User login


-

-

- Approximately 40% of people who undergo primary surgery develop adhesions and reformation occurs in 80% to 90% of cases.
- Microsurgical techniques such as gentle handling of tissues, careful hemostasis, and avoidance of heat may help reduce the incidence.
- Laparoscopy appears to be less likely to produce adhesions than laparotomy.
- Ob/Gyns should be aware of the potential for adhesion-related bowel obstruction and take steps to prevent it.
Are adhesions a pathologic response to injury or a normal aspect of healing? Can they be avoided, or are preventive efforts part of the problem? How useful are the different barriers in gynecologic surgery? What is the ideal adjuvant?
OBG Management convened a panel of experts to explore these and other questions.
Common problem, high recurrence rate
DECHERNEY: Adhesion formation is serious because it is associated with clinical entities such as infertility, pelvic pain, and bowel obstruction. We all agree that approximately 40% of people who undergo primary surgery develop adhesions and that 80% to 90% of patients who undergo lysis develop recurrent adhesions.
SANFILIPPO: One study several years ago explored adhesion formation.1 Unfortunately, no matter how meticulous the surgeon is, adhesions will form, even with microsurgical techniques and carefully ensured hemostasis.
HURD: The number of patients with significant adhesion formation after some gynecologic procedures has been reported to be greater than 90%.2
DECHERNEY: That higher incidence usually occurs after general surgery—and there’s a reason it is so high: General surgeons don’t use adjunctive therapy. They are critical of it. It is to our credit as gynecologic surgeons that we adopted adjunctive therapies about 15 years ago with the introduction of dextran 70 (Hyskon; Medisan Pharmaceuticals, Parsippany, NJ).
PAGIDAS: If anything, the pelvis seems to have even more of a predilection for adhesion formation than the abdomen, probably because of the close proximity of structures.
How and why adhesions form
DECHERNEY: What is the pathophysiology of adhesion formation? Let’s say you have 2 raw surface areas. What happens?
The process
PAGIDAS: The increase in leukotrienes and prostaglandins and the decrease in plasminogen activity (which actually initiates the inflammation) appear to be significant.
HURD: Vessel permeability also increases, and inflammatory cells leak through the vessels and set up a matrix for adhesion formation.
DECHERNEY: So we have 2 raw surface areas with fibrin leaking out and forming bridges between them.
PAGIDAS: The key is that it takes 2 surfaces to form these bridges. As I mentioned, the greater proximity of pelvic structures—particularly around the tube and ovary—probably contributes to adhesion formation.
DECHERNEY: Macrophage activity also is important. The macrophage “migrates” along these fibrin bridges and lays down collagen over a period of time. Then the collagen becomes organized and, eventually, vascular.
Window of opportunity
SANFILIPPO: Adhesion formation probably occurs and is pretty well established within 5 to 7 days of the precipitating event—usually surgery. Once that process is under way, attempts to halt it yield diminishing returns. Unfortunately, we don’t know how to interfere with it in a positive way.
HURD: Under normal conditions, there seems to be a balance between fibrin deposition and fibrinolysis. In some tissues, however, these functions become imbalanced. This disparity may contribute more to adhesions than the actual laying down of fibrin—especially in tissue that is hypoxic.
DECHERNEY: Would you say that adhesion formation represents normal or abnormal healing?
HURD: It is one of the body’s normal protective mechanisms and an important part of healing. Without it, any abdominal injury would likely result in death.
SANFILIPPO: I don’t think it differs that much from processes that occur externally. For example, if you get cut deeply enough, you develop a scar. Is that scar part of the normal healing process? It is.
PAGIDAS: Right. It is a normal process of tissue remodeling. The question is: What allows it to go astray?
What surgical techniques help prevent adhesions?
DECHERNEY: Let’s review the aspects of surgical technique that are important for adhesion prevention.
PAGIDAS: I emphasize the value of microsurgical techniques, which help to minimize severe tissue handling. It also is important to keep surfaces moistened so they don’t desiccate.
SANFILIPPO: I agree with Dr. Pagidas about microsurgical techniques such as gentle tissue handling, careful hemostasis, and keeping tissues moist. If we follow these principles, we create an environment that minimizes the potential for adhesion formation.
HURD: The findings of many well-controlled animal studies have been surprising. For example, it is difficult to demonstrate that drying of tissue increases adhesions.3 Probably the greatest contributor to adhesions in these models was abrasion.4 One way that laparoscopic surgery decreases adhesions is by avoiding abrasion of the bowel mucosa, which occurs specifically with packing.
A 38-year-old mother of 2 undergoes myomectomy for menorrhagia.
SANFILIPPO: The initial question is: Can this case be managed laparoscopically? I do myomectomies laparoscopically whenever possible, although I do close the uterus with a minilaparotomy incision. The reason is my strong concern about reapproximating the myometrium, since wound dehiscence sometimes occurs at the site of myoma removal.
In this case, depending on the size of the myomas, I would do as much as possible laparoscopically and then reapproximate the myometrium. I would plan my incisions carefully, to maximize the number of myomas that can be removed. I would end with meticulous hemostasis and, assuming it is successful, use a barrier over the incision—in this case, Interceed.
HURD: Does the patient desire future childbearing? If so, I would avoid the laparoscopic approach because of the possibly increased risk of uterine rupture during pregnancy. If she isn’t planning pregnancy, there are more options.
The next question is: How many myomas are there, and where are they located? If they are intrauterine, a hysteroscopic approach would avoid extrauterine adhesions. If they are multiple and large, I am pretty much limited to laparotomy. If there is 1 or only a few myomas, a laparoscopic approach would be best.
I have not used Interceed. In laparoscopic cases, I worry that it would create more problems because, as you allow the carbon dioxide to decrease at the end of a case, oozing begins. Instead of a barrier, I would use limited hydroflotation.
SANFILIPPO: That’s a good point. At the end of the myomectomy, with the laparoscope in place, I decrease the insufflation, eliminating the tamponade effect. Then, assuming good hemostasis, I apply Interceed.
HURD: With open cases, I use Seprafilm, which takes practice because, as it gets wet, it sticks to anything, including gloves and instruments. But if you can put it down dry on the uterus, it sticks and stays in place. If oozing occurs, it seems to block or stop it.
PAGIDAS: I want to reiterate the importance of determining whether childbearing is an issue. In this case, the biggest concern is the risk of adhesions developing on our incision, so I would use a barrier. My preference would be Seprafilm or GoreTex. If we can limit adhesions at the incision site, then hopefully we can minimize bowel and tuboovarian adhesions, too.
In open cases, one thing we can do to minimize the risk of adhesions is to pack gently when needed. Also, we should avoid using packing to reposition the bowel.
Another factor frequently overlooked is the application of heat, which appears to be a very effective way to create adhesions. This probably isn’t an issue for laparoscopic cases, but when you use irrigation fluid in an open case, watch the temperature. If it feels hot to you, you need to worry about potential injury to the bowel surfaces.
PAGIDAS: That is critical. In abdominal cases you want to make sure irrigation fluid is warm, but not too warm, because heat increases the vascular permeability of vessels and leads to more macrophages, more prostaglandins, and more leukotrienes.
HURD: Another important element is the type of suture material used.
DECHERNEY: Overall, we need to minimize the use of sutures. For example, when I am operating laparoscopically on an ovarian cyst, I try to apply bipolar energy to the edges so that they will coapt without a stitch.
HURD: When it first became clear that suturing ovaries increased adhesion formation, we conducted a controlled trial of different kinds of sutures in animals. Not surprisingly, we found that the less reactive the suture, the fewer adhesions.5 Sutures that are absorbed more slowly, such as polydioxanone, seem to be less reactive.
Obviously, inert sutures like nylon are the least reactive, but they are permanent. It is assumed that animal-protein sutures such as chromic and plain gut are the most reactive, although I am not sure there are sufficient data to support that conclusion.
Multiple clinical studies have shown laparoscopy to be associated with a lower adhesion rate, although it isn’t clear why. It may be related to decreased suturing.
DECHERNEY: Bulk is important, too—that is, the number of throws in the suture. When Vicryl (polyglactin 910) became available, we conducted a study in mice using proportionately small Vicryl plaques to determine whether this would be good a barrier (A. DeCherney, MD, unpublished data). It caused a tremendous amount of adhesion because so much foreign matter was applied.
We also did a study using human-size titanium clips in rats (A. DeCherney, MD, unpublished data). Not surprisingly, there was a lot of adhesion formation.
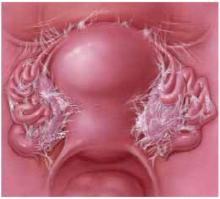
FIGURE 1 Pelvic adhesions: How they develop, problems they cause
Adhesions occur when 2 or more raw surfaces are exposed to leaking fibrin, which forms a bridge between the surfaces. Macrophages “migrate” along these bridges, depositing collagen.
The pelvis has a greater predilection for adhesions than the abdomen because of the close proximity of structures.
Although adhesions represent one of the body’s protective mechanisms, they may also cause pain or interfere with fertility, bowel function, or other processes.
Laparoscopy versus laparotomy: More adhesions in open cases?
DECHERNEY: Based on all the techniques we have learned from microsurgery—with the exception of magnification—it appears that laparoscopic procedures are less likely to cause adhesions than laparotomy. Do you agree?
PAGIDAS: I think so. As Dr. Hurd noted, a main reason is the diminished tissue handling, because there is no packing.
HURD: Multiple clinical studies have shown laparoscopy to be associated with a lower adhesion rate, although it isn’t clear why.6,7 It may be related to decreased suturing.
DECHERNEY: Less bleeding occurs because surgeons are less aggressive laparoscopically than in laparotomy.
A 15-year-old undergoes removal of a dermoid cyst, which was shelled out laparoscopically.
PAGIDAS: This case is easier because the cyst has been successfully shelled out. It is not the spill of a cyst’s contents at surgery that creates adhesions, but a chronic leak, which can occur if you do not remove the cyst in its entirety.
Once the cyst has been excised completely, I would ensure hemostasis with bipolar cautery and reapproximate the edges. I would not suture. There seems to be no clear advantage to suturing. I would use hydroflotation. Although Ringer’s lactate solution has not been shown to be effective, it is safe and has no toxicity.
DECHERNEY: Would you remove the cyst via laparotomy?
PAGIDAS: I would do it laparoscopically, using the endobag to minimize spillage, even though we know that a spill doesn’t necessarily change the outcome. If spillage does occur, I would perform copious irrigation to ensure that nothing is left behind.
HURD: My priority would be minimizing the use of power on the ovary. Studies of ovarian drilling have demonstrated that burning an ovary stimulates adhesion formation.21,22 If the dermoid cyst spills, as happens occasionally, I perform copious rinsing until no more oil is visible on the surface of the peritoneal fluid.
I also would minimize the amount of ovarian capsule that is removed. Good studies of endometriomas have shown that the more capsulate that is removed, the more adhesions. Even if the capsule looks redundant and floppy, the concern should be to achieve hemostasis with bipolar cautery and then leave it alone.
DECHERNEY: Would you use crystalloids in this case?
HURD: Yes.
SANFILIPPO: If spillage occurs, I would ensure that the patient is taken out of the Trendelenburg position. I want to emphasize the importance of thorough irrigation to eliminate any material that could produce chemical peritonitis.
DECHERNEY: Over the years, I have seen a fair number of cases of Fitz-Hugh and Curtis syndrome. You rigorously lavage a ruptured dermoid cyst, which sometimes presents with low-grade fever, but always with pain.
I’m surprised that none of you would use Interceed, since wrapping the ovary is the only thing for which it has been clearly shown to be effective. Since the cortex is relatively avascular, you don’t get a lot of bleeding. Unfortunately, it is not technically easy to wrap the ovary.
HURD: Since we do not know the effect on future fertility of changing the ovarian surface, less would seem to be better in patients this young.
I have stopped doing difficult cases laparoscopically. For example, it is rare for me to operate laparoscopically on a patient with stage IV endometriosis, at least when it comes to infertility—I might consider laparoscopy for pain.
I think case selection plays a role as well, although there are few data to back that up. It is purely clinical opinion.
SANFILIPPO: We need a well-designed prospective study to explore the effects of laparotomy versus laparoscopy. Existing data are not clear. You would assume laparoscopy would be associated with less adhesion formation. But genetic or other factors may explain why patient A is more prone to adhesions than patient B.
Does anybody think carbon dioxide plays a role in adhesion formation?
HURD: In the laboratory, carbon dioxide increases cell growth.8 Without an increased carbon dioxide concentration in the atmosphere, cell cultures don’t grow well. This might suggest that the carbon dioxide used for laparoscopy could actually enhance adhesion growth. Fortunately, this does not appear to be the case clinically.
With myomectomy, the surgeon needs to plan ahead to maximize the number of myomas removed from a single incision.
DECHERNEY: What about second-look laparoscopies? Do any of you perform them after a patient has undergone lysis of adhesions?
SANFILIPPO: Only as part of a research protocol. It amazes me how rapidly adhesions can form and how dense they are 2 or more weeks after the initial laparoscopic surgery.
PAGIDAS: We tend to limit second-look laparoscopy to a research protocol, although it is sometimes valuable after laparoscopic or abdominal myomectomy, which has the highest incidence of adhesions. If the surgeon can perform a second look and lyse adhesions, he or she may potentially alter the reproductive outcome. However, with assisted reproductive techniques becoming integral to every infertility case, that approach has begun to go out of style.
SANFILIPPO: That’s a good point. With myomectomy, the surgeon needs to plan ahead to maximize the number of myomas removed from a single incision. If adhesions do occur, it is best if they occur toward the bladder rather than in the area of the tubes and ovaries.
HURD: For second-look laparoscopy, we must keep in mind the cost and the small but real risks of surgery. Until good controlled studies show a reasonable clinical advantage, this approach probably should remain a research protocol.
SANFILIPPO: The literature suggests it is helpful, but does not help fertility, so second-look laparoscopy is used mainly to evaluate adjunctive therapies. I don’t think anybody uses it as a primary therapy anymore.
Bowel obstruction still a risk, though rarely seen by Ob/Gyns
DECHERNEY: Although bowel obstruction is fairly common, Ob/Gyns do not often encounter it because it occurs relatively distant from the index surgery. Even though a patient may not experience bowel obstruction in the first year, an obstruction related to the index surgery is just as likely to develop 20 years later as 2 years later. These patients usually are treated by general surgeons. Still, we should beware of the potential for bowel obstruction and take steps to prevent it, if at all possible. Do you agree?
PAGIDAS: Yes. We tend to forget about bowel obstruction because we rarely follow patients past pregnancy or the first trimester if they are seeking infertility treatment.
HURD: The primary problem seems to be the abdominal wall incision. Fortunately, cesarean section seems to carry a decreased risk of abdominal wall adhesions, probably because the uterus serves as a splint over the incision.
The Pfannenstiel incision also appears to have some advantage. Both human and animal models suggest little advantage or disadvantage when peritoneal closure is compared to nonclosure.9,10
SANFILIPPO: I’m curious about how the panelists manage loose clips. If you are using an EndoGIA (US Surgical, Norwalk, Conn) or other stapling device and you have free-floating clips, do you make a concerted effort to find them? In some cases, they have been implicated in bowel adhesion and obstruction. I try to retrieve loose clips, whether open or closed.
HURD: The advantage of those devices is minimal tissue damage, and the clips are inert. In general, inert, nonreactive clips have not been implicated as much in adhesion formation. I retrieve them if I see them, but I don’t search them out.
PAGIDAS: I do the same. If the clips are visible, I remove them. But I would not repack the bowel or do anything more heroic than look in locations where they might be.
What drugs may inhibit inflammatory response?
DECHERNEY: What about use of pharmacologic agents to prevent adhesions? Is there reason to think research should focus on inhibiting the inflammatory response? How important is polymorphonuclear cell infiltration?
Cyclooxygenase (COX) 2 agents could be helpful for inhibition of platelet function, since they are low in side effects. Thus, high doses of these drugs might be effective. At one time, aspirin was proposed, but you’d have to give a human so much aspirin that her ears would ring.
PAGIDAS: Pharmacologic agents have a role, especially for dampening the inflammatory immune response. But you don’t want to dampen it completely because, as we observed, it is an important part of healing. The difficulty is finding a balance between allowing the tissue to heal and preventing adhesions.
HURD: We studied the ability of a water-soluble prostaglandin inhibitor to prevent postoperative adhesion formation. Like many other agents, we found only a partial response.11
DECHERNEY: With current options, the best you can aim for is a 50% reduction.
Adjunctive therapy likely to limit adhesion rate Hydroflotation
DECHERNEY: The original adjunctive therapy was 20 mg dexamethasone and 25 mg femergin in 200 cc of Ringer’s lactate, with an equivalent amount of dexamethasone and femergin every 4 hours for a total of 6 doses. I prescribed that regimen because I was trained to do so. I stopped after it became clear that hydroflotation from the fluid—not the medication itself—was responsible for the improvement.
I must admit I gave it up reluctantly; patients felt fabulous with those higher load doses of glucocorticoids after surgery.
Do any of you use crystalloids as adjunctive therapy?
SANFILIPPO: In the animal model, they are so rapidly absorbed that they aren’t effective. I was a strong advocate, but now I don’t use them at all.
HURD: A lot depends on the kind of case. For instance, at the end of an open myomectomy, the patient often is oozing, so you want to use a barrier that blood won’t affect.
For ovarian surgery, you might want to specifically target the ovaries with some kind of coverage. But when you are doing a broad lysis of adhesions, you have few choices to cover the pelvis. In those cases I use hydroflotation with Ringer’s lactate. Both human and animal studies have shown some benefit in preventing adhesions, and it appears to have little risk.12,13
It’s better than nothing, in my opinion.
DECHERNEY: Do you use dextran 70 or crystalloids?
HURD: I use Ringer’s lactate solution. I was trained in the dextran 70 era, and there were certain problems with that approach. Since studies have failed to show a consistent effect of dextran 70, I no longer use this solution.14,15
DECHERNEY: Another problem with crystalloids is that they leak, which is disconcerting to the patient.
HURD: They also can mask an injury to the bladder in difficult cases.
DECHERNEY: I agree that dextran 70 is only appropriate in certain cases, but it is a good hydroflotation agent. Every cubic centimeter of dextran 70 brings in 1.2 cc of transudate, so it hangs around for at least 4 days.
It is appropriate only for certain surface areas—mainly the cul-de-sac. It is harmful on raw surface areas on the lateral pelvic sidewall because it tends to push the ovary and tube to those areas. Unless you are doing a lot of work in the deep pelvis, I would avoid dextran 70.
A 45-year-old woman undergoes an abdominal hysterectomy. The cuff is closed and the ovaries are intact.
PAGIDAS: I would do nothing other than ensure adequate hemostasis, check that I have left no round surfaces and, probably, use hydroflotation. I see no advantage to barriers.
HURD: One of the main causes of adhesions is devascularized tissue, and the perfect devascularized tissue might be the vaginal cuff. Re-“peritonealizing” the cuff might be advantageous. Thus, I would use minimal sutures—probably a slowly absorbable, light polydioxanone suture to place the peritoneum over the cuff so there are no pedicles.
DECHERNEY: All the pedicles are exteriorized.
HURD: Yes, that could be. We don’t bring all of it down like we used to years ago, but we do cover the cuff.
PAGIDAS: I agree that closing the cuff and reperitonealizing may actually minimize formation of hematomas—clearly an advantage.
SANFILIPPO: I agree. I guess I’m old fashioned. If it looks good, then hopefully it will stimulate less adhesion formation, so peritonealization is important.
As far as the abdominal incision is concerned, I would not close that peritoneum. I’m convinced now that there is no advantage.
DECHERNEY: Reperitonealizing the cuff is controversial. Most gynecologic surgeons do not do it, the theory being that the peritoneum is being stretched, attenuating the vessels that go through it and thereby creating an ischemic barrier that contributes to adhesions. Personally, I like to do it because it looks better—and that is certainly an important aspect of a surgery. No evidence shows that it is bad or good, either way.
In addition, there have been allergic reactions, most of which seem to occur in patients with fluid overload; a lot of the dextran 70 is absorbed.
With infertility patients, even if you lyse dense adhesions, you do not render the ovarian surface normal.
SANFILIPPO: Dextran 70 is not recommended for patients with sugar beet allergy, either.
We completed a study in a rabbit model, in which the peritoneal cavity was lavaged with either chlorhexidine or iodine.16 At the time of second-look surgery, the rate of adhesion formation was decreased, especially with the iodine preparation. I would hope that this has potential in humans.
DECHERNEY: In your lavage procedures to prevent adhesions, do any of you use heparin?
HURD: No.
PAGIDAS: I don’t think any evidence suggests that local administration changes the outcome.
DECHERNEY: I agree. When heparin has been used, the doses have been so low that it was not terribly helpful. And when you consider that hemorrhage can be a problem, heparin is probably deleterious rather than helpful.
Barriers
DECHERNEY: What about barriers? The first to become available, Interceed (Gynecare, a division of Ethicon, Somerville, NJ), is oxidized cellulose, similar to Surgicell (Johnson & Johnson, New Brunswick, NJ). Since it gelates quickly, there is no fenestration, so the fibrin is unable to penetrate. However, if the patient has bleeding by capillary action, the raw surface just moves from one side of the Interceed barrier to the other.
What has been your experience? Do you use it?
PAGIDAS: I do not use Interceed, although prospective randomized trials and a meta-analysis confirmed its benefits in de novo formation and reformation.17-19 I don’t use it because it requires complete hemostasis. Also, with the surfaces we work on—notably, the ovary and tube—it is difficult to apply to just 1 surface area. From a clinical perspective, I appreciate the data, but it is hard to ensure a good application to optimize its effectiveness.
A 29-year-old woman is undergoing her third cesarean section, although adhesions cause difficulty getting through anteriorly.
DECHERNEY: In this case, will you use barriers or re-peritonealize the surface? Will you do a 1- or a 2-layered closure?
HURD: In these cases, I have not been doing anything, since there is no peritoneum to reperitonealize—just old scar tissue. I assume that the uterus will immediately readhere to the anterior peritoneum where it was before.
DECHERNEY: You would use a barrier?
HURD: No. I would not.
PAGIDAS: I would take the same approach, although I have not performed cesarean sections in about 4 years. I don’t think any intervention would change the outcome. And, as Dr. Hurd mentioned, that is pretty much old scar tissue anyway.
SANFILIPPO: I use Interceed, but I agree with you about its limitations. Meticulous hemostasis is a prerequisite.
HURD: With infertility patients, even if you lyse dense adhesions, you do not render the ovarian surface normal. If those patients have dense adhesions of the ovary or the sidewall, I generally leave them alone, and I try to avoid putting Interceed around the ovaries. No study has shown that using Interceed improves pregnancy.
In contrast, when a chronic pain patient’s ovaries are densely adherent to the cul-de-sac, which appears to be highly associated with dyspareunia, I lyse the adhesions, achieve meticulous hemostasis, and then use Interceed. It is hard to demonstrate in a study that this approach decreases the chance of pain. Even so, it certainly does decrease the chance of the ovaries being adherent.
DECHERNEY: One issue with Interceed is that we don’t know what happens to it once the abdomen is closed. It may migrate significantly.
Psychological issues may also be involved. For example, patients with multiple somatic complaints may be less likely to benefit from lysis of adhesions.
PAGIDAS: Right. Interestingly, a meta-analysis of all the randomized trials involving mechanical barriers found no correlation to pregnancy outcome or pelvic pain.18 If we were to consider new trials, the psychological aspect would be worth looking into.
Seprafilm
DECHERNEY: Let’s move on to Seprafilm (Genzyme, Cambridge, Mass). What is it and how useful is it?
HURD: Seprafilm is modified hyaluronic acid, which forms a brittle, thin plastic layer. It is somewhat difficult to work with but, once it is in place, seems to adhere well. The presence of blood does not appear to be a problem, since the Seprafilm forms an impermeable barrier—unless it breaks. I have found it especially useful in myomectomies, which produce postoperative oozing through the incisions no matter how hard you try to prevent it.
In addition, in open cases, surfaces can easily be covered with this material. Unfortunately, it can’t be used laparoscopically because it is so brittle.
DECHERNEY: In my opinion, that is its major drawback.
PAGIDAS: In cardiac surgery, Seprafilm appears to work quite effectively.
SANFILIPPO: The manufacturer initially focused on surgeons in the context of sigmoid colon surgery, and it seems to work well in that setting.
Intergel
DECHERNEY: That brings us to the current state of the art: gels. I’m sure you all are familiar with Intergel (Lifecore Biomedical, Chaska, Minn), which is a ferrous derivative of hyaluronic acid that works by coating the raw surface areas. It also has the theoretical advantage of ease of use. Have any of you used Intergel?
HURD: As you know it was only recently approved by the US Food and Drug Administration, but not for laparoscopic use. It may work best on abraded bowel, which is avoided by laparoscopic surgery.
As you are probably also aware, the manufacturer recently took it off the market because of unusual side effects, namely a chemical peritonitis. Although peritonitis was cited as being rare, we encountered it in probably half the patients we operated on.
PAGIDAS: When we used it on hospitalized patients, the peritonitis wasn’t that obvious, since there was an expectation of significant pain. However, when we used Intergel on short-stay patients, we had to readmit them and do a full workup because we were concerned about bowel perforations. I’m surprised the manufacturer didn’t take it off the market sooner.
DECHERNEY: It seems strange, since Intergel has been used in Europe for a while now. I’ve used it in only 1 case and didn’t have adverse effects. It seemed to work well.
SANFILIPPO: It had all the right ingredients for success. It is unfortunate that these side effects have prohibited its use.
There is no question that adhesion prevention is one of the unmet challenges in all surgeries, especially reproductive surgery.
Gels and the cost factor
DECHERNEY: Other gels are in the pipeline. I’m reminded of plasminogen activator, which is a powerful antiadhesive agent that lyses fibrin effectively. Unfortunately, it is prohibitively expensive.
The next phase likely will involve the so-called polymers. If you spray them on your hand, they are activated by light or another chemical and become a cellophane-like substance. The problem is viscosity. If sprayed on the sidewall, for instance, they run halfway down before they are activated, so the entire surface does not get covered.
PAGIDAS: One concern with polymers is that they could actually bring surfaces together when they polymerize. We still have a lot to learn.
DECHERNEY: Let’s say a new gel comes on the market that takes reformation adhesions from 90% to 10%, as opposed to 40% recurrence. Would you use it in all 4 of the cases we discuss here?
HURD: If it was that effective and had no adverse effects, it would be wonderful.
The cesarean-delivery case is different, as healing in a pregnant patient is 1 concern; the size of the uterus also has an effect. If the patient is breastfeeding, you would want to make sure the gel didn’t interfere.
PAGIDAS: We desperately need a product that can minimize adhesions regardless of the route of access or type of procedure. Even though we lack data on outcomes, I predict wide use of such a product, assuming it is nontoxic and effective.
DECHERNEY: What if it costs $1,000 a case?
SANFILIPPO: If it prevents 1 bowel obstruction, it still would be cost-effective.
DECHERNEY: The incidence of bowel obstruction for total abdominal hysterectomy is 2%, and 5% for radical hysterectomy.
HURD: We must be careful of the cost-benefit ratio. Bowel obstruction after gynecologic surgery is uncommon.
Is the gel worth $100? $1,000? $3,000? It’s difficult to say, but the more expensive it is, the less likely it will find widespread use.
PAGIDAS: I agree. We should remember that we still need to maintain microsurgical techniques and appropriate tissue handling, as well as avoid ischemia and infection.
Looking for the magic bullet
DECHERNEY: What is the future of adjunctive therapy?
SANFILIPPO: I would focus on noxythiolin; it has potential. Calcium channel blockers for adhesion prevention have also been studied.20 In 1 investigation involving a rat model, the calcium channel blocker verapamil as well as several other agents—including vitamin E, carboxymethylcellulose, cyclosporin, aprotinin, and tenoxicam—were compared with respect to tissue effects. A beneficial effect was noted with all agents except cyclosporin and carboxymethylcellulose.
Whoever succeeds in manufacturing an effective preventive will be a winner.
HURD: There is no question that adhesion prevention is one of the unmet challenges in all surgeries, especially reproductive surgery. The most effective agent would be applied intraabdominally, since any systemic agent that stops adhesion formation would probably decrease wound healing as well.
I hope the most effective agents can be used in both laparoscopy and laparotomy, and that they will decrease the adhesion-formation rate by more than 50%. We need to find the magic bullet that can cover the entire pelvis—if not the entire abdomen.
Dr. DeCherney reports small holdings with Lifecore Biomedical and Johnson & Johnson. Drs. Hurd and Pagidas report no financial relationship with any companies whose products are mentioned in this article. Dr. Sanfilippo serves on the speaker’s bureau for Berlex, Ortho Pharmaceuticals, and Wyeth, and receives grant support from Eli Lilly and Wyeth.
1. Operative Laparoscopy Study Group Postoperative adhesion development after operative laparoscopy: evaluation at early second look procedures. Fertil Steril. 1991;55:700-704.
2. Tulandi T, Murray C, Guralnick M. Adhesion formation and reproductive outcome after myomectomy and second-look laparoscopy. Obstet Gynecol. 1993;82:213-215.
3. Larsson B, Perbeck L. The possible advantage of keeping the uterine and intestinal serosa irrigated with saline to prevent intraabdominal adhesions in operations for infertility. An experimental study in rats. Acta Chir Scand Suppl. 1985;530:15-18.
4. Zamir G, Bloom AI, Reissman P. Prevention of intestinal adhesions after laparotomy in a rat model—a randomized prospective study. Res Exp Med (Berl). 1998;197:349-353.
5. Hurd WW, Himebaugh KS, Cofer KF, Gauvin JM, Elkins TE. The etiology of closure-related adhesion formation after wedge resection of the rabbit ovary. J Reprod Med. 1993;38:465-468.
6. Chen MD, Teigen GA, Reynolds HT, Johnson PR, Fowler JM. Laparoscopy versus laparotomy: an evaluation of adhesion formation after pelvic and paraaortic lymphadenectomy in a porcine model. Am J Obstet Gynecol. 1998;178:499-503.
7. Polymeneas G, Theodosopoulos T, Stamatiadis A, Kourias E. A comparative study of postoperative adhesion formation after laparoscopic vs. open cholecystectomy. Surg Endosc. 2001;15:41-43.
8. Smidt VJ, Singh DM, Hurteau JA, Hurd WW. Effect of carbon dioxide on human ovarian carcinoma cell growth. Am J Obstet Gynecol. 2001;185:1314-1317.
9. Tulandi T, Hum HS, Gelfand MM. Closure of laparotomy incisions with or without peritoneal suturing and second look laparoscopy. Am J Obstet Gynecol. 1988;158:536-537.
10. Kapur ML, Daneswar A, Chopra P. Evaluation of peritoneal closure at laparotomy. Am J Surg. 1979;137:650-652.
11. Cofer KF, Himebaugh KS, Gauvin JM, Hurd WW. Inhibition of adhesion reformation in the rabbit model by meclofenamate: an inhibitor of both prostaglandin and leukotriene production. Fertil Steril. 1994;62:1262-1265.
12. Elkelani OA, Molinas CR, Mynbaev O, Koninckx PR. Prevention of adhesions with crystalloids during laparoscopic surgery in mice. J Am Assoc Gynecol Laparosc. 2002;9:447-452.
13. Chan KL, Marino T, Qu WM, Tulandi T. Effects of intraperitoneal Ringer’s lactate instillation and infusion on postsurgical adhesion formation. J Gynecol Surg. 1995;11:241-243.
14. Watson A, Vandekerckhove P, Lilford R. Pharmacological adjuvants during infertility surgery: a systematic review of evidence derived from randomized controlled trial. Hum Fertil (Camb). 1999;2:149-157.
15. Larson B. Dextran—later clinical studies. clinical and experimental evaluation of different adjuvant therapies. Prog Clin Biol Res. 1990;358:165-175.
16. Roberts L, Sanfilippo JS, Ehrlich G, Raab S. Adhesion formation, peritoneal effects and the presence of bacterial biofilms after laparoscopic lavage in an animal model of pelvic inflammatory disease. J Am Assoc Gynecol Laparosc. 2002;9:4.-
17. Barrier agents for preventing adhesions after surgery for subfertility Cochrane Database Syst Rev. 2000;CD000475.-
18. Wiseman DM, Trout JR, Franklin RR, Diamond MP. Metaanalysis of the safety and efficacy of an adhesion barrier (Interceed TC7) in laparotomy. J Reprod Med. 1999;44:325-331.
19. Sawada T, Nishizawa H, Nishio E, Kadowaki M. Postoperative adhesion prevention with an oxidized regenerated cellulose adhesion barrier in infertile women. J Reprod. Med. 2000;45:387-389.
20. Uzunkoy A, Akinci OF, Coskun A, Aslan O, Kocyigit A. Effects of antiadhesive agents on the healing of intestinal anastomosis. Dis Colon Rectum. 2000;43:370-375.
21. Farquhar C, Vandekerckhove P, Arnot M, Lilford R. Laparoscopic “drilling” by diathermy or laser for ovulation induction in anovulatory polycystic ovary syndrome. Cochrane Database Syst Rev. 2000(2);CD001122.-
22. Greenblatt EM, Casper RF. Laparoscopic ovarian drilling in women with polycystic ovarian syndrome. Prog Clin Biol Res. 1993;381:129-138.


-

-

- Approximately 40% of people who undergo primary surgery develop adhesions and reformation occurs in 80% to 90% of cases.
- Microsurgical techniques such as gentle handling of tissues, careful hemostasis, and avoidance of heat may help reduce the incidence.
- Laparoscopy appears to be less likely to produce adhesions than laparotomy.
- Ob/Gyns should be aware of the potential for adhesion-related bowel obstruction and take steps to prevent it.
Are adhesions a pathologic response to injury or a normal aspect of healing? Can they be avoided, or are preventive efforts part of the problem? How useful are the different barriers in gynecologic surgery? What is the ideal adjuvant?
OBG Management convened a panel of experts to explore these and other questions.
Common problem, high recurrence rate
DECHERNEY: Adhesion formation is serious because it is associated with clinical entities such as infertility, pelvic pain, and bowel obstruction. We all agree that approximately 40% of people who undergo primary surgery develop adhesions and that 80% to 90% of patients who undergo lysis develop recurrent adhesions.
SANFILIPPO: One study several years ago explored adhesion formation.1 Unfortunately, no matter how meticulous the surgeon is, adhesions will form, even with microsurgical techniques and carefully ensured hemostasis.
HURD: The number of patients with significant adhesion formation after some gynecologic procedures has been reported to be greater than 90%.2
DECHERNEY: That higher incidence usually occurs after general surgery—and there’s a reason it is so high: General surgeons don’t use adjunctive therapy. They are critical of it. It is to our credit as gynecologic surgeons that we adopted adjunctive therapies about 15 years ago with the introduction of dextran 70 (Hyskon; Medisan Pharmaceuticals, Parsippany, NJ).
PAGIDAS: If anything, the pelvis seems to have even more of a predilection for adhesion formation than the abdomen, probably because of the close proximity of structures.
How and why adhesions form
DECHERNEY: What is the pathophysiology of adhesion formation? Let’s say you have 2 raw surface areas. What happens?
The process
PAGIDAS: The increase in leukotrienes and prostaglandins and the decrease in plasminogen activity (which actually initiates the inflammation) appear to be significant.
HURD: Vessel permeability also increases, and inflammatory cells leak through the vessels and set up a matrix for adhesion formation.
DECHERNEY: So we have 2 raw surface areas with fibrin leaking out and forming bridges between them.
PAGIDAS: The key is that it takes 2 surfaces to form these bridges. As I mentioned, the greater proximity of pelvic structures—particularly around the tube and ovary—probably contributes to adhesion formation.
DECHERNEY: Macrophage activity also is important. The macrophage “migrates” along these fibrin bridges and lays down collagen over a period of time. Then the collagen becomes organized and, eventually, vascular.
Window of opportunity
SANFILIPPO: Adhesion formation probably occurs and is pretty well established within 5 to 7 days of the precipitating event—usually surgery. Once that process is under way, attempts to halt it yield diminishing returns. Unfortunately, we don’t know how to interfere with it in a positive way.
HURD: Under normal conditions, there seems to be a balance between fibrin deposition and fibrinolysis. In some tissues, however, these functions become imbalanced. This disparity may contribute more to adhesions than the actual laying down of fibrin—especially in tissue that is hypoxic.
DECHERNEY: Would you say that adhesion formation represents normal or abnormal healing?
HURD: It is one of the body’s normal protective mechanisms and an important part of healing. Without it, any abdominal injury would likely result in death.
SANFILIPPO: I don’t think it differs that much from processes that occur externally. For example, if you get cut deeply enough, you develop a scar. Is that scar part of the normal healing process? It is.
PAGIDAS: Right. It is a normal process of tissue remodeling. The question is: What allows it to go astray?
What surgical techniques help prevent adhesions?
DECHERNEY: Let’s review the aspects of surgical technique that are important for adhesion prevention.
PAGIDAS: I emphasize the value of microsurgical techniques, which help to minimize severe tissue handling. It also is important to keep surfaces moistened so they don’t desiccate.
SANFILIPPO: I agree with Dr. Pagidas about microsurgical techniques such as gentle tissue handling, careful hemostasis, and keeping tissues moist. If we follow these principles, we create an environment that minimizes the potential for adhesion formation.
HURD: The findings of many well-controlled animal studies have been surprising. For example, it is difficult to demonstrate that drying of tissue increases adhesions.3 Probably the greatest contributor to adhesions in these models was abrasion.4 One way that laparoscopic surgery decreases adhesions is by avoiding abrasion of the bowel mucosa, which occurs specifically with packing.
A 38-year-old mother of 2 undergoes myomectomy for menorrhagia.
SANFILIPPO: The initial question is: Can this case be managed laparoscopically? I do myomectomies laparoscopically whenever possible, although I do close the uterus with a minilaparotomy incision. The reason is my strong concern about reapproximating the myometrium, since wound dehiscence sometimes occurs at the site of myoma removal.
In this case, depending on the size of the myomas, I would do as much as possible laparoscopically and then reapproximate the myometrium. I would plan my incisions carefully, to maximize the number of myomas that can be removed. I would end with meticulous hemostasis and, assuming it is successful, use a barrier over the incision—in this case, Interceed.
HURD: Does the patient desire future childbearing? If so, I would avoid the laparoscopic approach because of the possibly increased risk of uterine rupture during pregnancy. If she isn’t planning pregnancy, there are more options.
The next question is: How many myomas are there, and where are they located? If they are intrauterine, a hysteroscopic approach would avoid extrauterine adhesions. If they are multiple and large, I am pretty much limited to laparotomy. If there is 1 or only a few myomas, a laparoscopic approach would be best.
I have not used Interceed. In laparoscopic cases, I worry that it would create more problems because, as you allow the carbon dioxide to decrease at the end of a case, oozing begins. Instead of a barrier, I would use limited hydroflotation.
SANFILIPPO: That’s a good point. At the end of the myomectomy, with the laparoscope in place, I decrease the insufflation, eliminating the tamponade effect. Then, assuming good hemostasis, I apply Interceed.
HURD: With open cases, I use Seprafilm, which takes practice because, as it gets wet, it sticks to anything, including gloves and instruments. But if you can put it down dry on the uterus, it sticks and stays in place. If oozing occurs, it seems to block or stop it.
PAGIDAS: I want to reiterate the importance of determining whether childbearing is an issue. In this case, the biggest concern is the risk of adhesions developing on our incision, so I would use a barrier. My preference would be Seprafilm or GoreTex. If we can limit adhesions at the incision site, then hopefully we can minimize bowel and tuboovarian adhesions, too.
In open cases, one thing we can do to minimize the risk of adhesions is to pack gently when needed. Also, we should avoid using packing to reposition the bowel.
Another factor frequently overlooked is the application of heat, which appears to be a very effective way to create adhesions. This probably isn’t an issue for laparoscopic cases, but when you use irrigation fluid in an open case, watch the temperature. If it feels hot to you, you need to worry about potential injury to the bowel surfaces.
PAGIDAS: That is critical. In abdominal cases you want to make sure irrigation fluid is warm, but not too warm, because heat increases the vascular permeability of vessels and leads to more macrophages, more prostaglandins, and more leukotrienes.
HURD: Another important element is the type of suture material used.
DECHERNEY: Overall, we need to minimize the use of sutures. For example, when I am operating laparoscopically on an ovarian cyst, I try to apply bipolar energy to the edges so that they will coapt without a stitch.
HURD: When it first became clear that suturing ovaries increased adhesion formation, we conducted a controlled trial of different kinds of sutures in animals. Not surprisingly, we found that the less reactive the suture, the fewer adhesions.5 Sutures that are absorbed more slowly, such as polydioxanone, seem to be less reactive.
Obviously, inert sutures like nylon are the least reactive, but they are permanent. It is assumed that animal-protein sutures such as chromic and plain gut are the most reactive, although I am not sure there are sufficient data to support that conclusion.
Multiple clinical studies have shown laparoscopy to be associated with a lower adhesion rate, although it isn’t clear why. It may be related to decreased suturing.
DECHERNEY: Bulk is important, too—that is, the number of throws in the suture. When Vicryl (polyglactin 910) became available, we conducted a study in mice using proportionately small Vicryl plaques to determine whether this would be good a barrier (A. DeCherney, MD, unpublished data). It caused a tremendous amount of adhesion because so much foreign matter was applied.
We also did a study using human-size titanium clips in rats (A. DeCherney, MD, unpublished data). Not surprisingly, there was a lot of adhesion formation.
FIGURE 1 Pelvic adhesions: How they develop, problems they cause
Adhesions occur when 2 or more raw surfaces are exposed to leaking fibrin, which forms a bridge between the surfaces. Macrophages “migrate” along these bridges, depositing collagen.
The pelvis has a greater predilection for adhesions than the abdomen because of the close proximity of structures.
Although adhesions represent one of the body’s protective mechanisms, they may also cause pain or interfere with fertility, bowel function, or other processes.
Laparoscopy versus laparotomy: More adhesions in open cases?
DECHERNEY: Based on all the techniques we have learned from microsurgery—with the exception of magnification—it appears that laparoscopic procedures are less likely to cause adhesions than laparotomy. Do you agree?
PAGIDAS: I think so. As Dr. Hurd noted, a main reason is the diminished tissue handling, because there is no packing.
HURD: Multiple clinical studies have shown laparoscopy to be associated with a lower adhesion rate, although it isn’t clear why.6,7 It may be related to decreased suturing.
DECHERNEY: Less bleeding occurs because surgeons are less aggressive laparoscopically than in laparotomy.
A 15-year-old undergoes removal of a dermoid cyst, which was shelled out laparoscopically.
PAGIDAS: This case is easier because the cyst has been successfully shelled out. It is not the spill of a cyst’s contents at surgery that creates adhesions, but a chronic leak, which can occur if you do not remove the cyst in its entirety.
Once the cyst has been excised completely, I would ensure hemostasis with bipolar cautery and reapproximate the edges. I would not suture. There seems to be no clear advantage to suturing. I would use hydroflotation. Although Ringer’s lactate solution has not been shown to be effective, it is safe and has no toxicity.
DECHERNEY: Would you remove the cyst via laparotomy?
PAGIDAS: I would do it laparoscopically, using the endobag to minimize spillage, even though we know that a spill doesn’t necessarily change the outcome. If spillage does occur, I would perform copious irrigation to ensure that nothing is left behind.
HURD: My priority would be minimizing the use of power on the ovary. Studies of ovarian drilling have demonstrated that burning an ovary stimulates adhesion formation.21,22 If the dermoid cyst spills, as happens occasionally, I perform copious rinsing until no more oil is visible on the surface of the peritoneal fluid.
I also would minimize the amount of ovarian capsule that is removed. Good studies of endometriomas have shown that the more capsulate that is removed, the more adhesions. Even if the capsule looks redundant and floppy, the concern should be to achieve hemostasis with bipolar cautery and then leave it alone.
DECHERNEY: Would you use crystalloids in this case?
HURD: Yes.
SANFILIPPO: If spillage occurs, I would ensure that the patient is taken out of the Trendelenburg position. I want to emphasize the importance of thorough irrigation to eliminate any material that could produce chemical peritonitis.
DECHERNEY: Over the years, I have seen a fair number of cases of Fitz-Hugh and Curtis syndrome. You rigorously lavage a ruptured dermoid cyst, which sometimes presents with low-grade fever, but always with pain.
I’m surprised that none of you would use Interceed, since wrapping the ovary is the only thing for which it has been clearly shown to be effective. Since the cortex is relatively avascular, you don’t get a lot of bleeding. Unfortunately, it is not technically easy to wrap the ovary.
HURD: Since we do not know the effect on future fertility of changing the ovarian surface, less would seem to be better in patients this young.
I have stopped doing difficult cases laparoscopically. For example, it is rare for me to operate laparoscopically on a patient with stage IV endometriosis, at least when it comes to infertility—I might consider laparoscopy for pain.
I think case selection plays a role as well, although there are few data to back that up. It is purely clinical opinion.
SANFILIPPO: We need a well-designed prospective study to explore the effects of laparotomy versus laparoscopy. Existing data are not clear. You would assume laparoscopy would be associated with less adhesion formation. But genetic or other factors may explain why patient A is more prone to adhesions than patient B.
Does anybody think carbon dioxide plays a role in adhesion formation?
HURD: In the laboratory, carbon dioxide increases cell growth.8 Without an increased carbon dioxide concentration in the atmosphere, cell cultures don’t grow well. This might suggest that the carbon dioxide used for laparoscopy could actually enhance adhesion growth. Fortunately, this does not appear to be the case clinically.
With myomectomy, the surgeon needs to plan ahead to maximize the number of myomas removed from a single incision.
DECHERNEY: What about second-look laparoscopies? Do any of you perform them after a patient has undergone lysis of adhesions?
SANFILIPPO: Only as part of a research protocol. It amazes me how rapidly adhesions can form and how dense they are 2 or more weeks after the initial laparoscopic surgery.
PAGIDAS: We tend to limit second-look laparoscopy to a research protocol, although it is sometimes valuable after laparoscopic or abdominal myomectomy, which has the highest incidence of adhesions. If the surgeon can perform a second look and lyse adhesions, he or she may potentially alter the reproductive outcome. However, with assisted reproductive techniques becoming integral to every infertility case, that approach has begun to go out of style.
SANFILIPPO: That’s a good point. With myomectomy, the surgeon needs to plan ahead to maximize the number of myomas removed from a single incision. If adhesions do occur, it is best if they occur toward the bladder rather than in the area of the tubes and ovaries.
HURD: For second-look laparoscopy, we must keep in mind the cost and the small but real risks of surgery. Until good controlled studies show a reasonable clinical advantage, this approach probably should remain a research protocol.
SANFILIPPO: The literature suggests it is helpful, but does not help fertility, so second-look laparoscopy is used mainly to evaluate adjunctive therapies. I don’t think anybody uses it as a primary therapy anymore.
Bowel obstruction still a risk, though rarely seen by Ob/Gyns
DECHERNEY: Although bowel obstruction is fairly common, Ob/Gyns do not often encounter it because it occurs relatively distant from the index surgery. Even though a patient may not experience bowel obstruction in the first year, an obstruction related to the index surgery is just as likely to develop 20 years later as 2 years later. These patients usually are treated by general surgeons. Still, we should beware of the potential for bowel obstruction and take steps to prevent it, if at all possible. Do you agree?
PAGIDAS: Yes. We tend to forget about bowel obstruction because we rarely follow patients past pregnancy or the first trimester if they are seeking infertility treatment.
HURD: The primary problem seems to be the abdominal wall incision. Fortunately, cesarean section seems to carry a decreased risk of abdominal wall adhesions, probably because the uterus serves as a splint over the incision.
The Pfannenstiel incision also appears to have some advantage. Both human and animal models suggest little advantage or disadvantage when peritoneal closure is compared to nonclosure.9,10
SANFILIPPO: I’m curious about how the panelists manage loose clips. If you are using an EndoGIA (US Surgical, Norwalk, Conn) or other stapling device and you have free-floating clips, do you make a concerted effort to find them? In some cases, they have been implicated in bowel adhesion and obstruction. I try to retrieve loose clips, whether open or closed.
HURD: The advantage of those devices is minimal tissue damage, and the clips are inert. In general, inert, nonreactive clips have not been implicated as much in adhesion formation. I retrieve them if I see them, but I don’t search them out.
PAGIDAS: I do the same. If the clips are visible, I remove them. But I would not repack the bowel or do anything more heroic than look in locations where they might be.
What drugs may inhibit inflammatory response?
DECHERNEY: What about use of pharmacologic agents to prevent adhesions? Is there reason to think research should focus on inhibiting the inflammatory response? How important is polymorphonuclear cell infiltration?
Cyclooxygenase (COX) 2 agents could be helpful for inhibition of platelet function, since they are low in side effects. Thus, high doses of these drugs might be effective. At one time, aspirin was proposed, but you’d have to give a human so much aspirin that her ears would ring.
PAGIDAS: Pharmacologic agents have a role, especially for dampening the inflammatory immune response. But you don’t want to dampen it completely because, as we observed, it is an important part of healing. The difficulty is finding a balance between allowing the tissue to heal and preventing adhesions.
HURD: We studied the ability of a water-soluble prostaglandin inhibitor to prevent postoperative adhesion formation. Like many other agents, we found only a partial response.11
DECHERNEY: With current options, the best you can aim for is a 50% reduction.
Adjunctive therapy likely to limit adhesion rate Hydroflotation
DECHERNEY: The original adjunctive therapy was 20 mg dexamethasone and 25 mg femergin in 200 cc of Ringer’s lactate, with an equivalent amount of dexamethasone and femergin every 4 hours for a total of 6 doses. I prescribed that regimen because I was trained to do so. I stopped after it became clear that hydroflotation from the fluid—not the medication itself—was responsible for the improvement.
I must admit I gave it up reluctantly; patients felt fabulous with those higher load doses of glucocorticoids after surgery.
Do any of you use crystalloids as adjunctive therapy?
SANFILIPPO: In the animal model, they are so rapidly absorbed that they aren’t effective. I was a strong advocate, but now I don’t use them at all.
HURD: A lot depends on the kind of case. For instance, at the end of an open myomectomy, the patient often is oozing, so you want to use a barrier that blood won’t affect.
For ovarian surgery, you might want to specifically target the ovaries with some kind of coverage. But when you are doing a broad lysis of adhesions, you have few choices to cover the pelvis. In those cases I use hydroflotation with Ringer’s lactate. Both human and animal studies have shown some benefit in preventing adhesions, and it appears to have little risk.12,13
It’s better than nothing, in my opinion.
DECHERNEY: Do you use dextran 70 or crystalloids?
HURD: I use Ringer’s lactate solution. I was trained in the dextran 70 era, and there were certain problems with that approach. Since studies have failed to show a consistent effect of dextran 70, I no longer use this solution.14,15
DECHERNEY: Another problem with crystalloids is that they leak, which is disconcerting to the patient.
HURD: They also can mask an injury to the bladder in difficult cases.
DECHERNEY: I agree that dextran 70 is only appropriate in certain cases, but it is a good hydroflotation agent. Every cubic centimeter of dextran 70 brings in 1.2 cc of transudate, so it hangs around for at least 4 days.
It is appropriate only for certain surface areas—mainly the cul-de-sac. It is harmful on raw surface areas on the lateral pelvic sidewall because it tends to push the ovary and tube to those areas. Unless you are doing a lot of work in the deep pelvis, I would avoid dextran 70.
A 45-year-old woman undergoes an abdominal hysterectomy. The cuff is closed and the ovaries are intact.
PAGIDAS: I would do nothing other than ensure adequate hemostasis, check that I have left no round surfaces and, probably, use hydroflotation. I see no advantage to barriers.
HURD: One of the main causes of adhesions is devascularized tissue, and the perfect devascularized tissue might be the vaginal cuff. Re-“peritonealizing” the cuff might be advantageous. Thus, I would use minimal sutures—probably a slowly absorbable, light polydioxanone suture to place the peritoneum over the cuff so there are no pedicles.
DECHERNEY: All the pedicles are exteriorized.
HURD: Yes, that could be. We don’t bring all of it down like we used to years ago, but we do cover the cuff.
PAGIDAS: I agree that closing the cuff and reperitonealizing may actually minimize formation of hematomas—clearly an advantage.
SANFILIPPO: I agree. I guess I’m old fashioned. If it looks good, then hopefully it will stimulate less adhesion formation, so peritonealization is important.
As far as the abdominal incision is concerned, I would not close that peritoneum. I’m convinced now that there is no advantage.
DECHERNEY: Reperitonealizing the cuff is controversial. Most gynecologic surgeons do not do it, the theory being that the peritoneum is being stretched, attenuating the vessels that go through it and thereby creating an ischemic barrier that contributes to adhesions. Personally, I like to do it because it looks better—and that is certainly an important aspect of a surgery. No evidence shows that it is bad or good, either way.
In addition, there have been allergic reactions, most of which seem to occur in patients with fluid overload; a lot of the dextran 70 is absorbed.
With infertility patients, even if you lyse dense adhesions, you do not render the ovarian surface normal.
SANFILIPPO: Dextran 70 is not recommended for patients with sugar beet allergy, either.
We completed a study in a rabbit model, in which the peritoneal cavity was lavaged with either chlorhexidine or iodine.16 At the time of second-look surgery, the rate of adhesion formation was decreased, especially with the iodine preparation. I would hope that this has potential in humans.
DECHERNEY: In your lavage procedures to prevent adhesions, do any of you use heparin?
HURD: No.
PAGIDAS: I don’t think any evidence suggests that local administration changes the outcome.
DECHERNEY: I agree. When heparin has been used, the doses have been so low that it was not terribly helpful. And when you consider that hemorrhage can be a problem, heparin is probably deleterious rather than helpful.
Barriers
DECHERNEY: What about barriers? The first to become available, Interceed (Gynecare, a division of Ethicon, Somerville, NJ), is oxidized cellulose, similar to Surgicell (Johnson & Johnson, New Brunswick, NJ). Since it gelates quickly, there is no fenestration, so the fibrin is unable to penetrate. However, if the patient has bleeding by capillary action, the raw surface just moves from one side of the Interceed barrier to the other.
What has been your experience? Do you use it?
PAGIDAS: I do not use Interceed, although prospective randomized trials and a meta-analysis confirmed its benefits in de novo formation and reformation.17-19 I don’t use it because it requires complete hemostasis. Also, with the surfaces we work on—notably, the ovary and tube—it is difficult to apply to just 1 surface area. From a clinical perspective, I appreciate the data, but it is hard to ensure a good application to optimize its effectiveness.
A 29-year-old woman is undergoing her third cesarean section, although adhesions cause difficulty getting through anteriorly.
DECHERNEY: In this case, will you use barriers or re-peritonealize the surface? Will you do a 1- or a 2-layered closure?
HURD: In these cases, I have not been doing anything, since there is no peritoneum to reperitonealize—just old scar tissue. I assume that the uterus will immediately readhere to the anterior peritoneum where it was before.
DECHERNEY: You would use a barrier?
HURD: No. I would not.
PAGIDAS: I would take the same approach, although I have not performed cesarean sections in about 4 years. I don’t think any intervention would change the outcome. And, as Dr. Hurd mentioned, that is pretty much old scar tissue anyway.
SANFILIPPO: I use Interceed, but I agree with you about its limitations. Meticulous hemostasis is a prerequisite.
HURD: With infertility patients, even if you lyse dense adhesions, you do not render the ovarian surface normal. If those patients have dense adhesions of the ovary or the sidewall, I generally leave them alone, and I try to avoid putting Interceed around the ovaries. No study has shown that using Interceed improves pregnancy.
In contrast, when a chronic pain patient’s ovaries are densely adherent to the cul-de-sac, which appears to be highly associated with dyspareunia, I lyse the adhesions, achieve meticulous hemostasis, and then use Interceed. It is hard to demonstrate in a study that this approach decreases the chance of pain. Even so, it certainly does decrease the chance of the ovaries being adherent.
DECHERNEY: One issue with Interceed is that we don’t know what happens to it once the abdomen is closed. It may migrate significantly.
Psychological issues may also be involved. For example, patients with multiple somatic complaints may be less likely to benefit from lysis of adhesions.
PAGIDAS: Right. Interestingly, a meta-analysis of all the randomized trials involving mechanical barriers found no correlation to pregnancy outcome or pelvic pain.18 If we were to consider new trials, the psychological aspect would be worth looking into.
Seprafilm
DECHERNEY: Let’s move on to Seprafilm (Genzyme, Cambridge, Mass). What is it and how useful is it?
HURD: Seprafilm is modified hyaluronic acid, which forms a brittle, thin plastic layer. It is somewhat difficult to work with but, once it is in place, seems to adhere well. The presence of blood does not appear to be a problem, since the Seprafilm forms an impermeable barrier—unless it breaks. I have found it especially useful in myomectomies, which produce postoperative oozing through the incisions no matter how hard you try to prevent it.
In addition, in open cases, surfaces can easily be covered with this material. Unfortunately, it can’t be used laparoscopically because it is so brittle.
DECHERNEY: In my opinion, that is its major drawback.
PAGIDAS: In cardiac surgery, Seprafilm appears to work quite effectively.
SANFILIPPO: The manufacturer initially focused on surgeons in the context of sigmoid colon surgery, and it seems to work well in that setting.
Intergel
DECHERNEY: That brings us to the current state of the art: gels. I’m sure you all are familiar with Intergel (Lifecore Biomedical, Chaska, Minn), which is a ferrous derivative of hyaluronic acid that works by coating the raw surface areas. It also has the theoretical advantage of ease of use. Have any of you used Intergel?
HURD: As you know it was only recently approved by the US Food and Drug Administration, but not for laparoscopic use. It may work best on abraded bowel, which is avoided by laparoscopic surgery.
As you are probably also aware, the manufacturer recently took it off the market because of unusual side effects, namely a chemical peritonitis. Although peritonitis was cited as being rare, we encountered it in probably half the patients we operated on.
PAGIDAS: When we used it on hospitalized patients, the peritonitis wasn’t that obvious, since there was an expectation of significant pain. However, when we used Intergel on short-stay patients, we had to readmit them and do a full workup because we were concerned about bowel perforations. I’m surprised the manufacturer didn’t take it off the market sooner.
DECHERNEY: It seems strange, since Intergel has been used in Europe for a while now. I’ve used it in only 1 case and didn’t have adverse effects. It seemed to work well.
SANFILIPPO: It had all the right ingredients for success. It is unfortunate that these side effects have prohibited its use.
There is no question that adhesion prevention is one of the unmet challenges in all surgeries, especially reproductive surgery.
Gels and the cost factor
DECHERNEY: Other gels are in the pipeline. I’m reminded of plasminogen activator, which is a powerful antiadhesive agent that lyses fibrin effectively. Unfortunately, it is prohibitively expensive.
The next phase likely will involve the so-called polymers. If you spray them on your hand, they are activated by light or another chemical and become a cellophane-like substance. The problem is viscosity. If sprayed on the sidewall, for instance, they run halfway down before they are activated, so the entire surface does not get covered.
PAGIDAS: One concern with polymers is that they could actually bring surfaces together when they polymerize. We still have a lot to learn.
DECHERNEY: Let’s say a new gel comes on the market that takes reformation adhesions from 90% to 10%, as opposed to 40% recurrence. Would you use it in all 4 of the cases we discuss here?
HURD: If it was that effective and had no adverse effects, it would be wonderful.
The cesarean-delivery case is different, as healing in a pregnant patient is 1 concern; the size of the uterus also has an effect. If the patient is breastfeeding, you would want to make sure the gel didn’t interfere.
PAGIDAS: We desperately need a product that can minimize adhesions regardless of the route of access or type of procedure. Even though we lack data on outcomes, I predict wide use of such a product, assuming it is nontoxic and effective.
DECHERNEY: What if it costs $1,000 a case?
SANFILIPPO: If it prevents 1 bowel obstruction, it still would be cost-effective.
DECHERNEY: The incidence of bowel obstruction for total abdominal hysterectomy is 2%, and 5% for radical hysterectomy.
HURD: We must be careful of the cost-benefit ratio. Bowel obstruction after gynecologic surgery is uncommon.
Is the gel worth $100? $1,000? $3,000? It’s difficult to say, but the more expensive it is, the less likely it will find widespread use.
PAGIDAS: I agree. We should remember that we still need to maintain microsurgical techniques and appropriate tissue handling, as well as avoid ischemia and infection.
Looking for the magic bullet
DECHERNEY: What is the future of adjunctive therapy?
SANFILIPPO: I would focus on noxythiolin; it has potential. Calcium channel blockers for adhesion prevention have also been studied.20 In 1 investigation involving a rat model, the calcium channel blocker verapamil as well as several other agents—including vitamin E, carboxymethylcellulose, cyclosporin, aprotinin, and tenoxicam—were compared with respect to tissue effects. A beneficial effect was noted with all agents except cyclosporin and carboxymethylcellulose.
Whoever succeeds in manufacturing an effective preventive will be a winner.
HURD: There is no question that adhesion prevention is one of the unmet challenges in all surgeries, especially reproductive surgery. The most effective agent would be applied intraabdominally, since any systemic agent that stops adhesion formation would probably decrease wound healing as well.
I hope the most effective agents can be used in both laparoscopy and laparotomy, and that they will decrease the adhesion-formation rate by more than 50%. We need to find the magic bullet that can cover the entire pelvis—if not the entire abdomen.
Dr. DeCherney reports small holdings with Lifecore Biomedical and Johnson & Johnson. Drs. Hurd and Pagidas report no financial relationship with any companies whose products are mentioned in this article. Dr. Sanfilippo serves on the speaker’s bureau for Berlex, Ortho Pharmaceuticals, and Wyeth, and receives grant support from Eli Lilly and Wyeth.


-

-

- Approximately 40% of people who undergo primary surgery develop adhesions and reformation occurs in 80% to 90% of cases.
- Microsurgical techniques such as gentle handling of tissues, careful hemostasis, and avoidance of heat may help reduce the incidence.
- Laparoscopy appears to be less likely to produce adhesions than laparotomy.
- Ob/Gyns should be aware of the potential for adhesion-related bowel obstruction and take steps to prevent it.
Are adhesions a pathologic response to injury or a normal aspect of healing? Can they be avoided, or are preventive efforts part of the problem? How useful are the different barriers in gynecologic surgery? What is the ideal adjuvant?
OBG Management convened a panel of experts to explore these and other questions.
Common problem, high recurrence rate
DECHERNEY: Adhesion formation is serious because it is associated with clinical entities such as infertility, pelvic pain, and bowel obstruction. We all agree that approximately 40% of people who undergo primary surgery develop adhesions and that 80% to 90% of patients who undergo lysis develop recurrent adhesions.
SANFILIPPO: One study several years ago explored adhesion formation.1 Unfortunately, no matter how meticulous the surgeon is, adhesions will form, even with microsurgical techniques and carefully ensured hemostasis.
HURD: The number of patients with significant adhesion formation after some gynecologic procedures has been reported to be greater than 90%.2
DECHERNEY: That higher incidence usually occurs after general surgery—and there’s a reason it is so high: General surgeons don’t use adjunctive therapy. They are critical of it. It is to our credit as gynecologic surgeons that we adopted adjunctive therapies about 15 years ago with the introduction of dextran 70 (Hyskon; Medisan Pharmaceuticals, Parsippany, NJ).
PAGIDAS: If anything, the pelvis seems to have even more of a predilection for adhesion formation than the abdomen, probably because of the close proximity of structures.
How and why adhesions form
DECHERNEY: What is the pathophysiology of adhesion formation? Let’s say you have 2 raw surface areas. What happens?
The process
PAGIDAS: The increase in leukotrienes and prostaglandins and the decrease in plasminogen activity (which actually initiates the inflammation) appear to be significant.
HURD: Vessel permeability also increases, and inflammatory cells leak through the vessels and set up a matrix for adhesion formation.
DECHERNEY: So we have 2 raw surface areas with fibrin leaking out and forming bridges between them.
PAGIDAS: The key is that it takes 2 surfaces to form these bridges. As I mentioned, the greater proximity of pelvic structures—particularly around the tube and ovary—probably contributes to adhesion formation.
DECHERNEY: Macrophage activity also is important. The macrophage “migrates” along these fibrin bridges and lays down collagen over a period of time. Then the collagen becomes organized and, eventually, vascular.
Window of opportunity
SANFILIPPO: Adhesion formation probably occurs and is pretty well established within 5 to 7 days of the precipitating event—usually surgery. Once that process is under way, attempts to halt it yield diminishing returns. Unfortunately, we don’t know how to interfere with it in a positive way.
HURD: Under normal conditions, there seems to be a balance between fibrin deposition and fibrinolysis. In some tissues, however, these functions become imbalanced. This disparity may contribute more to adhesions than the actual laying down of fibrin—especially in tissue that is hypoxic.
DECHERNEY: Would you say that adhesion formation represents normal or abnormal healing?
HURD: It is one of the body’s normal protective mechanisms and an important part of healing. Without it, any abdominal injury would likely result in death.
SANFILIPPO: I don’t think it differs that much from processes that occur externally. For example, if you get cut deeply enough, you develop a scar. Is that scar part of the normal healing process? It is.
PAGIDAS: Right. It is a normal process of tissue remodeling. The question is: What allows it to go astray?
What surgical techniques help prevent adhesions?
DECHERNEY: Let’s review the aspects of surgical technique that are important for adhesion prevention.
PAGIDAS: I emphasize the value of microsurgical techniques, which help to minimize severe tissue handling. It also is important to keep surfaces moistened so they don’t desiccate.
SANFILIPPO: I agree with Dr. Pagidas about microsurgical techniques such as gentle tissue handling, careful hemostasis, and keeping tissues moist. If we follow these principles, we create an environment that minimizes the potential for adhesion formation.
HURD: The findings of many well-controlled animal studies have been surprising. For example, it is difficult to demonstrate that drying of tissue increases adhesions.3 Probably the greatest contributor to adhesions in these models was abrasion.4 One way that laparoscopic surgery decreases adhesions is by avoiding abrasion of the bowel mucosa, which occurs specifically with packing.
A 38-year-old mother of 2 undergoes myomectomy for menorrhagia.
SANFILIPPO: The initial question is: Can this case be managed laparoscopically? I do myomectomies laparoscopically whenever possible, although I do close the uterus with a minilaparotomy incision. The reason is my strong concern about reapproximating the myometrium, since wound dehiscence sometimes occurs at the site of myoma removal.
In this case, depending on the size of the myomas, I would do as much as possible laparoscopically and then reapproximate the myometrium. I would plan my incisions carefully, to maximize the number of myomas that can be removed. I would end with meticulous hemostasis and, assuming it is successful, use a barrier over the incision—in this case, Interceed.
HURD: Does the patient desire future childbearing? If so, I would avoid the laparoscopic approach because of the possibly increased risk of uterine rupture during pregnancy. If she isn’t planning pregnancy, there are more options.
The next question is: How many myomas are there, and where are they located? If they are intrauterine, a hysteroscopic approach would avoid extrauterine adhesions. If they are multiple and large, I am pretty much limited to laparotomy. If there is 1 or only a few myomas, a laparoscopic approach would be best.
I have not used Interceed. In laparoscopic cases, I worry that it would create more problems because, as you allow the carbon dioxide to decrease at the end of a case, oozing begins. Instead of a barrier, I would use limited hydroflotation.
SANFILIPPO: That’s a good point. At the end of the myomectomy, with the laparoscope in place, I decrease the insufflation, eliminating the tamponade effect. Then, assuming good hemostasis, I apply Interceed.
HURD: With open cases, I use Seprafilm, which takes practice because, as it gets wet, it sticks to anything, including gloves and instruments. But if you can put it down dry on the uterus, it sticks and stays in place. If oozing occurs, it seems to block or stop it.
PAGIDAS: I want to reiterate the importance of determining whether childbearing is an issue. In this case, the biggest concern is the risk of adhesions developing on our incision, so I would use a barrier. My preference would be Seprafilm or GoreTex. If we can limit adhesions at the incision site, then hopefully we can minimize bowel and tuboovarian adhesions, too.
In open cases, one thing we can do to minimize the risk of adhesions is to pack gently when needed. Also, we should avoid using packing to reposition the bowel.
Another factor frequently overlooked is the application of heat, which appears to be a very effective way to create adhesions. This probably isn’t an issue for laparoscopic cases, but when you use irrigation fluid in an open case, watch the temperature. If it feels hot to you, you need to worry about potential injury to the bowel surfaces.
PAGIDAS: That is critical. In abdominal cases you want to make sure irrigation fluid is warm, but not too warm, because heat increases the vascular permeability of vessels and leads to more macrophages, more prostaglandins, and more leukotrienes.
HURD: Another important element is the type of suture material used.
DECHERNEY: Overall, we need to minimize the use of sutures. For example, when I am operating laparoscopically on an ovarian cyst, I try to apply bipolar energy to the edges so that they will coapt without a stitch.
HURD: When it first became clear that suturing ovaries increased adhesion formation, we conducted a controlled trial of different kinds of sutures in animals. Not surprisingly, we found that the less reactive the suture, the fewer adhesions.5 Sutures that are absorbed more slowly, such as polydioxanone, seem to be less reactive.
Obviously, inert sutures like nylon are the least reactive, but they are permanent. It is assumed that animal-protein sutures such as chromic and plain gut are the most reactive, although I am not sure there are sufficient data to support that conclusion.
Multiple clinical studies have shown laparoscopy to be associated with a lower adhesion rate, although it isn’t clear why. It may be related to decreased suturing.
DECHERNEY: Bulk is important, too—that is, the number of throws in the suture. When Vicryl (polyglactin 910) became available, we conducted a study in mice using proportionately small Vicryl plaques to determine whether this would be good a barrier (A. DeCherney, MD, unpublished data). It caused a tremendous amount of adhesion because so much foreign matter was applied.
We also did a study using human-size titanium clips in rats (A. DeCherney, MD, unpublished data). Not surprisingly, there was a lot of adhesion formation.
FIGURE 1 Pelvic adhesions: How they develop, problems they cause
Adhesions occur when 2 or more raw surfaces are exposed to leaking fibrin, which forms a bridge between the surfaces. Macrophages “migrate” along these bridges, depositing collagen.
The pelvis has a greater predilection for adhesions than the abdomen because of the close proximity of structures.
Although adhesions represent one of the body’s protective mechanisms, they may also cause pain or interfere with fertility, bowel function, or other processes.
Laparoscopy versus laparotomy: More adhesions in open cases?
DECHERNEY: Based on all the techniques we have learned from microsurgery—with the exception of magnification—it appears that laparoscopic procedures are less likely to cause adhesions than laparotomy. Do you agree?
PAGIDAS: I think so. As Dr. Hurd noted, a main reason is the diminished tissue handling, because there is no packing.
HURD: Multiple clinical studies have shown laparoscopy to be associated with a lower adhesion rate, although it isn’t clear why.6,7 It may be related to decreased suturing.
DECHERNEY: Less bleeding occurs because surgeons are less aggressive laparoscopically than in laparotomy.
A 15-year-old undergoes removal of a dermoid cyst, which was shelled out laparoscopically.
PAGIDAS: This case is easier because the cyst has been successfully shelled out. It is not the spill of a cyst’s contents at surgery that creates adhesions, but a chronic leak, which can occur if you do not remove the cyst in its entirety.
Once the cyst has been excised completely, I would ensure hemostasis with bipolar cautery and reapproximate the edges. I would not suture. There seems to be no clear advantage to suturing. I would use hydroflotation. Although Ringer’s lactate solution has not been shown to be effective, it is safe and has no toxicity.
DECHERNEY: Would you remove the cyst via laparotomy?
PAGIDAS: I would do it laparoscopically, using the endobag to minimize spillage, even though we know that a spill doesn’t necessarily change the outcome. If spillage does occur, I would perform copious irrigation to ensure that nothing is left behind.
HURD: My priority would be minimizing the use of power on the ovary. Studies of ovarian drilling have demonstrated that burning an ovary stimulates adhesion formation.21,22 If the dermoid cyst spills, as happens occasionally, I perform copious rinsing until no more oil is visible on the surface of the peritoneal fluid.
I also would minimize the amount of ovarian capsule that is removed. Good studies of endometriomas have shown that the more capsulate that is removed, the more adhesions. Even if the capsule looks redundant and floppy, the concern should be to achieve hemostasis with bipolar cautery and then leave it alone.
DECHERNEY: Would you use crystalloids in this case?
HURD: Yes.
SANFILIPPO: If spillage occurs, I would ensure that the patient is taken out of the Trendelenburg position. I want to emphasize the importance of thorough irrigation to eliminate any material that could produce chemical peritonitis.
DECHERNEY: Over the years, I have seen a fair number of cases of Fitz-Hugh and Curtis syndrome. You rigorously lavage a ruptured dermoid cyst, which sometimes presents with low-grade fever, but always with pain.
I’m surprised that none of you would use Interceed, since wrapping the ovary is the only thing for which it has been clearly shown to be effective. Since the cortex is relatively avascular, you don’t get a lot of bleeding. Unfortunately, it is not technically easy to wrap the ovary.
HURD: Since we do not know the effect on future fertility of changing the ovarian surface, less would seem to be better in patients this young.
I have stopped doing difficult cases laparoscopically. For example, it is rare for me to operate laparoscopically on a patient with stage IV endometriosis, at least when it comes to infertility—I might consider laparoscopy for pain.
I think case selection plays a role as well, although there are few data to back that up. It is purely clinical opinion.
SANFILIPPO: We need a well-designed prospective study to explore the effects of laparotomy versus laparoscopy. Existing data are not clear. You would assume laparoscopy would be associated with less adhesion formation. But genetic or other factors may explain why patient A is more prone to adhesions than patient B.
Does anybody think carbon dioxide plays a role in adhesion formation?
HURD: In the laboratory, carbon dioxide increases cell growth.8 Without an increased carbon dioxide concentration in the atmosphere, cell cultures don’t grow well. This might suggest that the carbon dioxide used for laparoscopy could actually enhance adhesion growth. Fortunately, this does not appear to be the case clinically.
With myomectomy, the surgeon needs to plan ahead to maximize the number of myomas removed from a single incision.
DECHERNEY: What about second-look laparoscopies? Do any of you perform them after a patient has undergone lysis of adhesions?
SANFILIPPO: Only as part of a research protocol. It amazes me how rapidly adhesions can form and how dense they are 2 or more weeks after the initial laparoscopic surgery.
PAGIDAS: We tend to limit second-look laparoscopy to a research protocol, although it is sometimes valuable after laparoscopic or abdominal myomectomy, which has the highest incidence of adhesions. If the surgeon can perform a second look and lyse adhesions, he or she may potentially alter the reproductive outcome. However, with assisted reproductive techniques becoming integral to every infertility case, that approach has begun to go out of style.
SANFILIPPO: That’s a good point. With myomectomy, the surgeon needs to plan ahead to maximize the number of myomas removed from a single incision. If adhesions do occur, it is best if they occur toward the bladder rather than in the area of the tubes and ovaries.
HURD: For second-look laparoscopy, we must keep in mind the cost and the small but real risks of surgery. Until good controlled studies show a reasonable clinical advantage, this approach probably should remain a research protocol.
SANFILIPPO: The literature suggests it is helpful, but does not help fertility, so second-look laparoscopy is used mainly to evaluate adjunctive therapies. I don’t think anybody uses it as a primary therapy anymore.
Bowel obstruction still a risk, though rarely seen by Ob/Gyns
DECHERNEY: Although bowel obstruction is fairly common, Ob/Gyns do not often encounter it because it occurs relatively distant from the index surgery. Even though a patient may not experience bowel obstruction in the first year, an obstruction related to the index surgery is just as likely to develop 20 years later as 2 years later. These patients usually are treated by general surgeons. Still, we should beware of the potential for bowel obstruction and take steps to prevent it, if at all possible. Do you agree?
PAGIDAS: Yes. We tend to forget about bowel obstruction because we rarely follow patients past pregnancy or the first trimester if they are seeking infertility treatment.
HURD: The primary problem seems to be the abdominal wall incision. Fortunately, cesarean section seems to carry a decreased risk of abdominal wall adhesions, probably because the uterus serves as a splint over the incision.
The Pfannenstiel incision also appears to have some advantage. Both human and animal models suggest little advantage or disadvantage when peritoneal closure is compared to nonclosure.9,10
SANFILIPPO: I’m curious about how the panelists manage loose clips. If you are using an EndoGIA (US Surgical, Norwalk, Conn) or other stapling device and you have free-floating clips, do you make a concerted effort to find them? In some cases, they have been implicated in bowel adhesion and obstruction. I try to retrieve loose clips, whether open or closed.
HURD: The advantage of those devices is minimal tissue damage, and the clips are inert. In general, inert, nonreactive clips have not been implicated as much in adhesion formation. I retrieve them if I see them, but I don’t search them out.
PAGIDAS: I do the same. If the clips are visible, I remove them. But I would not repack the bowel or do anything more heroic than look in locations where they might be.
What drugs may inhibit inflammatory response?
DECHERNEY: What about use of pharmacologic agents to prevent adhesions? Is there reason to think research should focus on inhibiting the inflammatory response? How important is polymorphonuclear cell infiltration?
Cyclooxygenase (COX) 2 agents could be helpful for inhibition of platelet function, since they are low in side effects. Thus, high doses of these drugs might be effective. At one time, aspirin was proposed, but you’d have to give a human so much aspirin that her ears would ring.
PAGIDAS: Pharmacologic agents have a role, especially for dampening the inflammatory immune response. But you don’t want to dampen it completely because, as we observed, it is an important part of healing. The difficulty is finding a balance between allowing the tissue to heal and preventing adhesions.
HURD: We studied the ability of a water-soluble prostaglandin inhibitor to prevent postoperative adhesion formation. Like many other agents, we found only a partial response.11
DECHERNEY: With current options, the best you can aim for is a 50% reduction.
Adjunctive therapy likely to limit adhesion rate Hydroflotation
DECHERNEY: The original adjunctive therapy was 20 mg dexamethasone and 25 mg femergin in 200 cc of Ringer’s lactate, with an equivalent amount of dexamethasone and femergin every 4 hours for a total of 6 doses. I prescribed that regimen because I was trained to do so. I stopped after it became clear that hydroflotation from the fluid—not the medication itself—was responsible for the improvement.
I must admit I gave it up reluctantly; patients felt fabulous with those higher load doses of glucocorticoids after surgery.
Do any of you use crystalloids as adjunctive therapy?
SANFILIPPO: In the animal model, they are so rapidly absorbed that they aren’t effective. I was a strong advocate, but now I don’t use them at all.
HURD: A lot depends on the kind of case. For instance, at the end of an open myomectomy, the patient often is oozing, so you want to use a barrier that blood won’t affect.
For ovarian surgery, you might want to specifically target the ovaries with some kind of coverage. But when you are doing a broad lysis of adhesions, you have few choices to cover the pelvis. In those cases I use hydroflotation with Ringer’s lactate. Both human and animal studies have shown some benefit in preventing adhesions, and it appears to have little risk.12,13
It’s better than nothing, in my opinion.
DECHERNEY: Do you use dextran 70 or crystalloids?
HURD: I use Ringer’s lactate solution. I was trained in the dextran 70 era, and there were certain problems with that approach. Since studies have failed to show a consistent effect of dextran 70, I no longer use this solution.14,15
DECHERNEY: Another problem with crystalloids is that they leak, which is disconcerting to the patient.
HURD: They also can mask an injury to the bladder in difficult cases.
DECHERNEY: I agree that dextran 70 is only appropriate in certain cases, but it is a good hydroflotation agent. Every cubic centimeter of dextran 70 brings in 1.2 cc of transudate, so it hangs around for at least 4 days.
It is appropriate only for certain surface areas—mainly the cul-de-sac. It is harmful on raw surface areas on the lateral pelvic sidewall because it tends to push the ovary and tube to those areas. Unless you are doing a lot of work in the deep pelvis, I would avoid dextran 70.
A 45-year-old woman undergoes an abdominal hysterectomy. The cuff is closed and the ovaries are intact.
PAGIDAS: I would do nothing other than ensure adequate hemostasis, check that I have left no round surfaces and, probably, use hydroflotation. I see no advantage to barriers.
HURD: One of the main causes of adhesions is devascularized tissue, and the perfect devascularized tissue might be the vaginal cuff. Re-“peritonealizing” the cuff might be advantageous. Thus, I would use minimal sutures—probably a slowly absorbable, light polydioxanone suture to place the peritoneum over the cuff so there are no pedicles.
DECHERNEY: All the pedicles are exteriorized.
HURD: Yes, that could be. We don’t bring all of it down like we used to years ago, but we do cover the cuff.
PAGIDAS: I agree that closing the cuff and reperitonealizing may actually minimize formation of hematomas—clearly an advantage.
SANFILIPPO: I agree. I guess I’m old fashioned. If it looks good, then hopefully it will stimulate less adhesion formation, so peritonealization is important.
As far as the abdominal incision is concerned, I would not close that peritoneum. I’m convinced now that there is no advantage.
DECHERNEY: Reperitonealizing the cuff is controversial. Most gynecologic surgeons do not do it, the theory being that the peritoneum is being stretched, attenuating the vessels that go through it and thereby creating an ischemic barrier that contributes to adhesions. Personally, I like to do it because it looks better—and that is certainly an important aspect of a surgery. No evidence shows that it is bad or good, either way.
In addition, there have been allergic reactions, most of which seem to occur in patients with fluid overload; a lot of the dextran 70 is absorbed.
With infertility patients, even if you lyse dense adhesions, you do not render the ovarian surface normal.
SANFILIPPO: Dextran 70 is not recommended for patients with sugar beet allergy, either.
We completed a study in a rabbit model, in which the peritoneal cavity was lavaged with either chlorhexidine or iodine.16 At the time of second-look surgery, the rate of adhesion formation was decreased, especially with the iodine preparation. I would hope that this has potential in humans.
DECHERNEY: In your lavage procedures to prevent adhesions, do any of you use heparin?
HURD: No.
PAGIDAS: I don’t think any evidence suggests that local administration changes the outcome.
DECHERNEY: I agree. When heparin has been used, the doses have been so low that it was not terribly helpful. And when you consider that hemorrhage can be a problem, heparin is probably deleterious rather than helpful.
Barriers
DECHERNEY: What about barriers? The first to become available, Interceed (Gynecare, a division of Ethicon, Somerville, NJ), is oxidized cellulose, similar to Surgicell (Johnson & Johnson, New Brunswick, NJ). Since it gelates quickly, there is no fenestration, so the fibrin is unable to penetrate. However, if the patient has bleeding by capillary action, the raw surface just moves from one side of the Interceed barrier to the other.
What has been your experience? Do you use it?
PAGIDAS: I do not use Interceed, although prospective randomized trials and a meta-analysis confirmed its benefits in de novo formation and reformation.17-19 I don’t use it because it requires complete hemostasis. Also, with the surfaces we work on—notably, the ovary and tube—it is difficult to apply to just 1 surface area. From a clinical perspective, I appreciate the data, but it is hard to ensure a good application to optimize its effectiveness.
A 29-year-old woman is undergoing her third cesarean section, although adhesions cause difficulty getting through anteriorly.
DECHERNEY: In this case, will you use barriers or re-peritonealize the surface? Will you do a 1- or a 2-layered closure?
HURD: In these cases, I have not been doing anything, since there is no peritoneum to reperitonealize—just old scar tissue. I assume that the uterus will immediately readhere to the anterior peritoneum where it was before.
DECHERNEY: You would use a barrier?
HURD: No. I would not.
PAGIDAS: I would take the same approach, although I have not performed cesarean sections in about 4 years. I don’t think any intervention would change the outcome. And, as Dr. Hurd mentioned, that is pretty much old scar tissue anyway.
SANFILIPPO: I use Interceed, but I agree with you about its limitations. Meticulous hemostasis is a prerequisite.
HURD: With infertility patients, even if you lyse dense adhesions, you do not render the ovarian surface normal. If those patients have dense adhesions of the ovary or the sidewall, I generally leave them alone, and I try to avoid putting Interceed around the ovaries. No study has shown that using Interceed improves pregnancy.
In contrast, when a chronic pain patient’s ovaries are densely adherent to the cul-de-sac, which appears to be highly associated with dyspareunia, I lyse the adhesions, achieve meticulous hemostasis, and then use Interceed. It is hard to demonstrate in a study that this approach decreases the chance of pain. Even so, it certainly does decrease the chance of the ovaries being adherent.
DECHERNEY: One issue with Interceed is that we don’t know what happens to it once the abdomen is closed. It may migrate significantly.
Psychological issues may also be involved. For example, patients with multiple somatic complaints may be less likely to benefit from lysis of adhesions.
PAGIDAS: Right. Interestingly, a meta-analysis of all the randomized trials involving mechanical barriers found no correlation to pregnancy outcome or pelvic pain.18 If we were to consider new trials, the psychological aspect would be worth looking into.
Seprafilm
DECHERNEY: Let’s move on to Seprafilm (Genzyme, Cambridge, Mass). What is it and how useful is it?
HURD: Seprafilm is modified hyaluronic acid, which forms a brittle, thin plastic layer. It is somewhat difficult to work with but, once it is in place, seems to adhere well. The presence of blood does not appear to be a problem, since the Seprafilm forms an impermeable barrier—unless it breaks. I have found it especially useful in myomectomies, which produce postoperative oozing through the incisions no matter how hard you try to prevent it.
In addition, in open cases, surfaces can easily be covered with this material. Unfortunately, it can’t be used laparoscopically because it is so brittle.
DECHERNEY: In my opinion, that is its major drawback.
PAGIDAS: In cardiac surgery, Seprafilm appears to work quite effectively.
SANFILIPPO: The manufacturer initially focused on surgeons in the context of sigmoid colon surgery, and it seems to work well in that setting.
Intergel
DECHERNEY: That brings us to the current state of the art: gels. I’m sure you all are familiar with Intergel (Lifecore Biomedical, Chaska, Minn), which is a ferrous derivative of hyaluronic acid that works by coating the raw surface areas. It also has the theoretical advantage of ease of use. Have any of you used Intergel?
HURD: As you know it was only recently approved by the US Food and Drug Administration, but not for laparoscopic use. It may work best on abraded bowel, which is avoided by laparoscopic surgery.
As you are probably also aware, the manufacturer recently took it off the market because of unusual side effects, namely a chemical peritonitis. Although peritonitis was cited as being rare, we encountered it in probably half the patients we operated on.
PAGIDAS: When we used it on hospitalized patients, the peritonitis wasn’t that obvious, since there was an expectation of significant pain. However, when we used Intergel on short-stay patients, we had to readmit them and do a full workup because we were concerned about bowel perforations. I’m surprised the manufacturer didn’t take it off the market sooner.
DECHERNEY: It seems strange, since Intergel has been used in Europe for a while now. I’ve used it in only 1 case and didn’t have adverse effects. It seemed to work well.
SANFILIPPO: It had all the right ingredients for success. It is unfortunate that these side effects have prohibited its use.
There is no question that adhesion prevention is one of the unmet challenges in all surgeries, especially reproductive surgery.
Gels and the cost factor
DECHERNEY: Other gels are in the pipeline. I’m reminded of plasminogen activator, which is a powerful antiadhesive agent that lyses fibrin effectively. Unfortunately, it is prohibitively expensive.
The next phase likely will involve the so-called polymers. If you spray them on your hand, they are activated by light or another chemical and become a cellophane-like substance. The problem is viscosity. If sprayed on the sidewall, for instance, they run halfway down before they are activated, so the entire surface does not get covered.
PAGIDAS: One concern with polymers is that they could actually bring surfaces together when they polymerize. We still have a lot to learn.
DECHERNEY: Let’s say a new gel comes on the market that takes reformation adhesions from 90% to 10%, as opposed to 40% recurrence. Would you use it in all 4 of the cases we discuss here?
HURD: If it was that effective and had no adverse effects, it would be wonderful.
The cesarean-delivery case is different, as healing in a pregnant patient is 1 concern; the size of the uterus also has an effect. If the patient is breastfeeding, you would want to make sure the gel didn’t interfere.
PAGIDAS: We desperately need a product that can minimize adhesions regardless of the route of access or type of procedure. Even though we lack data on outcomes, I predict wide use of such a product, assuming it is nontoxic and effective.
DECHERNEY: What if it costs $1,000 a case?
SANFILIPPO: If it prevents 1 bowel obstruction, it still would be cost-effective.
DECHERNEY: The incidence of bowel obstruction for total abdominal hysterectomy is 2%, and 5% for radical hysterectomy.
HURD: We must be careful of the cost-benefit ratio. Bowel obstruction after gynecologic surgery is uncommon.
Is the gel worth $100? $1,000? $3,000? It’s difficult to say, but the more expensive it is, the less likely it will find widespread use.
PAGIDAS: I agree. We should remember that we still need to maintain microsurgical techniques and appropriate tissue handling, as well as avoid ischemia and infection.
Looking for the magic bullet
DECHERNEY: What is the future of adjunctive therapy?
SANFILIPPO: I would focus on noxythiolin; it has potential. Calcium channel blockers for adhesion prevention have also been studied.20 In 1 investigation involving a rat model, the calcium channel blocker verapamil as well as several other agents—including vitamin E, carboxymethylcellulose, cyclosporin, aprotinin, and tenoxicam—were compared with respect to tissue effects. A beneficial effect was noted with all agents except cyclosporin and carboxymethylcellulose.
Whoever succeeds in manufacturing an effective preventive will be a winner.
HURD: There is no question that adhesion prevention is one of the unmet challenges in all surgeries, especially reproductive surgery. The most effective agent would be applied intraabdominally, since any systemic agent that stops adhesion formation would probably decrease wound healing as well.
I hope the most effective agents can be used in both laparoscopy and laparotomy, and that they will decrease the adhesion-formation rate by more than 50%. We need to find the magic bullet that can cover the entire pelvis—if not the entire abdomen.
Dr. DeCherney reports small holdings with Lifecore Biomedical and Johnson & Johnson. Drs. Hurd and Pagidas report no financial relationship with any companies whose products are mentioned in this article. Dr. Sanfilippo serves on the speaker’s bureau for Berlex, Ortho Pharmaceuticals, and Wyeth, and receives grant support from Eli Lilly and Wyeth.
1. Operative Laparoscopy Study Group Postoperative adhesion development after operative laparoscopy: evaluation at early second look procedures. Fertil Steril. 1991;55:700-704.
2. Tulandi T, Murray C, Guralnick M. Adhesion formation and reproductive outcome after myomectomy and second-look laparoscopy. Obstet Gynecol. 1993;82:213-215.
3. Larsson B, Perbeck L. The possible advantage of keeping the uterine and intestinal serosa irrigated with saline to prevent intraabdominal adhesions in operations for infertility. An experimental study in rats. Acta Chir Scand Suppl. 1985;530:15-18.
4. Zamir G, Bloom AI, Reissman P. Prevention of intestinal adhesions after laparotomy in a rat model—a randomized prospective study. Res Exp Med (Berl). 1998;197:349-353.
5. Hurd WW, Himebaugh KS, Cofer KF, Gauvin JM, Elkins TE. The etiology of closure-related adhesion formation after wedge resection of the rabbit ovary. J Reprod Med. 1993;38:465-468.
6. Chen MD, Teigen GA, Reynolds HT, Johnson PR, Fowler JM. Laparoscopy versus laparotomy: an evaluation of adhesion formation after pelvic and paraaortic lymphadenectomy in a porcine model. Am J Obstet Gynecol. 1998;178:499-503.
7. Polymeneas G, Theodosopoulos T, Stamatiadis A, Kourias E. A comparative study of postoperative adhesion formation after laparoscopic vs. open cholecystectomy. Surg Endosc. 2001;15:41-43.
8. Smidt VJ, Singh DM, Hurteau JA, Hurd WW. Effect of carbon dioxide on human ovarian carcinoma cell growth. Am J Obstet Gynecol. 2001;185:1314-1317.
9. Tulandi T, Hum HS, Gelfand MM. Closure of laparotomy incisions with or without peritoneal suturing and second look laparoscopy. Am J Obstet Gynecol. 1988;158:536-537.
10. Kapur ML, Daneswar A, Chopra P. Evaluation of peritoneal closure at laparotomy. Am J Surg. 1979;137:650-652.
11. Cofer KF, Himebaugh KS, Gauvin JM, Hurd WW. Inhibition of adhesion reformation in the rabbit model by meclofenamate: an inhibitor of both prostaglandin and leukotriene production. Fertil Steril. 1994;62:1262-1265.
12. Elkelani OA, Molinas CR, Mynbaev O, Koninckx PR. Prevention of adhesions with crystalloids during laparoscopic surgery in mice. J Am Assoc Gynecol Laparosc. 2002;9:447-452.
13. Chan KL, Marino T, Qu WM, Tulandi T. Effects of intraperitoneal Ringer’s lactate instillation and infusion on postsurgical adhesion formation. J Gynecol Surg. 1995;11:241-243.
14. Watson A, Vandekerckhove P, Lilford R. Pharmacological adjuvants during infertility surgery: a systematic review of evidence derived from randomized controlled trial. Hum Fertil (Camb). 1999;2:149-157.
15. Larson B. Dextran—later clinical studies. clinical and experimental evaluation of different adjuvant therapies. Prog Clin Biol Res. 1990;358:165-175.
16. Roberts L, Sanfilippo JS, Ehrlich G, Raab S. Adhesion formation, peritoneal effects and the presence of bacterial biofilms after laparoscopic lavage in an animal model of pelvic inflammatory disease. J Am Assoc Gynecol Laparosc. 2002;9:4.-
17. Barrier agents for preventing adhesions after surgery for subfertility Cochrane Database Syst Rev. 2000;CD000475.-
18. Wiseman DM, Trout JR, Franklin RR, Diamond MP. Metaanalysis of the safety and efficacy of an adhesion barrier (Interceed TC7) in laparotomy. J Reprod Med. 1999;44:325-331.
19. Sawada T, Nishizawa H, Nishio E, Kadowaki M. Postoperative adhesion prevention with an oxidized regenerated cellulose adhesion barrier in infertile women. J Reprod. Med. 2000;45:387-389.
20. Uzunkoy A, Akinci OF, Coskun A, Aslan O, Kocyigit A. Effects of antiadhesive agents on the healing of intestinal anastomosis. Dis Colon Rectum. 2000;43:370-375.
21. Farquhar C, Vandekerckhove P, Arnot M, Lilford R. Laparoscopic “drilling” by diathermy or laser for ovulation induction in anovulatory polycystic ovary syndrome. Cochrane Database Syst Rev. 2000(2);CD001122.-
22. Greenblatt EM, Casper RF. Laparoscopic ovarian drilling in women with polycystic ovarian syndrome. Prog Clin Biol Res. 1993;381:129-138.
1. Operative Laparoscopy Study Group Postoperative adhesion development after operative laparoscopy: evaluation at early second look procedures. Fertil Steril. 1991;55:700-704.
2. Tulandi T, Murray C, Guralnick M. Adhesion formation and reproductive outcome after myomectomy and second-look laparoscopy. Obstet Gynecol. 1993;82:213-215.
3. Larsson B, Perbeck L. The possible advantage of keeping the uterine and intestinal serosa irrigated with saline to prevent intraabdominal adhesions in operations for infertility. An experimental study in rats. Acta Chir Scand Suppl. 1985;530:15-18.
4. Zamir G, Bloom AI, Reissman P. Prevention of intestinal adhesions after laparotomy in a rat model—a randomized prospective study. Res Exp Med (Berl). 1998;197:349-353.
5. Hurd WW, Himebaugh KS, Cofer KF, Gauvin JM, Elkins TE. The etiology of closure-related adhesion formation after wedge resection of the rabbit ovary. J Reprod Med. 1993;38:465-468.
6. Chen MD, Teigen GA, Reynolds HT, Johnson PR, Fowler JM. Laparoscopy versus laparotomy: an evaluation of adhesion formation after pelvic and paraaortic lymphadenectomy in a porcine model. Am J Obstet Gynecol. 1998;178:499-503.
7. Polymeneas G, Theodosopoulos T, Stamatiadis A, Kourias E. A comparative study of postoperative adhesion formation after laparoscopic vs. open cholecystectomy. Surg Endosc. 2001;15:41-43.
8. Smidt VJ, Singh DM, Hurteau JA, Hurd WW. Effect of carbon dioxide on human ovarian carcinoma cell growth. Am J Obstet Gynecol. 2001;185:1314-1317.
9. Tulandi T, Hum HS, Gelfand MM. Closure of laparotomy incisions with or without peritoneal suturing and second look laparoscopy. Am J Obstet Gynecol. 1988;158:536-537.
10. Kapur ML, Daneswar A, Chopra P. Evaluation of peritoneal closure at laparotomy. Am J Surg. 1979;137:650-652.
11. Cofer KF, Himebaugh KS, Gauvin JM, Hurd WW. Inhibition of adhesion reformation in the rabbit model by meclofenamate: an inhibitor of both prostaglandin and leukotriene production. Fertil Steril. 1994;62:1262-1265.
12. Elkelani OA, Molinas CR, Mynbaev O, Koninckx PR. Prevention of adhesions with crystalloids during laparoscopic surgery in mice. J Am Assoc Gynecol Laparosc. 2002;9:447-452.
13. Chan KL, Marino T, Qu WM, Tulandi T. Effects of intraperitoneal Ringer’s lactate instillation and infusion on postsurgical adhesion formation. J Gynecol Surg. 1995;11:241-243.
14. Watson A, Vandekerckhove P, Lilford R. Pharmacological adjuvants during infertility surgery: a systematic review of evidence derived from randomized controlled trial. Hum Fertil (Camb). 1999;2:149-157.
15. Larson B. Dextran—later clinical studies. clinical and experimental evaluation of different adjuvant therapies. Prog Clin Biol Res. 1990;358:165-175.
16. Roberts L, Sanfilippo JS, Ehrlich G, Raab S. Adhesion formation, peritoneal effects and the presence of bacterial biofilms after laparoscopic lavage in an animal model of pelvic inflammatory disease. J Am Assoc Gynecol Laparosc. 2002;9:4.-
17. Barrier agents for preventing adhesions after surgery for subfertility Cochrane Database Syst Rev. 2000;CD000475.-
18. Wiseman DM, Trout JR, Franklin RR, Diamond MP. Metaanalysis of the safety and efficacy of an adhesion barrier (Interceed TC7) in laparotomy. J Reprod Med. 1999;44:325-331.
19. Sawada T, Nishizawa H, Nishio E, Kadowaki M. Postoperative adhesion prevention with an oxidized regenerated cellulose adhesion barrier in infertile women. J Reprod. Med. 2000;45:387-389.
20. Uzunkoy A, Akinci OF, Coskun A, Aslan O, Kocyigit A. Effects of antiadhesive agents on the healing of intestinal anastomosis. Dis Colon Rectum. 2000;43:370-375.
21. Farquhar C, Vandekerckhove P, Arnot M, Lilford R. Laparoscopic “drilling” by diathermy or laser for ovulation induction in anovulatory polycystic ovary syndrome. Cochrane Database Syst Rev. 2000(2);CD001122.-
22. Greenblatt EM, Casper RF. Laparoscopic ovarian drilling in women with polycystic ovarian syndrome. Prog Clin Biol Res. 1993;381:129-138.