User login
A 55-year-old woman came to the clinic complaining of severe itching on her arms and legs. Although she itched throughout the day, it became intolerable at night, disrupting her sleep. She would sometimes scratch her arms and legs until exhaustion but could find no relief. Being outside in warm and sunny weather aggravated the problem. She had used moisturizers, emollients, and topical corticosteroids, but they only alleviated the itching temporarily. The itching began 10 months earlier, just after she finalized the divorce from her husband of 20 years.
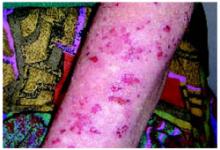
Examination of the skin revealed numerous excoriations with ulcerations and xerosis on the arms and left leg (Figure 1 and 2). The excoriations were located extensively from the dorsum of her left foot to above the knee and bilaterally from the wrist to above the elbow. They also showed signs of infection. The patient admitted they were self-inflicted. The patient’s right leg had been amputated 5 years before after a car accident, and she wore a prosthetic leg. Examination of other areas showed nothing remarkable.
The patient readily admitted to a great deal of psychological distress. She described feeling depressed since her divorce. She has had difficulty securing a full-time job and has high anxiety about being able to pay her rent and bills.
FIGURE 1
Excoriations on the arms…
FIGURE 2
…and the left leg
WHAT IS THE DIAGNOSIS?
WHAT IS THE TREATMENT STRATEGY?
DIFFERENTIAL DIAGNOSIS: PSYCHODERMATOLOGIC DISORDER
The patient’s history and physical examination points to a psychodermatologic disorder. Psycho-dermatologic disorders are conditions involving an interaction between the mind and skin and are classified as:3
- Psychophysiologic disorders:skin disorders worsened by emotional stress
- Primary psychiatric disorders:usually caused by psychological conditions with self-induced skin damage
- Secondary psychiatric disorders: psychological problems developed as a consequence of a disfiguring skin disorder, which negatively effects self-esteem and body image.3
This patient’s excoriations and ulcers are due to self-mutilation. The differential diagnosis includes psychogenic parasitosis, factitial dermatitis, and neurotic excoriations. These 3 skin conditions are primary psychiatric symptoms, and proper diagnosis revolves around being able to assess the dermatologic features and associated psychological disorder.2
Psychogenic parasitosis
Also known as delusional parasitosis, psychogenic parasitosis is a psychodermatologic disorder in which patients believe they are infested with parasites. Patients with this disorder report seeing or feeling parasites on their skin, and they damage their skin in an attempt to remove them. Patients create excoriations and ulcers on easily reached areas, usually the ears, eyes, nose, and extremities. They often present with what is termed the “matchbox sign,” in which they bring containers filled with “small bits of excoriated skin, dried blood, debris, or insect parts as proof of infestation.”2
Women over the age of 50 years are more often affected with psychogenic parasitosis, and the disorder is associated with anxiety, depression, and hypochondriasis.
Factitial dermatitis
Factitial dermatitis, also known as dermatitis artefacta, is a psychodermatologic disorder in which patients damage their skin but deny their self-involvement. This disorder encompasses a wide range of lesions, including blisters, cuts, ulcers, and burns. Patients often are unable to describe how the lesions evolved. Lesions exhibit bizarre patterns not characteristic of any disease.
Young adults and adolescents are more commonly affected, and it is 4 times more common among women than men. Psychological disorders involved with factitial dermatitis include personality disorders and posttraumatic stress disorder.2
Neurotic excoriations
Neurotic excoriations, sometimes referred to as neurodermatitis, are a result of a psychodermatologic disorder in which patients inflict excoriations and ulcers on their skin and admit to their involvement.3 The condition is characterized by excoriations similar in size and shape that are localized on areas easily reached by the patient, such as the arms, legs, and upper back.
The lesions may present in various stages, varying from dugout ulcers to ulcers covered with crusts and surrounded by erythema to areas receding into depressed scars. These lesions are a result of repetitive scratching and digging by the patient, usually without an underlying physical pathology but sometimes initiated by pruritus.1,2
Studies show the condition primarily affects women, with a mean onset between the ages of 30 to 45 years.1 Common psychiatric problems associated with neurotic excoriations include significant social stress, depression, anxiety, and obsessive-compulsive disorder.
Diagnosis: Neurotic excoriations due to depression and stress
The patient’s history and physical examination suggests a diagnosis of neurotic excoriations due to the characteristics of the excoriations and ulcers on her arms and leg, her admission of their self-inflicted nature, and the associated depression and psychosocial stress.
Laboratory tests
Although there are no available laboratory tests to confirm a positive finding of neurotic excoriations, tests could be performed to disprove any systemic causes of pruritus and the resulting dermatological damage.5 These tests include complete blood count with differential, chemistry profile, determination of thyroid-stimulating hormone levels, fasting plasma glucose level, and skin biopsies.1,
Laboratory tests for systemic causes of pruritus should be based on the patient’s physical and history, avoiding a broad approach.
Treatment: address the skin and the psyche
The treatment of neurotic excoriations requires a dual approach, addressing both the dermatological problems and the underlying psychological disorder.3 Supportive dermatologic care is necessary to avoid secondary complications and to ensure that the patient feels supported.3
Dermatologic care
Topical steroids can be helpful to decrease the pruritus and inflammation. The steroid strength should be chosen based upon the severity of the lesions and the thickness of the skin. Steroid ointments are preferred to creams when there are skin ulcers and deep excoriations.
If there is significant crusting or exudate, there is probably a secondary bacterial infection and oral antibiotics are indicated ( Figure 3). A first-generation cephalosporin or dicloxacillin should provide adequate coverage against the most likely organisms, Staphylococcus aureus and Streptococcus pyogenes.
FIGURE 3
Detail of lesions on the arm
Psychological care
The selective serotonin reuptake inhibitors produce a strong antipruritic response in patients with neurotic excoriations. Doxepin is a tricyclic antidepressant with one of the most powerful antihistamines for pruritus. When prescribing doxepin, limit the amount of medication dispensed at one time to minimize the risk of suicide.3 The patient should trim the fingernails to reduce the amount of damage caused by scratching and digging.
Treating the underlying psychological disorder requires supportive and empathic counseling. It may be necessary to collaborate with other mental health specialists. Management options include psychotropic medication, stress management courses, and referral to a psychiatrist. Patients with psychodermatologic disorders frequently resist referral to mental health professionals.3 If this is the case, family physicians are well positioned to help patients with psychological problems.
Alternative courses of treatment include hypnosis to disrupt the itch-scratch cycle, and acupuncture and supportive therapy to reduce underlying stressors.1
Patient’s outcome
By showing support and concern for the patient’s health during the visit, the physician strengthened the relationship with the patient, who felt comfortable disclosing many of her concerns and troubles. She received prescriptions for cephalexin 500 mg orally 3 times daily, 0.1% triamcinolone ointment to be applied twice daily, and doxepin 25 mg once nightly. She also received a referral for counseling.
At first she refused to trim her fingernails, but as she began to see that her ulcers were self-inflicted, she reconsidered and agreed. In fact, she asked to borrow our nail clippers before leaving the office.
- Cephalexin • Biocef, Keflex, Keftab
- Dicloxacillin • Dycill, Dynapen, Pathocil
- Doxepin • Adapin, Sinequan
Corresponding author
Richard P. Usatine, MD, University of Texas Health Sceicnes Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900.
Note: A handout developed by the American Academy of Family Physicians for patients with neurotic excoriations is available to print or photocopy at the following website: www.aafp.org/afp/20011215/neurph.html.
1. Cyr PR, Dreher GK. Neurotic excoriations. Am Fam Physician 2001;64:1981-1984.
2. Habif TP. Clinical Dermatology.4th ed. New York: Mosby; 2004.
3. Koo J, Lebwohl A. Psychodermatology: the mind and skin connection. Am Fam Physician 2001;64:1873-1878.
4. Moses S. Pruritic condition. In Family Practice Notebook [database online]. 2000; updated June 6, 2004. Available at:www.fpnotebook.com/DER258.htm. Accessed July 23, 2004.
5. Moses S. Pruritus causes. In Family Practice Notebook [database online]. 2000; updated June 6, 2004. Available at:www.fpnotebook.com/DER259.htm. Accessed July 23, 2004.
A 55-year-old woman came to the clinic complaining of severe itching on her arms and legs. Although she itched throughout the day, it became intolerable at night, disrupting her sleep. She would sometimes scratch her arms and legs until exhaustion but could find no relief. Being outside in warm and sunny weather aggravated the problem. She had used moisturizers, emollients, and topical corticosteroids, but they only alleviated the itching temporarily. The itching began 10 months earlier, just after she finalized the divorce from her husband of 20 years.
Examination of the skin revealed numerous excoriations with ulcerations and xerosis on the arms and left leg (Figure 1 and 2). The excoriations were located extensively from the dorsum of her left foot to above the knee and bilaterally from the wrist to above the elbow. They also showed signs of infection. The patient admitted they were self-inflicted. The patient’s right leg had been amputated 5 years before after a car accident, and she wore a prosthetic leg. Examination of other areas showed nothing remarkable.
The patient readily admitted to a great deal of psychological distress. She described feeling depressed since her divorce. She has had difficulty securing a full-time job and has high anxiety about being able to pay her rent and bills.
FIGURE 1
Excoriations on the arms…
FIGURE 2
…and the left leg
WHAT IS THE DIAGNOSIS?
WHAT IS THE TREATMENT STRATEGY?
DIFFERENTIAL DIAGNOSIS: PSYCHODERMATOLOGIC DISORDER
The patient’s history and physical examination points to a psychodermatologic disorder. Psycho-dermatologic disorders are conditions involving an interaction between the mind and skin and are classified as:3
- Psychophysiologic disorders:skin disorders worsened by emotional stress
- Primary psychiatric disorders:usually caused by psychological conditions with self-induced skin damage
- Secondary psychiatric disorders: psychological problems developed as a consequence of a disfiguring skin disorder, which negatively effects self-esteem and body image.3
This patient’s excoriations and ulcers are due to self-mutilation. The differential diagnosis includes psychogenic parasitosis, factitial dermatitis, and neurotic excoriations. These 3 skin conditions are primary psychiatric symptoms, and proper diagnosis revolves around being able to assess the dermatologic features and associated psychological disorder.2
Psychogenic parasitosis
Also known as delusional parasitosis, psychogenic parasitosis is a psychodermatologic disorder in which patients believe they are infested with parasites. Patients with this disorder report seeing or feeling parasites on their skin, and they damage their skin in an attempt to remove them. Patients create excoriations and ulcers on easily reached areas, usually the ears, eyes, nose, and extremities. They often present with what is termed the “matchbox sign,” in which they bring containers filled with “small bits of excoriated skin, dried blood, debris, or insect parts as proof of infestation.”2
Women over the age of 50 years are more often affected with psychogenic parasitosis, and the disorder is associated with anxiety, depression, and hypochondriasis.
Factitial dermatitis
Factitial dermatitis, also known as dermatitis artefacta, is a psychodermatologic disorder in which patients damage their skin but deny their self-involvement. This disorder encompasses a wide range of lesions, including blisters, cuts, ulcers, and burns. Patients often are unable to describe how the lesions evolved. Lesions exhibit bizarre patterns not characteristic of any disease.
Young adults and adolescents are more commonly affected, and it is 4 times more common among women than men. Psychological disorders involved with factitial dermatitis include personality disorders and posttraumatic stress disorder.2
Neurotic excoriations
Neurotic excoriations, sometimes referred to as neurodermatitis, are a result of a psychodermatologic disorder in which patients inflict excoriations and ulcers on their skin and admit to their involvement.3 The condition is characterized by excoriations similar in size and shape that are localized on areas easily reached by the patient, such as the arms, legs, and upper back.
The lesions may present in various stages, varying from dugout ulcers to ulcers covered with crusts and surrounded by erythema to areas receding into depressed scars. These lesions are a result of repetitive scratching and digging by the patient, usually without an underlying physical pathology but sometimes initiated by pruritus.1,2
Studies show the condition primarily affects women, with a mean onset between the ages of 30 to 45 years.1 Common psychiatric problems associated with neurotic excoriations include significant social stress, depression, anxiety, and obsessive-compulsive disorder.
Diagnosis: Neurotic excoriations due to depression and stress
The patient’s history and physical examination suggests a diagnosis of neurotic excoriations due to the characteristics of the excoriations and ulcers on her arms and leg, her admission of their self-inflicted nature, and the associated depression and psychosocial stress.
Laboratory tests
Although there are no available laboratory tests to confirm a positive finding of neurotic excoriations, tests could be performed to disprove any systemic causes of pruritus and the resulting dermatological damage.5 These tests include complete blood count with differential, chemistry profile, determination of thyroid-stimulating hormone levels, fasting plasma glucose level, and skin biopsies.1,
Laboratory tests for systemic causes of pruritus should be based on the patient’s physical and history, avoiding a broad approach.
Treatment: address the skin and the psyche
The treatment of neurotic excoriations requires a dual approach, addressing both the dermatological problems and the underlying psychological disorder.3 Supportive dermatologic care is necessary to avoid secondary complications and to ensure that the patient feels supported.3
Dermatologic care
Topical steroids can be helpful to decrease the pruritus and inflammation. The steroid strength should be chosen based upon the severity of the lesions and the thickness of the skin. Steroid ointments are preferred to creams when there are skin ulcers and deep excoriations.
If there is significant crusting or exudate, there is probably a secondary bacterial infection and oral antibiotics are indicated ( Figure 3). A first-generation cephalosporin or dicloxacillin should provide adequate coverage against the most likely organisms, Staphylococcus aureus and Streptococcus pyogenes.
FIGURE 3
Detail of lesions on the arm
Psychological care
The selective serotonin reuptake inhibitors produce a strong antipruritic response in patients with neurotic excoriations. Doxepin is a tricyclic antidepressant with one of the most powerful antihistamines for pruritus. When prescribing doxepin, limit the amount of medication dispensed at one time to minimize the risk of suicide.3 The patient should trim the fingernails to reduce the amount of damage caused by scratching and digging.
Treating the underlying psychological disorder requires supportive and empathic counseling. It may be necessary to collaborate with other mental health specialists. Management options include psychotropic medication, stress management courses, and referral to a psychiatrist. Patients with psychodermatologic disorders frequently resist referral to mental health professionals.3 If this is the case, family physicians are well positioned to help patients with psychological problems.
Alternative courses of treatment include hypnosis to disrupt the itch-scratch cycle, and acupuncture and supportive therapy to reduce underlying stressors.1
Patient’s outcome
By showing support and concern for the patient’s health during the visit, the physician strengthened the relationship with the patient, who felt comfortable disclosing many of her concerns and troubles. She received prescriptions for cephalexin 500 mg orally 3 times daily, 0.1% triamcinolone ointment to be applied twice daily, and doxepin 25 mg once nightly. She also received a referral for counseling.
At first she refused to trim her fingernails, but as she began to see that her ulcers were self-inflicted, she reconsidered and agreed. In fact, she asked to borrow our nail clippers before leaving the office.
- Cephalexin • Biocef, Keflex, Keftab
- Dicloxacillin • Dycill, Dynapen, Pathocil
- Doxepin • Adapin, Sinequan
Corresponding author
Richard P. Usatine, MD, University of Texas Health Sceicnes Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900.
Note: A handout developed by the American Academy of Family Physicians for patients with neurotic excoriations is available to print or photocopy at the following website: www.aafp.org/afp/20011215/neurph.html.
A 55-year-old woman came to the clinic complaining of severe itching on her arms and legs. Although she itched throughout the day, it became intolerable at night, disrupting her sleep. She would sometimes scratch her arms and legs until exhaustion but could find no relief. Being outside in warm and sunny weather aggravated the problem. She had used moisturizers, emollients, and topical corticosteroids, but they only alleviated the itching temporarily. The itching began 10 months earlier, just after she finalized the divorce from her husband of 20 years.
Examination of the skin revealed numerous excoriations with ulcerations and xerosis on the arms and left leg (Figure 1 and 2). The excoriations were located extensively from the dorsum of her left foot to above the knee and bilaterally from the wrist to above the elbow. They also showed signs of infection. The patient admitted they were self-inflicted. The patient’s right leg had been amputated 5 years before after a car accident, and she wore a prosthetic leg. Examination of other areas showed nothing remarkable.
The patient readily admitted to a great deal of psychological distress. She described feeling depressed since her divorce. She has had difficulty securing a full-time job and has high anxiety about being able to pay her rent and bills.
FIGURE 1
Excoriations on the arms…
FIGURE 2
…and the left leg
WHAT IS THE DIAGNOSIS?
WHAT IS THE TREATMENT STRATEGY?
DIFFERENTIAL DIAGNOSIS: PSYCHODERMATOLOGIC DISORDER
The patient’s history and physical examination points to a psychodermatologic disorder. Psycho-dermatologic disorders are conditions involving an interaction between the mind and skin and are classified as:3
- Psychophysiologic disorders:skin disorders worsened by emotional stress
- Primary psychiatric disorders:usually caused by psychological conditions with self-induced skin damage
- Secondary psychiatric disorders: psychological problems developed as a consequence of a disfiguring skin disorder, which negatively effects self-esteem and body image.3
This patient’s excoriations and ulcers are due to self-mutilation. The differential diagnosis includes psychogenic parasitosis, factitial dermatitis, and neurotic excoriations. These 3 skin conditions are primary psychiatric symptoms, and proper diagnosis revolves around being able to assess the dermatologic features and associated psychological disorder.2
Psychogenic parasitosis
Also known as delusional parasitosis, psychogenic parasitosis is a psychodermatologic disorder in which patients believe they are infested with parasites. Patients with this disorder report seeing or feeling parasites on their skin, and they damage their skin in an attempt to remove them. Patients create excoriations and ulcers on easily reached areas, usually the ears, eyes, nose, and extremities. They often present with what is termed the “matchbox sign,” in which they bring containers filled with “small bits of excoriated skin, dried blood, debris, or insect parts as proof of infestation.”2
Women over the age of 50 years are more often affected with psychogenic parasitosis, and the disorder is associated with anxiety, depression, and hypochondriasis.
Factitial dermatitis
Factitial dermatitis, also known as dermatitis artefacta, is a psychodermatologic disorder in which patients damage their skin but deny their self-involvement. This disorder encompasses a wide range of lesions, including blisters, cuts, ulcers, and burns. Patients often are unable to describe how the lesions evolved. Lesions exhibit bizarre patterns not characteristic of any disease.
Young adults and adolescents are more commonly affected, and it is 4 times more common among women than men. Psychological disorders involved with factitial dermatitis include personality disorders and posttraumatic stress disorder.2
Neurotic excoriations
Neurotic excoriations, sometimes referred to as neurodermatitis, are a result of a psychodermatologic disorder in which patients inflict excoriations and ulcers on their skin and admit to their involvement.3 The condition is characterized by excoriations similar in size and shape that are localized on areas easily reached by the patient, such as the arms, legs, and upper back.
The lesions may present in various stages, varying from dugout ulcers to ulcers covered with crusts and surrounded by erythema to areas receding into depressed scars. These lesions are a result of repetitive scratching and digging by the patient, usually without an underlying physical pathology but sometimes initiated by pruritus.1,2
Studies show the condition primarily affects women, with a mean onset between the ages of 30 to 45 years.1 Common psychiatric problems associated with neurotic excoriations include significant social stress, depression, anxiety, and obsessive-compulsive disorder.
Diagnosis: Neurotic excoriations due to depression and stress
The patient’s history and physical examination suggests a diagnosis of neurotic excoriations due to the characteristics of the excoriations and ulcers on her arms and leg, her admission of their self-inflicted nature, and the associated depression and psychosocial stress.
Laboratory tests
Although there are no available laboratory tests to confirm a positive finding of neurotic excoriations, tests could be performed to disprove any systemic causes of pruritus and the resulting dermatological damage.5 These tests include complete blood count with differential, chemistry profile, determination of thyroid-stimulating hormone levels, fasting plasma glucose level, and skin biopsies.1,
Laboratory tests for systemic causes of pruritus should be based on the patient’s physical and history, avoiding a broad approach.
Treatment: address the skin and the psyche
The treatment of neurotic excoriations requires a dual approach, addressing both the dermatological problems and the underlying psychological disorder.3 Supportive dermatologic care is necessary to avoid secondary complications and to ensure that the patient feels supported.3
Dermatologic care
Topical steroids can be helpful to decrease the pruritus and inflammation. The steroid strength should be chosen based upon the severity of the lesions and the thickness of the skin. Steroid ointments are preferred to creams when there are skin ulcers and deep excoriations.
If there is significant crusting or exudate, there is probably a secondary bacterial infection and oral antibiotics are indicated ( Figure 3). A first-generation cephalosporin or dicloxacillin should provide adequate coverage against the most likely organisms, Staphylococcus aureus and Streptococcus pyogenes.
FIGURE 3
Detail of lesions on the arm
Psychological care
The selective serotonin reuptake inhibitors produce a strong antipruritic response in patients with neurotic excoriations. Doxepin is a tricyclic antidepressant with one of the most powerful antihistamines for pruritus. When prescribing doxepin, limit the amount of medication dispensed at one time to minimize the risk of suicide.3 The patient should trim the fingernails to reduce the amount of damage caused by scratching and digging.
Treating the underlying psychological disorder requires supportive and empathic counseling. It may be necessary to collaborate with other mental health specialists. Management options include psychotropic medication, stress management courses, and referral to a psychiatrist. Patients with psychodermatologic disorders frequently resist referral to mental health professionals.3 If this is the case, family physicians are well positioned to help patients with psychological problems.
Alternative courses of treatment include hypnosis to disrupt the itch-scratch cycle, and acupuncture and supportive therapy to reduce underlying stressors.1
Patient’s outcome
By showing support and concern for the patient’s health during the visit, the physician strengthened the relationship with the patient, who felt comfortable disclosing many of her concerns and troubles. She received prescriptions for cephalexin 500 mg orally 3 times daily, 0.1% triamcinolone ointment to be applied twice daily, and doxepin 25 mg once nightly. She also received a referral for counseling.
At first she refused to trim her fingernails, but as she began to see that her ulcers were self-inflicted, she reconsidered and agreed. In fact, she asked to borrow our nail clippers before leaving the office.
- Cephalexin • Biocef, Keflex, Keftab
- Dicloxacillin • Dycill, Dynapen, Pathocil
- Doxepin • Adapin, Sinequan
Corresponding author
Richard P. Usatine, MD, University of Texas Health Sceicnes Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900.
Note: A handout developed by the American Academy of Family Physicians for patients with neurotic excoriations is available to print or photocopy at the following website: www.aafp.org/afp/20011215/neurph.html.
1. Cyr PR, Dreher GK. Neurotic excoriations. Am Fam Physician 2001;64:1981-1984.
2. Habif TP. Clinical Dermatology.4th ed. New York: Mosby; 2004.
3. Koo J, Lebwohl A. Psychodermatology: the mind and skin connection. Am Fam Physician 2001;64:1873-1878.
4. Moses S. Pruritic condition. In Family Practice Notebook [database online]. 2000; updated June 6, 2004. Available at:www.fpnotebook.com/DER258.htm. Accessed July 23, 2004.
5. Moses S. Pruritus causes. In Family Practice Notebook [database online]. 2000; updated June 6, 2004. Available at:www.fpnotebook.com/DER259.htm. Accessed July 23, 2004.
1. Cyr PR, Dreher GK. Neurotic excoriations. Am Fam Physician 2001;64:1981-1984.
2. Habif TP. Clinical Dermatology.4th ed. New York: Mosby; 2004.
3. Koo J, Lebwohl A. Psychodermatology: the mind and skin connection. Am Fam Physician 2001;64:1873-1878.
4. Moses S. Pruritic condition. In Family Practice Notebook [database online]. 2000; updated June 6, 2004. Available at:www.fpnotebook.com/DER258.htm. Accessed July 23, 2004.
5. Moses S. Pruritus causes. In Family Practice Notebook [database online]. 2000; updated June 6, 2004. Available at:www.fpnotebook.com/DER259.htm. Accessed July 23, 2004.