User login
DALLAS – The use of an electronic health record order-set with built-in clinical decision support for ischemic stroke patients in the emergency department was associated with markedly improved patient outcomes in a large observational study.
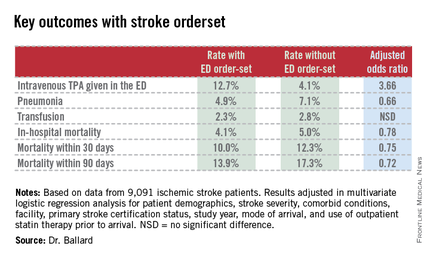
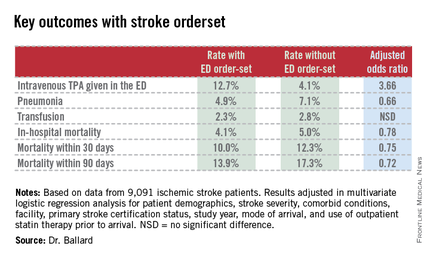
Where the order-set was used, stroke patients were significantly more likely to receive tissue plasminogen activator (TPA) therapy in the ED. They were also significantly less likely to develop pneumonia, including aspiration pneumonia. And they had significantly reduced in-hospital, 30- and 90-day mortality, compared with patients in EDs where the stroke order-set wasn’t yet available, Dr. Dustin W. Ballard reported at the annual meeting of the Society for Academic Emergency Medicine.
"The magnitude of the difference in outcomes was greater than we expected, for certain," commented Dr. Ballard, an emergency medicine physician at Kaiser Permanente San Rafael (Calif.) Medical Center.
This retrospective observational study took advantage of a natural experiment going on within the 21–medical center Kaiser Permanente of Northern California integrated health care delivery system. During 2007-2012, an electronic health record (EHR) with stroke order-set was introduced across the system in staggered fashion such that it was up and running in some of the 21 EDs, while in others, it wasn’t yet available. As a result, Dr. Ballard was able to report on 9,091 ischemic stroke patients who presented to Kaiser Permanente EDs during the study period, 53% of whom were managed with the assistance of the stroke order-set.
The order-set incorporates laboratory tests, neuroimaging orders, and other diagnostic options as well as inclusion and exclusion criteria for TPA therapy, TPA dosing recommendations, criteria for conducting a swallowing evaluation, and dysphagia orders.
"Where it was available for use, there was no mandate that ED physicians had to use it. It’s intended to be the first thing you open up when you see a patient who you think might have a stroke. I use the order-set in all patients I think might have stroke. It gives me back-up, regardless of whether I think I’m going to use TPA or not. But certainly if I were going to use TPA, I can scan through the inclusion/exclusion criteria really quickly, and the dosing recommendations are right there. There are certainly other ways to get that information, but the order-set just makes it much simpler and much easier. I think that’s the primary reason why we’re seeing much higher TPA utilization rates," Dr. Ballard explained.
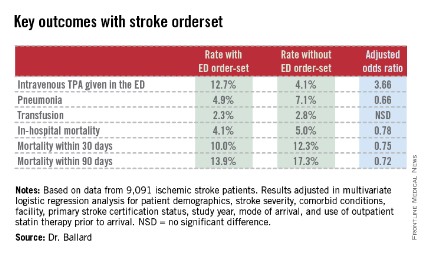
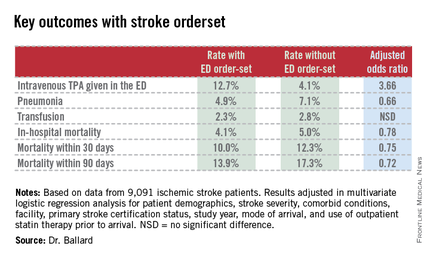
Indeed, when the order-set was used, 12.7% of stroke patients received intravenous TPA in the ED. Where it wasn’t, the rate was 4.1%. And reassuringly, this nearly 3.7-fold greater use of TPA wasn’t accompanied by an increased rate of bleeding requiring transfusion (see chart).
Audience members who feel pressure to convince their hospital administrators that an ED provides good value to a medical center even if the ED isn’t a major profit center greeted the study results enthusiastically.
"This could be very exciting," one physician rose to comment. "Now we’ve not only got a checklist for stroke, but we’ve also got a mortality reduction in those patients it’s provided to."
Other audience members cautioned that confounding by indication is always a potential concern in a retrospective study such as this. That is, perhaps when ED physicians encountered a patient with a really severe stroke and low likelihood of successful recovery, they dispensed with the order-set. Dr. Ballard responded that patient stroke severity scores and overall comorbidity burden were similar in the groups with and without the order-set. And while secular trends in stroke diagnosis and treatment during 2007-2012 led to an overall reduction in stroke mortality at Kaiser Permanente during that period, "it was not anywhere near as dramatic as what we see with the order-set," he added.
Dr. Ballard noted that the Kaiser Permanente results add to a growing body of evidence that carefully designed order-sets for selected disorders leads to improved clinical outcomes. Most of those studies, however, involved paper order-sets rather than electronic aids.
The study was supported by the Kaiser Permanente Division of Research. Dr. Ballard is a Kaiser Permanente employee.
|
|
Physician apprehension of "cookbook" medicine should be relegated to a bygone era. The seamless use of standard work processes such as checklists or well constructed EMR order sets can support the delivery of consistent evidence-based care and let the clinician focus their time on communication and management decisions for the clinical outliers. The growing body of evidence supporting integration of standard work continues to expand–an ED based stroke order set in this study by Kaiser is just one more excellent example.
Dr. Robert Pendleton is codirector of University of Utah Hospitalist Program, director of University Healthcare Thrombosis Service, both in Salt Lake City, and an adviser to Hospitalist News.
|
|
Physician apprehension of "cookbook" medicine should be relegated to a bygone era. The seamless use of standard work processes such as checklists or well constructed EMR order sets can support the delivery of consistent evidence-based care and let the clinician focus their time on communication and management decisions for the clinical outliers. The growing body of evidence supporting integration of standard work continues to expand–an ED based stroke order set in this study by Kaiser is just one more excellent example.
Dr. Robert Pendleton is codirector of University of Utah Hospitalist Program, director of University Healthcare Thrombosis Service, both in Salt Lake City, and an adviser to Hospitalist News.
|
|
Physician apprehension of "cookbook" medicine should be relegated to a bygone era. The seamless use of standard work processes such as checklists or well constructed EMR order sets can support the delivery of consistent evidence-based care and let the clinician focus their time on communication and management decisions for the clinical outliers. The growing body of evidence supporting integration of standard work continues to expand–an ED based stroke order set in this study by Kaiser is just one more excellent example.
Dr. Robert Pendleton is codirector of University of Utah Hospitalist Program, director of University Healthcare Thrombosis Service, both in Salt Lake City, and an adviser to Hospitalist News.
DALLAS – The use of an electronic health record order-set with built-in clinical decision support for ischemic stroke patients in the emergency department was associated with markedly improved patient outcomes in a large observational study.
Where the order-set was used, stroke patients were significantly more likely to receive tissue plasminogen activator (TPA) therapy in the ED. They were also significantly less likely to develop pneumonia, including aspiration pneumonia. And they had significantly reduced in-hospital, 30- and 90-day mortality, compared with patients in EDs where the stroke order-set wasn’t yet available, Dr. Dustin W. Ballard reported at the annual meeting of the Society for Academic Emergency Medicine.
"The magnitude of the difference in outcomes was greater than we expected, for certain," commented Dr. Ballard, an emergency medicine physician at Kaiser Permanente San Rafael (Calif.) Medical Center.
This retrospective observational study took advantage of a natural experiment going on within the 21–medical center Kaiser Permanente of Northern California integrated health care delivery system. During 2007-2012, an electronic health record (EHR) with stroke order-set was introduced across the system in staggered fashion such that it was up and running in some of the 21 EDs, while in others, it wasn’t yet available. As a result, Dr. Ballard was able to report on 9,091 ischemic stroke patients who presented to Kaiser Permanente EDs during the study period, 53% of whom were managed with the assistance of the stroke order-set.
The order-set incorporates laboratory tests, neuroimaging orders, and other diagnostic options as well as inclusion and exclusion criteria for TPA therapy, TPA dosing recommendations, criteria for conducting a swallowing evaluation, and dysphagia orders.
"Where it was available for use, there was no mandate that ED physicians had to use it. It’s intended to be the first thing you open up when you see a patient who you think might have a stroke. I use the order-set in all patients I think might have stroke. It gives me back-up, regardless of whether I think I’m going to use TPA or not. But certainly if I were going to use TPA, I can scan through the inclusion/exclusion criteria really quickly, and the dosing recommendations are right there. There are certainly other ways to get that information, but the order-set just makes it much simpler and much easier. I think that’s the primary reason why we’re seeing much higher TPA utilization rates," Dr. Ballard explained.
Indeed, when the order-set was used, 12.7% of stroke patients received intravenous TPA in the ED. Where it wasn’t, the rate was 4.1%. And reassuringly, this nearly 3.7-fold greater use of TPA wasn’t accompanied by an increased rate of bleeding requiring transfusion (see chart).
Audience members who feel pressure to convince their hospital administrators that an ED provides good value to a medical center even if the ED isn’t a major profit center greeted the study results enthusiastically.
"This could be very exciting," one physician rose to comment. "Now we’ve not only got a checklist for stroke, but we’ve also got a mortality reduction in those patients it’s provided to."
Other audience members cautioned that confounding by indication is always a potential concern in a retrospective study such as this. That is, perhaps when ED physicians encountered a patient with a really severe stroke and low likelihood of successful recovery, they dispensed with the order-set. Dr. Ballard responded that patient stroke severity scores and overall comorbidity burden were similar in the groups with and without the order-set. And while secular trends in stroke diagnosis and treatment during 2007-2012 led to an overall reduction in stroke mortality at Kaiser Permanente during that period, "it was not anywhere near as dramatic as what we see with the order-set," he added.
Dr. Ballard noted that the Kaiser Permanente results add to a growing body of evidence that carefully designed order-sets for selected disorders leads to improved clinical outcomes. Most of those studies, however, involved paper order-sets rather than electronic aids.
The study was supported by the Kaiser Permanente Division of Research. Dr. Ballard is a Kaiser Permanente employee.
DALLAS – The use of an electronic health record order-set with built-in clinical decision support for ischemic stroke patients in the emergency department was associated with markedly improved patient outcomes in a large observational study.
Where the order-set was used, stroke patients were significantly more likely to receive tissue plasminogen activator (TPA) therapy in the ED. They were also significantly less likely to develop pneumonia, including aspiration pneumonia. And they had significantly reduced in-hospital, 30- and 90-day mortality, compared with patients in EDs where the stroke order-set wasn’t yet available, Dr. Dustin W. Ballard reported at the annual meeting of the Society for Academic Emergency Medicine.
"The magnitude of the difference in outcomes was greater than we expected, for certain," commented Dr. Ballard, an emergency medicine physician at Kaiser Permanente San Rafael (Calif.) Medical Center.
This retrospective observational study took advantage of a natural experiment going on within the 21–medical center Kaiser Permanente of Northern California integrated health care delivery system. During 2007-2012, an electronic health record (EHR) with stroke order-set was introduced across the system in staggered fashion such that it was up and running in some of the 21 EDs, while in others, it wasn’t yet available. As a result, Dr. Ballard was able to report on 9,091 ischemic stroke patients who presented to Kaiser Permanente EDs during the study period, 53% of whom were managed with the assistance of the stroke order-set.
The order-set incorporates laboratory tests, neuroimaging orders, and other diagnostic options as well as inclusion and exclusion criteria for TPA therapy, TPA dosing recommendations, criteria for conducting a swallowing evaluation, and dysphagia orders.
"Where it was available for use, there was no mandate that ED physicians had to use it. It’s intended to be the first thing you open up when you see a patient who you think might have a stroke. I use the order-set in all patients I think might have stroke. It gives me back-up, regardless of whether I think I’m going to use TPA or not. But certainly if I were going to use TPA, I can scan through the inclusion/exclusion criteria really quickly, and the dosing recommendations are right there. There are certainly other ways to get that information, but the order-set just makes it much simpler and much easier. I think that’s the primary reason why we’re seeing much higher TPA utilization rates," Dr. Ballard explained.
Indeed, when the order-set was used, 12.7% of stroke patients received intravenous TPA in the ED. Where it wasn’t, the rate was 4.1%. And reassuringly, this nearly 3.7-fold greater use of TPA wasn’t accompanied by an increased rate of bleeding requiring transfusion (see chart).
Audience members who feel pressure to convince their hospital administrators that an ED provides good value to a medical center even if the ED isn’t a major profit center greeted the study results enthusiastically.
"This could be very exciting," one physician rose to comment. "Now we’ve not only got a checklist for stroke, but we’ve also got a mortality reduction in those patients it’s provided to."
Other audience members cautioned that confounding by indication is always a potential concern in a retrospective study such as this. That is, perhaps when ED physicians encountered a patient with a really severe stroke and low likelihood of successful recovery, they dispensed with the order-set. Dr. Ballard responded that patient stroke severity scores and overall comorbidity burden were similar in the groups with and without the order-set. And while secular trends in stroke diagnosis and treatment during 2007-2012 led to an overall reduction in stroke mortality at Kaiser Permanente during that period, "it was not anywhere near as dramatic as what we see with the order-set," he added.
Dr. Ballard noted that the Kaiser Permanente results add to a growing body of evidence that carefully designed order-sets for selected disorders leads to improved clinical outcomes. Most of those studies, however, involved paper order-sets rather than electronic aids.
The study was supported by the Kaiser Permanente Division of Research. Dr. Ballard is a Kaiser Permanente employee.
AT SAEM 2014
Key clinical point: Embrace EHR stroke order-sets to improve clinical decision making.
Major finding: In-hospital mortality in patients who presented to the ED with ischemic stroke was 4.1% if ED physicians used an EHR stroke order-set and significantly worse at 5.0% if physicians didn’t yet have access to the electronic order-set.
Data source: This was a retrospective observational study of 9,091 patients who presented with ischemic stroke to 1 of 21 EDs in an integrated health system during 2007-2012. A total of 53% were managed with the assistance of an EHR stroke order-set for the ED.
Disclosures: The study was sponsored by Kaiser Permanente. The presenter is employed as an emergency medicine physician by the health system.