User login
U.S. endocrinologists reported an average income that continues to be among the lowest of all specialist groups, according to results from the latest Medscape Annual Compensation Report.
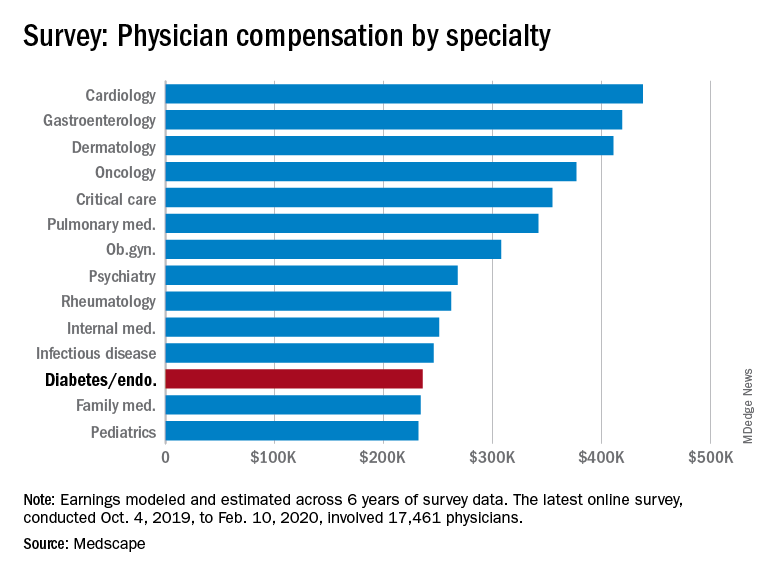
In the survey, which represents the responses of over 17,000 physicians in more than 30 specialties, endocrinologists report an average annual income of $236,000, which is unchanged from that detailed last year.
The report reflects data collected from Oct. 4, 2019 to Feb. 10, 2020, so does not take into account any effects of the COVID-19 pandemic.
It puts the diabetes and endocrinology specialty above family medicine, public health and preventive medicine, and pediatrics but nevertheless among the lowest-earning specialties.
At the opposite end of the earnings scale, orthopedics is at the top, with those doctors earning an average of $511,000 per year, followed by plastic surgery, otolaryngology, cardiology, and radiology.
The reported compensation reflects full-time salaries with patient care, including salary, bonus, and profit-sharing contributions for employed physicians, and earnings after taxes and deductible business expenses for self-employed physicians practicing medicine in the United States.
A gender gap in compensation is still apparent, with male endocrinologists earning about 23% more ($258,000) than their female counterparts ($209,000).
Overall, male specialists earn 31% more than women, which is a slight improvement on the 33% gender pay gap reported in 2019.
Survey respondents were 64% male and 34% female, with 2% declining to respond.
Half happy with pay, most would still choose same path
Around half (49%) of endocrinologists reported feeling fairly compensated for their work, an increase from last year’s rate of 42%.
In all, 82% said – if given another chance – they would choose a career in medicine again, higher than the rate of 77% of physicians overall. And as many as 80% said they would remain in the specialty of endocrinology.
For 35% of endocrinologists, the most rewarding part of their job is gratitude and relationships with patients. The most challenging part is “having so many rules and regulations,” cited by 25% of respondents, followed by working with an EHR system, reported by 20%.
Endocrinologists spent an average of about 34 hours per week seeing patients, lower than the 37.9 hours per week reported among all physicians. And the average of 16.5 hours per week spent on paperwork and administration by endocrinologists is similar to the 15.6 hours reported by physicians overall.
In terms of Medicare and Medicaid patients, 71% of endocrinologists said they had no plans to stop providing services to Medicare and Medicaid patients, which is similar to the overall rate of 73%.
About half of endocrinologists (51%) reported using nurse practitioners and 25% used physician assistants, while 42% used neither.
Among those using nurse practitioners or physician assistants, 50% reported that the assistance increased profitability; 44% said the staffers had no effect on profitability, and 6% reported decreased profitability.
Only about 13% of endocrinologists reported having claims denied or needing to be resubmitted, well below the highest levels of 28% and 22% reported in plastic surgery and emergency medicine, respectively.
COVID-19 suppresses compensation, but boosts telemedicine
Subsequent compensation surveys can be expected to reflect the heavy toll that COVID-19 pandemic has taken on nearly all professions in health care – as well as global economies as a whole.
Specialist practices in general report as much as a 55% decrease in revenue, on average, and a 60% decrease in patient volume since the beginning of the crisis, according to the report.
As many as 43,000 U.S. health care workers were reportedly laid off in March 2020 alone, as hospitals and physician groups announced layoffs, furloughs, and pay cuts in response to the fallout from the pandemic. And a reported 9% of independent medical practices have had to close, at least temporarily.
Meanwhile, the use of remote technologies for patient engagement has increased by 225%.
Specialties that rely heavily on elective procedures that were for the most part delayed during the pandemic have been particularly hard-hit, notably in those practicing orthopedics, plastic surgery, dermatology, cardiology, and ophthalmology.
“The health impact of COVID-19 has been grave, and the financial fallout is widespread,” according to the Medscape report.
A version of this article originally appeared on Medscape.com.
U.S. endocrinologists reported an average income that continues to be among the lowest of all specialist groups, according to results from the latest Medscape Annual Compensation Report.
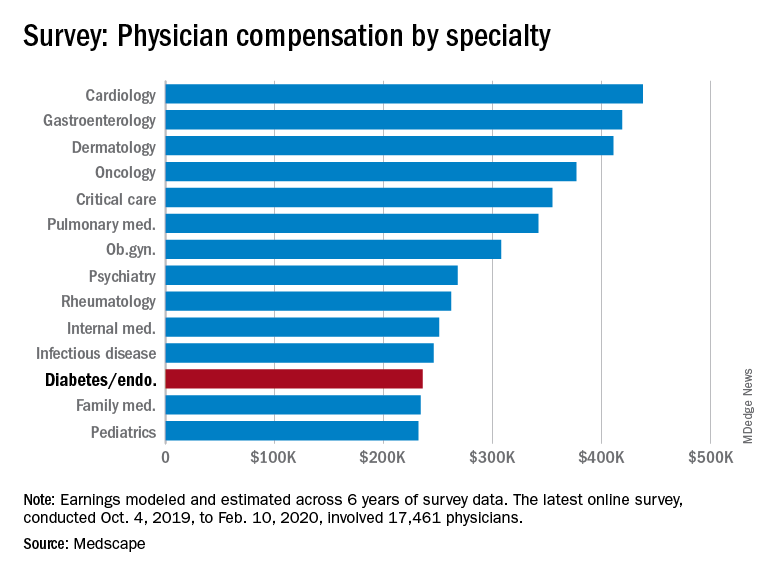
In the survey, which represents the responses of over 17,000 physicians in more than 30 specialties, endocrinologists report an average annual income of $236,000, which is unchanged from that detailed last year.
The report reflects data collected from Oct. 4, 2019 to Feb. 10, 2020, so does not take into account any effects of the COVID-19 pandemic.
It puts the diabetes and endocrinology specialty above family medicine, public health and preventive medicine, and pediatrics but nevertheless among the lowest-earning specialties.
At the opposite end of the earnings scale, orthopedics is at the top, with those doctors earning an average of $511,000 per year, followed by plastic surgery, otolaryngology, cardiology, and radiology.
The reported compensation reflects full-time salaries with patient care, including salary, bonus, and profit-sharing contributions for employed physicians, and earnings after taxes and deductible business expenses for self-employed physicians practicing medicine in the United States.
A gender gap in compensation is still apparent, with male endocrinologists earning about 23% more ($258,000) than their female counterparts ($209,000).
Overall, male specialists earn 31% more than women, which is a slight improvement on the 33% gender pay gap reported in 2019.
Survey respondents were 64% male and 34% female, with 2% declining to respond.
Half happy with pay, most would still choose same path
Around half (49%) of endocrinologists reported feeling fairly compensated for their work, an increase from last year’s rate of 42%.
In all, 82% said – if given another chance – they would choose a career in medicine again, higher than the rate of 77% of physicians overall. And as many as 80% said they would remain in the specialty of endocrinology.
For 35% of endocrinologists, the most rewarding part of their job is gratitude and relationships with patients. The most challenging part is “having so many rules and regulations,” cited by 25% of respondents, followed by working with an EHR system, reported by 20%.
Endocrinologists spent an average of about 34 hours per week seeing patients, lower than the 37.9 hours per week reported among all physicians. And the average of 16.5 hours per week spent on paperwork and administration by endocrinologists is similar to the 15.6 hours reported by physicians overall.
In terms of Medicare and Medicaid patients, 71% of endocrinologists said they had no plans to stop providing services to Medicare and Medicaid patients, which is similar to the overall rate of 73%.
About half of endocrinologists (51%) reported using nurse practitioners and 25% used physician assistants, while 42% used neither.
Among those using nurse practitioners or physician assistants, 50% reported that the assistance increased profitability; 44% said the staffers had no effect on profitability, and 6% reported decreased profitability.
Only about 13% of endocrinologists reported having claims denied or needing to be resubmitted, well below the highest levels of 28% and 22% reported in plastic surgery and emergency medicine, respectively.
COVID-19 suppresses compensation, but boosts telemedicine
Subsequent compensation surveys can be expected to reflect the heavy toll that COVID-19 pandemic has taken on nearly all professions in health care – as well as global economies as a whole.
Specialist practices in general report as much as a 55% decrease in revenue, on average, and a 60% decrease in patient volume since the beginning of the crisis, according to the report.
As many as 43,000 U.S. health care workers were reportedly laid off in March 2020 alone, as hospitals and physician groups announced layoffs, furloughs, and pay cuts in response to the fallout from the pandemic. And a reported 9% of independent medical practices have had to close, at least temporarily.
Meanwhile, the use of remote technologies for patient engagement has increased by 225%.
Specialties that rely heavily on elective procedures that were for the most part delayed during the pandemic have been particularly hard-hit, notably in those practicing orthopedics, plastic surgery, dermatology, cardiology, and ophthalmology.
“The health impact of COVID-19 has been grave, and the financial fallout is widespread,” according to the Medscape report.
A version of this article originally appeared on Medscape.com.
U.S. endocrinologists reported an average income that continues to be among the lowest of all specialist groups, according to results from the latest Medscape Annual Compensation Report.
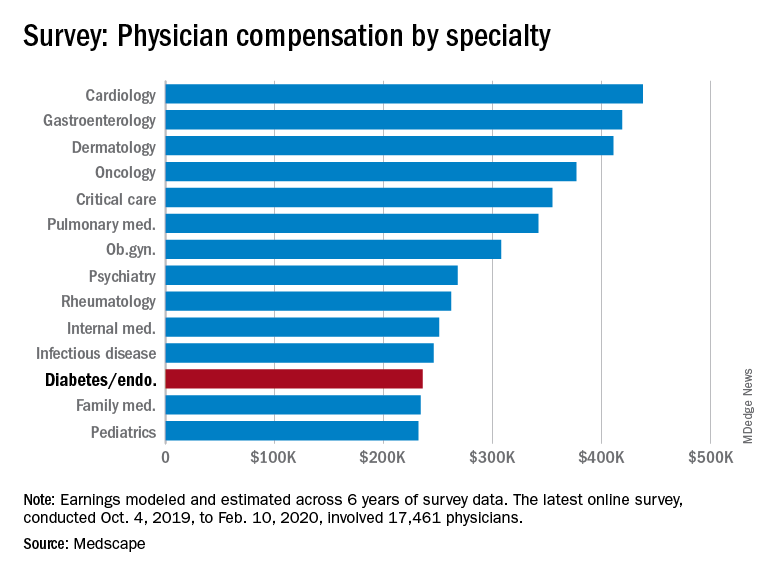
In the survey, which represents the responses of over 17,000 physicians in more than 30 specialties, endocrinologists report an average annual income of $236,000, which is unchanged from that detailed last year.
The report reflects data collected from Oct. 4, 2019 to Feb. 10, 2020, so does not take into account any effects of the COVID-19 pandemic.
It puts the diabetes and endocrinology specialty above family medicine, public health and preventive medicine, and pediatrics but nevertheless among the lowest-earning specialties.
At the opposite end of the earnings scale, orthopedics is at the top, with those doctors earning an average of $511,000 per year, followed by plastic surgery, otolaryngology, cardiology, and radiology.
The reported compensation reflects full-time salaries with patient care, including salary, bonus, and profit-sharing contributions for employed physicians, and earnings after taxes and deductible business expenses for self-employed physicians practicing medicine in the United States.
A gender gap in compensation is still apparent, with male endocrinologists earning about 23% more ($258,000) than their female counterparts ($209,000).
Overall, male specialists earn 31% more than women, which is a slight improvement on the 33% gender pay gap reported in 2019.
Survey respondents were 64% male and 34% female, with 2% declining to respond.
Half happy with pay, most would still choose same path
Around half (49%) of endocrinologists reported feeling fairly compensated for their work, an increase from last year’s rate of 42%.
In all, 82% said – if given another chance – they would choose a career in medicine again, higher than the rate of 77% of physicians overall. And as many as 80% said they would remain in the specialty of endocrinology.
For 35% of endocrinologists, the most rewarding part of their job is gratitude and relationships with patients. The most challenging part is “having so many rules and regulations,” cited by 25% of respondents, followed by working with an EHR system, reported by 20%.
Endocrinologists spent an average of about 34 hours per week seeing patients, lower than the 37.9 hours per week reported among all physicians. And the average of 16.5 hours per week spent on paperwork and administration by endocrinologists is similar to the 15.6 hours reported by physicians overall.
In terms of Medicare and Medicaid patients, 71% of endocrinologists said they had no plans to stop providing services to Medicare and Medicaid patients, which is similar to the overall rate of 73%.
About half of endocrinologists (51%) reported using nurse practitioners and 25% used physician assistants, while 42% used neither.
Among those using nurse practitioners or physician assistants, 50% reported that the assistance increased profitability; 44% said the staffers had no effect on profitability, and 6% reported decreased profitability.
Only about 13% of endocrinologists reported having claims denied or needing to be resubmitted, well below the highest levels of 28% and 22% reported in plastic surgery and emergency medicine, respectively.
COVID-19 suppresses compensation, but boosts telemedicine
Subsequent compensation surveys can be expected to reflect the heavy toll that COVID-19 pandemic has taken on nearly all professions in health care – as well as global economies as a whole.
Specialist practices in general report as much as a 55% decrease in revenue, on average, and a 60% decrease in patient volume since the beginning of the crisis, according to the report.
As many as 43,000 U.S. health care workers were reportedly laid off in March 2020 alone, as hospitals and physician groups announced layoffs, furloughs, and pay cuts in response to the fallout from the pandemic. And a reported 9% of independent medical practices have had to close, at least temporarily.
Meanwhile, the use of remote technologies for patient engagement has increased by 225%.
Specialties that rely heavily on elective procedures that were for the most part delayed during the pandemic have been particularly hard-hit, notably in those practicing orthopedics, plastic surgery, dermatology, cardiology, and ophthalmology.
“The health impact of COVID-19 has been grave, and the financial fallout is widespread,” according to the Medscape report.
A version of this article originally appeared on Medscape.com.