User login
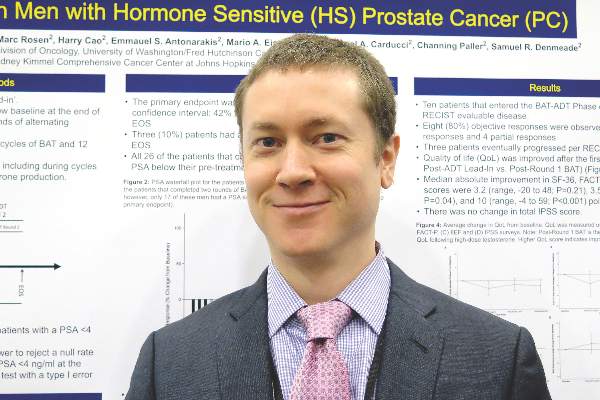
SAN FRANCISCO – Depriving hormone-sensitive prostate cancer of testosterone and then hitting it with a supraphysiologic dose keeps the disease under control and nets good quality of life, results of a phase II trial suggest.
With this alternating strategy, called bipolar androgen therapy, nearly 60% of men in the trial achieved a prostate-specific antigen level of less than 4 ng/mL after two rounds of therapy, first author Dr. Michael T. Schweizer reported at the Genitourinary Cancers Symposium. Moreover, men had improvements in quality of life after receiving the testosterone.
Many view androgen deprivation therapy (ADT) as the standard of care for such metastatic or biochemically recurrent disease, he explained in an interview. “In a sense, this is kind of analogous to forced intermittent androgen deprivation therapy, whereas instead of allowing testosterone levels to slowly recover, like is done in clinical practice, we administer high doses of testosterone.”
The prostate-specific antigen results achieved “are relatively comparable to what you see with prior intermittent androgen deprivation therapy studies. So this looks like it may be as good as intermittent therapy, and it has the added benefit of improved quality of life,” said Dr. Schweizer of the University of Washington and Fred Hutchinson Cancer Research Center, both in Seattle.
“This data is preliminary, and I don’t think it should be used to guide treatment. But we think that it’s promising enough as a justification for a future prospective study, ideally a randomized trial,” he added. “Additional studies should probably include additional biomarker assessments to see if we can discover predictors for response to this type of therapy.”
In a previous trial, Dr. Schweizer and his colleagues tested bipolar androgen therapy in men with castration-resistant disease, finding a paradoxical antitumor effect, with a high response rate and some patients staying on the therapy for more than a year (Sci Transl Med. 2015 Jan 7;7:269ra2).
The new trial was conducted among 33 men who had a biochemical recurrence only, or had metastatic disease with a low tumor burden, and had not received therapy for advanced disease with a second-line hormonal agent or ADT. Most had previously undergone radical prostatectomy, radiation therapy, or both.
During a 6-month lead-in phase, they received ADT. “The idea behind that was that would allow for the androgen receptor to adaptively up-regulate, one of the molecular events we think sensitizes cells to this form of therapy,” he explained at the symposium, sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Overall, 29 men achieved a prostate-specific antigen suppression to less than 4 ng/mL or a value at least 50% below their baseline value, and therefore went on to receive two rounds of bipolar androgen therapy: monthly injections of testosterone cypionate or testosterone enanthate for 3 months, followed by ADT for 3 months.
At the end of the study, 59% had a prostate-specific antigen level of less than 4 ng/mL, exceeding the trial’s prespecified value for success of 40% based on previous trials.
“It seemed like this therapy did quickly approximate the results of what you would expect from men with biochemical disease receiving intermittent androgen deprivation therapy,” Dr. Schweizer said. Among the 10 men who had RECIST-evaluable disease, 8 had a response to the therapy.
The patients also experienced an improvement in quality of life, going from the end of the lead-in phase to the end of the first round of testosterone. Specifically, they had median improvements in the Functional Assessment of Cancer Therapy-Prostate (FACT-P) (3.5 points, P = .04) and in the International Index of Erectile Function (IIEF) (10 points, P less than .001).
Among all 29 men receiving at least one dose of testosterone, 79% had an adverse event thought to be at least possibly related to the hormone, most commonly hot flashes (52%), edema (38%), and weight gain (14%), according to Dr. Schweizer, who disclosed that he had no relevant conflicts of interest. However, all events were grade 1 or 2 in severity.
SAN FRANCISCO – Depriving hormone-sensitive prostate cancer of testosterone and then hitting it with a supraphysiologic dose keeps the disease under control and nets good quality of life, results of a phase II trial suggest.
With this alternating strategy, called bipolar androgen therapy, nearly 60% of men in the trial achieved a prostate-specific antigen level of less than 4 ng/mL after two rounds of therapy, first author Dr. Michael T. Schweizer reported at the Genitourinary Cancers Symposium. Moreover, men had improvements in quality of life after receiving the testosterone.
Many view androgen deprivation therapy (ADT) as the standard of care for such metastatic or biochemically recurrent disease, he explained in an interview. “In a sense, this is kind of analogous to forced intermittent androgen deprivation therapy, whereas instead of allowing testosterone levels to slowly recover, like is done in clinical practice, we administer high doses of testosterone.”
The prostate-specific antigen results achieved “are relatively comparable to what you see with prior intermittent androgen deprivation therapy studies. So this looks like it may be as good as intermittent therapy, and it has the added benefit of improved quality of life,” said Dr. Schweizer of the University of Washington and Fred Hutchinson Cancer Research Center, both in Seattle.
“This data is preliminary, and I don’t think it should be used to guide treatment. But we think that it’s promising enough as a justification for a future prospective study, ideally a randomized trial,” he added. “Additional studies should probably include additional biomarker assessments to see if we can discover predictors for response to this type of therapy.”
In a previous trial, Dr. Schweizer and his colleagues tested bipolar androgen therapy in men with castration-resistant disease, finding a paradoxical antitumor effect, with a high response rate and some patients staying on the therapy for more than a year (Sci Transl Med. 2015 Jan 7;7:269ra2).
The new trial was conducted among 33 men who had a biochemical recurrence only, or had metastatic disease with a low tumor burden, and had not received therapy for advanced disease with a second-line hormonal agent or ADT. Most had previously undergone radical prostatectomy, radiation therapy, or both.
During a 6-month lead-in phase, they received ADT. “The idea behind that was that would allow for the androgen receptor to adaptively up-regulate, one of the molecular events we think sensitizes cells to this form of therapy,” he explained at the symposium, sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Overall, 29 men achieved a prostate-specific antigen suppression to less than 4 ng/mL or a value at least 50% below their baseline value, and therefore went on to receive two rounds of bipolar androgen therapy: monthly injections of testosterone cypionate or testosterone enanthate for 3 months, followed by ADT for 3 months.
At the end of the study, 59% had a prostate-specific antigen level of less than 4 ng/mL, exceeding the trial’s prespecified value for success of 40% based on previous trials.
“It seemed like this therapy did quickly approximate the results of what you would expect from men with biochemical disease receiving intermittent androgen deprivation therapy,” Dr. Schweizer said. Among the 10 men who had RECIST-evaluable disease, 8 had a response to the therapy.
The patients also experienced an improvement in quality of life, going from the end of the lead-in phase to the end of the first round of testosterone. Specifically, they had median improvements in the Functional Assessment of Cancer Therapy-Prostate (FACT-P) (3.5 points, P = .04) and in the International Index of Erectile Function (IIEF) (10 points, P less than .001).
Among all 29 men receiving at least one dose of testosterone, 79% had an adverse event thought to be at least possibly related to the hormone, most commonly hot flashes (52%), edema (38%), and weight gain (14%), according to Dr. Schweizer, who disclosed that he had no relevant conflicts of interest. However, all events were grade 1 or 2 in severity.
SAN FRANCISCO – Depriving hormone-sensitive prostate cancer of testosterone and then hitting it with a supraphysiologic dose keeps the disease under control and nets good quality of life, results of a phase II trial suggest.
With this alternating strategy, called bipolar androgen therapy, nearly 60% of men in the trial achieved a prostate-specific antigen level of less than 4 ng/mL after two rounds of therapy, first author Dr. Michael T. Schweizer reported at the Genitourinary Cancers Symposium. Moreover, men had improvements in quality of life after receiving the testosterone.
Many view androgen deprivation therapy (ADT) as the standard of care for such metastatic or biochemically recurrent disease, he explained in an interview. “In a sense, this is kind of analogous to forced intermittent androgen deprivation therapy, whereas instead of allowing testosterone levels to slowly recover, like is done in clinical practice, we administer high doses of testosterone.”
The prostate-specific antigen results achieved “are relatively comparable to what you see with prior intermittent androgen deprivation therapy studies. So this looks like it may be as good as intermittent therapy, and it has the added benefit of improved quality of life,” said Dr. Schweizer of the University of Washington and Fred Hutchinson Cancer Research Center, both in Seattle.
“This data is preliminary, and I don’t think it should be used to guide treatment. But we think that it’s promising enough as a justification for a future prospective study, ideally a randomized trial,” he added. “Additional studies should probably include additional biomarker assessments to see if we can discover predictors for response to this type of therapy.”
In a previous trial, Dr. Schweizer and his colleagues tested bipolar androgen therapy in men with castration-resistant disease, finding a paradoxical antitumor effect, with a high response rate and some patients staying on the therapy for more than a year (Sci Transl Med. 2015 Jan 7;7:269ra2).
The new trial was conducted among 33 men who had a biochemical recurrence only, or had metastatic disease with a low tumor burden, and had not received therapy for advanced disease with a second-line hormonal agent or ADT. Most had previously undergone radical prostatectomy, radiation therapy, or both.
During a 6-month lead-in phase, they received ADT. “The idea behind that was that would allow for the androgen receptor to adaptively up-regulate, one of the molecular events we think sensitizes cells to this form of therapy,” he explained at the symposium, sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Overall, 29 men achieved a prostate-specific antigen suppression to less than 4 ng/mL or a value at least 50% below their baseline value, and therefore went on to receive two rounds of bipolar androgen therapy: monthly injections of testosterone cypionate or testosterone enanthate for 3 months, followed by ADT for 3 months.
At the end of the study, 59% had a prostate-specific antigen level of less than 4 ng/mL, exceeding the trial’s prespecified value for success of 40% based on previous trials.
“It seemed like this therapy did quickly approximate the results of what you would expect from men with biochemical disease receiving intermittent androgen deprivation therapy,” Dr. Schweizer said. Among the 10 men who had RECIST-evaluable disease, 8 had a response to the therapy.
The patients also experienced an improvement in quality of life, going from the end of the lead-in phase to the end of the first round of testosterone. Specifically, they had median improvements in the Functional Assessment of Cancer Therapy-Prostate (FACT-P) (3.5 points, P = .04) and in the International Index of Erectile Function (IIEF) (10 points, P less than .001).
Among all 29 men receiving at least one dose of testosterone, 79% had an adverse event thought to be at least possibly related to the hormone, most commonly hot flashes (52%), edema (38%), and weight gain (14%), according to Dr. Schweizer, who disclosed that he had no relevant conflicts of interest. However, all events were grade 1 or 2 in severity.
AT THE GENITOURINARY CANCERS SYMPOSIUM
Key clinical point: Bipolar androgen therapy may be an effective, more tolerable alternative to intermittent ADT.
Major finding: Overall, 59% of patients achieved a prostate-specific antigen level of less than 4 ng/mL after two rounds of therapy.
Data source: A single-arm, single-institution phase II trial among 33 men with recurrent hormone-sensitive prostate cancer.
Disclosures: Dr. Schweizer disclosed that he had no relevant conflicts of interest.