User login
Subspecialty May Be on the Horizon
DENVER – Pediatric hospitalists adhere more closely to bronchiolitis management guidelines than do nonhospitalist pediatricians, according to a multicenter chart review.
The implication is that hospitalists therefore provide a higher quality of care. This notion is supported by the study finding that hospitalist-managed patients were less likely to be admitted to the intensive care unit. On the other hand, neither overall length of stay nor rates of rehospitalization within 4 weeks were significantly different for pediatric hospitalist- and nonhospitalist-managed patients with bronchiolitis, Dr. Russell McCulloh reported at the annual meeting of the Pediatric Academic Societies.
Prior attempts to compare the quality of care provided by pediatric hospitalists and nonhospitalists have generally relied upon self-reported rates of guideline adherence obtained in physician surveys. To generate more objective data, Dr. McCulloh and coworkers at Hasbro Children’s Hospital in Providence, R.I., analyzed the charts of 713 children with bronchiolitis who were admitted to the pediatric hospitalist and nonhospitalist pediatric services at two academic tertiary medical centers in 2007-2008.
The investigators selected bronchiolitis as the index diagnosis for their quality-of-care study because it is the No. 1 cause of hospital admission in children. The quality standard against which physician management was measured was the 2006 American Academy of Pediatrics guidelines for bronchiolitis diagnosis and management (Pediatrics 2006;118:1774-93).
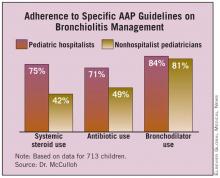
Reviewers focused on three quality indicators contained in the guidelines. First, the AAP guidelines recommend that corticosteroids shouldn’t be used routinely in the management of bronchiolitis. Pediatric hospitalists were clearly more in step with this guidance. The review showed that they discontinued systemic steroids when no indication existed 75% of the time, compared with 42% for nonhospitalists, according to Dr. McCulloh.
Second, hospitalists similarly discontinued antibiotics in the absence of specific indications of a coexistent bacterial infection 71% of the time. Nonhospitalist pediatricians were in step with this AAP recommendation only 49% of the time.
Third, regarding the discontinuation of bronchodilators in the absence of a documented, objective, positive clinical response, both types of physicians showed room for improvement. Hospitalists stopped albuterol in only 84% of cases when it had been proved ineffective; nonhospitalist pediatricians did so 81% of the time. Those rates of guideline adherence are insufficient, Dr. McCulloh commented.
On the other hand, hospitalists discontinued unneeded racemic epinephrine 93% of the time, as did nonhospitalists in 91% of cases in which it was appropriate to do so.
Rehospitalization within 4 weeks occurred in 4.6% of pediatric hospitalist–managed patients and in 7.2% of those managed by nonhospitalist pediatricians, a nonsignificant difference. In contrast, the 10.9% ICU admission rate for hospitalist-managed bronchiolitis patients was significantly lower than the 16.3% rate among children managed by nonhospitalists.
Dr. McCulloh declared having no financial conflicts.
Medical knowledge
is too vast to be mastered by an individual. The location in which medical care
is delivered, rather than the organ system involved, has become a common
paradigm for delineating subspecialization.
The PICU, NICU and ED have
all become boarded pediatric subspecialties. Pediatric inpatient medicine
continues to evolve and has yet to determine whether to adopt a traditional
board format (3-year fellowship with a research requirement), follow adult
hospitalists with a focused practice certification (after 3 years of real-world
and real-income experience), or to become a separate track within a 3-year pediatric
residency program. As an already large and the fastest-growing subspecialty,
hospitalists may break those molds and establish their own accreditation
format. Committees are examining these options, each sparking debate at the
annual Pediatric Hospital Medicine meeting.
Requiring less start up
time than an outpatient practice, for the past decade hospital positions have
been attractive to those seeking a temporary position after residency. But as these
numbers show, the vast and growing majority of hospitalists are adopting
inpatient medicine as an exciting career path. As a lifestyle choice, it is
also more amenable to part-time positions, shift work such as nocturnists, and
extended leaves of absence.
Intellectually, hospital
medicine demands different knowledge and skills than outpatient medicine. These
include the treatment of diseases in seriously ill children, coordinating care
for technology-dependent children, and providing procedural sedation.
More recently, the
emphasis of hospital medicine has focused on systemic issues, such as reducing
errors and other quality improvement programs. In the near future, providing
cost-effective care will gain importance.
Kevin Powell, M.D., Ph.D.,
is associate professor of pediatrics at St. Louis
University and a pediatric hospitalist
at SSM Cardinal Glennon Children’s Medical
Center in St. Louis. He has no relevant disclosures nor
conflicts of interest to report.
Medical knowledge
is too vast to be mastered by an individual. The location in which medical care
is delivered, rather than the organ system involved, has become a common
paradigm for delineating subspecialization.
The PICU, NICU and ED have
all become boarded pediatric subspecialties. Pediatric inpatient medicine
continues to evolve and has yet to determine whether to adopt a traditional
board format (3-year fellowship with a research requirement), follow adult
hospitalists with a focused practice certification (after 3 years of real-world
and real-income experience), or to become a separate track within a 3-year pediatric
residency program. As an already large and the fastest-growing subspecialty,
hospitalists may break those molds and establish their own accreditation
format. Committees are examining these options, each sparking debate at the
annual Pediatric Hospital Medicine meeting.
Requiring less start up
time than an outpatient practice, for the past decade hospital positions have
been attractive to those seeking a temporary position after residency. But as these
numbers show, the vast and growing majority of hospitalists are adopting
inpatient medicine as an exciting career path. As a lifestyle choice, it is
also more amenable to part-time positions, shift work such as nocturnists, and
extended leaves of absence.
Intellectually, hospital
medicine demands different knowledge and skills than outpatient medicine. These
include the treatment of diseases in seriously ill children, coordinating care
for technology-dependent children, and providing procedural sedation.
More recently, the
emphasis of hospital medicine has focused on systemic issues, such as reducing
errors and other quality improvement programs. In the near future, providing
cost-effective care will gain importance.
Kevin Powell, M.D., Ph.D.,
is associate professor of pediatrics at St. Louis
University and a pediatric hospitalist
at SSM Cardinal Glennon Children’s Medical
Center in St. Louis. He has no relevant disclosures nor
conflicts of interest to report.
Medical knowledge
is too vast to be mastered by an individual. The location in which medical care
is delivered, rather than the organ system involved, has become a common
paradigm for delineating subspecialization.
The PICU, NICU and ED have
all become boarded pediatric subspecialties. Pediatric inpatient medicine
continues to evolve and has yet to determine whether to adopt a traditional
board format (3-year fellowship with a research requirement), follow adult
hospitalists with a focused practice certification (after 3 years of real-world
and real-income experience), or to become a separate track within a 3-year pediatric
residency program. As an already large and the fastest-growing subspecialty,
hospitalists may break those molds and establish their own accreditation
format. Committees are examining these options, each sparking debate at the
annual Pediatric Hospital Medicine meeting.
Requiring less start up
time than an outpatient practice, for the past decade hospital positions have
been attractive to those seeking a temporary position after residency. But as these
numbers show, the vast and growing majority of hospitalists are adopting
inpatient medicine as an exciting career path. As a lifestyle choice, it is
also more amenable to part-time positions, shift work such as nocturnists, and
extended leaves of absence.
Intellectually, hospital
medicine demands different knowledge and skills than outpatient medicine. These
include the treatment of diseases in seriously ill children, coordinating care
for technology-dependent children, and providing procedural sedation.
More recently, the
emphasis of hospital medicine has focused on systemic issues, such as reducing
errors and other quality improvement programs. In the near future, providing
cost-effective care will gain importance.
Kevin Powell, M.D., Ph.D.,
is associate professor of pediatrics at St. Louis
University and a pediatric hospitalist
at SSM Cardinal Glennon Children’s Medical
Center in St. Louis. He has no relevant disclosures nor
conflicts of interest to report.
Subspecialty May Be on the Horizon
Subspecialty May Be on the Horizon
DENVER – Pediatric hospitalists adhere more closely to bronchiolitis management guidelines than do nonhospitalist pediatricians, according to a multicenter chart review.
The implication is that hospitalists therefore provide a higher quality of care. This notion is supported by the study finding that hospitalist-managed patients were less likely to be admitted to the intensive care unit. On the other hand, neither overall length of stay nor rates of rehospitalization within 4 weeks were significantly different for pediatric hospitalist- and nonhospitalist-managed patients with bronchiolitis, Dr. Russell McCulloh reported at the annual meeting of the Pediatric Academic Societies.
Prior attempts to compare the quality of care provided by pediatric hospitalists and nonhospitalists have generally relied upon self-reported rates of guideline adherence obtained in physician surveys. To generate more objective data, Dr. McCulloh and coworkers at Hasbro Children’s Hospital in Providence, R.I., analyzed the charts of 713 children with bronchiolitis who were admitted to the pediatric hospitalist and nonhospitalist pediatric services at two academic tertiary medical centers in 2007-2008.
The investigators selected bronchiolitis as the index diagnosis for their quality-of-care study because it is the No. 1 cause of hospital admission in children. The quality standard against which physician management was measured was the 2006 American Academy of Pediatrics guidelines for bronchiolitis diagnosis and management (Pediatrics 2006;118:1774-93).
Reviewers focused on three quality indicators contained in the guidelines. First, the AAP guidelines recommend that corticosteroids shouldn’t be used routinely in the management of bronchiolitis. Pediatric hospitalists were clearly more in step with this guidance. The review showed that they discontinued systemic steroids when no indication existed 75% of the time, compared with 42% for nonhospitalists, according to Dr. McCulloh.
Second, hospitalists similarly discontinued antibiotics in the absence of specific indications of a coexistent bacterial infection 71% of the time. Nonhospitalist pediatricians were in step with this AAP recommendation only 49% of the time.
Third, regarding the discontinuation of bronchodilators in the absence of a documented, objective, positive clinical response, both types of physicians showed room for improvement. Hospitalists stopped albuterol in only 84% of cases when it had been proved ineffective; nonhospitalist pediatricians did so 81% of the time. Those rates of guideline adherence are insufficient, Dr. McCulloh commented.
On the other hand, hospitalists discontinued unneeded racemic epinephrine 93% of the time, as did nonhospitalists in 91% of cases in which it was appropriate to do so.
Rehospitalization within 4 weeks occurred in 4.6% of pediatric hospitalist–managed patients and in 7.2% of those managed by nonhospitalist pediatricians, a nonsignificant difference. In contrast, the 10.9% ICU admission rate for hospitalist-managed bronchiolitis patients was significantly lower than the 16.3% rate among children managed by nonhospitalists.
Dr. McCulloh declared having no financial conflicts.
DENVER – Pediatric hospitalists adhere more closely to bronchiolitis management guidelines than do nonhospitalist pediatricians, according to a multicenter chart review.
The implication is that hospitalists therefore provide a higher quality of care. This notion is supported by the study finding that hospitalist-managed patients were less likely to be admitted to the intensive care unit. On the other hand, neither overall length of stay nor rates of rehospitalization within 4 weeks were significantly different for pediatric hospitalist- and nonhospitalist-managed patients with bronchiolitis, Dr. Russell McCulloh reported at the annual meeting of the Pediatric Academic Societies.
Prior attempts to compare the quality of care provided by pediatric hospitalists and nonhospitalists have generally relied upon self-reported rates of guideline adherence obtained in physician surveys. To generate more objective data, Dr. McCulloh and coworkers at Hasbro Children’s Hospital in Providence, R.I., analyzed the charts of 713 children with bronchiolitis who were admitted to the pediatric hospitalist and nonhospitalist pediatric services at two academic tertiary medical centers in 2007-2008.
The investigators selected bronchiolitis as the index diagnosis for their quality-of-care study because it is the No. 1 cause of hospital admission in children. The quality standard against which physician management was measured was the 2006 American Academy of Pediatrics guidelines for bronchiolitis diagnosis and management (Pediatrics 2006;118:1774-93).
Reviewers focused on three quality indicators contained in the guidelines. First, the AAP guidelines recommend that corticosteroids shouldn’t be used routinely in the management of bronchiolitis. Pediatric hospitalists were clearly more in step with this guidance. The review showed that they discontinued systemic steroids when no indication existed 75% of the time, compared with 42% for nonhospitalists, according to Dr. McCulloh.
Second, hospitalists similarly discontinued antibiotics in the absence of specific indications of a coexistent bacterial infection 71% of the time. Nonhospitalist pediatricians were in step with this AAP recommendation only 49% of the time.
Third, regarding the discontinuation of bronchodilators in the absence of a documented, objective, positive clinical response, both types of physicians showed room for improvement. Hospitalists stopped albuterol in only 84% of cases when it had been proved ineffective; nonhospitalist pediatricians did so 81% of the time. Those rates of guideline adherence are insufficient, Dr. McCulloh commented.
On the other hand, hospitalists discontinued unneeded racemic epinephrine 93% of the time, as did nonhospitalists in 91% of cases in which it was appropriate to do so.
Rehospitalization within 4 weeks occurred in 4.6% of pediatric hospitalist–managed patients and in 7.2% of those managed by nonhospitalist pediatricians, a nonsignificant difference. In contrast, the 10.9% ICU admission rate for hospitalist-managed bronchiolitis patients was significantly lower than the 16.3% rate among children managed by nonhospitalists.
Dr. McCulloh declared having no financial conflicts.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES