User login
A year ago, 81% of gastroenterologists were happy outside of work. Not anymore.
In these COVID-19–pandemic times, that number is down to 54%, according to a survey of more than 12,000 physicians in 29 specialties that was conducted by Medscape.
“Whether on the front lines of treating COVID-19 patients, pivoting from in-person to virtual care, or even having to shutter their practices, physicians faced an onslaught of crises, while political tensions, social unrest, and environmental concerns probably affected their lives outside of medicine,” Keith L. Martin and Mary Lyn Koval of Medscape wrote in the Gastroenterologist Lifestyle, Happiness & Burnout Report 2021.
Surprisingly, perhaps, the proportion of GIs who say that they’re burned out or are both burned out and depressed now is only a little higher (40%) than in last year’s survey (36%). It’s also just under this year’s burnout rate of 42% for all physicians, which has not changed since last year.
COVID-19 may have had some effect on burnout, though. Among the gastroenterologists with burnout, 15% said it began after the pandemic started, which was, again, less than physicians overall, who had a distribution of 79% before and 21% after. The GIs were slightly less likely to report that their burnout had a severe impact on their everyday lives than physicians overall – 44% versus 47% – but more likely to say that it was bad enough to consider leaving medicine – 15% versus 10%.
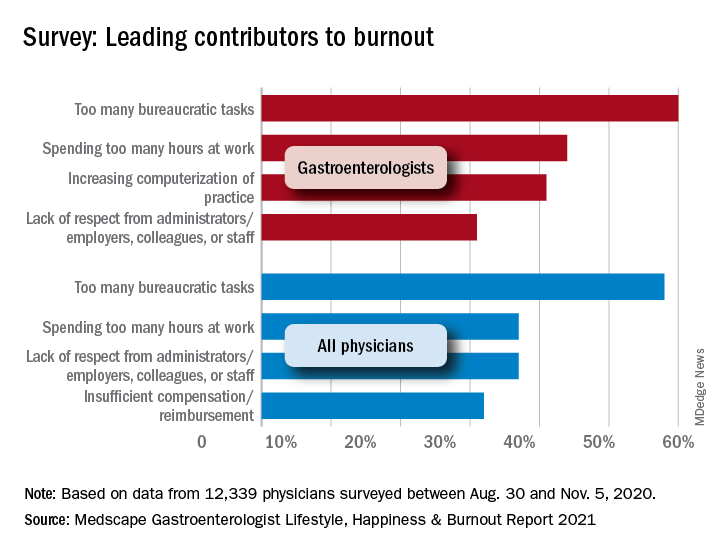
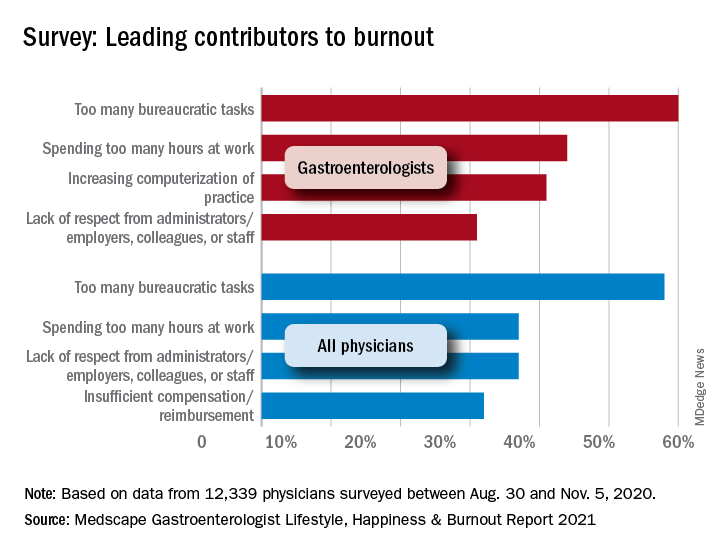
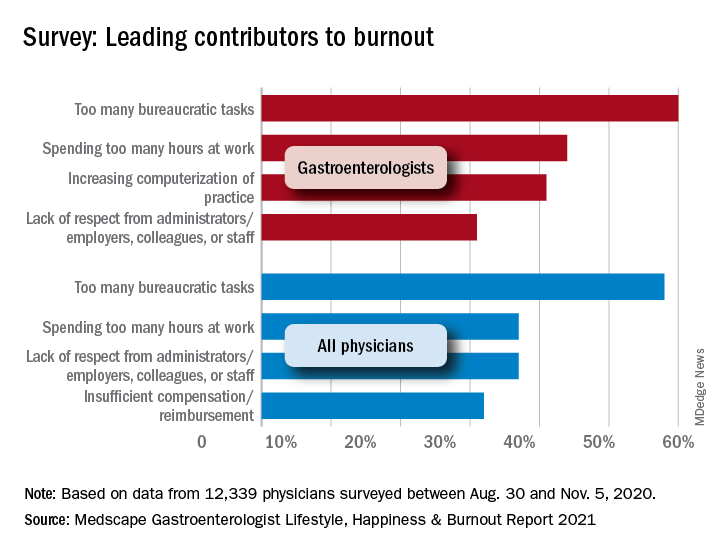
“The chief causes of burnout remain consistent from past years and are pushing physicians to the breaking point,” the Medscape report noted, citing one physician who called it “death by 1,000 cuts.” The biggest contributor to burnout over this past year was, for 60% of gastroenterologists, the excessive number of bureaucratic tasks, followed by spending too much time at work (44%) and increasing computerization (41%).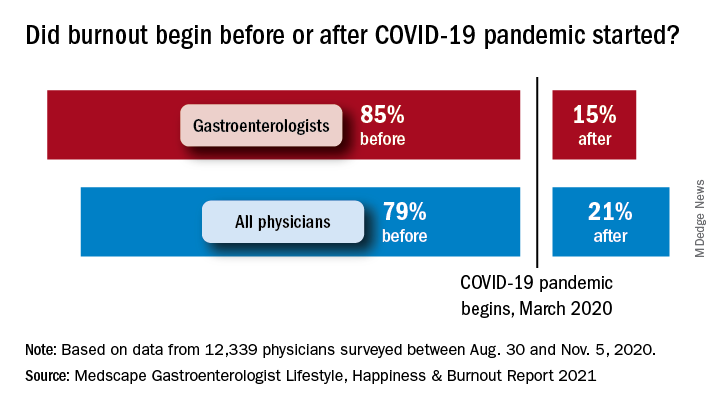
The two pandemic-related contributors included in the survey were near the bottom of the list for gastroenterologists: stress from social distancing/societal issues (15%) and stress related to treating COVID-19 patients (8%), based on data for the 12,339 physicians – of whom about 2% were GIs – polled from Aug. 30 to Nov. 5, 2020.
To deal with their burnout, many gastroenterologists are exercising – at least 51% of them, anyway. Other popular coping mechanisms include talking with family members and close friends (39%), playing or listening to music (38%), isolating themselves from others (36%), and sleeping (26%). For all physicians, the top choices were exercise (48%), talking with family members/friends (43%), and isolation (43%).
When the subject of professional help was raised, a large majority (84%) of GIs planned to forgo such care. That information was not available for physicians as a group, but 70% of internists agreed, as did 83% of nephrologists, 80% of cardiologists, 80% of oncologists, 89% of urologists, and 80% of general surgeons.
A majority of gastroenterologists (58%) said that their symptoms weren’t severe enough to warrant such help, but 38% said they were too busy, and 11% didn’t want to risk disclosure. Some physicians commented on their own situations:
- “I have no energy when I get home and I feel like I’m ignoring my family, but I need to decompress and process what I dealt with during the day” (oncologist).
- “I can’t do the things that I enjoy to relieve stress, such as traveling. My hair is falling out because I can’t destress” (ob.gyn.).
- “I’m tired and discouraged. It stresses my marriage. I have a hard time getting out of bed in the morning. I count the days until Friday” (psychiatrist).
A year ago, 81% of gastroenterologists were happy outside of work. Not anymore.
In these COVID-19–pandemic times, that number is down to 54%, according to a survey of more than 12,000 physicians in 29 specialties that was conducted by Medscape.
“Whether on the front lines of treating COVID-19 patients, pivoting from in-person to virtual care, or even having to shutter their practices, physicians faced an onslaught of crises, while political tensions, social unrest, and environmental concerns probably affected their lives outside of medicine,” Keith L. Martin and Mary Lyn Koval of Medscape wrote in the Gastroenterologist Lifestyle, Happiness & Burnout Report 2021.
Surprisingly, perhaps, the proportion of GIs who say that they’re burned out or are both burned out and depressed now is only a little higher (40%) than in last year’s survey (36%). It’s also just under this year’s burnout rate of 42% for all physicians, which has not changed since last year.
COVID-19 may have had some effect on burnout, though. Among the gastroenterologists with burnout, 15% said it began after the pandemic started, which was, again, less than physicians overall, who had a distribution of 79% before and 21% after. The GIs were slightly less likely to report that their burnout had a severe impact on their everyday lives than physicians overall – 44% versus 47% – but more likely to say that it was bad enough to consider leaving medicine – 15% versus 10%.
“The chief causes of burnout remain consistent from past years and are pushing physicians to the breaking point,” the Medscape report noted, citing one physician who called it “death by 1,000 cuts.” The biggest contributor to burnout over this past year was, for 60% of gastroenterologists, the excessive number of bureaucratic tasks, followed by spending too much time at work (44%) and increasing computerization (41%).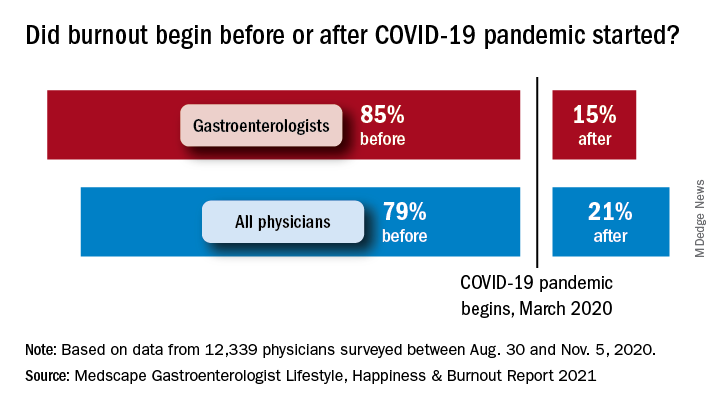
The two pandemic-related contributors included in the survey were near the bottom of the list for gastroenterologists: stress from social distancing/societal issues (15%) and stress related to treating COVID-19 patients (8%), based on data for the 12,339 physicians – of whom about 2% were GIs – polled from Aug. 30 to Nov. 5, 2020.
To deal with their burnout, many gastroenterologists are exercising – at least 51% of them, anyway. Other popular coping mechanisms include talking with family members and close friends (39%), playing or listening to music (38%), isolating themselves from others (36%), and sleeping (26%). For all physicians, the top choices were exercise (48%), talking with family members/friends (43%), and isolation (43%).
When the subject of professional help was raised, a large majority (84%) of GIs planned to forgo such care. That information was not available for physicians as a group, but 70% of internists agreed, as did 83% of nephrologists, 80% of cardiologists, 80% of oncologists, 89% of urologists, and 80% of general surgeons.
A majority of gastroenterologists (58%) said that their symptoms weren’t severe enough to warrant such help, but 38% said they were too busy, and 11% didn’t want to risk disclosure. Some physicians commented on their own situations:
- “I have no energy when I get home and I feel like I’m ignoring my family, but I need to decompress and process what I dealt with during the day” (oncologist).
- “I can’t do the things that I enjoy to relieve stress, such as traveling. My hair is falling out because I can’t destress” (ob.gyn.).
- “I’m tired and discouraged. It stresses my marriage. I have a hard time getting out of bed in the morning. I count the days until Friday” (psychiatrist).
A year ago, 81% of gastroenterologists were happy outside of work. Not anymore.
In these COVID-19–pandemic times, that number is down to 54%, according to a survey of more than 12,000 physicians in 29 specialties that was conducted by Medscape.
“Whether on the front lines of treating COVID-19 patients, pivoting from in-person to virtual care, or even having to shutter their practices, physicians faced an onslaught of crises, while political tensions, social unrest, and environmental concerns probably affected their lives outside of medicine,” Keith L. Martin and Mary Lyn Koval of Medscape wrote in the Gastroenterologist Lifestyle, Happiness & Burnout Report 2021.
Surprisingly, perhaps, the proportion of GIs who say that they’re burned out or are both burned out and depressed now is only a little higher (40%) than in last year’s survey (36%). It’s also just under this year’s burnout rate of 42% for all physicians, which has not changed since last year.
COVID-19 may have had some effect on burnout, though. Among the gastroenterologists with burnout, 15% said it began after the pandemic started, which was, again, less than physicians overall, who had a distribution of 79% before and 21% after. The GIs were slightly less likely to report that their burnout had a severe impact on their everyday lives than physicians overall – 44% versus 47% – but more likely to say that it was bad enough to consider leaving medicine – 15% versus 10%.
“The chief causes of burnout remain consistent from past years and are pushing physicians to the breaking point,” the Medscape report noted, citing one physician who called it “death by 1,000 cuts.” The biggest contributor to burnout over this past year was, for 60% of gastroenterologists, the excessive number of bureaucratic tasks, followed by spending too much time at work (44%) and increasing computerization (41%).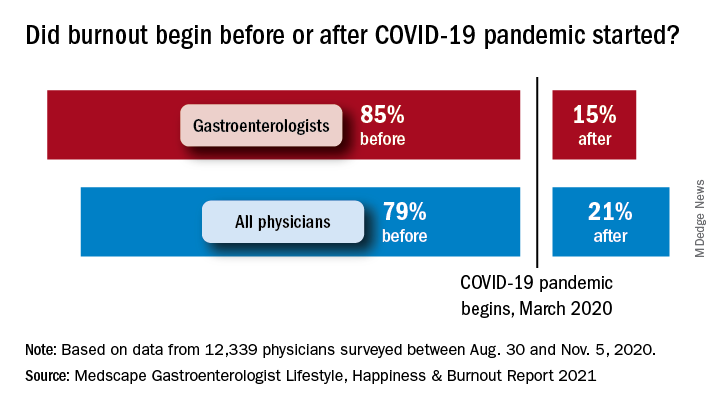
The two pandemic-related contributors included in the survey were near the bottom of the list for gastroenterologists: stress from social distancing/societal issues (15%) and stress related to treating COVID-19 patients (8%), based on data for the 12,339 physicians – of whom about 2% were GIs – polled from Aug. 30 to Nov. 5, 2020.
To deal with their burnout, many gastroenterologists are exercising – at least 51% of them, anyway. Other popular coping mechanisms include talking with family members and close friends (39%), playing or listening to music (38%), isolating themselves from others (36%), and sleeping (26%). For all physicians, the top choices were exercise (48%), talking with family members/friends (43%), and isolation (43%).
When the subject of professional help was raised, a large majority (84%) of GIs planned to forgo such care. That information was not available for physicians as a group, but 70% of internists agreed, as did 83% of nephrologists, 80% of cardiologists, 80% of oncologists, 89% of urologists, and 80% of general surgeons.
A majority of gastroenterologists (58%) said that their symptoms weren’t severe enough to warrant such help, but 38% said they were too busy, and 11% didn’t want to risk disclosure. Some physicians commented on their own situations:
- “I have no energy when I get home and I feel like I’m ignoring my family, but I need to decompress and process what I dealt with during the day” (oncologist).
- “I can’t do the things that I enjoy to relieve stress, such as traveling. My hair is falling out because I can’t destress” (ob.gyn.).
- “I’m tired and discouraged. It stresses my marriage. I have a hard time getting out of bed in the morning. I count the days until Friday” (psychiatrist).