User login
Last month The Hospitalist reported new 2012 State of Hospital Medicine survey data showing that 57% of those adult medicine hospitalist groups providing surgical comanagement services typically do so as admitting/attending physician, as opposed to serving in a consultant role. For groups providing medical subspecialty comanagement, the admitting/attending rate was a whopping 85%.
But just how common is comanagement these days, and what else do we know about hospitalists’ evolving scope of practice? It’s hard to compare this year’s survey results with those presented in last year’s report because previously this information was reported for all HM groups combined while this year adult and pediatric groups are reported separately. In addition, the survey population was different this year since MGMA survey participants were no longer included. But if you ask almost anyone working in HM today, they probably will tell you that the pressure to assume increased comanagement responsibilities for more and more types of patients is intense.
One of the new questions this year asked respondents to characterize their scope of services by selecting one of the following three options:
- We maintain a scope of practice that resembles traditional hospital-based internal medicine (or pediatrics, if applicable).
- Our practice scope has evolved to include some services that are outside of traditional internal medicine practice (or pediatrics, if applicable), e.g., admitting/managing patients with intracranial hemorrhage, small bowel obstruction or hip fracture.
- Our practice scope has evolved to encompass admitting a full range of hospital patients in the age group for which we are responsible, with the exception of OB and emergency surgery patients (i.e. nearly “universal admitter”).
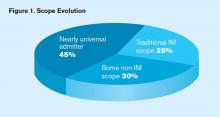
A remarkable 45% of adult medicine hospitalist groups reported that their scope has evolved toward a nearly universal admitter role, while only a quarter of such groups reported maintaining a traditional internal medicine scope (see Figure 1, below). The broader scope of practice was more common in the Midwest, among private hospitalist-only groups and those employed by management companies, and in non-teaching hospitals. Not surprisingly, academic hospital medicine groups and those employed by university/medical schools tended to maintain narrower internal medicine-focused scopes.
As to the prevalence of comanagement, this year 94% of groups serving adults only reported providing surgical comanagement services (either admitting or consulting), while 70% reported providing comanagement for medical subspecialty patients. Seven years ago, SHM’s 2005 survey found that 87% of adult medicine groups provided surgical comanagement (SHM didn’t ask about medical comanagement).
So yes, the proportion of groups providing surgical comanagement has increased, but not dramatically.
Although we don’t know for sure since the question wasn’t asked in 2005, I suspect we’d find that most groups providing surgical (and probably medical subspecialty) comanagement in 2005 served as consultants; today the preponderance serve as admitting/attending physician for such patients. That’s a significant scope evolution that’s not obvious from just looking at the percent of groups that provide comanagement.
A comprehensive list of services routinely provided by HM groups is available in the new 2012 State of Hospital Medicine report, with breakdowns by group type, geographic region, employment model, and academic/teaching status. Hopefully, SHM will continue to survey this important topic so that scope evolution can be tracked going forward.
Last month The Hospitalist reported new 2012 State of Hospital Medicine survey data showing that 57% of those adult medicine hospitalist groups providing surgical comanagement services typically do so as admitting/attending physician, as opposed to serving in a consultant role. For groups providing medical subspecialty comanagement, the admitting/attending rate was a whopping 85%.
But just how common is comanagement these days, and what else do we know about hospitalists’ evolving scope of practice? It’s hard to compare this year’s survey results with those presented in last year’s report because previously this information was reported for all HM groups combined while this year adult and pediatric groups are reported separately. In addition, the survey population was different this year since MGMA survey participants were no longer included. But if you ask almost anyone working in HM today, they probably will tell you that the pressure to assume increased comanagement responsibilities for more and more types of patients is intense.
One of the new questions this year asked respondents to characterize their scope of services by selecting one of the following three options:
- We maintain a scope of practice that resembles traditional hospital-based internal medicine (or pediatrics, if applicable).
- Our practice scope has evolved to include some services that are outside of traditional internal medicine practice (or pediatrics, if applicable), e.g., admitting/managing patients with intracranial hemorrhage, small bowel obstruction or hip fracture.
- Our practice scope has evolved to encompass admitting a full range of hospital patients in the age group for which we are responsible, with the exception of OB and emergency surgery patients (i.e. nearly “universal admitter”).
A remarkable 45% of adult medicine hospitalist groups reported that their scope has evolved toward a nearly universal admitter role, while only a quarter of such groups reported maintaining a traditional internal medicine scope (see Figure 1, below). The broader scope of practice was more common in the Midwest, among private hospitalist-only groups and those employed by management companies, and in non-teaching hospitals. Not surprisingly, academic hospital medicine groups and those employed by university/medical schools tended to maintain narrower internal medicine-focused scopes.
As to the prevalence of comanagement, this year 94% of groups serving adults only reported providing surgical comanagement services (either admitting or consulting), while 70% reported providing comanagement for medical subspecialty patients. Seven years ago, SHM’s 2005 survey found that 87% of adult medicine groups provided surgical comanagement (SHM didn’t ask about medical comanagement).
So yes, the proportion of groups providing surgical comanagement has increased, but not dramatically.
Although we don’t know for sure since the question wasn’t asked in 2005, I suspect we’d find that most groups providing surgical (and probably medical subspecialty) comanagement in 2005 served as consultants; today the preponderance serve as admitting/attending physician for such patients. That’s a significant scope evolution that’s not obvious from just looking at the percent of groups that provide comanagement.
A comprehensive list of services routinely provided by HM groups is available in the new 2012 State of Hospital Medicine report, with breakdowns by group type, geographic region, employment model, and academic/teaching status. Hopefully, SHM will continue to survey this important topic so that scope evolution can be tracked going forward.
Last month The Hospitalist reported new 2012 State of Hospital Medicine survey data showing that 57% of those adult medicine hospitalist groups providing surgical comanagement services typically do so as admitting/attending physician, as opposed to serving in a consultant role. For groups providing medical subspecialty comanagement, the admitting/attending rate was a whopping 85%.
But just how common is comanagement these days, and what else do we know about hospitalists’ evolving scope of practice? It’s hard to compare this year’s survey results with those presented in last year’s report because previously this information was reported for all HM groups combined while this year adult and pediatric groups are reported separately. In addition, the survey population was different this year since MGMA survey participants were no longer included. But if you ask almost anyone working in HM today, they probably will tell you that the pressure to assume increased comanagement responsibilities for more and more types of patients is intense.
One of the new questions this year asked respondents to characterize their scope of services by selecting one of the following three options:
- We maintain a scope of practice that resembles traditional hospital-based internal medicine (or pediatrics, if applicable).
- Our practice scope has evolved to include some services that are outside of traditional internal medicine practice (or pediatrics, if applicable), e.g., admitting/managing patients with intracranial hemorrhage, small bowel obstruction or hip fracture.
- Our practice scope has evolved to encompass admitting a full range of hospital patients in the age group for which we are responsible, with the exception of OB and emergency surgery patients (i.e. nearly “universal admitter”).
A remarkable 45% of adult medicine hospitalist groups reported that their scope has evolved toward a nearly universal admitter role, while only a quarter of such groups reported maintaining a traditional internal medicine scope (see Figure 1, below). The broader scope of practice was more common in the Midwest, among private hospitalist-only groups and those employed by management companies, and in non-teaching hospitals. Not surprisingly, academic hospital medicine groups and those employed by university/medical schools tended to maintain narrower internal medicine-focused scopes.
As to the prevalence of comanagement, this year 94% of groups serving adults only reported providing surgical comanagement services (either admitting or consulting), while 70% reported providing comanagement for medical subspecialty patients. Seven years ago, SHM’s 2005 survey found that 87% of adult medicine groups provided surgical comanagement (SHM didn’t ask about medical comanagement).
So yes, the proportion of groups providing surgical comanagement has increased, but not dramatically.
Although we don’t know for sure since the question wasn’t asked in 2005, I suspect we’d find that most groups providing surgical (and probably medical subspecialty) comanagement in 2005 served as consultants; today the preponderance serve as admitting/attending physician for such patients. That’s a significant scope evolution that’s not obvious from just looking at the percent of groups that provide comanagement.
A comprehensive list of services routinely provided by HM groups is available in the new 2012 State of Hospital Medicine report, with breakdowns by group type, geographic region, employment model, and academic/teaching status. Hopefully, SHM will continue to survey this important topic so that scope evolution can be tracked going forward.