User login
A 48-year-old African American woman came to our office because the discoloration of one fingernail that began months earlier had spread to a second finger, and the first finger to become discolored had begun to hurt.
The patient had initially seen another physician, who prescribed itraconazole for presumptive onychomycosis. The patient received a pulse therapy course of itraconazole for 3 months and had no improvement. Therapy ended 4 months ago, and a month ago the end of her left index finger began to ache.
The patient works at a computer, and typing causes pain in the left index finger. A review of her chart reveals she is taking a diuretic for hypertension; there are no other health problems.
What is the diagnosis?
Before taking a more extensive history, it is appropriate to look at her fingers more closely to collect data that will inform questioning. By applying pattern recognition skills first, you can form hypotheses and use the remainder of the exam to test them.
How would you describe the abnormalities seen in Figure 1 and Figure 2 (pattern recognition), and what would be the differential diagnosis (hypotheses)?
What further history, physical exam, or laboratory tests should be completed (hypothesis testing)?
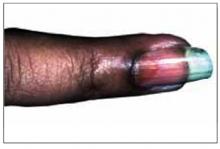
FIGURE 1
This patient’s fingernail had been discolored for months and the fingertip had recently begun to hurt.
A brown discoloration (oil spot) in the patient’s proximal nail.
Figure 1 shows a brownish discoloration of the fingernail, with small pits particularly prominent around the lunula (the semicircular light area adjacent to the proximal nail fold). There is also evidence of onycholysis (separation of the nail from the nail bed). The vertical ridging is not abnormal.
Figure 2 shows a well-circumscribed brown discoloration in the proximal nail called an oil spot. These nail findings are classic for psoriasis.1
Figure 1 also shows subtle swelling of the distal interphalangeal (DIP) joint. It is this area the patient said was painful, and she had joint tenderness to palpation over this DIP joint only.
Hypotheses
The 2 most likely diagnoses are:
- psoriasis causing nail changes while psoriatic arthritis is developing
- onychomycosis with incidental joint pain of the DIP joint.
Other causes of nail changes include lichen planus, chronic candida paronychia, and Reiter’s disease. Epidemiologically the most likely diagnosis is onychomycosis, which is far more prevalent than the other conditions. However, this patient has already failed a course of an oral antifungal agent, and her nail changes are more consistent with psoriasis.
Hypothesis testing
Questions and physical examination focus on collecting data to determine the more likely of the two diagnoses, psoriasis and fungal nail disease. The patient denied having any skin lesions and a history of psoriasis. She also said she had no athlete’s foot or problems with her toenails or other hand. Her knees ache from time to time, which she attributed to aging.
Physical exam revealed no evidence of psoriasis on the skin and no tinea pedis or onychomycosis of the toenails. She had no other skin findings suggestive of lichen planus or Reiter’s disease. Looking more closely at the fingernails, we saw no evidence of subungual keratoses, which are frequently found in onychomycosis.
A scraping and clipping of the fingernail was sent for fungal culture, and an x-ray film of that digit revealed no bony changes. The fungal culture results 2 weeks later were negative.
Patient follow-up
We made a presumptive diagnosis of psoriatic nail changes and psoriatic arthritis, and the patient was sent to a rheumatologist for consultation. The rheumatologist agreed with the diagnosis and placed the patient on nonsteroidal anti-inflammatory drugs to treat the early psoriatic arthritis.
The patient developed more areas of psoriatic arthritis involvement over the subsequent years and became less concerned about the appearance of her nails. Eventually the psoriatic arthritis progressed to the point where the patient was taking remititive agents for inflammatory arthropathy. She never did develop the skin lesions of psoriasis.
Nail changes of psoriasis
It has been reported that 30% of patients with psoriasis have nail changes, the most common being pitting. Onycholysis is the next most frequent change, and the oil spot is less frequent but not rare.
Not everyone with nail pitting has psoriasis; however, there is a high correlation between psoriatic arthritis and nail pitting.
Patients with psoriasis and psoriatic arthritis have a higher percentage of nail changes than patients with psoriasis of the skin only. In 1 study, nail changes were noted in 86.5% of patients affected by arthropathic psoriasis, and the most common fingernail change was pitting.2
This particular case shows it is possible to have psoriatic arthritis and psoriatic nail changes without psoriasis of the skin. Fortunately, the patient did not have an adverse reaction to the itraconazole prescribed for the incorrectly diagnosed onychomycosis.
It is debatable whether fungal cultures are needed before prescribing oral antifungal agents for onychomycosis. This was 1 case in which the nail findings may have steered the clinician toward getting a nail scraping for microscopic analysis using potassium hydroxide or a fungal culture. Negative findings would have spared the patient the treatment with an expensive agent with known liver toxicity.
The onset of pain, swelling, and tenderness of the DIP joint of the affected nail helped to make the diagnosis. It is the finger joint most commonly affected by psoriatic arthritis.
Treatment of psoriasis of the nails
There is no good treatment for psoriasis of the nails. Treatment regimens that have been studied include injection of steroids into the nail matrix and use of topical retinoids. Intralesional steroid injections are very painful, and the results are not adequate to recommend this treatment.
A study of topical retinoid tazorotene showed some promise.3 The study size was small, however, and the measured change was not great. But for patients desperately looking for help for psoriatic nail changes, the topical treatment may be worth a try.
Figure 3 shows a different patient with an interesting connection between involvement of psoriatic arthritis in the finger and accompanying nail changes. This man had psoriatic plaques over his fingers and a severely swollen DIP joint of the middle finger with significant accompanying nail changes. The inflammatory reaction in the DIP joint is accompanied by abnormal changes in the nail matrix, producing a psoriatic nail on the same finger.
FIGURE 3
Another patient’s hand, with psoriatic plaques and swollen distal interphalangeal joint.
1. Habif T. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 3rd ed. St. Louis, Mo: Mosby; 1996.
2. Lavaroni G, Kokelj F, Pauluzzi P, Trevisan G. The nails in psoriatic arthritis. Acta Derm Venereol Suppl (Stockh) 1994;186:113.-
3. Scher RK, Stiller M, Zhu YI. Tazarotene 0.1% gel in the treatment of fingernail psoriasis: a double-blind, randomized, vehicle-controlled study. Cutis 2001;68:355-8.
A 48-year-old African American woman came to our office because the discoloration of one fingernail that began months earlier had spread to a second finger, and the first finger to become discolored had begun to hurt.
The patient had initially seen another physician, who prescribed itraconazole for presumptive onychomycosis. The patient received a pulse therapy course of itraconazole for 3 months and had no improvement. Therapy ended 4 months ago, and a month ago the end of her left index finger began to ache.
The patient works at a computer, and typing causes pain in the left index finger. A review of her chart reveals she is taking a diuretic for hypertension; there are no other health problems.
What is the diagnosis?
Before taking a more extensive history, it is appropriate to look at her fingers more closely to collect data that will inform questioning. By applying pattern recognition skills first, you can form hypotheses and use the remainder of the exam to test them.
How would you describe the abnormalities seen in Figure 1 and Figure 2 (pattern recognition), and what would be the differential diagnosis (hypotheses)?
What further history, physical exam, or laboratory tests should be completed (hypothesis testing)?
FIGURE 1
This patient’s fingernail had been discolored for months and the fingertip had recently begun to hurt.
A brown discoloration (oil spot) in the patient’s proximal nail.
Figure 1 shows a brownish discoloration of the fingernail, with small pits particularly prominent around the lunula (the semicircular light area adjacent to the proximal nail fold). There is also evidence of onycholysis (separation of the nail from the nail bed). The vertical ridging is not abnormal.
Figure 2 shows a well-circumscribed brown discoloration in the proximal nail called an oil spot. These nail findings are classic for psoriasis.1
Figure 1 also shows subtle swelling of the distal interphalangeal (DIP) joint. It is this area the patient said was painful, and she had joint tenderness to palpation over this DIP joint only.
Hypotheses
The 2 most likely diagnoses are:
- psoriasis causing nail changes while psoriatic arthritis is developing
- onychomycosis with incidental joint pain of the DIP joint.
Other causes of nail changes include lichen planus, chronic candida paronychia, and Reiter’s disease. Epidemiologically the most likely diagnosis is onychomycosis, which is far more prevalent than the other conditions. However, this patient has already failed a course of an oral antifungal agent, and her nail changes are more consistent with psoriasis.
Hypothesis testing
Questions and physical examination focus on collecting data to determine the more likely of the two diagnoses, psoriasis and fungal nail disease. The patient denied having any skin lesions and a history of psoriasis. She also said she had no athlete’s foot or problems with her toenails or other hand. Her knees ache from time to time, which she attributed to aging.
Physical exam revealed no evidence of psoriasis on the skin and no tinea pedis or onychomycosis of the toenails. She had no other skin findings suggestive of lichen planus or Reiter’s disease. Looking more closely at the fingernails, we saw no evidence of subungual keratoses, which are frequently found in onychomycosis.
A scraping and clipping of the fingernail was sent for fungal culture, and an x-ray film of that digit revealed no bony changes. The fungal culture results 2 weeks later were negative.
Patient follow-up
We made a presumptive diagnosis of psoriatic nail changes and psoriatic arthritis, and the patient was sent to a rheumatologist for consultation. The rheumatologist agreed with the diagnosis and placed the patient on nonsteroidal anti-inflammatory drugs to treat the early psoriatic arthritis.
The patient developed more areas of psoriatic arthritis involvement over the subsequent years and became less concerned about the appearance of her nails. Eventually the psoriatic arthritis progressed to the point where the patient was taking remititive agents for inflammatory arthropathy. She never did develop the skin lesions of psoriasis.
Nail changes of psoriasis
It has been reported that 30% of patients with psoriasis have nail changes, the most common being pitting. Onycholysis is the next most frequent change, and the oil spot is less frequent but not rare.
Not everyone with nail pitting has psoriasis; however, there is a high correlation between psoriatic arthritis and nail pitting.
Patients with psoriasis and psoriatic arthritis have a higher percentage of nail changes than patients with psoriasis of the skin only. In 1 study, nail changes were noted in 86.5% of patients affected by arthropathic psoriasis, and the most common fingernail change was pitting.2
This particular case shows it is possible to have psoriatic arthritis and psoriatic nail changes without psoriasis of the skin. Fortunately, the patient did not have an adverse reaction to the itraconazole prescribed for the incorrectly diagnosed onychomycosis.
It is debatable whether fungal cultures are needed before prescribing oral antifungal agents for onychomycosis. This was 1 case in which the nail findings may have steered the clinician toward getting a nail scraping for microscopic analysis using potassium hydroxide or a fungal culture. Negative findings would have spared the patient the treatment with an expensive agent with known liver toxicity.
The onset of pain, swelling, and tenderness of the DIP joint of the affected nail helped to make the diagnosis. It is the finger joint most commonly affected by psoriatic arthritis.
Treatment of psoriasis of the nails
There is no good treatment for psoriasis of the nails. Treatment regimens that have been studied include injection of steroids into the nail matrix and use of topical retinoids. Intralesional steroid injections are very painful, and the results are not adequate to recommend this treatment.
A study of topical retinoid tazorotene showed some promise.3 The study size was small, however, and the measured change was not great. But for patients desperately looking for help for psoriatic nail changes, the topical treatment may be worth a try.
Figure 3 shows a different patient with an interesting connection between involvement of psoriatic arthritis in the finger and accompanying nail changes. This man had psoriatic plaques over his fingers and a severely swollen DIP joint of the middle finger with significant accompanying nail changes. The inflammatory reaction in the DIP joint is accompanied by abnormal changes in the nail matrix, producing a psoriatic nail on the same finger.
FIGURE 3
Another patient’s hand, with psoriatic plaques and swollen distal interphalangeal joint.
A 48-year-old African American woman came to our office because the discoloration of one fingernail that began months earlier had spread to a second finger, and the first finger to become discolored had begun to hurt.
The patient had initially seen another physician, who prescribed itraconazole for presumptive onychomycosis. The patient received a pulse therapy course of itraconazole for 3 months and had no improvement. Therapy ended 4 months ago, and a month ago the end of her left index finger began to ache.
The patient works at a computer, and typing causes pain in the left index finger. A review of her chart reveals she is taking a diuretic for hypertension; there are no other health problems.
What is the diagnosis?
Before taking a more extensive history, it is appropriate to look at her fingers more closely to collect data that will inform questioning. By applying pattern recognition skills first, you can form hypotheses and use the remainder of the exam to test them.
How would you describe the abnormalities seen in Figure 1 and Figure 2 (pattern recognition), and what would be the differential diagnosis (hypotheses)?
What further history, physical exam, or laboratory tests should be completed (hypothesis testing)?
FIGURE 1
This patient’s fingernail had been discolored for months and the fingertip had recently begun to hurt.
A brown discoloration (oil spot) in the patient’s proximal nail.
Figure 1 shows a brownish discoloration of the fingernail, with small pits particularly prominent around the lunula (the semicircular light area adjacent to the proximal nail fold). There is also evidence of onycholysis (separation of the nail from the nail bed). The vertical ridging is not abnormal.
Figure 2 shows a well-circumscribed brown discoloration in the proximal nail called an oil spot. These nail findings are classic for psoriasis.1
Figure 1 also shows subtle swelling of the distal interphalangeal (DIP) joint. It is this area the patient said was painful, and she had joint tenderness to palpation over this DIP joint only.
Hypotheses
The 2 most likely diagnoses are:
- psoriasis causing nail changes while psoriatic arthritis is developing
- onychomycosis with incidental joint pain of the DIP joint.
Other causes of nail changes include lichen planus, chronic candida paronychia, and Reiter’s disease. Epidemiologically the most likely diagnosis is onychomycosis, which is far more prevalent than the other conditions. However, this patient has already failed a course of an oral antifungal agent, and her nail changes are more consistent with psoriasis.
Hypothesis testing
Questions and physical examination focus on collecting data to determine the more likely of the two diagnoses, psoriasis and fungal nail disease. The patient denied having any skin lesions and a history of psoriasis. She also said she had no athlete’s foot or problems with her toenails or other hand. Her knees ache from time to time, which she attributed to aging.
Physical exam revealed no evidence of psoriasis on the skin and no tinea pedis or onychomycosis of the toenails. She had no other skin findings suggestive of lichen planus or Reiter’s disease. Looking more closely at the fingernails, we saw no evidence of subungual keratoses, which are frequently found in onychomycosis.
A scraping and clipping of the fingernail was sent for fungal culture, and an x-ray film of that digit revealed no bony changes. The fungal culture results 2 weeks later were negative.
Patient follow-up
We made a presumptive diagnosis of psoriatic nail changes and psoriatic arthritis, and the patient was sent to a rheumatologist for consultation. The rheumatologist agreed with the diagnosis and placed the patient on nonsteroidal anti-inflammatory drugs to treat the early psoriatic arthritis.
The patient developed more areas of psoriatic arthritis involvement over the subsequent years and became less concerned about the appearance of her nails. Eventually the psoriatic arthritis progressed to the point where the patient was taking remititive agents for inflammatory arthropathy. She never did develop the skin lesions of psoriasis.
Nail changes of psoriasis
It has been reported that 30% of patients with psoriasis have nail changes, the most common being pitting. Onycholysis is the next most frequent change, and the oil spot is less frequent but not rare.
Not everyone with nail pitting has psoriasis; however, there is a high correlation between psoriatic arthritis and nail pitting.
Patients with psoriasis and psoriatic arthritis have a higher percentage of nail changes than patients with psoriasis of the skin only. In 1 study, nail changes were noted in 86.5% of patients affected by arthropathic psoriasis, and the most common fingernail change was pitting.2
This particular case shows it is possible to have psoriatic arthritis and psoriatic nail changes without psoriasis of the skin. Fortunately, the patient did not have an adverse reaction to the itraconazole prescribed for the incorrectly diagnosed onychomycosis.
It is debatable whether fungal cultures are needed before prescribing oral antifungal agents for onychomycosis. This was 1 case in which the nail findings may have steered the clinician toward getting a nail scraping for microscopic analysis using potassium hydroxide or a fungal culture. Negative findings would have spared the patient the treatment with an expensive agent with known liver toxicity.
The onset of pain, swelling, and tenderness of the DIP joint of the affected nail helped to make the diagnosis. It is the finger joint most commonly affected by psoriatic arthritis.
Treatment of psoriasis of the nails
There is no good treatment for psoriasis of the nails. Treatment regimens that have been studied include injection of steroids into the nail matrix and use of topical retinoids. Intralesional steroid injections are very painful, and the results are not adequate to recommend this treatment.
A study of topical retinoid tazorotene showed some promise.3 The study size was small, however, and the measured change was not great. But for patients desperately looking for help for psoriatic nail changes, the topical treatment may be worth a try.
Figure 3 shows a different patient with an interesting connection between involvement of psoriatic arthritis in the finger and accompanying nail changes. This man had psoriatic plaques over his fingers and a severely swollen DIP joint of the middle finger with significant accompanying nail changes. The inflammatory reaction in the DIP joint is accompanied by abnormal changes in the nail matrix, producing a psoriatic nail on the same finger.
FIGURE 3
Another patient’s hand, with psoriatic plaques and swollen distal interphalangeal joint.
1. Habif T. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 3rd ed. St. Louis, Mo: Mosby; 1996.
2. Lavaroni G, Kokelj F, Pauluzzi P, Trevisan G. The nails in psoriatic arthritis. Acta Derm Venereol Suppl (Stockh) 1994;186:113.-
3. Scher RK, Stiller M, Zhu YI. Tazarotene 0.1% gel in the treatment of fingernail psoriasis: a double-blind, randomized, vehicle-controlled study. Cutis 2001;68:355-8.
1. Habif T. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 3rd ed. St. Louis, Mo: Mosby; 1996.
2. Lavaroni G, Kokelj F, Pauluzzi P, Trevisan G. The nails in psoriatic arthritis. Acta Derm Venereol Suppl (Stockh) 1994;186:113.-
3. Scher RK, Stiller M, Zhu YI. Tazarotene 0.1% gel in the treatment of fingernail psoriasis: a double-blind, randomized, vehicle-controlled study. Cutis 2001;68:355-8.