User login
- Moderator Mickey Karram, MD, Director of Urogynecology, Good Samaritan Hospital, Cincinnati, and Professor of Obstetrics and Gynecology, University of Cincinnati.
- Matthew Barber, MD, MHS, Section of Urogynecology and Reconstructive Pelvic Surgery, Departments of Obstetrics & Gynecology and Urology, Cleveland Clinic, Cleveland.
- Alfred Bent, MD, Head, Division of Gynecology, Department of Obstetrics and Gynecology, Dalhousie University, IWK Health Center, Halifax, Nova Scotia.
- Geoffrey Cundiff, MD, Professor of Obstetrics and Gynecology, Johns Hopkins University, Baltimore.
Unfortunate but true: Many complications of pelvic surgery involve injury to the lower urinary tract—and many of these injuries go undetected and increase the patient’s risk of serious morbidity and the physician’s chances of being sued.
Even more unfortunate: These injuries are on the rise, thanks to the proliferation of anti-incontinence surgeries, greater use of laparoscopy, and the need for increasingly complex vaginal dissection.
Fortunately, most lower urinary tract injuries can be avoided, or at least detected early, and this discussion centers on techniques to accomplish those goals and ensure bladder integrity and ureteral patency.
The rising injury rate
There appear to be more injuries to the lower urinary tract arising from pelvic surgery. Why do you think that is?
BARBER: I think the increase is due to the increasing popularity of midurethral slings, such as the tension-free vaginal tape (TVT). With these blind retropubic procedures, the risk of bladder injury is approximately 5%, which is considerably higher than in most other procedures we perform.1
Fortunately, the negative consequences of placing the TVT trocar into the dome of the bladder are minimal, since the trocar can be removed and placed in the appropriate location without the need for bladder repair and without causing long-term bladder dysfunction.
KARRAM: The higher rate of injury also may be linked, in part, to greater use of energy sources during laparoscopic surgery. Over the past 2 years, we have seen numerous cases of delayed injury to the lower urinary tract or bowel secondary to thermal damage from energy devices including electrosurgical instruments and ultrasonic shears.
BARBER: I think there is an increase in lower urinary tract and ureteral injury because of the rising popularity of operative laparoscopy. Lower urinary tract injury is certainly more common with laparoscopic hysterectomy than with abdominal or vaginal hysterectomy.
Increase has no single cause
BENT: There may be a small increase overall in lower urinary tract injury during pelvic surgery, since we now do more procedures that require complicated vaginal dissection and exploration of tissue planes in close proximity to the ureters. This has increased the rate of ureteral injuries.
There also have been a few more urethral injuries, again related to tension-free suburethral slings, most often involving the transobturator approach.
KARRAM: The higher rate of cesarean sections also plays a role. Many women undergoing hysterectomies have had 1 or more cesarean deliveries. We recently completed a study that shows that cesarean section is an independent risk factor for cystotomy at the time of hysterectomy.2
Unfortunately, many surgeons still use aggressive blunt dissection when they attempt to mobilize the bladder off the uterus—whether a hysterectomy is being performed abdominally or vaginally. This can lead to inadvertent entry into the bladder. For this reason, sharp dissection should always be used.
CUNDIFF: Based on my reading of the literature, the incidence of operative injury to the lower urinary tract during gynecologic surgery in general has not changed noticeably since Samson reviewed the subject in 19023—although gynecologic surgery is the leading cause of such injuries and the leading cause of litigation against gynecologists.4
Most injuries involve hysterectomy
CUNDIFF: Most injuries occur during straightforward hysterectomies. Estimates of the prevalence of ureteral injury range from 0.4% to 2.4%.5-8 Since most studies estimating prevalence have not evaluated the lower urinary tract in the whole study population, they may underestimate true prevalence. However, a recent study by Vakili and colleagues9 included universal endoscopy of all patients undergoing hysterectomy and reported rates of ureteral injury (1.7%) and bladder injury (3.6%) similar to those of less rigorous studies.
Overall, the incidence of lower urinary tract injury during other types of urogynecologic surgery is higher than during hysterectomy. Evidence of the higher prevalence during urogynecologic surgery comes from several recent studies. Harris et al10 reported a 5.7% injury rate during reconstructive surgery for incontinence or prolapse. Importantly, 4% were unrecognized prior to urinary tract endoscopy.
Procedures most commonly associated with urinary tract injury were retropubic urethropexy and apical prolapse procedures using the uterosacral ligament in this series. This higher prevalence in urogynecologic procedures may explain the perceived increase in injuries overall.
How can a surgeon prevent bladder or ureteral injury during open hysterectomy?
BENT: Any procedure—regardless of the approach—demands careful dissection, good lighting, and exposure of appropriate structures. It is hard to avoid what you cannot see!
CUNDIFF: When I enter the peritoneal cavity, especially in patients undergoing reoperation, I make the incision more superiorly and avoid the bladder when extending the incision inferiorly. I always open the pararectal space and identify the ureters to ensure their safety during clamping.
Dissection of the vesicovaginal space is most effective when it is done sharply with adequate traction and countertraction. This can be achieved by gently pulling the bladder anteriorly with a Babcock clamp, using scissors to dissect close to the cervix.
For very large fundi, dissection of the vesicovaginal space can be difficult if the uterus is brought through the laparotomy. In these cases I generally take the round ligaments and infundibulopelvic ligaments first and then push the fundus into the upper abdomen. This helps keep the bowel out of the field and gives better visualization of the vesicovaginal space.
I generally enter the anterior fornix with a scalpel and then use Jorgensen scissors to excise the cervix. This helps protect the bladder, and also maximizes vaginal length.
By the way, I use a modified lithotomy position with universal stirrups to maintain access to the bladder for cystoscopy, in case it is needed later.
Follow the ureter
BARBER: During abdominal hysterectomy, I routinely identify the course of the ureter in the retroperitoneum and follow it from where it enters the pelvis until it disappears into the cardinal ligament and below the uterine artery. Following its course helps me avoid ureteral injury.
BENT: If there is scarring of the tube or ovary, or a mass is present, the ureter may have to be localized and dissected completely free of the adnexal structures before any clamps are placed. In addition, the bladder flap should routinely be mobilized using sharp dissection, never blunt dissection.
Mobilization of the bladder downward also pushes the ureters further out of the way during clamping of the uterine vessels. If bleeding occurs, secure hemostasis after observing the location of the ureters. If there is any concern about injury, cystoscopy with injected dye is required.
Next, as the uterosacral and cardinal ligaments are approached, the bladder must be reflected well inferior to this area. This will keep the ureters somewhat removed from the clamps.
Other tricks include performing intrafascial hysterectomy, in which the fascia is peeled away from the uterus and cervix, protecting the ureters.
Clamps placed across the cardinal and uterosacral ligament complexes must hug the uterus and roll off the cervix to protect the ureter.
When the cuff is sutured after removal of the uterus, clear planes of vagina must be seen anteriorly and posteriorly to avoid suturing the bladder into the vaginal cuff.
3 preventive strategies
KARRAM: For abdominal hysterectomy, I recommend 3 techniques:
- Skeletonize the infundibulopelvic ligament. Most surgeons do this routinely during the abdominal approach; I also recommend it for laparoscopic hysterectomy. Once there is a window in the broad ligament and the infundibulopelvic ligament is skeletonized, one can be sure the ureter is well below this area and probably out of harm’s way.
- Use sharp dissection to mobilize the bladder off the anterior cervix.
- Maintain awareness of the close proximity of the lower ureter to the uterosacral cardinal ligament. As the ureter enters the bladder, it can be as close as 1 cm lateral to the uterosacral ligament. This is an area where it is almost impossible to dissect out the ureter, so the surgeon needs to appreciate this anatomy and refrain from taking aggressive bites in the lateral direction when supporting or closing the vaginal cuff.
How can a surgeon prevent bladder or ureteral injury during laparoscopic hysterectomy?
BARBER: I think the ureter is best identified by direct visualization transperitoneally. The angle of the laparoscope makes visualizing the ureter much easier than from an abdominal approach, so retroperitoneal dissection is not necessary as often.
If the course of the ureter is not readily identified by direct transperitoneal visualization, a peritoneal incision can be made below and parallel to the infundibulopelvic ligament, which allows entry into the retroperitoneum and, typically, easy visualization of the ureter throughout its course.
Alternatively, the retroperitoneum can be entered lateral to the infundibulopelvic ligament, and the ureter can be identified in the same manner as in abdominal hysterectomy.
If laparoscopically assisted hysterectomy is planned, I prefer to dissect the bladder flap vaginally rather than laparoscopically, as the risk of bladder injury is considerably lower from a vaginal approach than it is laparoscopically. Obviously, if a total laparoscopic hysterectomy is necessary because of poor vaginal access, laparoscopic bladder flap dissection is necessary. In this case, I again favor sharp dissection and minimal use of cautery to avoid bladder injury.
How can a surgeon prevent bladder or ureteral injury during vaginal hysterectomy?
BENT: Traditional methods in which each clamp is rolled off the cervix or uterus until the procedure is completed help keep unsuspecting surgeons out of the bladder and away from the ureter. The only risk involves bladder mobilization (ie, creation of the bladder flap), which should always be done sharply to prevent bladder perforation. Avoid blunt finger or sponge-stick dissection! Knowing how to sharply dissect the bladder flap is vital—then even cases of prior cesarean section are manageable.
Salpingo-oophorectomy can also proceed under direct vision. Avoid the ureter by making sure the clamp closes only over the pedicles of the tube and ovary, with no intervening tissues in the clamp. If space is very tight, divide the round ligament and take the pedicle in a smaller bite. Traction on the cervix during the procedure, and mobilization of the bladder, allow the ureters to slide upward, well out of harm’s way, as the procedure progresses.
The importance of sharp dissection
BARBER: During vaginal hysterectomy, I usually have the operative assistant hold the cervical tenaculum so that there is tension on the uterus. I then use forceps to elevate the bladder directly vertically in order to place the bladder fibers on tension. Next, I dissect the bladder off the cervix and lower uterine segment using sharp dissection, and identify the peritoneum by direct finger palpation. Almost always, it is smooth and slippery.
After identifying the peritoneum, I grasp it with a tonsil clamp and elevate it so that it can be entered easily with scissors. I always confirm peritoneal entry by visualizing and identifying intraperitoneal structures such as bowel fat, the uterine serosal surface, or adnexae.
Some people advocate palpating the ureter during vaginal cases.
CUNDIFF: The most common time of injury during vaginal hysterectomy is during dissection of the vesicovaginal space; and suture ligation of the infundibulopelvic ligaments and uterine arteries carries the greatest potential for ureteral injury.
During vaginal hysterectomy, I try to dissect the vesicovaginal space early. I use a Deever retractor to retract the bladder anteriorly, maximizing my ability to sharply dissect close to the cervix until entering the peritoneal cavity. Once I’m in the peritoneal cavity, I advance the Deever retractor to protect the bladder through the rest of the procedure. I maximize protection of the ureters by applying downward traction on the cervix during vaginal clamp placement.
KARRAM: I agree. Never try to enter the anterior cul-de-sac until the vesicouterine space has been identified and is easily palpated. Rushing to enter the anterior cul-de-sac will only lead to inadvertent cystotomy.
Assessing ureteral patency
After what pelvic surgeries do you think ureteral patency should be assessed, and how should it be accomplished?
CUNDIFF: The literature contains several studies10-13 that involved universal endoscopy of the lower urinary tract. These studies demonstrate that most injuries are not recognized by the surgeon prior to endoscopy. In fact, the vast majority of injuries occur after straightforward hysterectomies. This may be due in part to the sheer volume of hysterectomies, compared with other pelvic surgeries. However, it also shows that, when lower urinary tract evaluation is performed solely when the surgeon suspects an injury, a substantial proportion of injuries are missed.
KARRAM: When do you assess ureteral patency?
CUNDIFF: My personal practice is to evaluate it in all cases that carry the potential for injury to the ureter. The complexity of the evaluation is proportional to the probability of ureteral injury.
For all laparotomies and laparoscopies, I identify the course of the ureter and confirm peristalsis. In the simplest of cases, this can be done by identifying the ureter beneath the peritoneum as it crosses the pelvic brim and courses across the pelvic sidewall. More frequently, it involves opening the pararectal space to identify the course of the ureter. In the most complex cases, it requires ureterolysis.
I strongly believe that identifying the ureter during any dissection that endangers it is the best way to avoid injury. Even after these precautions, I frequently perform cystoscopy with intravenous indigo carmine to confirm ureteral patency. This is my standard approach with all vaginal procedures, as I am not confident that I can palpate the course of the ureter.
Postoperative cystoscopy is virtually without morbidity and adds no more than 3 minutes to the procedure when properly planned. It also affords an excellent opportunity to train residents in cystoscopy.
How to assess patency after selected procedures
BENT: Ureteral patency should be assured after any repair of the pelvic floor.
After abdominal hysterectomy, if there is blood in the catheter bag or any difficulty has been encountered during surgery, I perform cystoscopy after injecting indigo carmine dye, to observe ureteral function.
At abdominal or laparoscopic sacrocolpopexy, I follow the path of the ureters over the pelvic brim and inferiorly to the adnexal area by direct inspection.
During abdominal or laparoscopic paravaginal repair, the Burch procedure, or uterosacral ligament suspension, I perform cystoscopy after tying sutures and injecting indigo carmine to ensure ureteral function.
To safeguard the ureter, follow its course
Vaginal hysterectomy is not usually associated with ureteral injury, and very uncommonly with bladder injury. However, if bladder injury is observed or the procedure has been difficult, it is wise to perform cystoscopy with dye injection. This also extends to traditional cystocele repair.
I also recommend cystoscopy with dye injection any time there is a vaginal approach to paravaginal defect repair, vault suspension, or colpocleisis.
Cystoscopy—safe, simple, and efficient
KARRAM: For vaginal surgery, I think cystoscopy is the simplest way to assess the lower urinary tract. I routinely use it after any procedures involving the posterior cul-de-sac such as McCall culdoplasty or vaginal vault suspension from the uterosacral ligaments. I also use it routinely after advanced prolapse repairs involving anterior colporrhaphy, as well as paravaginal defect repairs, and I certainly use it routinely after any lower urinary tract reconstructive procedures such as fistula repairs.
As for laparoscopic surgery, I think cystoscopy is again the most efficient way to assess the lower urinary tract. I do so after any retropubic suspension, be it a Burch colposuspension or a paravaginal repair, any type of vault suspension or sacrocolpopexy, and any type of hysterectomy or adnexectomy that involves dissection of the retroperitoneal space. I also do so if an energy source was used extensively in the vicinity of the retroperitoneal space on either side.
After abdominal surgery, it is probably more efficient (assuming the patient is not in stirrups) to perform a high extraperitoneal cystotomy or suprapubic telescopy. The indications are any difficult dissection in which I have concerns about ureteral patency, as well as any abdominal prolapse or anti-incontinence procedures.
Ureteral stenting
Is ureteral stenting ever indicated preoperatively? If so, when?
BARBER: I do not think ureteral stenting is indicated routinely for any procedure. There may be individual cases where a stent may help the surgeon avoid ureteral injury, but I can’t think of a procedure in which it should be routinely used.
CUNDIFF: I agree. Although ureteral stenting is an important tool for the pelvic floor surgeon to investigate potential ureteral obstruction, I think it has very limited value as a preoperative maneuver to avoid injury. My opinion is based on the following observations:
The surgeon cannot really assess the potential difficulty of identifying the course of the ureter until the peritoneal cavity is entered.
For the truly hostile pelvis, in which pelvic sidewall pathology prevents identification of the course of the ureter, I do not find that a stent facilitates dissection of the pararectal space and ureterolysis. In fact, it could increase the chance of ureteral injury by creating a backboard against which to cut it during dissection.
Any potential benefit of ureteral stents—which I believe is minimal—must be balanced against the potential risks, which include 20 to 30 minutes of added OR time and the risk of ureteral spasm or perforation.
BENT: I also agree that ureteral stenting is seldom helpful during gynecologic surgery. At laparotomy, direct dissection of the structures and exposure of the ureter are best; there is no need to feel for a ureter.
At laparoscopy, however, if there are large fibroids, scarring from endometriomas, or adnexal masses, then preoperative placement of lighted stents can help the surgeon identify the ureters during dissection. The case would still require dissection of the ureter away from the operative field, but the lighted path provides a starting point in this procedure.
For vaginal surgical procedures, it is easier to avoid the ureter. However, not all surgeons can palpate a nonstented ureter, which may be required during a high uterosacral ligament suspension. A stent can readily take the surgeon to the ureter and avoid injury in most cases. This may be helpful for less experienced operators.
What should residents be trained to do?
Do most obstetrics and gynecology residency programs appropriately train young physicians to evaluate and manage lower urinary tract injury during pelvic surgery?
CUNDIFF: I am afraid not. Although residency directors increasingly recognize the importance of educating doctors to prevent and manage these injuries, this recognition has not yet risen to the policy level.
For example, the Council on Resident Education in Obstetrics and Gynecology (CREOG) includes a bladder surgery educational model that necessitates dissection of the ureter, cystoscopy, ureteral stenting, bladder repair, and ureteral reanastomosis.
However, the CREOG surgical curriculum makes no mention of protecting or evaluating the lower urinary tract during pelvic surgery.
This spectrum seems to reflect the wide variation among residency programs, too. While some programs such as ours at Johns Hopkins provide comprehensive training in prevention, evaluation, and management of lower urinary tract injury, many others do not. This might be because some programs lack technically skilled faculty. Interdisciplinary politics also likely influences local credentialing.
BARBER: In my opinion, a graduating ObGyn resident should be able to:
- identify and mobilize the ureter to avoid injury during abdominal and laparoscopic surgery
- safely mobilize the bladder during abdominal, vaginal, or laparoscopic hysterectomy
- perform intraoperative cystoscopy to evaluate for injury
- repair bladder injuries abdominally and vaginally
However, I don’t think it is realistic for a graduating resident to be able to manage ureteral injuries, as residents are unlikely to encounter very many during training. These injuries are best left to our urology colleagues.
BENT: Very little or no education is provided in preventing lower urinary tract injury; evaluation is better managed in many programs. A conservative estimate is that 20% of programs have a reasonable curriculum for preoperative assessment and evaluation of incontinence and prolapse.
The management of pelvic floor disorders is better handled in almost all programs, especially as it relates to surgery. Many residents spend a lot of time on the urogynecology service and are exposed to the surgical aspect of rotations.
Dr. Karram and Dr. Barber have no financial relationships relevant to this article. Dr. Bent serves on the gynecology advisory board of ACMI and is a speaker for Novartis, Pfizer, Watson, and Asetellas (formerly Yamanouchi). He also has received research funding from Cook, Eli Lilly, and Mentor; and is a consultant for C.R. Bard. Dr. Cundiff has received grant/research support from Cook, is a consultant to C.R. Bard and Eli Lilly, and is a speaker for GlaxoSmithKline.
1. Karram MM, Segal JL, Vassallo BJ, Kleeman SD. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol 2003;101:929-932.
2. Rooney C, Crawford A, Vassaco B, Kleeman S, Karram M. Is cesarean section a risk factor for incidental cystotomy at the time of hysterectomy? Am J Obstet Gynecol. In press.
3. Samson JA. Ligation and clamping of the ureter as complications of surgical operations. Am Med. 1902;4:693.-
4. Wiskind AK, Thompson JD. Should cystoscopy be performed at every gynecologic operation to diagnose unsuspected ureteral injury? J Pelvic Surg. 1995;1:134-137.
5. St. Martin EC, et al. Ureteral injury in gynecologic surgery. J Urol. 1953;70:51-57.
6. Conger K, Beecham CT, Horrax TM. Ureteral injury in pelvic surgery: current thought on incidence, pathogenesis, prophylaxis and treatment. Obstet Gynecol. 1954;3:343-357.
7. Mann WJ, Arato M, Patsner B, et al. Ureteral injuries in an obstetrics and gynecology training program: etiology and management. Obstet Gynecol. 1988;72:82-85.
8. Stanhope CR, Wilson TO, Utz WJ, Smith LH, O’Brien PC. Suture entrapment and secondary ureteral obstruction. Am J Obstet Gynecol. 1991;164:1513-1519.
9. Vakili B, Chesson RR, Kyle BL, et al. The incidence of urinary tract injury during hysterectomy: a prospective analysis based on universal cystoscopy. Am J Obstet Gynecol. 2005;192:1599-1604.
10. Harris RL, Cundiff GW, Theofrastous JT, Yoon HW, Bump RC, Addison WA. The value of intraoperative cystoscopy in urogynecologic and reconstructive pelvic surgery. Am J Obstet Gynecol. 1997;177:1367-1369.
11. Gill EJ, Elser DM, Bonidie MJ, Roberts KM, Hurt WG. The routine use of cystoscopy with the Burch procedure. Am J Obstet Gynecol. 2002;186:1108.-
12. Kwon CH, Goldberg RO, Koduri S, Sand PK. The use of intraoperative cystoscopy in major vaginal and urogynecologic surgeries. Am J Obstet Gynecol. 2002;187:1466-1471; discussion 1471-1472.
13. Tulikangas PK, Weber AM, et al. Intraoperative cystoscopy in conjunction with anti-incontinence surgery. Obstet Gynecol. 2000;95(6 Pt 1):794-796.
- Moderator Mickey Karram, MD, Director of Urogynecology, Good Samaritan Hospital, Cincinnati, and Professor of Obstetrics and Gynecology, University of Cincinnati.
- Matthew Barber, MD, MHS, Section of Urogynecology and Reconstructive Pelvic Surgery, Departments of Obstetrics & Gynecology and Urology, Cleveland Clinic, Cleveland.
- Alfred Bent, MD, Head, Division of Gynecology, Department of Obstetrics and Gynecology, Dalhousie University, IWK Health Center, Halifax, Nova Scotia.
- Geoffrey Cundiff, MD, Professor of Obstetrics and Gynecology, Johns Hopkins University, Baltimore.
Unfortunate but true: Many complications of pelvic surgery involve injury to the lower urinary tract—and many of these injuries go undetected and increase the patient’s risk of serious morbidity and the physician’s chances of being sued.
Even more unfortunate: These injuries are on the rise, thanks to the proliferation of anti-incontinence surgeries, greater use of laparoscopy, and the need for increasingly complex vaginal dissection.
Fortunately, most lower urinary tract injuries can be avoided, or at least detected early, and this discussion centers on techniques to accomplish those goals and ensure bladder integrity and ureteral patency.
The rising injury rate
There appear to be more injuries to the lower urinary tract arising from pelvic surgery. Why do you think that is?
BARBER: I think the increase is due to the increasing popularity of midurethral slings, such as the tension-free vaginal tape (TVT). With these blind retropubic procedures, the risk of bladder injury is approximately 5%, which is considerably higher than in most other procedures we perform.1
Fortunately, the negative consequences of placing the TVT trocar into the dome of the bladder are minimal, since the trocar can be removed and placed in the appropriate location without the need for bladder repair and without causing long-term bladder dysfunction.
KARRAM: The higher rate of injury also may be linked, in part, to greater use of energy sources during laparoscopic surgery. Over the past 2 years, we have seen numerous cases of delayed injury to the lower urinary tract or bowel secondary to thermal damage from energy devices including electrosurgical instruments and ultrasonic shears.
BARBER: I think there is an increase in lower urinary tract and ureteral injury because of the rising popularity of operative laparoscopy. Lower urinary tract injury is certainly more common with laparoscopic hysterectomy than with abdominal or vaginal hysterectomy.
Increase has no single cause
BENT: There may be a small increase overall in lower urinary tract injury during pelvic surgery, since we now do more procedures that require complicated vaginal dissection and exploration of tissue planes in close proximity to the ureters. This has increased the rate of ureteral injuries.
There also have been a few more urethral injuries, again related to tension-free suburethral slings, most often involving the transobturator approach.
KARRAM: The higher rate of cesarean sections also plays a role. Many women undergoing hysterectomies have had 1 or more cesarean deliveries. We recently completed a study that shows that cesarean section is an independent risk factor for cystotomy at the time of hysterectomy.2
Unfortunately, many surgeons still use aggressive blunt dissection when they attempt to mobilize the bladder off the uterus—whether a hysterectomy is being performed abdominally or vaginally. This can lead to inadvertent entry into the bladder. For this reason, sharp dissection should always be used.
CUNDIFF: Based on my reading of the literature, the incidence of operative injury to the lower urinary tract during gynecologic surgery in general has not changed noticeably since Samson reviewed the subject in 19023—although gynecologic surgery is the leading cause of such injuries and the leading cause of litigation against gynecologists.4
Most injuries involve hysterectomy
CUNDIFF: Most injuries occur during straightforward hysterectomies. Estimates of the prevalence of ureteral injury range from 0.4% to 2.4%.5-8 Since most studies estimating prevalence have not evaluated the lower urinary tract in the whole study population, they may underestimate true prevalence. However, a recent study by Vakili and colleagues9 included universal endoscopy of all patients undergoing hysterectomy and reported rates of ureteral injury (1.7%) and bladder injury (3.6%) similar to those of less rigorous studies.
Overall, the incidence of lower urinary tract injury during other types of urogynecologic surgery is higher than during hysterectomy. Evidence of the higher prevalence during urogynecologic surgery comes from several recent studies. Harris et al10 reported a 5.7% injury rate during reconstructive surgery for incontinence or prolapse. Importantly, 4% were unrecognized prior to urinary tract endoscopy.
Procedures most commonly associated with urinary tract injury were retropubic urethropexy and apical prolapse procedures using the uterosacral ligament in this series. This higher prevalence in urogynecologic procedures may explain the perceived increase in injuries overall.
How can a surgeon prevent bladder or ureteral injury during open hysterectomy?
BENT: Any procedure—regardless of the approach—demands careful dissection, good lighting, and exposure of appropriate structures. It is hard to avoid what you cannot see!
CUNDIFF: When I enter the peritoneal cavity, especially in patients undergoing reoperation, I make the incision more superiorly and avoid the bladder when extending the incision inferiorly. I always open the pararectal space and identify the ureters to ensure their safety during clamping.
Dissection of the vesicovaginal space is most effective when it is done sharply with adequate traction and countertraction. This can be achieved by gently pulling the bladder anteriorly with a Babcock clamp, using scissors to dissect close to the cervix.
For very large fundi, dissection of the vesicovaginal space can be difficult if the uterus is brought through the laparotomy. In these cases I generally take the round ligaments and infundibulopelvic ligaments first and then push the fundus into the upper abdomen. This helps keep the bowel out of the field and gives better visualization of the vesicovaginal space.
I generally enter the anterior fornix with a scalpel and then use Jorgensen scissors to excise the cervix. This helps protect the bladder, and also maximizes vaginal length.
By the way, I use a modified lithotomy position with universal stirrups to maintain access to the bladder for cystoscopy, in case it is needed later.
Follow the ureter
BARBER: During abdominal hysterectomy, I routinely identify the course of the ureter in the retroperitoneum and follow it from where it enters the pelvis until it disappears into the cardinal ligament and below the uterine artery. Following its course helps me avoid ureteral injury.
BENT: If there is scarring of the tube or ovary, or a mass is present, the ureter may have to be localized and dissected completely free of the adnexal structures before any clamps are placed. In addition, the bladder flap should routinely be mobilized using sharp dissection, never blunt dissection.
Mobilization of the bladder downward also pushes the ureters further out of the way during clamping of the uterine vessels. If bleeding occurs, secure hemostasis after observing the location of the ureters. If there is any concern about injury, cystoscopy with injected dye is required.
Next, as the uterosacral and cardinal ligaments are approached, the bladder must be reflected well inferior to this area. This will keep the ureters somewhat removed from the clamps.
Other tricks include performing intrafascial hysterectomy, in which the fascia is peeled away from the uterus and cervix, protecting the ureters.
Clamps placed across the cardinal and uterosacral ligament complexes must hug the uterus and roll off the cervix to protect the ureter.
When the cuff is sutured after removal of the uterus, clear planes of vagina must be seen anteriorly and posteriorly to avoid suturing the bladder into the vaginal cuff.
3 preventive strategies
KARRAM: For abdominal hysterectomy, I recommend 3 techniques:
- Skeletonize the infundibulopelvic ligament. Most surgeons do this routinely during the abdominal approach; I also recommend it for laparoscopic hysterectomy. Once there is a window in the broad ligament and the infundibulopelvic ligament is skeletonized, one can be sure the ureter is well below this area and probably out of harm’s way.
- Use sharp dissection to mobilize the bladder off the anterior cervix.
- Maintain awareness of the close proximity of the lower ureter to the uterosacral cardinal ligament. As the ureter enters the bladder, it can be as close as 1 cm lateral to the uterosacral ligament. This is an area where it is almost impossible to dissect out the ureter, so the surgeon needs to appreciate this anatomy and refrain from taking aggressive bites in the lateral direction when supporting or closing the vaginal cuff.
How can a surgeon prevent bladder or ureteral injury during laparoscopic hysterectomy?
BARBER: I think the ureter is best identified by direct visualization transperitoneally. The angle of the laparoscope makes visualizing the ureter much easier than from an abdominal approach, so retroperitoneal dissection is not necessary as often.
If the course of the ureter is not readily identified by direct transperitoneal visualization, a peritoneal incision can be made below and parallel to the infundibulopelvic ligament, which allows entry into the retroperitoneum and, typically, easy visualization of the ureter throughout its course.
Alternatively, the retroperitoneum can be entered lateral to the infundibulopelvic ligament, and the ureter can be identified in the same manner as in abdominal hysterectomy.
If laparoscopically assisted hysterectomy is planned, I prefer to dissect the bladder flap vaginally rather than laparoscopically, as the risk of bladder injury is considerably lower from a vaginal approach than it is laparoscopically. Obviously, if a total laparoscopic hysterectomy is necessary because of poor vaginal access, laparoscopic bladder flap dissection is necessary. In this case, I again favor sharp dissection and minimal use of cautery to avoid bladder injury.
How can a surgeon prevent bladder or ureteral injury during vaginal hysterectomy?
BENT: Traditional methods in which each clamp is rolled off the cervix or uterus until the procedure is completed help keep unsuspecting surgeons out of the bladder and away from the ureter. The only risk involves bladder mobilization (ie, creation of the bladder flap), which should always be done sharply to prevent bladder perforation. Avoid blunt finger or sponge-stick dissection! Knowing how to sharply dissect the bladder flap is vital—then even cases of prior cesarean section are manageable.
Salpingo-oophorectomy can also proceed under direct vision. Avoid the ureter by making sure the clamp closes only over the pedicles of the tube and ovary, with no intervening tissues in the clamp. If space is very tight, divide the round ligament and take the pedicle in a smaller bite. Traction on the cervix during the procedure, and mobilization of the bladder, allow the ureters to slide upward, well out of harm’s way, as the procedure progresses.
The importance of sharp dissection
BARBER: During vaginal hysterectomy, I usually have the operative assistant hold the cervical tenaculum so that there is tension on the uterus. I then use forceps to elevate the bladder directly vertically in order to place the bladder fibers on tension. Next, I dissect the bladder off the cervix and lower uterine segment using sharp dissection, and identify the peritoneum by direct finger palpation. Almost always, it is smooth and slippery.
After identifying the peritoneum, I grasp it with a tonsil clamp and elevate it so that it can be entered easily with scissors. I always confirm peritoneal entry by visualizing and identifying intraperitoneal structures such as bowel fat, the uterine serosal surface, or adnexae.
Some people advocate palpating the ureter during vaginal cases.
CUNDIFF: The most common time of injury during vaginal hysterectomy is during dissection of the vesicovaginal space; and suture ligation of the infundibulopelvic ligaments and uterine arteries carries the greatest potential for ureteral injury.
During vaginal hysterectomy, I try to dissect the vesicovaginal space early. I use a Deever retractor to retract the bladder anteriorly, maximizing my ability to sharply dissect close to the cervix until entering the peritoneal cavity. Once I’m in the peritoneal cavity, I advance the Deever retractor to protect the bladder through the rest of the procedure. I maximize protection of the ureters by applying downward traction on the cervix during vaginal clamp placement.
KARRAM: I agree. Never try to enter the anterior cul-de-sac until the vesicouterine space has been identified and is easily palpated. Rushing to enter the anterior cul-de-sac will only lead to inadvertent cystotomy.
Assessing ureteral patency
After what pelvic surgeries do you think ureteral patency should be assessed, and how should it be accomplished?
CUNDIFF: The literature contains several studies10-13 that involved universal endoscopy of the lower urinary tract. These studies demonstrate that most injuries are not recognized by the surgeon prior to endoscopy. In fact, the vast majority of injuries occur after straightforward hysterectomies. This may be due in part to the sheer volume of hysterectomies, compared with other pelvic surgeries. However, it also shows that, when lower urinary tract evaluation is performed solely when the surgeon suspects an injury, a substantial proportion of injuries are missed.
KARRAM: When do you assess ureteral patency?
CUNDIFF: My personal practice is to evaluate it in all cases that carry the potential for injury to the ureter. The complexity of the evaluation is proportional to the probability of ureteral injury.
For all laparotomies and laparoscopies, I identify the course of the ureter and confirm peristalsis. In the simplest of cases, this can be done by identifying the ureter beneath the peritoneum as it crosses the pelvic brim and courses across the pelvic sidewall. More frequently, it involves opening the pararectal space to identify the course of the ureter. In the most complex cases, it requires ureterolysis.
I strongly believe that identifying the ureter during any dissection that endangers it is the best way to avoid injury. Even after these precautions, I frequently perform cystoscopy with intravenous indigo carmine to confirm ureteral patency. This is my standard approach with all vaginal procedures, as I am not confident that I can palpate the course of the ureter.
Postoperative cystoscopy is virtually without morbidity and adds no more than 3 minutes to the procedure when properly planned. It also affords an excellent opportunity to train residents in cystoscopy.
How to assess patency after selected procedures
BENT: Ureteral patency should be assured after any repair of the pelvic floor.
After abdominal hysterectomy, if there is blood in the catheter bag or any difficulty has been encountered during surgery, I perform cystoscopy after injecting indigo carmine dye, to observe ureteral function.
At abdominal or laparoscopic sacrocolpopexy, I follow the path of the ureters over the pelvic brim and inferiorly to the adnexal area by direct inspection.
During abdominal or laparoscopic paravaginal repair, the Burch procedure, or uterosacral ligament suspension, I perform cystoscopy after tying sutures and injecting indigo carmine to ensure ureteral function.
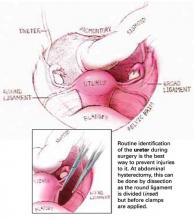
To safeguard the ureter, follow its course
Vaginal hysterectomy is not usually associated with ureteral injury, and very uncommonly with bladder injury. However, if bladder injury is observed or the procedure has been difficult, it is wise to perform cystoscopy with dye injection. This also extends to traditional cystocele repair.
I also recommend cystoscopy with dye injection any time there is a vaginal approach to paravaginal defect repair, vault suspension, or colpocleisis.
Cystoscopy—safe, simple, and efficient
KARRAM: For vaginal surgery, I think cystoscopy is the simplest way to assess the lower urinary tract. I routinely use it after any procedures involving the posterior cul-de-sac such as McCall culdoplasty or vaginal vault suspension from the uterosacral ligaments. I also use it routinely after advanced prolapse repairs involving anterior colporrhaphy, as well as paravaginal defect repairs, and I certainly use it routinely after any lower urinary tract reconstructive procedures such as fistula repairs.
As for laparoscopic surgery, I think cystoscopy is again the most efficient way to assess the lower urinary tract. I do so after any retropubic suspension, be it a Burch colposuspension or a paravaginal repair, any type of vault suspension or sacrocolpopexy, and any type of hysterectomy or adnexectomy that involves dissection of the retroperitoneal space. I also do so if an energy source was used extensively in the vicinity of the retroperitoneal space on either side.
After abdominal surgery, it is probably more efficient (assuming the patient is not in stirrups) to perform a high extraperitoneal cystotomy or suprapubic telescopy. The indications are any difficult dissection in which I have concerns about ureteral patency, as well as any abdominal prolapse or anti-incontinence procedures.
Ureteral stenting
Is ureteral stenting ever indicated preoperatively? If so, when?
BARBER: I do not think ureteral stenting is indicated routinely for any procedure. There may be individual cases where a stent may help the surgeon avoid ureteral injury, but I can’t think of a procedure in which it should be routinely used.
CUNDIFF: I agree. Although ureteral stenting is an important tool for the pelvic floor surgeon to investigate potential ureteral obstruction, I think it has very limited value as a preoperative maneuver to avoid injury. My opinion is based on the following observations:
The surgeon cannot really assess the potential difficulty of identifying the course of the ureter until the peritoneal cavity is entered.
For the truly hostile pelvis, in which pelvic sidewall pathology prevents identification of the course of the ureter, I do not find that a stent facilitates dissection of the pararectal space and ureterolysis. In fact, it could increase the chance of ureteral injury by creating a backboard against which to cut it during dissection.
Any potential benefit of ureteral stents—which I believe is minimal—must be balanced against the potential risks, which include 20 to 30 minutes of added OR time and the risk of ureteral spasm or perforation.
BENT: I also agree that ureteral stenting is seldom helpful during gynecologic surgery. At laparotomy, direct dissection of the structures and exposure of the ureter are best; there is no need to feel for a ureter.
At laparoscopy, however, if there are large fibroids, scarring from endometriomas, or adnexal masses, then preoperative placement of lighted stents can help the surgeon identify the ureters during dissection. The case would still require dissection of the ureter away from the operative field, but the lighted path provides a starting point in this procedure.
For vaginal surgical procedures, it is easier to avoid the ureter. However, not all surgeons can palpate a nonstented ureter, which may be required during a high uterosacral ligament suspension. A stent can readily take the surgeon to the ureter and avoid injury in most cases. This may be helpful for less experienced operators.
What should residents be trained to do?
Do most obstetrics and gynecology residency programs appropriately train young physicians to evaluate and manage lower urinary tract injury during pelvic surgery?
CUNDIFF: I am afraid not. Although residency directors increasingly recognize the importance of educating doctors to prevent and manage these injuries, this recognition has not yet risen to the policy level.
For example, the Council on Resident Education in Obstetrics and Gynecology (CREOG) includes a bladder surgery educational model that necessitates dissection of the ureter, cystoscopy, ureteral stenting, bladder repair, and ureteral reanastomosis.
However, the CREOG surgical curriculum makes no mention of protecting or evaluating the lower urinary tract during pelvic surgery.
This spectrum seems to reflect the wide variation among residency programs, too. While some programs such as ours at Johns Hopkins provide comprehensive training in prevention, evaluation, and management of lower urinary tract injury, many others do not. This might be because some programs lack technically skilled faculty. Interdisciplinary politics also likely influences local credentialing.
BARBER: In my opinion, a graduating ObGyn resident should be able to:
- identify and mobilize the ureter to avoid injury during abdominal and laparoscopic surgery
- safely mobilize the bladder during abdominal, vaginal, or laparoscopic hysterectomy
- perform intraoperative cystoscopy to evaluate for injury
- repair bladder injuries abdominally and vaginally
However, I don’t think it is realistic for a graduating resident to be able to manage ureteral injuries, as residents are unlikely to encounter very many during training. These injuries are best left to our urology colleagues.
BENT: Very little or no education is provided in preventing lower urinary tract injury; evaluation is better managed in many programs. A conservative estimate is that 20% of programs have a reasonable curriculum for preoperative assessment and evaluation of incontinence and prolapse.
The management of pelvic floor disorders is better handled in almost all programs, especially as it relates to surgery. Many residents spend a lot of time on the urogynecology service and are exposed to the surgical aspect of rotations.
Dr. Karram and Dr. Barber have no financial relationships relevant to this article. Dr. Bent serves on the gynecology advisory board of ACMI and is a speaker for Novartis, Pfizer, Watson, and Asetellas (formerly Yamanouchi). He also has received research funding from Cook, Eli Lilly, and Mentor; and is a consultant for C.R. Bard. Dr. Cundiff has received grant/research support from Cook, is a consultant to C.R. Bard and Eli Lilly, and is a speaker for GlaxoSmithKline.
- Moderator Mickey Karram, MD, Director of Urogynecology, Good Samaritan Hospital, Cincinnati, and Professor of Obstetrics and Gynecology, University of Cincinnati.
- Matthew Barber, MD, MHS, Section of Urogynecology and Reconstructive Pelvic Surgery, Departments of Obstetrics & Gynecology and Urology, Cleveland Clinic, Cleveland.
- Alfred Bent, MD, Head, Division of Gynecology, Department of Obstetrics and Gynecology, Dalhousie University, IWK Health Center, Halifax, Nova Scotia.
- Geoffrey Cundiff, MD, Professor of Obstetrics and Gynecology, Johns Hopkins University, Baltimore.
Unfortunate but true: Many complications of pelvic surgery involve injury to the lower urinary tract—and many of these injuries go undetected and increase the patient’s risk of serious morbidity and the physician’s chances of being sued.
Even more unfortunate: These injuries are on the rise, thanks to the proliferation of anti-incontinence surgeries, greater use of laparoscopy, and the need for increasingly complex vaginal dissection.
Fortunately, most lower urinary tract injuries can be avoided, or at least detected early, and this discussion centers on techniques to accomplish those goals and ensure bladder integrity and ureteral patency.
The rising injury rate
There appear to be more injuries to the lower urinary tract arising from pelvic surgery. Why do you think that is?
BARBER: I think the increase is due to the increasing popularity of midurethral slings, such as the tension-free vaginal tape (TVT). With these blind retropubic procedures, the risk of bladder injury is approximately 5%, which is considerably higher than in most other procedures we perform.1
Fortunately, the negative consequences of placing the TVT trocar into the dome of the bladder are minimal, since the trocar can be removed and placed in the appropriate location without the need for bladder repair and without causing long-term bladder dysfunction.
KARRAM: The higher rate of injury also may be linked, in part, to greater use of energy sources during laparoscopic surgery. Over the past 2 years, we have seen numerous cases of delayed injury to the lower urinary tract or bowel secondary to thermal damage from energy devices including electrosurgical instruments and ultrasonic shears.
BARBER: I think there is an increase in lower urinary tract and ureteral injury because of the rising popularity of operative laparoscopy. Lower urinary tract injury is certainly more common with laparoscopic hysterectomy than with abdominal or vaginal hysterectomy.
Increase has no single cause
BENT: There may be a small increase overall in lower urinary tract injury during pelvic surgery, since we now do more procedures that require complicated vaginal dissection and exploration of tissue planes in close proximity to the ureters. This has increased the rate of ureteral injuries.
There also have been a few more urethral injuries, again related to tension-free suburethral slings, most often involving the transobturator approach.
KARRAM: The higher rate of cesarean sections also plays a role. Many women undergoing hysterectomies have had 1 or more cesarean deliveries. We recently completed a study that shows that cesarean section is an independent risk factor for cystotomy at the time of hysterectomy.2
Unfortunately, many surgeons still use aggressive blunt dissection when they attempt to mobilize the bladder off the uterus—whether a hysterectomy is being performed abdominally or vaginally. This can lead to inadvertent entry into the bladder. For this reason, sharp dissection should always be used.
CUNDIFF: Based on my reading of the literature, the incidence of operative injury to the lower urinary tract during gynecologic surgery in general has not changed noticeably since Samson reviewed the subject in 19023—although gynecologic surgery is the leading cause of such injuries and the leading cause of litigation against gynecologists.4
Most injuries involve hysterectomy
CUNDIFF: Most injuries occur during straightforward hysterectomies. Estimates of the prevalence of ureteral injury range from 0.4% to 2.4%.5-8 Since most studies estimating prevalence have not evaluated the lower urinary tract in the whole study population, they may underestimate true prevalence. However, a recent study by Vakili and colleagues9 included universal endoscopy of all patients undergoing hysterectomy and reported rates of ureteral injury (1.7%) and bladder injury (3.6%) similar to those of less rigorous studies.
Overall, the incidence of lower urinary tract injury during other types of urogynecologic surgery is higher than during hysterectomy. Evidence of the higher prevalence during urogynecologic surgery comes from several recent studies. Harris et al10 reported a 5.7% injury rate during reconstructive surgery for incontinence or prolapse. Importantly, 4% were unrecognized prior to urinary tract endoscopy.
Procedures most commonly associated with urinary tract injury were retropubic urethropexy and apical prolapse procedures using the uterosacral ligament in this series. This higher prevalence in urogynecologic procedures may explain the perceived increase in injuries overall.
How can a surgeon prevent bladder or ureteral injury during open hysterectomy?
BENT: Any procedure—regardless of the approach—demands careful dissection, good lighting, and exposure of appropriate structures. It is hard to avoid what you cannot see!
CUNDIFF: When I enter the peritoneal cavity, especially in patients undergoing reoperation, I make the incision more superiorly and avoid the bladder when extending the incision inferiorly. I always open the pararectal space and identify the ureters to ensure their safety during clamping.
Dissection of the vesicovaginal space is most effective when it is done sharply with adequate traction and countertraction. This can be achieved by gently pulling the bladder anteriorly with a Babcock clamp, using scissors to dissect close to the cervix.
For very large fundi, dissection of the vesicovaginal space can be difficult if the uterus is brought through the laparotomy. In these cases I generally take the round ligaments and infundibulopelvic ligaments first and then push the fundus into the upper abdomen. This helps keep the bowel out of the field and gives better visualization of the vesicovaginal space.
I generally enter the anterior fornix with a scalpel and then use Jorgensen scissors to excise the cervix. This helps protect the bladder, and also maximizes vaginal length.
By the way, I use a modified lithotomy position with universal stirrups to maintain access to the bladder for cystoscopy, in case it is needed later.
Follow the ureter
BARBER: During abdominal hysterectomy, I routinely identify the course of the ureter in the retroperitoneum and follow it from where it enters the pelvis until it disappears into the cardinal ligament and below the uterine artery. Following its course helps me avoid ureteral injury.
BENT: If there is scarring of the tube or ovary, or a mass is present, the ureter may have to be localized and dissected completely free of the adnexal structures before any clamps are placed. In addition, the bladder flap should routinely be mobilized using sharp dissection, never blunt dissection.
Mobilization of the bladder downward also pushes the ureters further out of the way during clamping of the uterine vessels. If bleeding occurs, secure hemostasis after observing the location of the ureters. If there is any concern about injury, cystoscopy with injected dye is required.
Next, as the uterosacral and cardinal ligaments are approached, the bladder must be reflected well inferior to this area. This will keep the ureters somewhat removed from the clamps.
Other tricks include performing intrafascial hysterectomy, in which the fascia is peeled away from the uterus and cervix, protecting the ureters.
Clamps placed across the cardinal and uterosacral ligament complexes must hug the uterus and roll off the cervix to protect the ureter.
When the cuff is sutured after removal of the uterus, clear planes of vagina must be seen anteriorly and posteriorly to avoid suturing the bladder into the vaginal cuff.
3 preventive strategies
KARRAM: For abdominal hysterectomy, I recommend 3 techniques:
- Skeletonize the infundibulopelvic ligament. Most surgeons do this routinely during the abdominal approach; I also recommend it for laparoscopic hysterectomy. Once there is a window in the broad ligament and the infundibulopelvic ligament is skeletonized, one can be sure the ureter is well below this area and probably out of harm’s way.
- Use sharp dissection to mobilize the bladder off the anterior cervix.
- Maintain awareness of the close proximity of the lower ureter to the uterosacral cardinal ligament. As the ureter enters the bladder, it can be as close as 1 cm lateral to the uterosacral ligament. This is an area where it is almost impossible to dissect out the ureter, so the surgeon needs to appreciate this anatomy and refrain from taking aggressive bites in the lateral direction when supporting or closing the vaginal cuff.
How can a surgeon prevent bladder or ureteral injury during laparoscopic hysterectomy?
BARBER: I think the ureter is best identified by direct visualization transperitoneally. The angle of the laparoscope makes visualizing the ureter much easier than from an abdominal approach, so retroperitoneal dissection is not necessary as often.
If the course of the ureter is not readily identified by direct transperitoneal visualization, a peritoneal incision can be made below and parallel to the infundibulopelvic ligament, which allows entry into the retroperitoneum and, typically, easy visualization of the ureter throughout its course.
Alternatively, the retroperitoneum can be entered lateral to the infundibulopelvic ligament, and the ureter can be identified in the same manner as in abdominal hysterectomy.
If laparoscopically assisted hysterectomy is planned, I prefer to dissect the bladder flap vaginally rather than laparoscopically, as the risk of bladder injury is considerably lower from a vaginal approach than it is laparoscopically. Obviously, if a total laparoscopic hysterectomy is necessary because of poor vaginal access, laparoscopic bladder flap dissection is necessary. In this case, I again favor sharp dissection and minimal use of cautery to avoid bladder injury.
How can a surgeon prevent bladder or ureteral injury during vaginal hysterectomy?
BENT: Traditional methods in which each clamp is rolled off the cervix or uterus until the procedure is completed help keep unsuspecting surgeons out of the bladder and away from the ureter. The only risk involves bladder mobilization (ie, creation of the bladder flap), which should always be done sharply to prevent bladder perforation. Avoid blunt finger or sponge-stick dissection! Knowing how to sharply dissect the bladder flap is vital—then even cases of prior cesarean section are manageable.
Salpingo-oophorectomy can also proceed under direct vision. Avoid the ureter by making sure the clamp closes only over the pedicles of the tube and ovary, with no intervening tissues in the clamp. If space is very tight, divide the round ligament and take the pedicle in a smaller bite. Traction on the cervix during the procedure, and mobilization of the bladder, allow the ureters to slide upward, well out of harm’s way, as the procedure progresses.
The importance of sharp dissection
BARBER: During vaginal hysterectomy, I usually have the operative assistant hold the cervical tenaculum so that there is tension on the uterus. I then use forceps to elevate the bladder directly vertically in order to place the bladder fibers on tension. Next, I dissect the bladder off the cervix and lower uterine segment using sharp dissection, and identify the peritoneum by direct finger palpation. Almost always, it is smooth and slippery.
After identifying the peritoneum, I grasp it with a tonsil clamp and elevate it so that it can be entered easily with scissors. I always confirm peritoneal entry by visualizing and identifying intraperitoneal structures such as bowel fat, the uterine serosal surface, or adnexae.
Some people advocate palpating the ureter during vaginal cases.
CUNDIFF: The most common time of injury during vaginal hysterectomy is during dissection of the vesicovaginal space; and suture ligation of the infundibulopelvic ligaments and uterine arteries carries the greatest potential for ureteral injury.
During vaginal hysterectomy, I try to dissect the vesicovaginal space early. I use a Deever retractor to retract the bladder anteriorly, maximizing my ability to sharply dissect close to the cervix until entering the peritoneal cavity. Once I’m in the peritoneal cavity, I advance the Deever retractor to protect the bladder through the rest of the procedure. I maximize protection of the ureters by applying downward traction on the cervix during vaginal clamp placement.
KARRAM: I agree. Never try to enter the anterior cul-de-sac until the vesicouterine space has been identified and is easily palpated. Rushing to enter the anterior cul-de-sac will only lead to inadvertent cystotomy.
Assessing ureteral patency
After what pelvic surgeries do you think ureteral patency should be assessed, and how should it be accomplished?
CUNDIFF: The literature contains several studies10-13 that involved universal endoscopy of the lower urinary tract. These studies demonstrate that most injuries are not recognized by the surgeon prior to endoscopy. In fact, the vast majority of injuries occur after straightforward hysterectomies. This may be due in part to the sheer volume of hysterectomies, compared with other pelvic surgeries. However, it also shows that, when lower urinary tract evaluation is performed solely when the surgeon suspects an injury, a substantial proportion of injuries are missed.
KARRAM: When do you assess ureteral patency?
CUNDIFF: My personal practice is to evaluate it in all cases that carry the potential for injury to the ureter. The complexity of the evaluation is proportional to the probability of ureteral injury.
For all laparotomies and laparoscopies, I identify the course of the ureter and confirm peristalsis. In the simplest of cases, this can be done by identifying the ureter beneath the peritoneum as it crosses the pelvic brim and courses across the pelvic sidewall. More frequently, it involves opening the pararectal space to identify the course of the ureter. In the most complex cases, it requires ureterolysis.
I strongly believe that identifying the ureter during any dissection that endangers it is the best way to avoid injury. Even after these precautions, I frequently perform cystoscopy with intravenous indigo carmine to confirm ureteral patency. This is my standard approach with all vaginal procedures, as I am not confident that I can palpate the course of the ureter.
Postoperative cystoscopy is virtually without morbidity and adds no more than 3 minutes to the procedure when properly planned. It also affords an excellent opportunity to train residents in cystoscopy.
How to assess patency after selected procedures
BENT: Ureteral patency should be assured after any repair of the pelvic floor.
After abdominal hysterectomy, if there is blood in the catheter bag or any difficulty has been encountered during surgery, I perform cystoscopy after injecting indigo carmine dye, to observe ureteral function.
At abdominal or laparoscopic sacrocolpopexy, I follow the path of the ureters over the pelvic brim and inferiorly to the adnexal area by direct inspection.
During abdominal or laparoscopic paravaginal repair, the Burch procedure, or uterosacral ligament suspension, I perform cystoscopy after tying sutures and injecting indigo carmine to ensure ureteral function.
To safeguard the ureter, follow its course
Vaginal hysterectomy is not usually associated with ureteral injury, and very uncommonly with bladder injury. However, if bladder injury is observed or the procedure has been difficult, it is wise to perform cystoscopy with dye injection. This also extends to traditional cystocele repair.
I also recommend cystoscopy with dye injection any time there is a vaginal approach to paravaginal defect repair, vault suspension, or colpocleisis.
Cystoscopy—safe, simple, and efficient
KARRAM: For vaginal surgery, I think cystoscopy is the simplest way to assess the lower urinary tract. I routinely use it after any procedures involving the posterior cul-de-sac such as McCall culdoplasty or vaginal vault suspension from the uterosacral ligaments. I also use it routinely after advanced prolapse repairs involving anterior colporrhaphy, as well as paravaginal defect repairs, and I certainly use it routinely after any lower urinary tract reconstructive procedures such as fistula repairs.
As for laparoscopic surgery, I think cystoscopy is again the most efficient way to assess the lower urinary tract. I do so after any retropubic suspension, be it a Burch colposuspension or a paravaginal repair, any type of vault suspension or sacrocolpopexy, and any type of hysterectomy or adnexectomy that involves dissection of the retroperitoneal space. I also do so if an energy source was used extensively in the vicinity of the retroperitoneal space on either side.
After abdominal surgery, it is probably more efficient (assuming the patient is not in stirrups) to perform a high extraperitoneal cystotomy or suprapubic telescopy. The indications are any difficult dissection in which I have concerns about ureteral patency, as well as any abdominal prolapse or anti-incontinence procedures.
Ureteral stenting
Is ureteral stenting ever indicated preoperatively? If so, when?
BARBER: I do not think ureteral stenting is indicated routinely for any procedure. There may be individual cases where a stent may help the surgeon avoid ureteral injury, but I can’t think of a procedure in which it should be routinely used.
CUNDIFF: I agree. Although ureteral stenting is an important tool for the pelvic floor surgeon to investigate potential ureteral obstruction, I think it has very limited value as a preoperative maneuver to avoid injury. My opinion is based on the following observations:
The surgeon cannot really assess the potential difficulty of identifying the course of the ureter until the peritoneal cavity is entered.
For the truly hostile pelvis, in which pelvic sidewall pathology prevents identification of the course of the ureter, I do not find that a stent facilitates dissection of the pararectal space and ureterolysis. In fact, it could increase the chance of ureteral injury by creating a backboard against which to cut it during dissection.
Any potential benefit of ureteral stents—which I believe is minimal—must be balanced against the potential risks, which include 20 to 30 minutes of added OR time and the risk of ureteral spasm or perforation.
BENT: I also agree that ureteral stenting is seldom helpful during gynecologic surgery. At laparotomy, direct dissection of the structures and exposure of the ureter are best; there is no need to feel for a ureter.
At laparoscopy, however, if there are large fibroids, scarring from endometriomas, or adnexal masses, then preoperative placement of lighted stents can help the surgeon identify the ureters during dissection. The case would still require dissection of the ureter away from the operative field, but the lighted path provides a starting point in this procedure.
For vaginal surgical procedures, it is easier to avoid the ureter. However, not all surgeons can palpate a nonstented ureter, which may be required during a high uterosacral ligament suspension. A stent can readily take the surgeon to the ureter and avoid injury in most cases. This may be helpful for less experienced operators.
What should residents be trained to do?
Do most obstetrics and gynecology residency programs appropriately train young physicians to evaluate and manage lower urinary tract injury during pelvic surgery?
CUNDIFF: I am afraid not. Although residency directors increasingly recognize the importance of educating doctors to prevent and manage these injuries, this recognition has not yet risen to the policy level.
For example, the Council on Resident Education in Obstetrics and Gynecology (CREOG) includes a bladder surgery educational model that necessitates dissection of the ureter, cystoscopy, ureteral stenting, bladder repair, and ureteral reanastomosis.
However, the CREOG surgical curriculum makes no mention of protecting or evaluating the lower urinary tract during pelvic surgery.
This spectrum seems to reflect the wide variation among residency programs, too. While some programs such as ours at Johns Hopkins provide comprehensive training in prevention, evaluation, and management of lower urinary tract injury, many others do not. This might be because some programs lack technically skilled faculty. Interdisciplinary politics also likely influences local credentialing.
BARBER: In my opinion, a graduating ObGyn resident should be able to:
- identify and mobilize the ureter to avoid injury during abdominal and laparoscopic surgery
- safely mobilize the bladder during abdominal, vaginal, or laparoscopic hysterectomy
- perform intraoperative cystoscopy to evaluate for injury
- repair bladder injuries abdominally and vaginally
However, I don’t think it is realistic for a graduating resident to be able to manage ureteral injuries, as residents are unlikely to encounter very many during training. These injuries are best left to our urology colleagues.
BENT: Very little or no education is provided in preventing lower urinary tract injury; evaluation is better managed in many programs. A conservative estimate is that 20% of programs have a reasonable curriculum for preoperative assessment and evaluation of incontinence and prolapse.
The management of pelvic floor disorders is better handled in almost all programs, especially as it relates to surgery. Many residents spend a lot of time on the urogynecology service and are exposed to the surgical aspect of rotations.
Dr. Karram and Dr. Barber have no financial relationships relevant to this article. Dr. Bent serves on the gynecology advisory board of ACMI and is a speaker for Novartis, Pfizer, Watson, and Asetellas (formerly Yamanouchi). He also has received research funding from Cook, Eli Lilly, and Mentor; and is a consultant for C.R. Bard. Dr. Cundiff has received grant/research support from Cook, is a consultant to C.R. Bard and Eli Lilly, and is a speaker for GlaxoSmithKline.
1. Karram MM, Segal JL, Vassallo BJ, Kleeman SD. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol 2003;101:929-932.
2. Rooney C, Crawford A, Vassaco B, Kleeman S, Karram M. Is cesarean section a risk factor for incidental cystotomy at the time of hysterectomy? Am J Obstet Gynecol. In press.
3. Samson JA. Ligation and clamping of the ureter as complications of surgical operations. Am Med. 1902;4:693.-
4. Wiskind AK, Thompson JD. Should cystoscopy be performed at every gynecologic operation to diagnose unsuspected ureteral injury? J Pelvic Surg. 1995;1:134-137.
5. St. Martin EC, et al. Ureteral injury in gynecologic surgery. J Urol. 1953;70:51-57.
6. Conger K, Beecham CT, Horrax TM. Ureteral injury in pelvic surgery: current thought on incidence, pathogenesis, prophylaxis and treatment. Obstet Gynecol. 1954;3:343-357.
7. Mann WJ, Arato M, Patsner B, et al. Ureteral injuries in an obstetrics and gynecology training program: etiology and management. Obstet Gynecol. 1988;72:82-85.
8. Stanhope CR, Wilson TO, Utz WJ, Smith LH, O’Brien PC. Suture entrapment and secondary ureteral obstruction. Am J Obstet Gynecol. 1991;164:1513-1519.
9. Vakili B, Chesson RR, Kyle BL, et al. The incidence of urinary tract injury during hysterectomy: a prospective analysis based on universal cystoscopy. Am J Obstet Gynecol. 2005;192:1599-1604.
10. Harris RL, Cundiff GW, Theofrastous JT, Yoon HW, Bump RC, Addison WA. The value of intraoperative cystoscopy in urogynecologic and reconstructive pelvic surgery. Am J Obstet Gynecol. 1997;177:1367-1369.
11. Gill EJ, Elser DM, Bonidie MJ, Roberts KM, Hurt WG. The routine use of cystoscopy with the Burch procedure. Am J Obstet Gynecol. 2002;186:1108.-
12. Kwon CH, Goldberg RO, Koduri S, Sand PK. The use of intraoperative cystoscopy in major vaginal and urogynecologic surgeries. Am J Obstet Gynecol. 2002;187:1466-1471; discussion 1471-1472.
13. Tulikangas PK, Weber AM, et al. Intraoperative cystoscopy in conjunction with anti-incontinence surgery. Obstet Gynecol. 2000;95(6 Pt 1):794-796.
1. Karram MM, Segal JL, Vassallo BJ, Kleeman SD. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol 2003;101:929-932.
2. Rooney C, Crawford A, Vassaco B, Kleeman S, Karram M. Is cesarean section a risk factor for incidental cystotomy at the time of hysterectomy? Am J Obstet Gynecol. In press.
3. Samson JA. Ligation and clamping of the ureter as complications of surgical operations. Am Med. 1902;4:693.-
4. Wiskind AK, Thompson JD. Should cystoscopy be performed at every gynecologic operation to diagnose unsuspected ureteral injury? J Pelvic Surg. 1995;1:134-137.
5. St. Martin EC, et al. Ureteral injury in gynecologic surgery. J Urol. 1953;70:51-57.
6. Conger K, Beecham CT, Horrax TM. Ureteral injury in pelvic surgery: current thought on incidence, pathogenesis, prophylaxis and treatment. Obstet Gynecol. 1954;3:343-357.
7. Mann WJ, Arato M, Patsner B, et al. Ureteral injuries in an obstetrics and gynecology training program: etiology and management. Obstet Gynecol. 1988;72:82-85.
8. Stanhope CR, Wilson TO, Utz WJ, Smith LH, O’Brien PC. Suture entrapment and secondary ureteral obstruction. Am J Obstet Gynecol. 1991;164:1513-1519.
9. Vakili B, Chesson RR, Kyle BL, et al. The incidence of urinary tract injury during hysterectomy: a prospective analysis based on universal cystoscopy. Am J Obstet Gynecol. 2005;192:1599-1604.
10. Harris RL, Cundiff GW, Theofrastous JT, Yoon HW, Bump RC, Addison WA. The value of intraoperative cystoscopy in urogynecologic and reconstructive pelvic surgery. Am J Obstet Gynecol. 1997;177:1367-1369.
11. Gill EJ, Elser DM, Bonidie MJ, Roberts KM, Hurt WG. The routine use of cystoscopy with the Burch procedure. Am J Obstet Gynecol. 2002;186:1108.-
12. Kwon CH, Goldberg RO, Koduri S, Sand PK. The use of intraoperative cystoscopy in major vaginal and urogynecologic surgeries. Am J Obstet Gynecol. 2002;187:1466-1471; discussion 1471-1472.
13. Tulikangas PK, Weber AM, et al. Intraoperative cystoscopy in conjunction with anti-incontinence surgery. Obstet Gynecol. 2000;95(6 Pt 1):794-796.