User login
DALLAS – Five newly recognized clinical predictors are useful in identifying which children with anaphylaxis are at increased risk for a biphasic reaction.
"Children who match none of the five criteria can actually be discharged sooner from the ED [emergency department]. These predictors can potentially improve the efficiency and quality of care in the ED," Dr. Waleed Alqurashi said at the annual meeting of the Society for Academic Emergency Medicine.

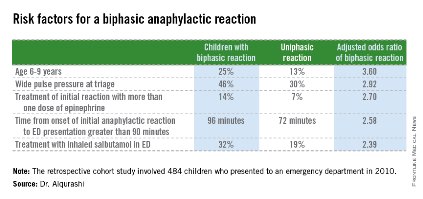
The five risk factors are age of 6-9 years, a wide pulse pressure at triage, treatment of initial reaction requiring more than one dose of epinephrine, time from onset of initial anaphylactic reaction to ED presentation, and treatment with inhaled salbutamol in the ED (see graphic).
The other key – and surprising – finding was that prophylactic administration of systemic corticosteroids was ineffective in preventing biphasic reactions. The result is at odds with classic teaching regarding the benefit of prophylactic steroids in patients with anaphylaxis. "This is the largest study to date of biphasic reactions in children, and we found no association. Also, there’s no biologic plausibility for systemic steroids to prevent anaphylaxis," asserted Dr. Alqurashi of Children’s Hospital of Eastern Ontario, Ottawa.
He presented a multicenter, retrospective cohort study of 484 children who presented with anaphylaxis to an ED during 2010. Biphasic reaction – the recurrence of anaphylactic symptoms at least 1 hour after initial resolution despite no additional exposure to the antigen – occurred in 71 (14.7%).
These biphasic events can be potentially fatal, he said. The 2010 guidelines on anaphylaxis from the National Institute of Allergy and Infectious Diseases underscore the fact that significant knowledge gaps exist regarding the incidence, predictors, and treatment of biphasic reactions (J. Allergy Clin. Immunol. 2010;126:S1-58).
In the Canadian study, 49% of biphasic reactions were sufficiently severe as to require treatment with epinephrine. Three-quarters of these children developed their biphasic reaction prior to ED discharge, at a median of 4.7 hours following onset of the initial reaction. Onset in those whose biphasic reaction occurred after ED discharge was a median of 18.5 hours after onset of the first anaphylactic reaction.
No validated anaphylaxis severity score exists, Dr. Alqurashi remarked, so it wasn’t possible to analyze the relationship between initial reaction severity and likelihood of a subsequent biphasic event. However, several of the clinical predictors identified in this study via multivariate logistic regression analysis are clearly proxies for a more severe reaction.
"If a patient had a severe biphasic reaction, it was more likely to occur within 6 hours. So those with a mild initial anaphylactic reaction, if they don’t match any of these five criteria, can be sent home early. The majority of biphasic reactions occurring after ED discharge did not require epinephrine therapy," he observed.
Anaphylaxis is no longer a rare event, according to Dr. Alqurashi. During the last decade, rates for food-induced anaphylaxis have climbed 350% and for non–food-induced anaphylaxis 230%.
Dr. Marianne Gausche-Hill rose from the audience to comment that she gleaned a slightly different lesson.
"My take-home message from this study is if [patients] didn’t have any of the risk factors, maybe you could discharge them in 6 hours because they’re really unlikely to get into trouble. But if they have any risk factor, it’s probably best just to admit them overnight, which is our standard practice," said Dr. Gausche-Hill, professor of emergency medicine and director of the division of pediatric emergency medicine at Harbor-UCLA Medical Center, Los Angeles.
Dr. Alqurashi reported having no financial conflicts of interest with regard to his study, which was conducted free of commercial support.
DALLAS – Five newly recognized clinical predictors are useful in identifying which children with anaphylaxis are at increased risk for a biphasic reaction.
"Children who match none of the five criteria can actually be discharged sooner from the ED [emergency department]. These predictors can potentially improve the efficiency and quality of care in the ED," Dr. Waleed Alqurashi said at the annual meeting of the Society for Academic Emergency Medicine.

The five risk factors are age of 6-9 years, a wide pulse pressure at triage, treatment of initial reaction requiring more than one dose of epinephrine, time from onset of initial anaphylactic reaction to ED presentation, and treatment with inhaled salbutamol in the ED (see graphic).
The other key – and surprising – finding was that prophylactic administration of systemic corticosteroids was ineffective in preventing biphasic reactions. The result is at odds with classic teaching regarding the benefit of prophylactic steroids in patients with anaphylaxis. "This is the largest study to date of biphasic reactions in children, and we found no association. Also, there’s no biologic plausibility for systemic steroids to prevent anaphylaxis," asserted Dr. Alqurashi of Children’s Hospital of Eastern Ontario, Ottawa.
He presented a multicenter, retrospective cohort study of 484 children who presented with anaphylaxis to an ED during 2010. Biphasic reaction – the recurrence of anaphylactic symptoms at least 1 hour after initial resolution despite no additional exposure to the antigen – occurred in 71 (14.7%).
These biphasic events can be potentially fatal, he said. The 2010 guidelines on anaphylaxis from the National Institute of Allergy and Infectious Diseases underscore the fact that significant knowledge gaps exist regarding the incidence, predictors, and treatment of biphasic reactions (J. Allergy Clin. Immunol. 2010;126:S1-58).
In the Canadian study, 49% of biphasic reactions were sufficiently severe as to require treatment with epinephrine. Three-quarters of these children developed their biphasic reaction prior to ED discharge, at a median of 4.7 hours following onset of the initial reaction. Onset in those whose biphasic reaction occurred after ED discharge was a median of 18.5 hours after onset of the first anaphylactic reaction.
No validated anaphylaxis severity score exists, Dr. Alqurashi remarked, so it wasn’t possible to analyze the relationship between initial reaction severity and likelihood of a subsequent biphasic event. However, several of the clinical predictors identified in this study via multivariate logistic regression analysis are clearly proxies for a more severe reaction.
"If a patient had a severe biphasic reaction, it was more likely to occur within 6 hours. So those with a mild initial anaphylactic reaction, if they don’t match any of these five criteria, can be sent home early. The majority of biphasic reactions occurring after ED discharge did not require epinephrine therapy," he observed.
Anaphylaxis is no longer a rare event, according to Dr. Alqurashi. During the last decade, rates for food-induced anaphylaxis have climbed 350% and for non–food-induced anaphylaxis 230%.
Dr. Marianne Gausche-Hill rose from the audience to comment that she gleaned a slightly different lesson.
"My take-home message from this study is if [patients] didn’t have any of the risk factors, maybe you could discharge them in 6 hours because they’re really unlikely to get into trouble. But if they have any risk factor, it’s probably best just to admit them overnight, which is our standard practice," said Dr. Gausche-Hill, professor of emergency medicine and director of the division of pediatric emergency medicine at Harbor-UCLA Medical Center, Los Angeles.
Dr. Alqurashi reported having no financial conflicts of interest with regard to his study, which was conducted free of commercial support.
DALLAS – Five newly recognized clinical predictors are useful in identifying which children with anaphylaxis are at increased risk for a biphasic reaction.
"Children who match none of the five criteria can actually be discharged sooner from the ED [emergency department]. These predictors can potentially improve the efficiency and quality of care in the ED," Dr. Waleed Alqurashi said at the annual meeting of the Society for Academic Emergency Medicine.

The five risk factors are age of 6-9 years, a wide pulse pressure at triage, treatment of initial reaction requiring more than one dose of epinephrine, time from onset of initial anaphylactic reaction to ED presentation, and treatment with inhaled salbutamol in the ED (see graphic).
The other key – and surprising – finding was that prophylactic administration of systemic corticosteroids was ineffective in preventing biphasic reactions. The result is at odds with classic teaching regarding the benefit of prophylactic steroids in patients with anaphylaxis. "This is the largest study to date of biphasic reactions in children, and we found no association. Also, there’s no biologic plausibility for systemic steroids to prevent anaphylaxis," asserted Dr. Alqurashi of Children’s Hospital of Eastern Ontario, Ottawa.
He presented a multicenter, retrospective cohort study of 484 children who presented with anaphylaxis to an ED during 2010. Biphasic reaction – the recurrence of anaphylactic symptoms at least 1 hour after initial resolution despite no additional exposure to the antigen – occurred in 71 (14.7%).
These biphasic events can be potentially fatal, he said. The 2010 guidelines on anaphylaxis from the National Institute of Allergy and Infectious Diseases underscore the fact that significant knowledge gaps exist regarding the incidence, predictors, and treatment of biphasic reactions (J. Allergy Clin. Immunol. 2010;126:S1-58).
In the Canadian study, 49% of biphasic reactions were sufficiently severe as to require treatment with epinephrine. Three-quarters of these children developed their biphasic reaction prior to ED discharge, at a median of 4.7 hours following onset of the initial reaction. Onset in those whose biphasic reaction occurred after ED discharge was a median of 18.5 hours after onset of the first anaphylactic reaction.
No validated anaphylaxis severity score exists, Dr. Alqurashi remarked, so it wasn’t possible to analyze the relationship between initial reaction severity and likelihood of a subsequent biphasic event. However, several of the clinical predictors identified in this study via multivariate logistic regression analysis are clearly proxies for a more severe reaction.
"If a patient had a severe biphasic reaction, it was more likely to occur within 6 hours. So those with a mild initial anaphylactic reaction, if they don’t match any of these five criteria, can be sent home early. The majority of biphasic reactions occurring after ED discharge did not require epinephrine therapy," he observed.
Anaphylaxis is no longer a rare event, according to Dr. Alqurashi. During the last decade, rates for food-induced anaphylaxis have climbed 350% and for non–food-induced anaphylaxis 230%.
Dr. Marianne Gausche-Hill rose from the audience to comment that she gleaned a slightly different lesson.
"My take-home message from this study is if [patients] didn’t have any of the risk factors, maybe you could discharge them in 6 hours because they’re really unlikely to get into trouble. But if they have any risk factor, it’s probably best just to admit them overnight, which is our standard practice," said Dr. Gausche-Hill, professor of emergency medicine and director of the division of pediatric emergency medicine at Harbor-UCLA Medical Center, Los Angeles.
Dr. Alqurashi reported having no financial conflicts of interest with regard to his study, which was conducted free of commercial support.
AT SAEM 2014
Key clinical point: Children with anaphylaxis may reasonably be discharged from the ED at 6 hours provided they don’t have any of five newly identified clinical predictors of increased risk for a biphasic reaction.
Major finding: In children presenting to the ED with anaphylaxis, 75% of biphasic reactions occurred within 6 hours after the onset of the initial reaction. Biphasic reactions occurring after more than 6 hours were seldom severe.
Data source: This was a multicenter, retrospective cohort study of 484 children who presented to EDs with anaphylaxis during 2010.
Disclosures: Dr. Alqurashi reported having no financial conflicts of interest with regard to his study, which was conducted free of commercial support.