competitive and recreational athlete. Am J Sports Med. 2005;33:726-733.
19. Vu D, McDiarmid T, Brown M. What is the most effective management of acute fractures of the base of the fifth metatarsal? J Fam Pract. 2006;55:713-717.
20. Monteleone GP. Stress fractures in the athlete. Orthop Clin North Am. 1995;26:423-432.
21. Torg JS, Pavlov H, Cooley LH, et al. Stress fractures of the tarsal navicular. A retrospective review of twenty-one cases. J Bone Joint Surg Am. 1982;64:700-712.
22. Khan KM, Fuller PJ, Brukner PD, et al. Outcome of conservative and surgical management of navicular stress fracture in athletes. Eighty-six cases proven with computerized tomography. Am J Sports Med. 1992;20:657-666.
23. Sizensky JA, Marks RM. Imaging of the navicular. Foot Ankle Clin. 2004;9:181-209.
24. Torg JS, Moyer J, Gaughan JP, et al. Management of tarsal navicular stress fractures: conservative versus surgical treatment: a meta-analysis. Am J Sports Med. 2010;38:1048-1053.
25. Bojanic I. Conservative treatment of stress fractures of the tarsal navicular in athletes. Rev Chir Orthop Reparatrice Appar Mot. 1997;83:133-138.
26. Ostlie DK, Simons SM. Tarsal navicular stress fracture in a young athlete: case report with clinical, radiologic, and pathophysiologic correlations. J Am Board Fam Pract. 2001;14:381-385.
27. Towne LC, Blazina ME, Cozen LN. Fatigue fracture of the tarsal navicular. J Bone Joint Surg Am. 1970;52:376-378.
28. Strauss JE, Fornberg JA, Lippert FG. Chronic lateral ankle instability and associated conditions: a rationale for treatment. Foot Ankle Int. 2007;28:1041-1044.
29. Schachter AK, Chen AL, Reddy PD, et al. Osteochondral lesions of the talus. J Am Acad Orthop Surg. 2005;13:152-158.
30. Taga I, Shino K, Inoue M, et al. Articular cartilage lesion in ankles with lateral ligament injury. Am J Sport Med. 1993;21:120-127.
31. O’Loughlin PF, Heyworth BE, Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010;38:392-404.
32. Shearer C, Loomer R, Clement D. Nonoperatively managed stage 5 osteochondral talar lesions. Foot Ankle Int. 2002;23:651-654.
33. Haverstock BD. Foot and ankle imaging in the athlete. Clin Podiatr Med Surg. 2008;25:249-262.
34. Geppert M, Sobel M, Bohne W. Lateral ankle instability as a cause of superior peroneal retinacular laxity: an anatomic and biomechanical study of cadaveric feet. Foot Ankle. 1993;14:330-334.
35. Butler BW, Lanthier J, Wertheimer SJ. Subluxing peroneals: a review of the literature and case report. J Foot Ankle Surg. 1993;32:134-139.
36. Roth JA, Taylor WC, Whalen J. Peroneal tendon subluxation: the other lateral ankle injury. Br J Sports Med. 2010;44:1047-1053.
37. Maffulli N, Ferran NA, Oliva F, et al. Recurrent subluxation of the peroneal tendons. Am J Sports Med. 2006;34:986-992.
38. Mason RB, Henderson JP. Traumatic peroneal tendon instability. Am J Sports Med. 1996;24:652-658.
39. Brodsky J, Krause J. Peroneus brevis tendon tears: pathophysiology, surgical reconstruction, and clinical results. Foot Ankle Int. 1998;19:271-279.
40. Marten MA, Noyez JF, Mulier JC. Recurrent dislocation of the peroneal tendons. Results of rerouting the tendons under the calcaneofibular ligament. Am J Sports Med. 1986;14:148-150.
41. Escalas F, Figueras JM, Merino JA. Dislocation of the peroneal tendons. Long-term results of surgical treatment. J Bone Joint Surg Am. 1980;62:451-453.