User login
Discuss this article at http://currentpsychiatry.blogspot.com/2010/07/cholesterol-mood-and-vascular-health.html#comments
A growing body of literature examining the putative links among cholesterol, mood disorders, and suicide has produced inconsistent findings and unclear clinical implications that may leave psychiatrists unsure of how to interpret the data. Understanding cholesterol’s role in mood disorders may be relevant to the 2 primary causes of excess deaths in patients with mood disorders: suicide and vascular disease.1
Plausible links
In the early 1990s several studies suggested a link between low cholesterol (<160 mg/dL) and unnatural deaths, including suicide.2-4 Follow-up studies confirmed associations between low cholesterol and suicide attempts, especially violent ones.5 These associations are compelling given the neurobiologic effects of cholesterol, such as a net reduction of serotonergic function (Box 1). Low cholesterol may predispose an individual to aggression, impulsivity, and violence (Table 1).6 Many studies have found that patients with mood disorders have lower cholesterol levels;7 however, other research suggests they are at increased risk of hyperlipidemia, typically hypertriglyceridemia rather than hypercholesterolemia.8
Depression. Several studies have shown an association between low cholesterol and depressive symptoms, although this finding has not been replicated in Asian subjects.9,10 Patients with manic or mixed syndromes have been found to have lower serum cholesterol,11 and individuals with major depression and bipolar disorder have lower cholesterol levels in the brain compared with healthy controls.12 Some studies have observed higher total cholesterol levels after patients receive pharmacotherapy for major depressive symptoms.13 These findings have led to speculation that low serum cholesterol in patients with mood disorders is partially a state-dependent effect of depressive illness.
Suicide. Cohort, case-control, and cross-sectional studies have linked low cholesterol to an increased risk of suicide.2,5 Individuals who attempt suicide by violent means have lower cholesterol compared with those who use less violent methods.5,14 A meta-analysis found statistically significant correlations between low cholesterol and future or past suicidal behavior; however, low cholesterol explained <0.01% of suicidal behavior.15 Studies comparing cholesterol levels of individuals following violent vs nonviolent suicide attempts have demonstrated stronger associations.15
Assessing suicide risk. Current evidence does not support considering low serum cholesterol a risk factor for suicide. One study used cholesterol as a clinical predictor of suicide,16 but this model has not been prospectively validated. As a whole, the evidence does not suggest that cholesterol levels explain a substantial portion of suicidal behaviors.
The neurobiologic effects of low cholesterol—particularly those related to serotonergic hypofunction—are thought to be mediate impulsive, aggressive, and violent behaviors that may predispose an individual to suicide.a,b The CNS contains one-fourth of the body’s free cholesterol,c which is synthesized primarily in situ.
Cholesterol improves membrane stability, reduces permeability, and may influence serotonergic function. Cholesterol depletion may impair function of 5-HT1A and 5-HT7 receptorsd,e and serotonin transporter activity.f Reduced cholesterol after treatment with simvastatin—an HMG-CoA reductase inhibitor that readily crosses the blood-brain barrier—resulted in acute (1-month) increases in serotonin transporter activity followed by subacute (>2 months) decreases.g Lower cholesterol levels may further decrease expression of serotonin receptors and cause a net reduction in serotonergic activity.
In addition, cholesterol is necessary for synapse formation and myelin production. Cholesterol depletion may have more diffuse effects on neurotransmission, such as gamma-aminobutyric acid receptors,hN-methyl-D-aspartate receptors,i opioid signaling,j and excitatory amino acids transport.k
Impulsivity associated with low serotonergic function and low total cholesterol has been suggested as a potential pathway for suicide.l Low cholesterol is associated with self-report measures of impulsivity;m however, increased impulsivity associated with lipid-lowering therapy may be temporary,n which is similar to the time-limited changes in serotonin transporter activity.g Human and animal data have suggested that low cholesterol may be linked to violent behaviors, including suicide.o
Source:
a. Vevera J, Fisar Z, Kvasnicka T, et al. Cholesterol-lowering therapy evokes time-limited changes in serotonergic transmission. Psychiatry Res. 2005;133(2-3):197-203.
b. Kaplan JR, Shively CA, Fontenot MB, et al. Demonstration of an association among dietary cholesterol, central serotonergic activity, and social behavior in monkeys. Psychosom Med. 1994;56(6):479-484.
c. Chattopadhyay A, Paila YD. Lipid-protein interactions, regulation and dysfunction of brain cholesterol. Biochem Biophys Res Commun. 2007;354(3):627-633.
d. Singh P, Paila YD, Chattopadhyay A. Differential effects of cholesterol and 7-dehydrocholesterol on the ligand binding activity of the hippocampal serotonin(1A) receptor: implications in SLOS. Biochem Biophys Res Commun. 2007;358(2):495-499.
e. Sjögren B, Hamblin MW, Svenningsson P. Cholesterol depletion reduces serotonin binding and signaling via human 5-HT(7(a)) receptors. Eur J Pharmacol. 2006;552(1-3):1-10.
f. Scanlon SM, Williams DC, Schloss P. Membrane cholesterol modulates serotonin transporter activity. Biochemistry. 2001;40(35):10507-10513.
g. Vevera J, Fisar Z, Kvasnicka T, et al. Cholesterol-lowering therapy evokes time-limited changes in serotonergic transmission. Psychiatry Res. 2005;133(2-3):197-203.
h. Sooksawate T, Simmonds MA. Effects of membrane cholesterol on the sensitivity of the GABA(A) receptor to GABA in acutely dissociated rat hippocampal neurones. Neuropharmacology. 2001;40(2):178-184.
i. Abulrob A, Tauskela JS, Mealing G, et al. Protection by cholesterol-extracting cyclodextrins: a role for N-methyl-daspartate receptor redistribution. J Neurochem. 2005;92(6):1477-1486.
j. Huang P, Xu W, Yoon SI, et al. Cholesterol reduction by methyl-beta-cyclodextrin attenuates the delta opioid receptor-mediated signaling in neuronal cells but enhances it in non-neuronal cells. Biochem Pharmacol. 2007;73(4):534-549.
k. Butchbach ME, Tian G, Guo H, et al. Association of excitatory amino acid transporters, especially EAAT2, with cholesterol-rich lipid raft microdomains: importance for excitatory amino acid transporter localization and function. J Biol Chem. 2004;279(33):34388-34396.
l. Fawcett J, Busch KA, Jacobs D, et al. Suicide: a four-pathway clinical-biochemical model. Annals N Y Acad Sci. 1997;836:288-301.
m. Garland M, Hickey D, Corvin A, et al. Total serum cholesterol in relation to psychological correlates in parasuicide. Br J Psychiatry. 2000;177:77-83.
n. Ormiston T, Wolkowitz OM, Reus VI, et al. Behavioral implications of lowering cholesterol levels: a double-blind pilot study. Psychosomatics. 2003;44(5):412-414.
o. Golomb BA. Cholesterol and violence: is there a connection? Ann Intern Med. 1998;128(6):478-487.
Table 1
Psychiatric features associated with low cholesterol*
| Symptoms |
| Anxiety, depressed mood, emotional lability, euphoria, impulsivity, irritability, suicidal ideation, aggression |
| Syndromes |
| Anorexia nervosa, bipolar disorder, borderline personality disorder, major depressive disorder, seasonal affective disorder |
| Behaviors |
| Suicide and suicide attempts, violence |
| *Small studies have suggested possible relationships with dissociative and panic disorders |
Effects of lipid-lowering agents
If there is a causal relationship between low cholesterol and mood disorders, then it stands to reason that using cholesterol-lowering drugs would increase the risk of depression and suicide. However, the data do not support that conclusion.
Many case reports have documented adverse psychiatric reactions to statins, including depression, suicidality, emotional lability, agitation, irritability, anxiety, panic, and euphoria.17 In an early analysis of primary prevention trials, patients receiving cholesterol-lowering treatment—mainly non-statins—were estimated to have twice the risk of death by suicide or violence compared with controls.3 However, a more recent meta-analysis of larger clinical trials of lipid-lowering agents including statins and observational studies did not reveal an association between lipid-lowering medications and suicide.15,18
In a large case-control study, statin users had a lower risk of depression (adjusted odds ratio [OR] 0.4, 95% confidence interval [CI], 0.2 to 0.9) than patients taking non-statin lipid-lowering drugs (adjusted OR 1.0, 95% CI, 0.5 to 2.1).19 However, statins reduced cholesterol more (30% to 50%) than non-statin drugs (10% to 20%). A clinical trial of >1,000 patients with stable coronary artery disease treated with pravastatin—an HMG-CoA reductase inhibitor with low lipophilicity that is less likely than other statins to cross the blood-brain barrier—revealed no changes in self-reported anger, impulsiveness, anxiety, or depression.20
This study did not exclude patients with psychiatric illness—who are at greatest risk of suicide—but other trials of lipid-lowering drugs did.21 As a result, the effects of lipid-lowering medications on psychiatric patients are unclear. A clinical trial is underway to assess the effects of pravastatin (low lipophilicity), simvastatin (high lipophilicity), or placebo on mood, sleep, and aggression.21
Low cholesterol: State or trait?
Much of the research linking low cholesterol, mood disorders, and suicidality could be confounded by depressed mood leading to reduced serum cholesterol. There has been considerable debate about whether low cholesterol predisposes patients to suicide or if depression independently leads to poor nutrition and therefore low cholesterol and increased suicide risk.6,22
Some researchers have suggested that depression lowers cholesterol and increases risk of suicide,23 but study designs have limited the ability to discern the directionality of the relationship. Attempts to control for depression-related malnutrition and weight loss—which lowers total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C)24—suggest the association may be independent of these variables.25-27 These findings suggest that cholesterol may be considered a trait marker and is not entirely state-dependent. However, multiple, large, long-term randomized controlled trials have not shown increased depression and suicide with use of lipid-lowering agents in healthy populations.20
The Figure illustrates known epidemiologic associations of low cholesterol, low serotoninergic function, and suicide and contrasts conceptual models of cholesterol as a state and a trait marker. A case can be made for cholesterol as both a state and a trait marker, and these models could overlap, with depression-induced decreases in cholesterol further mediating changes in serotonergic function and related behavioral sequelae.
Figure
Cholesterol, depression, and suicide: How are they linked? 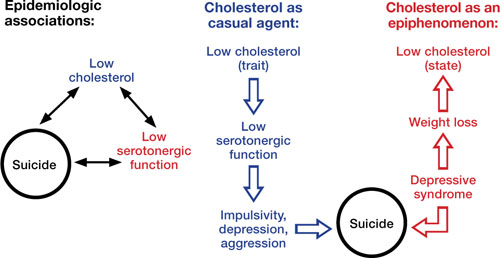
Low cholesterol may be considered a trait marker, predisposing patients to lower serotonergic function and placing them at greater risk for impulsivity, depression, aggression, and suicide. Other models suggest that lower cholesterol is a state-dependent consequence of depression, and not part of a causal chain toward suicide
Improving cardiac health
Limited epidemiologic studies suggest that patients with mood disorders may have lower levels of total cholesterol and LDL-C, but higher rates of hypertriglyceridemia compared with the general population.8 Unfortunately, psychiatric patients—who may be at increased risk of developing cardiovascular disease—may be less likely to be screened and appropriately treated for lipid abnormalities.28 To address this disparity, consider assuming an active role in assessing and managing hyperlipidemia in your patients with mood disorders. Be aware of your patients’ lipid profile and ensure that they follow monitoring recommendations.
The National Cholesterol Education Program recommends screening all adults age >20 for hyperlipidemia every 5 years using measures of total cholesterol, LDL-C, HDL-C, and triglycerides. If LDL-C or triglycerides exceed target values (Table 2), appropriate management includes recommending lifestyle changes and pharmacotherapy (Box 2).
Patients should receive a fasting lipid profile before and 12 weeks after starting any antipsychotic and semiannually thereafter.29 Consider closely monitoring lipids when patients gain weight with psychotropics. Refer patients with hyperlipidemia to a primary care physician, but in the absence of such a provider, mental health clinicians who are familiar with treatment guidelines can manage these patients.30
Closely monitor individuals with mood disorders for changes in behavior or mental status after starting a lipid-lowering agent. Consider discontinuing the drug if a patient develops an adverse reaction. If symptoms return after medication rechallenge, consider other management strategies such as an alternate lipid-lowering agent or re-emphasizing behavioral measures.
Table 2
National Cholesterol Education Program recommended LDL levels
| Risk category* | LDL goal | When to consider medications |
|---|---|---|
| CHD or CHD equivalent | <100 mg/dL | ≥130 mg/dL |
| ≥2 major risk factors | <130 mg/dL | ≥130 to 160 mg/dL (based on 10-year risk) |
| 0 or 1 risk factor | <160 mg/dL | ≥190 mg/dL |
| CHD: coronary heart disease; HDL: high-density lipoprotein; LDL: low-density lipoprotein | ||
| *Risk category is based on the presence of CHD or equivalent and major risk factors for CHD. CHD equivalents include symptomatic carotid artery disease, peripheral artery disease, and abdominal aortic aneurysm. Major risk factors include smoking, hypertension, low HDL, family history, and age. LDL levels to consider medications for those with ≥2 major risk factors vary by 10-year CHD risk | ||
| Source: National Cholesterol Education Program, Adult Treatment Panel III (ATP III) Quick Desk Reference. www.nhlbi.nih.gov/guidelines/cholesterol/atglance.htm | ||
National Cholesterol Education Program guidelines state that when a patient’s low-density lipoprotein cholesterol (LDL-C) exceeds targets (Table 2), first recommend lifestyle changes such as a diet low in saturated fat (<7% of calories) and cholesterol (<200 mg/d), weight management, and exercise. Increases in soluble fiber (10 to 25 g/d) and plant stanols/sterols also may be considered. If LDL-C levels are still too high, pharmacologic therapy such as an HMGCoA reductase inhibitor is suggested.
Treatment of elevated triglycerides (≥150 mg/dL) includes reaching the target LDL-C, intensifying a weight management program, and increasing exercise. Address quitting smoking and limiting alcohol when indicated. If triglyceride levels are ≥200 mg/dL after the LDL-C target is reached, set a secondary goal of reaching a target non-high-density lipoprotein cholesterol (HDL-C) (non-HDL-C; total cholesterol minus HDL-C) 30 mg/dL greater than the LDL goal. This can be achieved by adding an LDL-lowering drug such as a statin, nicotinic acid, or ezetimibe. When triglycerides are ≥500 mg/dL, more aggressive intervention, such as with a fibrate, omega-3 fatty acids, very low-fat diets, and exercise, is required to prevent pancreatitis.
Source: National Heart Lung and Blood Institute. National Cholesterol Education Program. www.nhlbi.nih.gov/guidelines/cholesterol/index.htm
Related Resources
- Fiedorowicz JG, Coryell WH. Cholesterol and suicide attempts: a prospective study of depressed inpatients. Psychiatry Res. 2007;152(1):11-20.
- National Cholesterol Education Program, Adult Treatment Panel III (ATP III) Quick Desk Reference. www.nhlbi.nih.gov/guidelines/cholesterol/atglance.htm.
- Executive Summary of the third report of the national Cholesterol Education Program (nCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486-2497.
Drug Brand Names
- Ezetimibe • Zetia
- Pravastatin • Pravachol
- Simvastatin • Zocor
Acknowledgements
Dr. Fiedorowicz thanks Lois Warren and Miriam Weiner for their editorial assistance.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Fiedorowicz is supported by the national Institutes of Health (1K23MH083695-01A210), nARSAD, and the Institute for Clinical and Translational Science at the University of Iowa (3 UL1 RR024979-03S4). He has received support for participating in a colleague’s investigator-initiated project with Eli Lilly. Dr. Haynes’ research is supported by grants from the national Institutes of Health (nHLBI: HL58972 & HL14388; nCRR CTSA: 1UL1RR024979).
1. Osby U, Brandt L, Correia N, et al. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58(9):844-850.
2. Lindberg G, Råstam L, Gullberg B, et al. Low serum cholesterol concentration and short term mortality from injuries in men and women. BMJ. 1992;305(6848):277-279.
3. Muldoon MF, Manuck SB, Matthews KA. Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. BMJ. 1990;301(6747):309-314.
4. Neaton JD, Blackburn H, Jacobs D, et al. Serum cholesterol level and mortality findings for men screened in the Multiple Risk Factor Intervention Trial. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med. 1992;152(7):1490-1500.
5. Fiedorowicz JG, Coryell WH. Cholesterol and suicide attempts: a prospective study of depressed inpatients. Psychiatry Res. 2007;152(1):11-20.
6. Golomb BA. Cholesterol and violence: is there a connection? Ann Intern Med. 1998;128(6):478-487.
7. Pae CU, Kim JJ, Lee SJ, et al. Aberration of cholesterol level in first-onset bipolar I patients. J Affect Disord. 2004;83(1):79-82.
8. Fiedorowicz JG, Palagummi NM, Forman-Hoffman VL, et al. Elevated prevalence of obesity, metabolic syndrome, and cardiovascular risk factors in bipolar disorder. Ann Clin Psychiatry. 2008;20(3):131-137.
9. Chung KH, Tsai SY, Lee HC. Mood symptoms and serum lipids in acute phase of bipolar disorder in Taiwan. Psychiatry Clin Neurosci. 2007;61(4):428-433.
10. Jow GM, Yang TT, Chen CL. Leptin and cholesterol levels are low in major depressive disorder, but high in schizophrenia. J Affect Disord. 2006;90(1):21-27.
11. Sagud M, Mihaljevic-Peles A, Pivac N, et al. Platelet serotonin and serum lipids in psychotic mania. J Affect Disord. 2007;97(1-3):247-251.
12. Beasley CL, Honer WG, Bergmann K, et al. Reductions in cholesterol and synaptic markers in association cortex in mood disorders. Bipolar Disord. 2005;7(5):449-455.
13. Gabriel A. Changes in plasma cholesterol in mood disorder patients: does treatment make a difference? J Affect Disord. 2007;99(1-3):273-278.
14. Lalovic A, Levy E, Luheshi G, et al. Cholesterol content in brains of suicide completers. Int J Neuropsychopharmacol. 2007;10(2):159-166.
15. Lester D. Serum cholesterol levels and suicide: a meta-analysis. Suicide Life Threat Behav. 2002;32(3):333-346.
16. Coryell W, Schlesser M. Combined biological tests for suicide prediction. Psychiatry Res. 2007;150(2):187-191.
17. Tatley M, Savage R. Psychiatric adverse reactions with statins, fibrates and ezetimibe: implications for the use of lipid-lowering agents. Drug Saf. 2007;30(3):195-201.
18. Callréus T, Agerskov Andersen U, Hallas J, et al. Cardiovascular drugs and the risk of suicide: a nested case-control study. Eur J Clin Pharmacol. 2007;63(6):591-596.
19. Yang CC, Jick SS, Jick H. Lipid-lowering drugs and the risk of depression and suicidal behavior. Arch Intern Med. 2003;163(16):1926-1932.
20. Stewart RA, Sharples KJ, North FM, et al. Long-term assessment of psychological well-being in a randomized placebo-controlled trial of cholesterol reduction with pravastatin. The LIPID Study Investigators. Arch Intern Med. 2000;160(20):3144-3152.
21. Golomb BA, Criqui MH, White HL, et al. The UCSD Statin Study: a randomized controlled trial assessing the impact of statins on selected noncardiac outcomes. Control Clin Trials. 2004;25(2):178-202.
22. Fawcett J, Busch KA, Jacobs D, et al. Suicide: a four-pathway clinical-biochemical model. Annals N Y Acad Sci. 1997;836:288-301.
23. Law MR, Thompson SG, Wald NJ. Assessing possible hazards of reducing serum cholesterol. BMJ. 1994;308(6925):373-379.
24. Dattilo AM, Kris-Etherton PM. Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr. 1992;56(2):320-328.
25. Garland M, Hickey D, Corvin A, et al. Total serum cholesterol in relation to psychological correlates in parasuicide. Br J Psychiatry. 2000;177:77-83.
26. Golier JA, Marzuk PM, Leon AC, et al. Low serum cholesterol level and attempted suicide. Am J Psychiatry. 1995;152(3):419-423.
27. Kunugi H, Takei N, Aoki H, et al. Low serum cholesterol in suicide attempters. Biol Psychiatry. 1997;41(2):196-200.
28. Murray DP, Weiner M, Prabhakar M, et al. Mania and mortality: why the excess cardiovascular risk in bipolar disorder? Curr Psychiatry Rep. 2009;11(6):475-480.
29. Sernyak MJ. Implementation of monitoring and management guidelines for second-generation antipsychotics. J Clin Psychiatry. 2007;68(suppl 4):14-18.
30. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry. 2004;161(8):1334-1349.
Discuss this article at http://currentpsychiatry.blogspot.com/2010/07/cholesterol-mood-and-vascular-health.html#comments
A growing body of literature examining the putative links among cholesterol, mood disorders, and suicide has produced inconsistent findings and unclear clinical implications that may leave psychiatrists unsure of how to interpret the data. Understanding cholesterol’s role in mood disorders may be relevant to the 2 primary causes of excess deaths in patients with mood disorders: suicide and vascular disease.1
Plausible links
In the early 1990s several studies suggested a link between low cholesterol (<160 mg/dL) and unnatural deaths, including suicide.2-4 Follow-up studies confirmed associations between low cholesterol and suicide attempts, especially violent ones.5 These associations are compelling given the neurobiologic effects of cholesterol, such as a net reduction of serotonergic function (Box 1). Low cholesterol may predispose an individual to aggression, impulsivity, and violence (Table 1).6 Many studies have found that patients with mood disorders have lower cholesterol levels;7 however, other research suggests they are at increased risk of hyperlipidemia, typically hypertriglyceridemia rather than hypercholesterolemia.8
Depression. Several studies have shown an association between low cholesterol and depressive symptoms, although this finding has not been replicated in Asian subjects.9,10 Patients with manic or mixed syndromes have been found to have lower serum cholesterol,11 and individuals with major depression and bipolar disorder have lower cholesterol levels in the brain compared with healthy controls.12 Some studies have observed higher total cholesterol levels after patients receive pharmacotherapy for major depressive symptoms.13 These findings have led to speculation that low serum cholesterol in patients with mood disorders is partially a state-dependent effect of depressive illness.
Suicide. Cohort, case-control, and cross-sectional studies have linked low cholesterol to an increased risk of suicide.2,5 Individuals who attempt suicide by violent means have lower cholesterol compared with those who use less violent methods.5,14 A meta-analysis found statistically significant correlations between low cholesterol and future or past suicidal behavior; however, low cholesterol explained <0.01% of suicidal behavior.15 Studies comparing cholesterol levels of individuals following violent vs nonviolent suicide attempts have demonstrated stronger associations.15
Assessing suicide risk. Current evidence does not support considering low serum cholesterol a risk factor for suicide. One study used cholesterol as a clinical predictor of suicide,16 but this model has not been prospectively validated. As a whole, the evidence does not suggest that cholesterol levels explain a substantial portion of suicidal behaviors.
The neurobiologic effects of low cholesterol—particularly those related to serotonergic hypofunction—are thought to be mediate impulsive, aggressive, and violent behaviors that may predispose an individual to suicide.a,b The CNS contains one-fourth of the body’s free cholesterol,c which is synthesized primarily in situ.
Cholesterol improves membrane stability, reduces permeability, and may influence serotonergic function. Cholesterol depletion may impair function of 5-HT1A and 5-HT7 receptorsd,e and serotonin transporter activity.f Reduced cholesterol after treatment with simvastatin—an HMG-CoA reductase inhibitor that readily crosses the blood-brain barrier—resulted in acute (1-month) increases in serotonin transporter activity followed by subacute (>2 months) decreases.g Lower cholesterol levels may further decrease expression of serotonin receptors and cause a net reduction in serotonergic activity.
In addition, cholesterol is necessary for synapse formation and myelin production. Cholesterol depletion may have more diffuse effects on neurotransmission, such as gamma-aminobutyric acid receptors,hN-methyl-D-aspartate receptors,i opioid signaling,j and excitatory amino acids transport.k
Impulsivity associated with low serotonergic function and low total cholesterol has been suggested as a potential pathway for suicide.l Low cholesterol is associated with self-report measures of impulsivity;m however, increased impulsivity associated with lipid-lowering therapy may be temporary,n which is similar to the time-limited changes in serotonin transporter activity.g Human and animal data have suggested that low cholesterol may be linked to violent behaviors, including suicide.o
Source:
a. Vevera J, Fisar Z, Kvasnicka T, et al. Cholesterol-lowering therapy evokes time-limited changes in serotonergic transmission. Psychiatry Res. 2005;133(2-3):197-203.
b. Kaplan JR, Shively CA, Fontenot MB, et al. Demonstration of an association among dietary cholesterol, central serotonergic activity, and social behavior in monkeys. Psychosom Med. 1994;56(6):479-484.
c. Chattopadhyay A, Paila YD. Lipid-protein interactions, regulation and dysfunction of brain cholesterol. Biochem Biophys Res Commun. 2007;354(3):627-633.
d. Singh P, Paila YD, Chattopadhyay A. Differential effects of cholesterol and 7-dehydrocholesterol on the ligand binding activity of the hippocampal serotonin(1A) receptor: implications in SLOS. Biochem Biophys Res Commun. 2007;358(2):495-499.
e. Sjögren B, Hamblin MW, Svenningsson P. Cholesterol depletion reduces serotonin binding and signaling via human 5-HT(7(a)) receptors. Eur J Pharmacol. 2006;552(1-3):1-10.
f. Scanlon SM, Williams DC, Schloss P. Membrane cholesterol modulates serotonin transporter activity. Biochemistry. 2001;40(35):10507-10513.
g. Vevera J, Fisar Z, Kvasnicka T, et al. Cholesterol-lowering therapy evokes time-limited changes in serotonergic transmission. Psychiatry Res. 2005;133(2-3):197-203.
h. Sooksawate T, Simmonds MA. Effects of membrane cholesterol on the sensitivity of the GABA(A) receptor to GABA in acutely dissociated rat hippocampal neurones. Neuropharmacology. 2001;40(2):178-184.
i. Abulrob A, Tauskela JS, Mealing G, et al. Protection by cholesterol-extracting cyclodextrins: a role for N-methyl-daspartate receptor redistribution. J Neurochem. 2005;92(6):1477-1486.
j. Huang P, Xu W, Yoon SI, et al. Cholesterol reduction by methyl-beta-cyclodextrin attenuates the delta opioid receptor-mediated signaling in neuronal cells but enhances it in non-neuronal cells. Biochem Pharmacol. 2007;73(4):534-549.
k. Butchbach ME, Tian G, Guo H, et al. Association of excitatory amino acid transporters, especially EAAT2, with cholesterol-rich lipid raft microdomains: importance for excitatory amino acid transporter localization and function. J Biol Chem. 2004;279(33):34388-34396.
l. Fawcett J, Busch KA, Jacobs D, et al. Suicide: a four-pathway clinical-biochemical model. Annals N Y Acad Sci. 1997;836:288-301.
m. Garland M, Hickey D, Corvin A, et al. Total serum cholesterol in relation to psychological correlates in parasuicide. Br J Psychiatry. 2000;177:77-83.
n. Ormiston T, Wolkowitz OM, Reus VI, et al. Behavioral implications of lowering cholesterol levels: a double-blind pilot study. Psychosomatics. 2003;44(5):412-414.
o. Golomb BA. Cholesterol and violence: is there a connection? Ann Intern Med. 1998;128(6):478-487.
Table 1
Psychiatric features associated with low cholesterol*
| Symptoms |
| Anxiety, depressed mood, emotional lability, euphoria, impulsivity, irritability, suicidal ideation, aggression |
| Syndromes |
| Anorexia nervosa, bipolar disorder, borderline personality disorder, major depressive disorder, seasonal affective disorder |
| Behaviors |
| Suicide and suicide attempts, violence |
| *Small studies have suggested possible relationships with dissociative and panic disorders |
Effects of lipid-lowering agents
If there is a causal relationship between low cholesterol and mood disorders, then it stands to reason that using cholesterol-lowering drugs would increase the risk of depression and suicide. However, the data do not support that conclusion.
Many case reports have documented adverse psychiatric reactions to statins, including depression, suicidality, emotional lability, agitation, irritability, anxiety, panic, and euphoria.17 In an early analysis of primary prevention trials, patients receiving cholesterol-lowering treatment—mainly non-statins—were estimated to have twice the risk of death by suicide or violence compared with controls.3 However, a more recent meta-analysis of larger clinical trials of lipid-lowering agents including statins and observational studies did not reveal an association between lipid-lowering medications and suicide.15,18
In a large case-control study, statin users had a lower risk of depression (adjusted odds ratio [OR] 0.4, 95% confidence interval [CI], 0.2 to 0.9) than patients taking non-statin lipid-lowering drugs (adjusted OR 1.0, 95% CI, 0.5 to 2.1).19 However, statins reduced cholesterol more (30% to 50%) than non-statin drugs (10% to 20%). A clinical trial of >1,000 patients with stable coronary artery disease treated with pravastatin—an HMG-CoA reductase inhibitor with low lipophilicity that is less likely than other statins to cross the blood-brain barrier—revealed no changes in self-reported anger, impulsiveness, anxiety, or depression.20
This study did not exclude patients with psychiatric illness—who are at greatest risk of suicide—but other trials of lipid-lowering drugs did.21 As a result, the effects of lipid-lowering medications on psychiatric patients are unclear. A clinical trial is underway to assess the effects of pravastatin (low lipophilicity), simvastatin (high lipophilicity), or placebo on mood, sleep, and aggression.21
Low cholesterol: State or trait?
Much of the research linking low cholesterol, mood disorders, and suicidality could be confounded by depressed mood leading to reduced serum cholesterol. There has been considerable debate about whether low cholesterol predisposes patients to suicide or if depression independently leads to poor nutrition and therefore low cholesterol and increased suicide risk.6,22
Some researchers have suggested that depression lowers cholesterol and increases risk of suicide,23 but study designs have limited the ability to discern the directionality of the relationship. Attempts to control for depression-related malnutrition and weight loss—which lowers total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C)24—suggest the association may be independent of these variables.25-27 These findings suggest that cholesterol may be considered a trait marker and is not entirely state-dependent. However, multiple, large, long-term randomized controlled trials have not shown increased depression and suicide with use of lipid-lowering agents in healthy populations.20
The Figure illustrates known epidemiologic associations of low cholesterol, low serotoninergic function, and suicide and contrasts conceptual models of cholesterol as a state and a trait marker. A case can be made for cholesterol as both a state and a trait marker, and these models could overlap, with depression-induced decreases in cholesterol further mediating changes in serotonergic function and related behavioral sequelae.
Figure
Cholesterol, depression, and suicide: How are they linked? 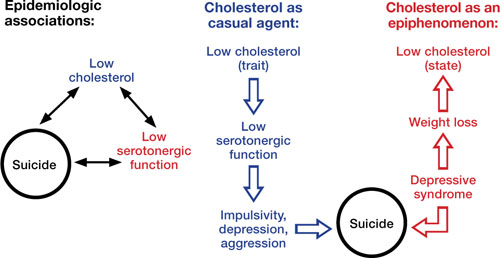
Low cholesterol may be considered a trait marker, predisposing patients to lower serotonergic function and placing them at greater risk for impulsivity, depression, aggression, and suicide. Other models suggest that lower cholesterol is a state-dependent consequence of depression, and not part of a causal chain toward suicide
Improving cardiac health
Limited epidemiologic studies suggest that patients with mood disorders may have lower levels of total cholesterol and LDL-C, but higher rates of hypertriglyceridemia compared with the general population.8 Unfortunately, psychiatric patients—who may be at increased risk of developing cardiovascular disease—may be less likely to be screened and appropriately treated for lipid abnormalities.28 To address this disparity, consider assuming an active role in assessing and managing hyperlipidemia in your patients with mood disorders. Be aware of your patients’ lipid profile and ensure that they follow monitoring recommendations.
The National Cholesterol Education Program recommends screening all adults age >20 for hyperlipidemia every 5 years using measures of total cholesterol, LDL-C, HDL-C, and triglycerides. If LDL-C or triglycerides exceed target values (Table 2), appropriate management includes recommending lifestyle changes and pharmacotherapy (Box 2).
Patients should receive a fasting lipid profile before and 12 weeks after starting any antipsychotic and semiannually thereafter.29 Consider closely monitoring lipids when patients gain weight with psychotropics. Refer patients with hyperlipidemia to a primary care physician, but in the absence of such a provider, mental health clinicians who are familiar with treatment guidelines can manage these patients.30
Closely monitor individuals with mood disorders for changes in behavior or mental status after starting a lipid-lowering agent. Consider discontinuing the drug if a patient develops an adverse reaction. If symptoms return after medication rechallenge, consider other management strategies such as an alternate lipid-lowering agent or re-emphasizing behavioral measures.
Table 2
National Cholesterol Education Program recommended LDL levels
| Risk category* | LDL goal | When to consider medications |
|---|---|---|
| CHD or CHD equivalent | <100 mg/dL | ≥130 mg/dL |
| ≥2 major risk factors | <130 mg/dL | ≥130 to 160 mg/dL (based on 10-year risk) |
| 0 or 1 risk factor | <160 mg/dL | ≥190 mg/dL |
| CHD: coronary heart disease; HDL: high-density lipoprotein; LDL: low-density lipoprotein | ||
| *Risk category is based on the presence of CHD or equivalent and major risk factors for CHD. CHD equivalents include symptomatic carotid artery disease, peripheral artery disease, and abdominal aortic aneurysm. Major risk factors include smoking, hypertension, low HDL, family history, and age. LDL levels to consider medications for those with ≥2 major risk factors vary by 10-year CHD risk | ||
| Source: National Cholesterol Education Program, Adult Treatment Panel III (ATP III) Quick Desk Reference. www.nhlbi.nih.gov/guidelines/cholesterol/atglance.htm | ||
National Cholesterol Education Program guidelines state that when a patient’s low-density lipoprotein cholesterol (LDL-C) exceeds targets (Table 2), first recommend lifestyle changes such as a diet low in saturated fat (<7% of calories) and cholesterol (<200 mg/d), weight management, and exercise. Increases in soluble fiber (10 to 25 g/d) and plant stanols/sterols also may be considered. If LDL-C levels are still too high, pharmacologic therapy such as an HMGCoA reductase inhibitor is suggested.
Treatment of elevated triglycerides (≥150 mg/dL) includes reaching the target LDL-C, intensifying a weight management program, and increasing exercise. Address quitting smoking and limiting alcohol when indicated. If triglyceride levels are ≥200 mg/dL after the LDL-C target is reached, set a secondary goal of reaching a target non-high-density lipoprotein cholesterol (HDL-C) (non-HDL-C; total cholesterol minus HDL-C) 30 mg/dL greater than the LDL goal. This can be achieved by adding an LDL-lowering drug such as a statin, nicotinic acid, or ezetimibe. When triglycerides are ≥500 mg/dL, more aggressive intervention, such as with a fibrate, omega-3 fatty acids, very low-fat diets, and exercise, is required to prevent pancreatitis.
Source: National Heart Lung and Blood Institute. National Cholesterol Education Program. www.nhlbi.nih.gov/guidelines/cholesterol/index.htm
Related Resources
- Fiedorowicz JG, Coryell WH. Cholesterol and suicide attempts: a prospective study of depressed inpatients. Psychiatry Res. 2007;152(1):11-20.
- National Cholesterol Education Program, Adult Treatment Panel III (ATP III) Quick Desk Reference. www.nhlbi.nih.gov/guidelines/cholesterol/atglance.htm.
- Executive Summary of the third report of the national Cholesterol Education Program (nCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486-2497.
Drug Brand Names
- Ezetimibe • Zetia
- Pravastatin • Pravachol
- Simvastatin • Zocor
Acknowledgements
Dr. Fiedorowicz thanks Lois Warren and Miriam Weiner for their editorial assistance.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Fiedorowicz is supported by the national Institutes of Health (1K23MH083695-01A210), nARSAD, and the Institute for Clinical and Translational Science at the University of Iowa (3 UL1 RR024979-03S4). He has received support for participating in a colleague’s investigator-initiated project with Eli Lilly. Dr. Haynes’ research is supported by grants from the national Institutes of Health (nHLBI: HL58972 & HL14388; nCRR CTSA: 1UL1RR024979).
Discuss this article at http://currentpsychiatry.blogspot.com/2010/07/cholesterol-mood-and-vascular-health.html#comments
A growing body of literature examining the putative links among cholesterol, mood disorders, and suicide has produced inconsistent findings and unclear clinical implications that may leave psychiatrists unsure of how to interpret the data. Understanding cholesterol’s role in mood disorders may be relevant to the 2 primary causes of excess deaths in patients with mood disorders: suicide and vascular disease.1
Plausible links
In the early 1990s several studies suggested a link between low cholesterol (<160 mg/dL) and unnatural deaths, including suicide.2-4 Follow-up studies confirmed associations between low cholesterol and suicide attempts, especially violent ones.5 These associations are compelling given the neurobiologic effects of cholesterol, such as a net reduction of serotonergic function (Box 1). Low cholesterol may predispose an individual to aggression, impulsivity, and violence (Table 1).6 Many studies have found that patients with mood disorders have lower cholesterol levels;7 however, other research suggests they are at increased risk of hyperlipidemia, typically hypertriglyceridemia rather than hypercholesterolemia.8
Depression. Several studies have shown an association between low cholesterol and depressive symptoms, although this finding has not been replicated in Asian subjects.9,10 Patients with manic or mixed syndromes have been found to have lower serum cholesterol,11 and individuals with major depression and bipolar disorder have lower cholesterol levels in the brain compared with healthy controls.12 Some studies have observed higher total cholesterol levels after patients receive pharmacotherapy for major depressive symptoms.13 These findings have led to speculation that low serum cholesterol in patients with mood disorders is partially a state-dependent effect of depressive illness.
Suicide. Cohort, case-control, and cross-sectional studies have linked low cholesterol to an increased risk of suicide.2,5 Individuals who attempt suicide by violent means have lower cholesterol compared with those who use less violent methods.5,14 A meta-analysis found statistically significant correlations between low cholesterol and future or past suicidal behavior; however, low cholesterol explained <0.01% of suicidal behavior.15 Studies comparing cholesterol levels of individuals following violent vs nonviolent suicide attempts have demonstrated stronger associations.15
Assessing suicide risk. Current evidence does not support considering low serum cholesterol a risk factor for suicide. One study used cholesterol as a clinical predictor of suicide,16 but this model has not been prospectively validated. As a whole, the evidence does not suggest that cholesterol levels explain a substantial portion of suicidal behaviors.
The neurobiologic effects of low cholesterol—particularly those related to serotonergic hypofunction—are thought to be mediate impulsive, aggressive, and violent behaviors that may predispose an individual to suicide.a,b The CNS contains one-fourth of the body’s free cholesterol,c which is synthesized primarily in situ.
Cholesterol improves membrane stability, reduces permeability, and may influence serotonergic function. Cholesterol depletion may impair function of 5-HT1A and 5-HT7 receptorsd,e and serotonin transporter activity.f Reduced cholesterol after treatment with simvastatin—an HMG-CoA reductase inhibitor that readily crosses the blood-brain barrier—resulted in acute (1-month) increases in serotonin transporter activity followed by subacute (>2 months) decreases.g Lower cholesterol levels may further decrease expression of serotonin receptors and cause a net reduction in serotonergic activity.
In addition, cholesterol is necessary for synapse formation and myelin production. Cholesterol depletion may have more diffuse effects on neurotransmission, such as gamma-aminobutyric acid receptors,hN-methyl-D-aspartate receptors,i opioid signaling,j and excitatory amino acids transport.k
Impulsivity associated with low serotonergic function and low total cholesterol has been suggested as a potential pathway for suicide.l Low cholesterol is associated with self-report measures of impulsivity;m however, increased impulsivity associated with lipid-lowering therapy may be temporary,n which is similar to the time-limited changes in serotonin transporter activity.g Human and animal data have suggested that low cholesterol may be linked to violent behaviors, including suicide.o
Source:
a. Vevera J, Fisar Z, Kvasnicka T, et al. Cholesterol-lowering therapy evokes time-limited changes in serotonergic transmission. Psychiatry Res. 2005;133(2-3):197-203.
b. Kaplan JR, Shively CA, Fontenot MB, et al. Demonstration of an association among dietary cholesterol, central serotonergic activity, and social behavior in monkeys. Psychosom Med. 1994;56(6):479-484.
c. Chattopadhyay A, Paila YD. Lipid-protein interactions, regulation and dysfunction of brain cholesterol. Biochem Biophys Res Commun. 2007;354(3):627-633.
d. Singh P, Paila YD, Chattopadhyay A. Differential effects of cholesterol and 7-dehydrocholesterol on the ligand binding activity of the hippocampal serotonin(1A) receptor: implications in SLOS. Biochem Biophys Res Commun. 2007;358(2):495-499.
e. Sjögren B, Hamblin MW, Svenningsson P. Cholesterol depletion reduces serotonin binding and signaling via human 5-HT(7(a)) receptors. Eur J Pharmacol. 2006;552(1-3):1-10.
f. Scanlon SM, Williams DC, Schloss P. Membrane cholesterol modulates serotonin transporter activity. Biochemistry. 2001;40(35):10507-10513.
g. Vevera J, Fisar Z, Kvasnicka T, et al. Cholesterol-lowering therapy evokes time-limited changes in serotonergic transmission. Psychiatry Res. 2005;133(2-3):197-203.
h. Sooksawate T, Simmonds MA. Effects of membrane cholesterol on the sensitivity of the GABA(A) receptor to GABA in acutely dissociated rat hippocampal neurones. Neuropharmacology. 2001;40(2):178-184.
i. Abulrob A, Tauskela JS, Mealing G, et al. Protection by cholesterol-extracting cyclodextrins: a role for N-methyl-daspartate receptor redistribution. J Neurochem. 2005;92(6):1477-1486.
j. Huang P, Xu W, Yoon SI, et al. Cholesterol reduction by methyl-beta-cyclodextrin attenuates the delta opioid receptor-mediated signaling in neuronal cells but enhances it in non-neuronal cells. Biochem Pharmacol. 2007;73(4):534-549.
k. Butchbach ME, Tian G, Guo H, et al. Association of excitatory amino acid transporters, especially EAAT2, with cholesterol-rich lipid raft microdomains: importance for excitatory amino acid transporter localization and function. J Biol Chem. 2004;279(33):34388-34396.
l. Fawcett J, Busch KA, Jacobs D, et al. Suicide: a four-pathway clinical-biochemical model. Annals N Y Acad Sci. 1997;836:288-301.
m. Garland M, Hickey D, Corvin A, et al. Total serum cholesterol in relation to psychological correlates in parasuicide. Br J Psychiatry. 2000;177:77-83.
n. Ormiston T, Wolkowitz OM, Reus VI, et al. Behavioral implications of lowering cholesterol levels: a double-blind pilot study. Psychosomatics. 2003;44(5):412-414.
o. Golomb BA. Cholesterol and violence: is there a connection? Ann Intern Med. 1998;128(6):478-487.
Table 1
Psychiatric features associated with low cholesterol*
| Symptoms |
| Anxiety, depressed mood, emotional lability, euphoria, impulsivity, irritability, suicidal ideation, aggression |
| Syndromes |
| Anorexia nervosa, bipolar disorder, borderline personality disorder, major depressive disorder, seasonal affective disorder |
| Behaviors |
| Suicide and suicide attempts, violence |
| *Small studies have suggested possible relationships with dissociative and panic disorders |
Effects of lipid-lowering agents
If there is a causal relationship between low cholesterol and mood disorders, then it stands to reason that using cholesterol-lowering drugs would increase the risk of depression and suicide. However, the data do not support that conclusion.
Many case reports have documented adverse psychiatric reactions to statins, including depression, suicidality, emotional lability, agitation, irritability, anxiety, panic, and euphoria.17 In an early analysis of primary prevention trials, patients receiving cholesterol-lowering treatment—mainly non-statins—were estimated to have twice the risk of death by suicide or violence compared with controls.3 However, a more recent meta-analysis of larger clinical trials of lipid-lowering agents including statins and observational studies did not reveal an association between lipid-lowering medications and suicide.15,18
In a large case-control study, statin users had a lower risk of depression (adjusted odds ratio [OR] 0.4, 95% confidence interval [CI], 0.2 to 0.9) than patients taking non-statin lipid-lowering drugs (adjusted OR 1.0, 95% CI, 0.5 to 2.1).19 However, statins reduced cholesterol more (30% to 50%) than non-statin drugs (10% to 20%). A clinical trial of >1,000 patients with stable coronary artery disease treated with pravastatin—an HMG-CoA reductase inhibitor with low lipophilicity that is less likely than other statins to cross the blood-brain barrier—revealed no changes in self-reported anger, impulsiveness, anxiety, or depression.20
This study did not exclude patients with psychiatric illness—who are at greatest risk of suicide—but other trials of lipid-lowering drugs did.21 As a result, the effects of lipid-lowering medications on psychiatric patients are unclear. A clinical trial is underway to assess the effects of pravastatin (low lipophilicity), simvastatin (high lipophilicity), or placebo on mood, sleep, and aggression.21
Low cholesterol: State or trait?
Much of the research linking low cholesterol, mood disorders, and suicidality could be confounded by depressed mood leading to reduced serum cholesterol. There has been considerable debate about whether low cholesterol predisposes patients to suicide or if depression independently leads to poor nutrition and therefore low cholesterol and increased suicide risk.6,22
Some researchers have suggested that depression lowers cholesterol and increases risk of suicide,23 but study designs have limited the ability to discern the directionality of the relationship. Attempts to control for depression-related malnutrition and weight loss—which lowers total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C)24—suggest the association may be independent of these variables.25-27 These findings suggest that cholesterol may be considered a trait marker and is not entirely state-dependent. However, multiple, large, long-term randomized controlled trials have not shown increased depression and suicide with use of lipid-lowering agents in healthy populations.20
The Figure illustrates known epidemiologic associations of low cholesterol, low serotoninergic function, and suicide and contrasts conceptual models of cholesterol as a state and a trait marker. A case can be made for cholesterol as both a state and a trait marker, and these models could overlap, with depression-induced decreases in cholesterol further mediating changes in serotonergic function and related behavioral sequelae.
Figure
Cholesterol, depression, and suicide: How are they linked? 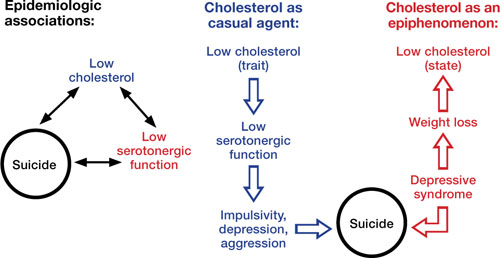
Low cholesterol may be considered a trait marker, predisposing patients to lower serotonergic function and placing them at greater risk for impulsivity, depression, aggression, and suicide. Other models suggest that lower cholesterol is a state-dependent consequence of depression, and not part of a causal chain toward suicide
Improving cardiac health
Limited epidemiologic studies suggest that patients with mood disorders may have lower levels of total cholesterol and LDL-C, but higher rates of hypertriglyceridemia compared with the general population.8 Unfortunately, psychiatric patients—who may be at increased risk of developing cardiovascular disease—may be less likely to be screened and appropriately treated for lipid abnormalities.28 To address this disparity, consider assuming an active role in assessing and managing hyperlipidemia in your patients with mood disorders. Be aware of your patients’ lipid profile and ensure that they follow monitoring recommendations.
The National Cholesterol Education Program recommends screening all adults age >20 for hyperlipidemia every 5 years using measures of total cholesterol, LDL-C, HDL-C, and triglycerides. If LDL-C or triglycerides exceed target values (Table 2), appropriate management includes recommending lifestyle changes and pharmacotherapy (Box 2).
Patients should receive a fasting lipid profile before and 12 weeks after starting any antipsychotic and semiannually thereafter.29 Consider closely monitoring lipids when patients gain weight with psychotropics. Refer patients with hyperlipidemia to a primary care physician, but in the absence of such a provider, mental health clinicians who are familiar with treatment guidelines can manage these patients.30
Closely monitor individuals with mood disorders for changes in behavior or mental status after starting a lipid-lowering agent. Consider discontinuing the drug if a patient develops an adverse reaction. If symptoms return after medication rechallenge, consider other management strategies such as an alternate lipid-lowering agent or re-emphasizing behavioral measures.
Table 2
National Cholesterol Education Program recommended LDL levels
| Risk category* | LDL goal | When to consider medications |
|---|---|---|
| CHD or CHD equivalent | <100 mg/dL | ≥130 mg/dL |
| ≥2 major risk factors | <130 mg/dL | ≥130 to 160 mg/dL (based on 10-year risk) |
| 0 or 1 risk factor | <160 mg/dL | ≥190 mg/dL |
| CHD: coronary heart disease; HDL: high-density lipoprotein; LDL: low-density lipoprotein | ||
| *Risk category is based on the presence of CHD or equivalent and major risk factors for CHD. CHD equivalents include symptomatic carotid artery disease, peripheral artery disease, and abdominal aortic aneurysm. Major risk factors include smoking, hypertension, low HDL, family history, and age. LDL levels to consider medications for those with ≥2 major risk factors vary by 10-year CHD risk | ||
| Source: National Cholesterol Education Program, Adult Treatment Panel III (ATP III) Quick Desk Reference. www.nhlbi.nih.gov/guidelines/cholesterol/atglance.htm | ||
National Cholesterol Education Program guidelines state that when a patient’s low-density lipoprotein cholesterol (LDL-C) exceeds targets (Table 2), first recommend lifestyle changes such as a diet low in saturated fat (<7% of calories) and cholesterol (<200 mg/d), weight management, and exercise. Increases in soluble fiber (10 to 25 g/d) and plant stanols/sterols also may be considered. If LDL-C levels are still too high, pharmacologic therapy such as an HMGCoA reductase inhibitor is suggested.
Treatment of elevated triglycerides (≥150 mg/dL) includes reaching the target LDL-C, intensifying a weight management program, and increasing exercise. Address quitting smoking and limiting alcohol when indicated. If triglyceride levels are ≥200 mg/dL after the LDL-C target is reached, set a secondary goal of reaching a target non-high-density lipoprotein cholesterol (HDL-C) (non-HDL-C; total cholesterol minus HDL-C) 30 mg/dL greater than the LDL goal. This can be achieved by adding an LDL-lowering drug such as a statin, nicotinic acid, or ezetimibe. When triglycerides are ≥500 mg/dL, more aggressive intervention, such as with a fibrate, omega-3 fatty acids, very low-fat diets, and exercise, is required to prevent pancreatitis.
Source: National Heart Lung and Blood Institute. National Cholesterol Education Program. www.nhlbi.nih.gov/guidelines/cholesterol/index.htm
Related Resources
- Fiedorowicz JG, Coryell WH. Cholesterol and suicide attempts: a prospective study of depressed inpatients. Psychiatry Res. 2007;152(1):11-20.
- National Cholesterol Education Program, Adult Treatment Panel III (ATP III) Quick Desk Reference. www.nhlbi.nih.gov/guidelines/cholesterol/atglance.htm.
- Executive Summary of the third report of the national Cholesterol Education Program (nCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486-2497.
Drug Brand Names
- Ezetimibe • Zetia
- Pravastatin • Pravachol
- Simvastatin • Zocor
Acknowledgements
Dr. Fiedorowicz thanks Lois Warren and Miriam Weiner for their editorial assistance.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Fiedorowicz is supported by the national Institutes of Health (1K23MH083695-01A210), nARSAD, and the Institute for Clinical and Translational Science at the University of Iowa (3 UL1 RR024979-03S4). He has received support for participating in a colleague’s investigator-initiated project with Eli Lilly. Dr. Haynes’ research is supported by grants from the national Institutes of Health (nHLBI: HL58972 & HL14388; nCRR CTSA: 1UL1RR024979).
1. Osby U, Brandt L, Correia N, et al. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58(9):844-850.
2. Lindberg G, Råstam L, Gullberg B, et al. Low serum cholesterol concentration and short term mortality from injuries in men and women. BMJ. 1992;305(6848):277-279.
3. Muldoon MF, Manuck SB, Matthews KA. Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. BMJ. 1990;301(6747):309-314.
4. Neaton JD, Blackburn H, Jacobs D, et al. Serum cholesterol level and mortality findings for men screened in the Multiple Risk Factor Intervention Trial. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med. 1992;152(7):1490-1500.
5. Fiedorowicz JG, Coryell WH. Cholesterol and suicide attempts: a prospective study of depressed inpatients. Psychiatry Res. 2007;152(1):11-20.
6. Golomb BA. Cholesterol and violence: is there a connection? Ann Intern Med. 1998;128(6):478-487.
7. Pae CU, Kim JJ, Lee SJ, et al. Aberration of cholesterol level in first-onset bipolar I patients. J Affect Disord. 2004;83(1):79-82.
8. Fiedorowicz JG, Palagummi NM, Forman-Hoffman VL, et al. Elevated prevalence of obesity, metabolic syndrome, and cardiovascular risk factors in bipolar disorder. Ann Clin Psychiatry. 2008;20(3):131-137.
9. Chung KH, Tsai SY, Lee HC. Mood symptoms and serum lipids in acute phase of bipolar disorder in Taiwan. Psychiatry Clin Neurosci. 2007;61(4):428-433.
10. Jow GM, Yang TT, Chen CL. Leptin and cholesterol levels are low in major depressive disorder, but high in schizophrenia. J Affect Disord. 2006;90(1):21-27.
11. Sagud M, Mihaljevic-Peles A, Pivac N, et al. Platelet serotonin and serum lipids in psychotic mania. J Affect Disord. 2007;97(1-3):247-251.
12. Beasley CL, Honer WG, Bergmann K, et al. Reductions in cholesterol and synaptic markers in association cortex in mood disorders. Bipolar Disord. 2005;7(5):449-455.
13. Gabriel A. Changes in plasma cholesterol in mood disorder patients: does treatment make a difference? J Affect Disord. 2007;99(1-3):273-278.
14. Lalovic A, Levy E, Luheshi G, et al. Cholesterol content in brains of suicide completers. Int J Neuropsychopharmacol. 2007;10(2):159-166.
15. Lester D. Serum cholesterol levels and suicide: a meta-analysis. Suicide Life Threat Behav. 2002;32(3):333-346.
16. Coryell W, Schlesser M. Combined biological tests for suicide prediction. Psychiatry Res. 2007;150(2):187-191.
17. Tatley M, Savage R. Psychiatric adverse reactions with statins, fibrates and ezetimibe: implications for the use of lipid-lowering agents. Drug Saf. 2007;30(3):195-201.
18. Callréus T, Agerskov Andersen U, Hallas J, et al. Cardiovascular drugs and the risk of suicide: a nested case-control study. Eur J Clin Pharmacol. 2007;63(6):591-596.
19. Yang CC, Jick SS, Jick H. Lipid-lowering drugs and the risk of depression and suicidal behavior. Arch Intern Med. 2003;163(16):1926-1932.
20. Stewart RA, Sharples KJ, North FM, et al. Long-term assessment of psychological well-being in a randomized placebo-controlled trial of cholesterol reduction with pravastatin. The LIPID Study Investigators. Arch Intern Med. 2000;160(20):3144-3152.
21. Golomb BA, Criqui MH, White HL, et al. The UCSD Statin Study: a randomized controlled trial assessing the impact of statins on selected noncardiac outcomes. Control Clin Trials. 2004;25(2):178-202.
22. Fawcett J, Busch KA, Jacobs D, et al. Suicide: a four-pathway clinical-biochemical model. Annals N Y Acad Sci. 1997;836:288-301.
23. Law MR, Thompson SG, Wald NJ. Assessing possible hazards of reducing serum cholesterol. BMJ. 1994;308(6925):373-379.
24. Dattilo AM, Kris-Etherton PM. Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr. 1992;56(2):320-328.
25. Garland M, Hickey D, Corvin A, et al. Total serum cholesterol in relation to psychological correlates in parasuicide. Br J Psychiatry. 2000;177:77-83.
26. Golier JA, Marzuk PM, Leon AC, et al. Low serum cholesterol level and attempted suicide. Am J Psychiatry. 1995;152(3):419-423.
27. Kunugi H, Takei N, Aoki H, et al. Low serum cholesterol in suicide attempters. Biol Psychiatry. 1997;41(2):196-200.
28. Murray DP, Weiner M, Prabhakar M, et al. Mania and mortality: why the excess cardiovascular risk in bipolar disorder? Curr Psychiatry Rep. 2009;11(6):475-480.
29. Sernyak MJ. Implementation of monitoring and management guidelines for second-generation antipsychotics. J Clin Psychiatry. 2007;68(suppl 4):14-18.
30. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry. 2004;161(8):1334-1349.
1. Osby U, Brandt L, Correia N, et al. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58(9):844-850.
2. Lindberg G, Råstam L, Gullberg B, et al. Low serum cholesterol concentration and short term mortality from injuries in men and women. BMJ. 1992;305(6848):277-279.
3. Muldoon MF, Manuck SB, Matthews KA. Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. BMJ. 1990;301(6747):309-314.
4. Neaton JD, Blackburn H, Jacobs D, et al. Serum cholesterol level and mortality findings for men screened in the Multiple Risk Factor Intervention Trial. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med. 1992;152(7):1490-1500.
5. Fiedorowicz JG, Coryell WH. Cholesterol and suicide attempts: a prospective study of depressed inpatients. Psychiatry Res. 2007;152(1):11-20.
6. Golomb BA. Cholesterol and violence: is there a connection? Ann Intern Med. 1998;128(6):478-487.
7. Pae CU, Kim JJ, Lee SJ, et al. Aberration of cholesterol level in first-onset bipolar I patients. J Affect Disord. 2004;83(1):79-82.
8. Fiedorowicz JG, Palagummi NM, Forman-Hoffman VL, et al. Elevated prevalence of obesity, metabolic syndrome, and cardiovascular risk factors in bipolar disorder. Ann Clin Psychiatry. 2008;20(3):131-137.
9. Chung KH, Tsai SY, Lee HC. Mood symptoms and serum lipids in acute phase of bipolar disorder in Taiwan. Psychiatry Clin Neurosci. 2007;61(4):428-433.
10. Jow GM, Yang TT, Chen CL. Leptin and cholesterol levels are low in major depressive disorder, but high in schizophrenia. J Affect Disord. 2006;90(1):21-27.
11. Sagud M, Mihaljevic-Peles A, Pivac N, et al. Platelet serotonin and serum lipids in psychotic mania. J Affect Disord. 2007;97(1-3):247-251.
12. Beasley CL, Honer WG, Bergmann K, et al. Reductions in cholesterol and synaptic markers in association cortex in mood disorders. Bipolar Disord. 2005;7(5):449-455.
13. Gabriel A. Changes in plasma cholesterol in mood disorder patients: does treatment make a difference? J Affect Disord. 2007;99(1-3):273-278.
14. Lalovic A, Levy E, Luheshi G, et al. Cholesterol content in brains of suicide completers. Int J Neuropsychopharmacol. 2007;10(2):159-166.
15. Lester D. Serum cholesterol levels and suicide: a meta-analysis. Suicide Life Threat Behav. 2002;32(3):333-346.
16. Coryell W, Schlesser M. Combined biological tests for suicide prediction. Psychiatry Res. 2007;150(2):187-191.
17. Tatley M, Savage R. Psychiatric adverse reactions with statins, fibrates and ezetimibe: implications for the use of lipid-lowering agents. Drug Saf. 2007;30(3):195-201.
18. Callréus T, Agerskov Andersen U, Hallas J, et al. Cardiovascular drugs and the risk of suicide: a nested case-control study. Eur J Clin Pharmacol. 2007;63(6):591-596.
19. Yang CC, Jick SS, Jick H. Lipid-lowering drugs and the risk of depression and suicidal behavior. Arch Intern Med. 2003;163(16):1926-1932.
20. Stewart RA, Sharples KJ, North FM, et al. Long-term assessment of psychological well-being in a randomized placebo-controlled trial of cholesterol reduction with pravastatin. The LIPID Study Investigators. Arch Intern Med. 2000;160(20):3144-3152.
21. Golomb BA, Criqui MH, White HL, et al. The UCSD Statin Study: a randomized controlled trial assessing the impact of statins on selected noncardiac outcomes. Control Clin Trials. 2004;25(2):178-202.
22. Fawcett J, Busch KA, Jacobs D, et al. Suicide: a four-pathway clinical-biochemical model. Annals N Y Acad Sci. 1997;836:288-301.
23. Law MR, Thompson SG, Wald NJ. Assessing possible hazards of reducing serum cholesterol. BMJ. 1994;308(6925):373-379.
24. Dattilo AM, Kris-Etherton PM. Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr. 1992;56(2):320-328.
25. Garland M, Hickey D, Corvin A, et al. Total serum cholesterol in relation to psychological correlates in parasuicide. Br J Psychiatry. 2000;177:77-83.
26. Golier JA, Marzuk PM, Leon AC, et al. Low serum cholesterol level and attempted suicide. Am J Psychiatry. 1995;152(3):419-423.
27. Kunugi H, Takei N, Aoki H, et al. Low serum cholesterol in suicide attempters. Biol Psychiatry. 1997;41(2):196-200.
28. Murray DP, Weiner M, Prabhakar M, et al. Mania and mortality: why the excess cardiovascular risk in bipolar disorder? Curr Psychiatry Rep. 2009;11(6):475-480.
29. Sernyak MJ. Implementation of monitoring and management guidelines for second-generation antipsychotics. J Clin Psychiatry. 2007;68(suppl 4):14-18.
30. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry. 2004;161(8):1334-1349.