User login
IN THIS ARTICLE
- Clinical presentation
- Disease triggers
- Outcome for the case patient
A 4-month-old white boy is brought to the allergy office for evaluation of a lesion on his back, first noticed when he was one month old. His parents report that on two separate occasions he developed a bright red, whole-body rash that resolved on its own. He is described as a “fussy” baby who has been on both milk- and soy-based formulas. Aside from mild eczema and infantile seborrheic dermatitis, his medical history is unremarkable.
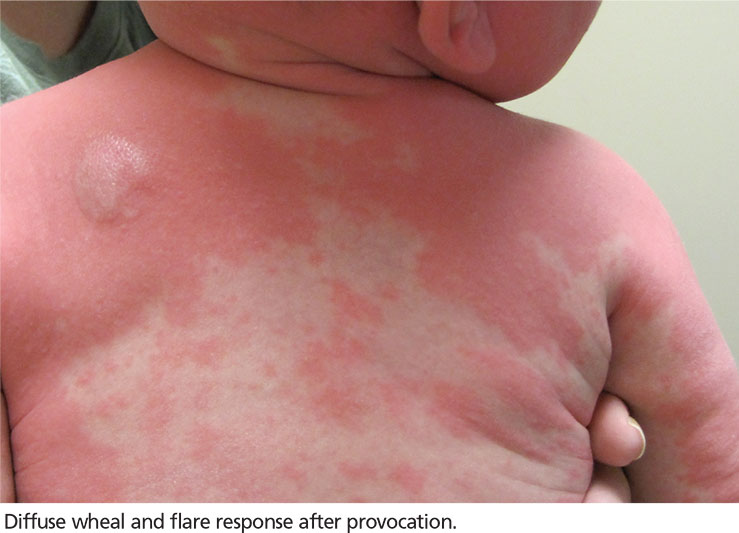
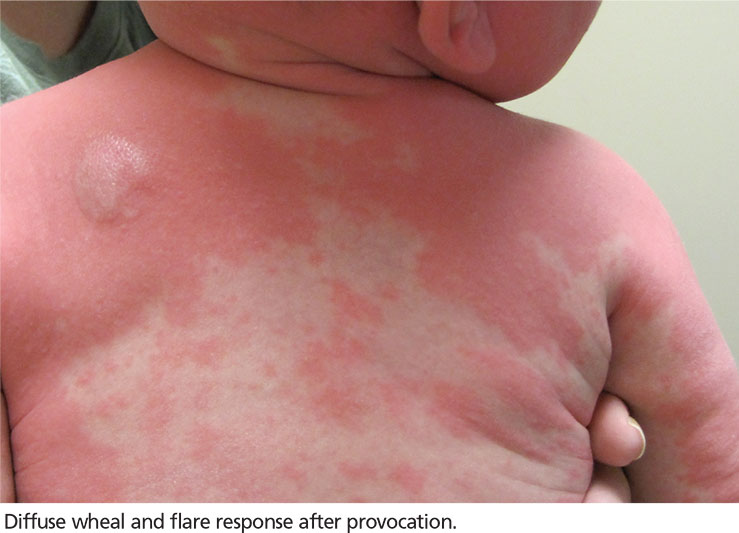
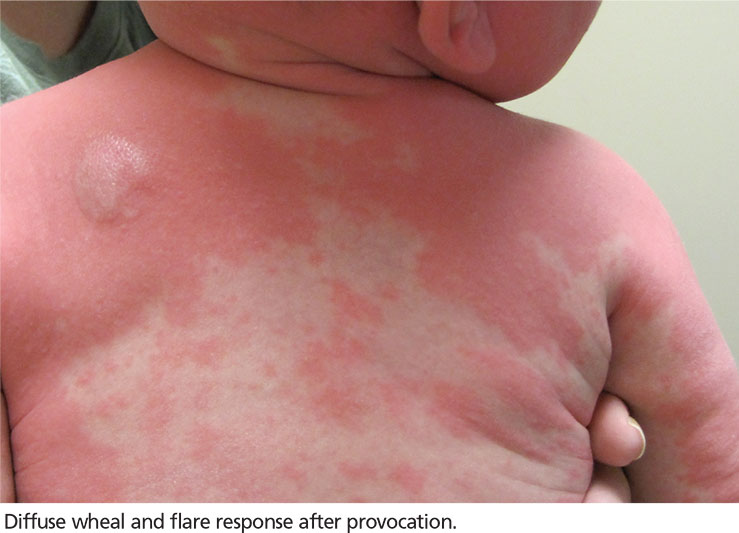
Physical examination reveals a reddish, 3-cm plaque on his left upper back that, when stroked, exhibits an immediate urticarial response. The patient is given cetirizine in the office and within 45 minutes, the flushing resolves. A normal tryptase level is obtained. The patient is diagnosed with a solitary mastocytoma.
DISCUSSION
Mast cells play a central role in allergic rhinitis, asthma, eczema, and anaphylaxis; they are also a vital component in the inflammatory process. Cutaneous mastocytosis is a pathologic increase in mast cells that, when degranulated, release histamine and tryptase.1 Histamine is produced equally by both mast cells and basophils, while the production of tryptase is relatively specific to mast cells. An elevated tryptase level is indicative of mast cell activation. The signs and symptoms associated with cutaneous mastocytosis are due to the release of these mediators.2
While there is no gender bias for cutaneous mastocytosis, there is a bimodal distribution: Children from birth to age 2 account for 55% of cases, whereas 35% of cases occur in those older than 15—the remaining 10% are between these ages.1 During the first year of life, 60% to 80% of patients with cutaneous mastocytosis will develop lesions. Familial cases are rare.2
Clinical presentation
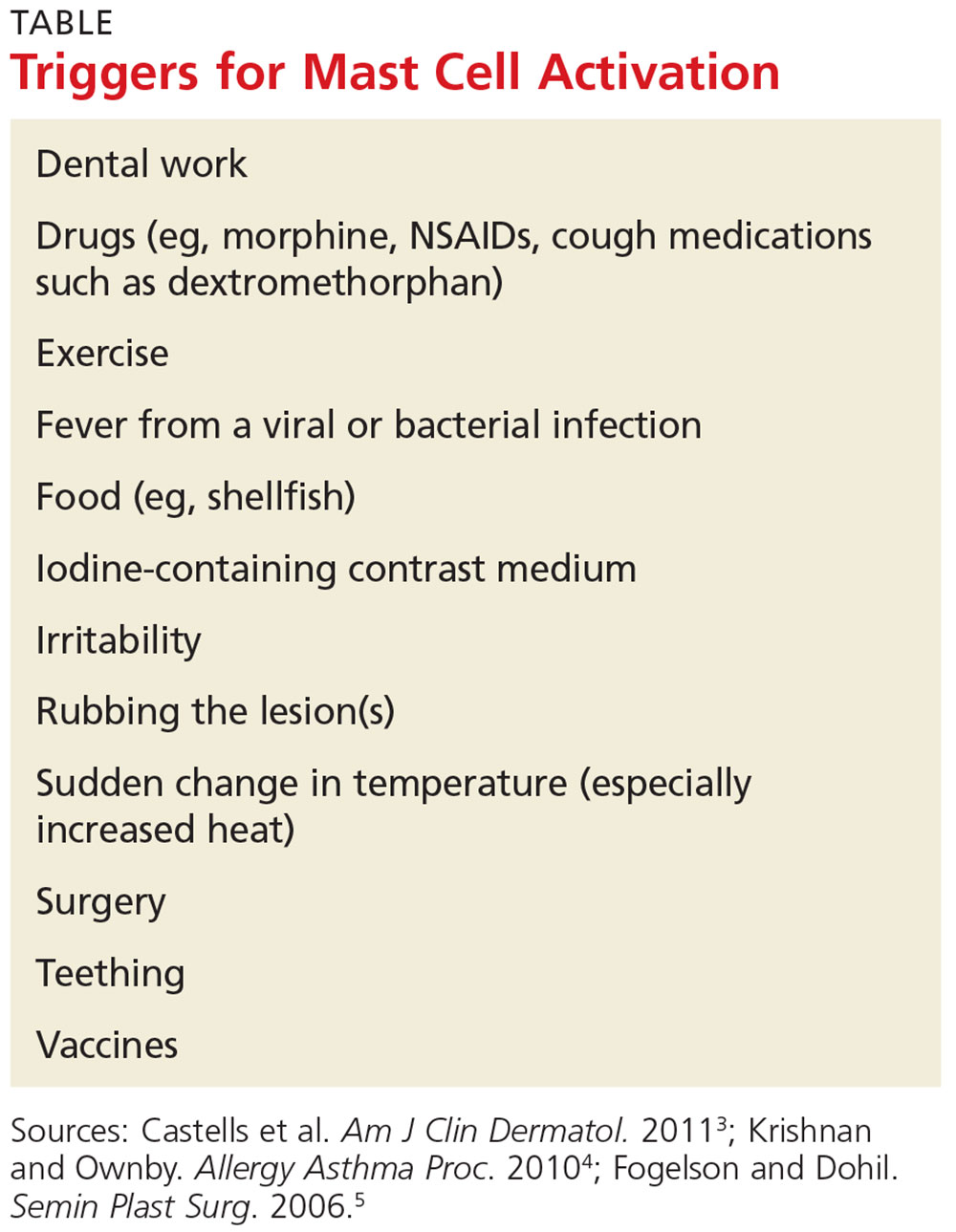
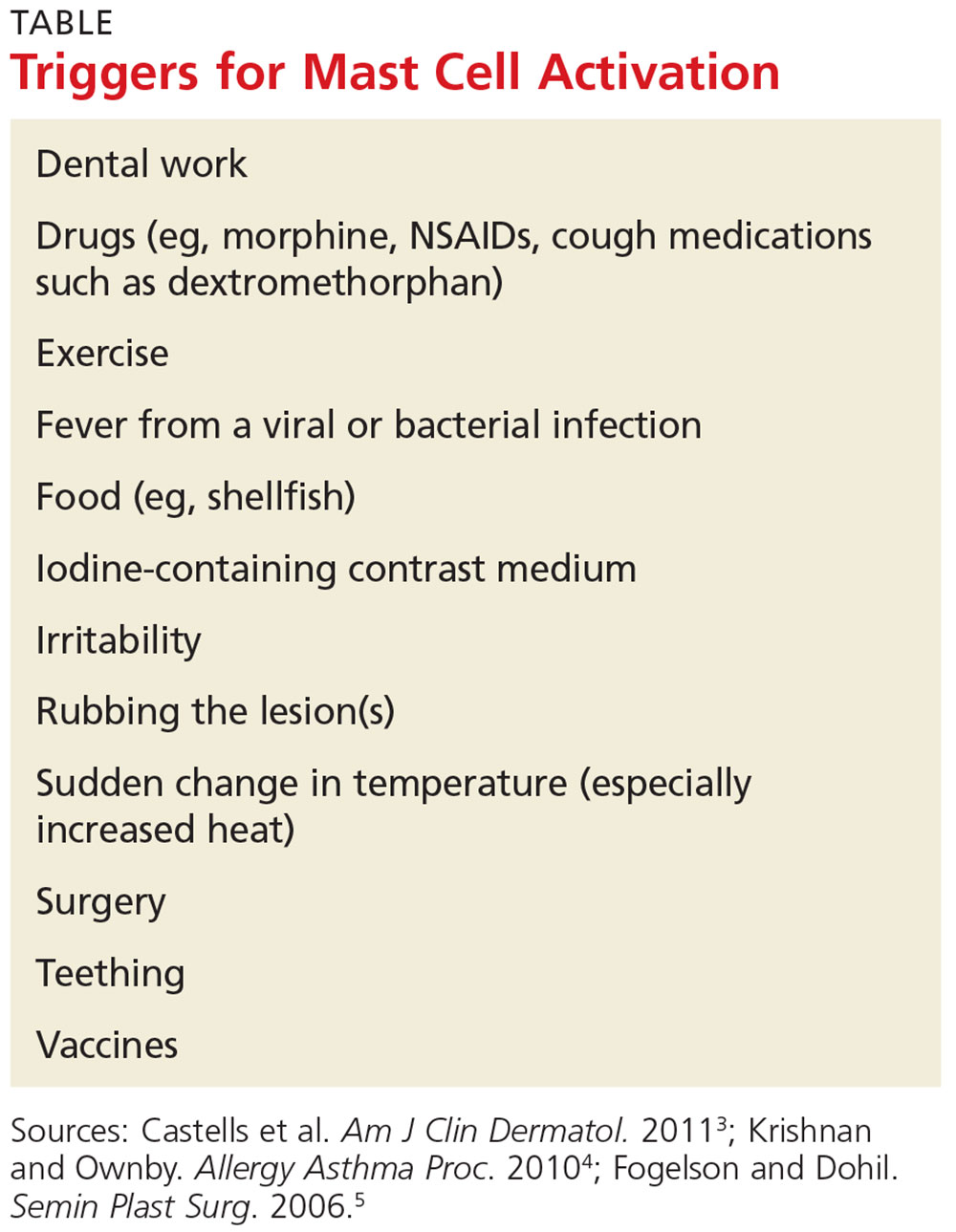
The presentation of cutaneous mastocytosis can vary. It is often mistaken for common childhood rashes such as poison ivy, eczema, or hives. The effects of histamine and tryptase cause children to present with pruritus, flushing, and headache. Gastrointestinal symptoms, such as abdominal pain and diarrhea, can also occur as a result of histamine release. Symptoms can occur spontaneously or be induced by certain triggers (see Table).3
There are three types of cutaneous mastocytosis: urticarial pigmentosa (UP), solitary mastocytoma, and diffuse cutaneous mastocytosis (DCM). UP is the most common, representing 70% to 90% of all cases.3 It typically manifests as multiple red, brown, or yellow lesions that are small (usually < 2 cm). A positive Darier sign (the formation of a wheal and flare after stroking one or several lesions) is common in these patients.2,3
Solitary mastocytomas are single, indurated, red-brown macules, papules, or plaques.4 Frequently seen on the trunk, extremities, head, or neck, these lesions resemble UP but are larger (up to several centimeters in diameter).2,4 A positive Darier sign is elicited in approximately 50% of these patients.4 Solitary mastocytomas are seen in 10% to 15% of children with cutaneous mastocytosis.4
DCM accounts for only 1% to 3% of cases and typically involves the entire skin, which is usually thick, with a normal or yellowish brown color.3 Affected patients may experience blistering and bullae. Severe symptoms, including whole-body flushing, pruritus, diarrhea, intestinal bleeding, hypotension, anemia, and hypovolemic shock, can occur; deaths have been reported.2
Diagnostic evaluation
Following a thorough history and physical exam, the diagnosis of cutaneous mastocytosis can be made based on clinical findings.5 It can be confirmed by a punch biopsy of the lesion and measurement of serum tryptase levels; higher levels have been shown to correlate to the number of mast cells in the skin and the child’s cutaneous disease burden.2,4 Ordering baseline tryptase levels can also help distinguish children at risk for severe episodes of mast cell activation from those who may just have a mild case.6
If the patient exhibits symptoms suggestive of systemic mastocytosis (an abnormal increase in mast cells in extracutaneous organs, including bone marrow) or there is suspicion for malignancy, efforts must be made to rule out these more serious diagnoses. A complete white blood cell count with differential, metabolic profile with liver enzymes, and sedimentation rate should be obtained.4
Treatment
The treatment of cutaneous mastocytosis is symptomatic, as it is typically a benign disease. The goal of therapy is to prevent mast cell activation, and hence the symptoms that occur when mast cells release their mediators, by avoiding obvious triggers.4
NSAIDs have been reported to cause mast cell mediator release and should therefore be avoided. Since extremes in temperature—particularly heat—can lead to mast cell activation, it is important to control the temperature of a bath or swimming pool and to be wary of exposure to air conditioning. Though easier said than done, soothing crying babies and children is also helpful, as irritability is a known trigger. Management of anxiety and avoidance of stress when possible is recommended.2
Treatment usually begins with H1 and H2 blockers. Cetirizine and diphenhydramine work to control the itching, while ranitidine and famotidine help manage gastric acid secretion when there are symptoms of abdominal pain and peptic ulcer disease.3 Hydroxyzine is effective in controlling both itch and gastric acid secretion.4 Water-soluble cromolyn sodium cream helps to decrease the itch and flare of a mastocytoma; the oral form is also effective.3 Another option to relieve itching is to apply topical corticosteroids with an occlusive dressing.
An epinephrine auto-injector is recommended due to the risk for anaphylaxis; this risk, however, has not been clearly established in cutaneous mastocytosis, specifically in DCM. During an acute and severe flare that induces hypotension, wheezing, and/or laryngeal edema, epinephrine should be administered while the child is lying down.3,4
Surgical excision can be considered when other treatment options fail, or if the lesion is located on the scalp, flexure area, palm, or sole.3,4
Prognosis
The prognosis for a child with a solitary mastocytoma is extremely good. By the time the child reaches puberty, there is typically spontaneous regression.
If any type of mastocytoma persists beyond adolescence, or tryptase levels continue to rise after puberty, however, that raises concern for progression to systemic mastocytosis. Although this diagnosis is rare in children, bone marrow studies may be necessary to determine the patient’s course.1
OUTCOME FOR THE CASE PATIENT
The patient was placed on daily cetirizine. His parents were advised not to irritate the lesion and were educated on possible triggers, including the need to avoid NSAIDs. They were also trained in the use of an epinephrine auto-injector.
CONCLUSION
Cutaneous mastocytosis should be included in the differential diagnosis of rashes and skin lesions in pediatric patients. It is important to be able to recognize the presenting signs and symptoms of a mastocytoma and to monitor the lesion over time.4 Educating the child’s parents, teachers, and caregivers about potential triggers and treatment of a mast cell activation attack can help minimize the symptoms.
1. Frieri M, Quershi M. Pediatric mastocytosis: a review of the literature. Pediatr Allergy Immunol Pulmonol. 2013;26(4):175-180.
2. Castells M, Metcalfe DD, Escribano L. Guidelines for the diagnosis and treatment of cutaneous mastocytosis in children. Am J Clin Dermatol. 2011;12(4):259-270.
3. Castells M, Metcalfe DD, Escribano L. Diagnosis and treatment of cutaneous mastocytosis in children: practical recommendations. Am J Clin Dermatol. 2011;12(4):259-270.
4. Krishnan K, Ownby DR. A solitary mastocytoma presenting with urticaria and angioedema in a 14-year-old boy. Allergy Asthma Proc. 2010;31(6):520-523.
5. Fogelson SK, Dohil MA. Papular and nodular skin lesions in children. Semin Plast Surg. 2006;20(3):180-191.
6. Alvarez-Twose I, Vañó-Galván S, Sánchez-Muñoz L, et al. Increased serum baseline tryptase levels and extensive skin involvement are predictors for the severity of mast cell activation episodes in children with mastocytosis. Allergy. 2012;67(6):813-821.
IN THIS ARTICLE
- Clinical presentation
- Disease triggers
- Outcome for the case patient
A 4-month-old white boy is brought to the allergy office for evaluation of a lesion on his back, first noticed when he was one month old. His parents report that on two separate occasions he developed a bright red, whole-body rash that resolved on its own. He is described as a “fussy” baby who has been on both milk- and soy-based formulas. Aside from mild eczema and infantile seborrheic dermatitis, his medical history is unremarkable.
Physical examination reveals a reddish, 3-cm plaque on his left upper back that, when stroked, exhibits an immediate urticarial response. The patient is given cetirizine in the office and within 45 minutes, the flushing resolves. A normal tryptase level is obtained. The patient is diagnosed with a solitary mastocytoma.
DISCUSSION
Mast cells play a central role in allergic rhinitis, asthma, eczema, and anaphylaxis; they are also a vital component in the inflammatory process. Cutaneous mastocytosis is a pathologic increase in mast cells that, when degranulated, release histamine and tryptase.1 Histamine is produced equally by both mast cells and basophils, while the production of tryptase is relatively specific to mast cells. An elevated tryptase level is indicative of mast cell activation. The signs and symptoms associated with cutaneous mastocytosis are due to the release of these mediators.2
While there is no gender bias for cutaneous mastocytosis, there is a bimodal distribution: Children from birth to age 2 account for 55% of cases, whereas 35% of cases occur in those older than 15—the remaining 10% are between these ages.1 During the first year of life, 60% to 80% of patients with cutaneous mastocytosis will develop lesions. Familial cases are rare.2
Clinical presentation
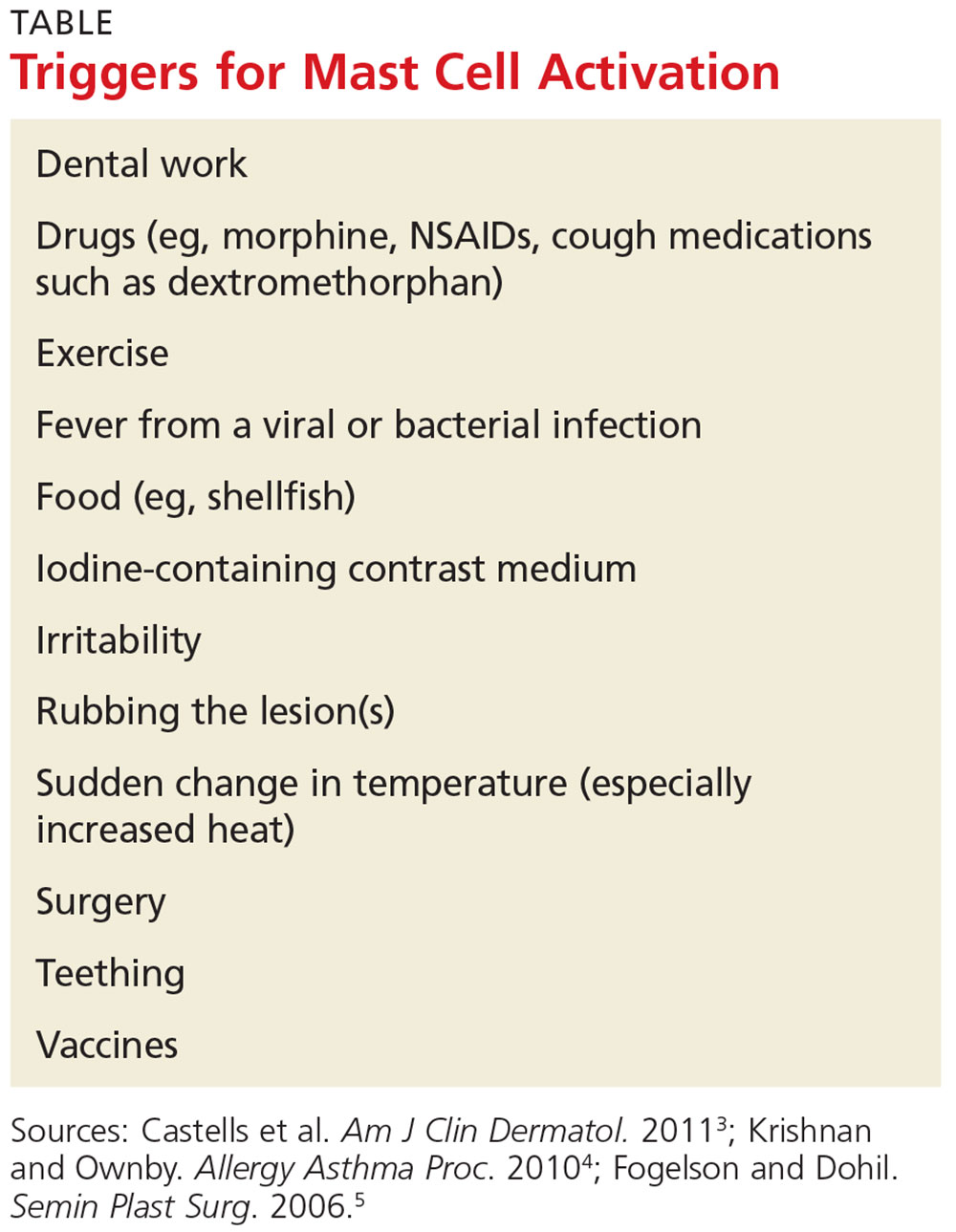
The presentation of cutaneous mastocytosis can vary. It is often mistaken for common childhood rashes such as poison ivy, eczema, or hives. The effects of histamine and tryptase cause children to present with pruritus, flushing, and headache. Gastrointestinal symptoms, such as abdominal pain and diarrhea, can also occur as a result of histamine release. Symptoms can occur spontaneously or be induced by certain triggers (see Table).3
There are three types of cutaneous mastocytosis: urticarial pigmentosa (UP), solitary mastocytoma, and diffuse cutaneous mastocytosis (DCM). UP is the most common, representing 70% to 90% of all cases.3 It typically manifests as multiple red, brown, or yellow lesions that are small (usually < 2 cm). A positive Darier sign (the formation of a wheal and flare after stroking one or several lesions) is common in these patients.2,3
Solitary mastocytomas are single, indurated, red-brown macules, papules, or plaques.4 Frequently seen on the trunk, extremities, head, or neck, these lesions resemble UP but are larger (up to several centimeters in diameter).2,4 A positive Darier sign is elicited in approximately 50% of these patients.4 Solitary mastocytomas are seen in 10% to 15% of children with cutaneous mastocytosis.4
DCM accounts for only 1% to 3% of cases and typically involves the entire skin, which is usually thick, with a normal or yellowish brown color.3 Affected patients may experience blistering and bullae. Severe symptoms, including whole-body flushing, pruritus, diarrhea, intestinal bleeding, hypotension, anemia, and hypovolemic shock, can occur; deaths have been reported.2
Diagnostic evaluation
Following a thorough history and physical exam, the diagnosis of cutaneous mastocytosis can be made based on clinical findings.5 It can be confirmed by a punch biopsy of the lesion and measurement of serum tryptase levels; higher levels have been shown to correlate to the number of mast cells in the skin and the child’s cutaneous disease burden.2,4 Ordering baseline tryptase levels can also help distinguish children at risk for severe episodes of mast cell activation from those who may just have a mild case.6
If the patient exhibits symptoms suggestive of systemic mastocytosis (an abnormal increase in mast cells in extracutaneous organs, including bone marrow) or there is suspicion for malignancy, efforts must be made to rule out these more serious diagnoses. A complete white blood cell count with differential, metabolic profile with liver enzymes, and sedimentation rate should be obtained.4
Treatment
The treatment of cutaneous mastocytosis is symptomatic, as it is typically a benign disease. The goal of therapy is to prevent mast cell activation, and hence the symptoms that occur when mast cells release their mediators, by avoiding obvious triggers.4
NSAIDs have been reported to cause mast cell mediator release and should therefore be avoided. Since extremes in temperature—particularly heat—can lead to mast cell activation, it is important to control the temperature of a bath or swimming pool and to be wary of exposure to air conditioning. Though easier said than done, soothing crying babies and children is also helpful, as irritability is a known trigger. Management of anxiety and avoidance of stress when possible is recommended.2
Treatment usually begins with H1 and H2 blockers. Cetirizine and diphenhydramine work to control the itching, while ranitidine and famotidine help manage gastric acid secretion when there are symptoms of abdominal pain and peptic ulcer disease.3 Hydroxyzine is effective in controlling both itch and gastric acid secretion.4 Water-soluble cromolyn sodium cream helps to decrease the itch and flare of a mastocytoma; the oral form is also effective.3 Another option to relieve itching is to apply topical corticosteroids with an occlusive dressing.
An epinephrine auto-injector is recommended due to the risk for anaphylaxis; this risk, however, has not been clearly established in cutaneous mastocytosis, specifically in DCM. During an acute and severe flare that induces hypotension, wheezing, and/or laryngeal edema, epinephrine should be administered while the child is lying down.3,4
Surgical excision can be considered when other treatment options fail, or if the lesion is located on the scalp, flexure area, palm, or sole.3,4
Prognosis
The prognosis for a child with a solitary mastocytoma is extremely good. By the time the child reaches puberty, there is typically spontaneous regression.
If any type of mastocytoma persists beyond adolescence, or tryptase levels continue to rise after puberty, however, that raises concern for progression to systemic mastocytosis. Although this diagnosis is rare in children, bone marrow studies may be necessary to determine the patient’s course.1
OUTCOME FOR THE CASE PATIENT
The patient was placed on daily cetirizine. His parents were advised not to irritate the lesion and were educated on possible triggers, including the need to avoid NSAIDs. They were also trained in the use of an epinephrine auto-injector.
CONCLUSION
Cutaneous mastocytosis should be included in the differential diagnosis of rashes and skin lesions in pediatric patients. It is important to be able to recognize the presenting signs and symptoms of a mastocytoma and to monitor the lesion over time.4 Educating the child’s parents, teachers, and caregivers about potential triggers and treatment of a mast cell activation attack can help minimize the symptoms.
IN THIS ARTICLE
- Clinical presentation
- Disease triggers
- Outcome for the case patient
A 4-month-old white boy is brought to the allergy office for evaluation of a lesion on his back, first noticed when he was one month old. His parents report that on two separate occasions he developed a bright red, whole-body rash that resolved on its own. He is described as a “fussy” baby who has been on both milk- and soy-based formulas. Aside from mild eczema and infantile seborrheic dermatitis, his medical history is unremarkable.
Physical examination reveals a reddish, 3-cm plaque on his left upper back that, when stroked, exhibits an immediate urticarial response. The patient is given cetirizine in the office and within 45 minutes, the flushing resolves. A normal tryptase level is obtained. The patient is diagnosed with a solitary mastocytoma.
DISCUSSION
Mast cells play a central role in allergic rhinitis, asthma, eczema, and anaphylaxis; they are also a vital component in the inflammatory process. Cutaneous mastocytosis is a pathologic increase in mast cells that, when degranulated, release histamine and tryptase.1 Histamine is produced equally by both mast cells and basophils, while the production of tryptase is relatively specific to mast cells. An elevated tryptase level is indicative of mast cell activation. The signs and symptoms associated with cutaneous mastocytosis are due to the release of these mediators.2
While there is no gender bias for cutaneous mastocytosis, there is a bimodal distribution: Children from birth to age 2 account for 55% of cases, whereas 35% of cases occur in those older than 15—the remaining 10% are between these ages.1 During the first year of life, 60% to 80% of patients with cutaneous mastocytosis will develop lesions. Familial cases are rare.2
Clinical presentation
The presentation of cutaneous mastocytosis can vary. It is often mistaken for common childhood rashes such as poison ivy, eczema, or hives. The effects of histamine and tryptase cause children to present with pruritus, flushing, and headache. Gastrointestinal symptoms, such as abdominal pain and diarrhea, can also occur as a result of histamine release. Symptoms can occur spontaneously or be induced by certain triggers (see Table).3
There are three types of cutaneous mastocytosis: urticarial pigmentosa (UP), solitary mastocytoma, and diffuse cutaneous mastocytosis (DCM). UP is the most common, representing 70% to 90% of all cases.3 It typically manifests as multiple red, brown, or yellow lesions that are small (usually < 2 cm). A positive Darier sign (the formation of a wheal and flare after stroking one or several lesions) is common in these patients.2,3
Solitary mastocytomas are single, indurated, red-brown macules, papules, or plaques.4 Frequently seen on the trunk, extremities, head, or neck, these lesions resemble UP but are larger (up to several centimeters in diameter).2,4 A positive Darier sign is elicited in approximately 50% of these patients.4 Solitary mastocytomas are seen in 10% to 15% of children with cutaneous mastocytosis.4
DCM accounts for only 1% to 3% of cases and typically involves the entire skin, which is usually thick, with a normal or yellowish brown color.3 Affected patients may experience blistering and bullae. Severe symptoms, including whole-body flushing, pruritus, diarrhea, intestinal bleeding, hypotension, anemia, and hypovolemic shock, can occur; deaths have been reported.2
Diagnostic evaluation
Following a thorough history and physical exam, the diagnosis of cutaneous mastocytosis can be made based on clinical findings.5 It can be confirmed by a punch biopsy of the lesion and measurement of serum tryptase levels; higher levels have been shown to correlate to the number of mast cells in the skin and the child’s cutaneous disease burden.2,4 Ordering baseline tryptase levels can also help distinguish children at risk for severe episodes of mast cell activation from those who may just have a mild case.6
If the patient exhibits symptoms suggestive of systemic mastocytosis (an abnormal increase in mast cells in extracutaneous organs, including bone marrow) or there is suspicion for malignancy, efforts must be made to rule out these more serious diagnoses. A complete white blood cell count with differential, metabolic profile with liver enzymes, and sedimentation rate should be obtained.4
Treatment
The treatment of cutaneous mastocytosis is symptomatic, as it is typically a benign disease. The goal of therapy is to prevent mast cell activation, and hence the symptoms that occur when mast cells release their mediators, by avoiding obvious triggers.4
NSAIDs have been reported to cause mast cell mediator release and should therefore be avoided. Since extremes in temperature—particularly heat—can lead to mast cell activation, it is important to control the temperature of a bath or swimming pool and to be wary of exposure to air conditioning. Though easier said than done, soothing crying babies and children is also helpful, as irritability is a known trigger. Management of anxiety and avoidance of stress when possible is recommended.2
Treatment usually begins with H1 and H2 blockers. Cetirizine and diphenhydramine work to control the itching, while ranitidine and famotidine help manage gastric acid secretion when there are symptoms of abdominal pain and peptic ulcer disease.3 Hydroxyzine is effective in controlling both itch and gastric acid secretion.4 Water-soluble cromolyn sodium cream helps to decrease the itch and flare of a mastocytoma; the oral form is also effective.3 Another option to relieve itching is to apply topical corticosteroids with an occlusive dressing.
An epinephrine auto-injector is recommended due to the risk for anaphylaxis; this risk, however, has not been clearly established in cutaneous mastocytosis, specifically in DCM. During an acute and severe flare that induces hypotension, wheezing, and/or laryngeal edema, epinephrine should be administered while the child is lying down.3,4
Surgical excision can be considered when other treatment options fail, or if the lesion is located on the scalp, flexure area, palm, or sole.3,4
Prognosis
The prognosis for a child with a solitary mastocytoma is extremely good. By the time the child reaches puberty, there is typically spontaneous regression.
If any type of mastocytoma persists beyond adolescence, or tryptase levels continue to rise after puberty, however, that raises concern for progression to systemic mastocytosis. Although this diagnosis is rare in children, bone marrow studies may be necessary to determine the patient’s course.1
OUTCOME FOR THE CASE PATIENT
The patient was placed on daily cetirizine. His parents were advised not to irritate the lesion and were educated on possible triggers, including the need to avoid NSAIDs. They were also trained in the use of an epinephrine auto-injector.
CONCLUSION
Cutaneous mastocytosis should be included in the differential diagnosis of rashes and skin lesions in pediatric patients. It is important to be able to recognize the presenting signs and symptoms of a mastocytoma and to monitor the lesion over time.4 Educating the child’s parents, teachers, and caregivers about potential triggers and treatment of a mast cell activation attack can help minimize the symptoms.
1. Frieri M, Quershi M. Pediatric mastocytosis: a review of the literature. Pediatr Allergy Immunol Pulmonol. 2013;26(4):175-180.
2. Castells M, Metcalfe DD, Escribano L. Guidelines for the diagnosis and treatment of cutaneous mastocytosis in children. Am J Clin Dermatol. 2011;12(4):259-270.
3. Castells M, Metcalfe DD, Escribano L. Diagnosis and treatment of cutaneous mastocytosis in children: practical recommendations. Am J Clin Dermatol. 2011;12(4):259-270.
4. Krishnan K, Ownby DR. A solitary mastocytoma presenting with urticaria and angioedema in a 14-year-old boy. Allergy Asthma Proc. 2010;31(6):520-523.
5. Fogelson SK, Dohil MA. Papular and nodular skin lesions in children. Semin Plast Surg. 2006;20(3):180-191.
6. Alvarez-Twose I, Vañó-Galván S, Sánchez-Muñoz L, et al. Increased serum baseline tryptase levels and extensive skin involvement are predictors for the severity of mast cell activation episodes in children with mastocytosis. Allergy. 2012;67(6):813-821.
1. Frieri M, Quershi M. Pediatric mastocytosis: a review of the literature. Pediatr Allergy Immunol Pulmonol. 2013;26(4):175-180.
2. Castells M, Metcalfe DD, Escribano L. Guidelines for the diagnosis and treatment of cutaneous mastocytosis in children. Am J Clin Dermatol. 2011;12(4):259-270.
3. Castells M, Metcalfe DD, Escribano L. Diagnosis and treatment of cutaneous mastocytosis in children: practical recommendations. Am J Clin Dermatol. 2011;12(4):259-270.
4. Krishnan K, Ownby DR. A solitary mastocytoma presenting with urticaria and angioedema in a 14-year-old boy. Allergy Asthma Proc. 2010;31(6):520-523.
5. Fogelson SK, Dohil MA. Papular and nodular skin lesions in children. Semin Plast Surg. 2006;20(3):180-191.
6. Alvarez-Twose I, Vañó-Galván S, Sánchez-Muñoz L, et al. Increased serum baseline tryptase levels and extensive skin involvement are predictors for the severity of mast cell activation episodes in children with mastocytosis. Allergy. 2012;67(6):813-821.
