User login
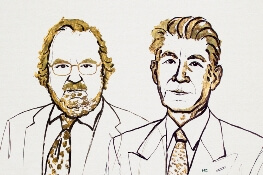
Two immunologists receive Nobel Prize in medicine
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
FDA lifts partial hold on tazemetostat trials
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
FDA Approves Galcanezumab for Migraine Prevention
The treatment is the third anti-CGRP antibody to receive regulatory approval.
ROCKVILLE, MD—The FDA has approved galcanezumab-gnlm (Emgality) for the preventive treatment of migraine in adults. Eli Lilly and Company manufactures the therapy. Emgality is the third calcitonin gene-related peptide (CGRP) antagonist to receive regulatory approval.
The approval is based on the results of three phase III clinical trials: EVOLVE-1, EVOLVE-2, and REGAIN. EVOLVE-1 and EVOLVE-2 were six-month, double-blind, placebo-controlled studies that included adults with episodic migraine. REGAIN was a three-month, double-blind, placebo-controlled study of adults with chronic migraine. The primary end point of all three trials was mean change from baseline in the number of monthly headache days.
In all trials, patients received either placebo, 120 mg of galcanezumab-gnlm after an initial loading dose of 240 mg, or 240 mg of galcanezumab-gnlm. In EVOLVE-1 and EVOLVE-2, people who received galcanezumab-gnlm had significantly fewer headache days per month than people who received placebo, and those who received galcanezumab-gnlm were also more likely to achieve a 50%, 75%, and 100% reduction in headache days.
In REGAIN, patients who received galcanezumab-gnlm experienced fewer monthly headache days than those who received placebo and were more likely to achieve a 50% reduction in headache days. There was no difference between groups in the likelihood of achieving a 75% or 100% reduction.
The recommended dosage, according to the label, is a monthly, 120-mg subcutaneous injection with an initial loading dose of 240 mg. The most common adverse event associated with galcanezumab-gnlm is injection-site reaction.
Galcanezumab-gnlm is under final review by the European Commission for approval in Europe.
—Lucas Franki
The treatment is the third anti-CGRP antibody to receive regulatory approval.
The treatment is the third anti-CGRP antibody to receive regulatory approval.
ROCKVILLE, MD—The FDA has approved galcanezumab-gnlm (Emgality) for the preventive treatment of migraine in adults. Eli Lilly and Company manufactures the therapy. Emgality is the third calcitonin gene-related peptide (CGRP) antagonist to receive regulatory approval.
The approval is based on the results of three phase III clinical trials: EVOLVE-1, EVOLVE-2, and REGAIN. EVOLVE-1 and EVOLVE-2 were six-month, double-blind, placebo-controlled studies that included adults with episodic migraine. REGAIN was a three-month, double-blind, placebo-controlled study of adults with chronic migraine. The primary end point of all three trials was mean change from baseline in the number of monthly headache days.
In all trials, patients received either placebo, 120 mg of galcanezumab-gnlm after an initial loading dose of 240 mg, or 240 mg of galcanezumab-gnlm. In EVOLVE-1 and EVOLVE-2, people who received galcanezumab-gnlm had significantly fewer headache days per month than people who received placebo, and those who received galcanezumab-gnlm were also more likely to achieve a 50%, 75%, and 100% reduction in headache days.
In REGAIN, patients who received galcanezumab-gnlm experienced fewer monthly headache days than those who received placebo and were more likely to achieve a 50% reduction in headache days. There was no difference between groups in the likelihood of achieving a 75% or 100% reduction.
The recommended dosage, according to the label, is a monthly, 120-mg subcutaneous injection with an initial loading dose of 240 mg. The most common adverse event associated with galcanezumab-gnlm is injection-site reaction.
Galcanezumab-gnlm is under final review by the European Commission for approval in Europe.
—Lucas Franki
ROCKVILLE, MD—The FDA has approved galcanezumab-gnlm (Emgality) for the preventive treatment of migraine in adults. Eli Lilly and Company manufactures the therapy. Emgality is the third calcitonin gene-related peptide (CGRP) antagonist to receive regulatory approval.
The approval is based on the results of three phase III clinical trials: EVOLVE-1, EVOLVE-2, and REGAIN. EVOLVE-1 and EVOLVE-2 were six-month, double-blind, placebo-controlled studies that included adults with episodic migraine. REGAIN was a three-month, double-blind, placebo-controlled study of adults with chronic migraine. The primary end point of all three trials was mean change from baseline in the number of monthly headache days.
In all trials, patients received either placebo, 120 mg of galcanezumab-gnlm after an initial loading dose of 240 mg, or 240 mg of galcanezumab-gnlm. In EVOLVE-1 and EVOLVE-2, people who received galcanezumab-gnlm had significantly fewer headache days per month than people who received placebo, and those who received galcanezumab-gnlm were also more likely to achieve a 50%, 75%, and 100% reduction in headache days.
In REGAIN, patients who received galcanezumab-gnlm experienced fewer monthly headache days than those who received placebo and were more likely to achieve a 50% reduction in headache days. There was no difference between groups in the likelihood of achieving a 75% or 100% reduction.
The recommended dosage, according to the label, is a monthly, 120-mg subcutaneous injection with an initial loading dose of 240 mg. The most common adverse event associated with galcanezumab-gnlm is injection-site reaction.
Galcanezumab-gnlm is under final review by the European Commission for approval in Europe.
—Lucas Franki
New MS Subtype Shows Absence of Cerebral White Matter Demyelination
A new subtype of multiple sclerosis (MS) called myelocortical MS is characterized by demyelination only in the spinal cord and cerebral cortex and not in the cerebral white matter, according to a study published online ahead of print August 21 in Lancet Neurology. The findings are based on an examination of the brains and spinal cords of 100 patients who died of MS.
Bruce D. Trapp, PhD, the Morris R. and Ruth V. Graham Endowed Chair in Biomedical Research at the Lerner Research Institute at the Cleveland Clinic in Ohio, and his coauthors said that while the demyelination of cerebral white matter is a pathologic hallmark of MS, previous research has found that only around half of cerebral T2-weighted hyperintense white matter lesions are demyelinated, and these lesions account for less than a third of variance in the rate of brain atrophy.
“In the absence of specific MRI metrics for demyelination, the relationship between cerebral white-matter demyelination and neurodegeneration remains speculative,” they said.
In this study, researchers scanned the brains with MRI before autopsy, then took centimeter-thick hemispheric slices to study the white-matter lesions. They identified 12 individuals as having what they describe as myelocortical MS, characterized by the absence of areas of cerebral white-matter discoloration indicative of demyelinated lesions.
The authors then compared these individuals with 12 individuals with typical MS matched by age, sex, MRI protocol, MS disease subtype, disease duration, and Expanded Disability Status Scale score.
Not Typical MS
They found that while individuals with myelocortical MS did not have demyelinated lesions in the cerebral white matter, they had areas of demyelinated lesions in the cerebral cortex similar to those of individuals with typical MS (median 4.45% vs 9.74%, respectively). However, the individuals with myelocortical MS had a significantly smaller area of spinal cord demyelination (median 3.81% vs 13.81%).
Individuals with myelocortical MS also had significantly lower mean cortical neuronal densities, compared with healthy control brains, in layer III, layer V, and layer VI. But individuals with typical MS only had a lower cortical neuronal density in layer V when compared with controls.
Dr. Trapp and colleagues also saw that in typical MS, neuronal density decreased as the area of brain white-matter demyelination increased. However, this negative linear correlation was not seen in myelocortical MS.
On MRI, researchers were still able to see abnormalities in the cerebral white matter in individuals with myelocortical MS, in T2-weighted, T1-weighted, and magnetization transfer ratios (MTR) images. They also found similar total T2-weighted and T1-weighted lesion volumes in individuals with myelocortical MS and those with typical MS, although individuals with typical MS had significantly greater MTR lesion volumes.
The Hallmarks of Myelocortical MS
“We propose that myelocortical MS is characterized by spinal cord demyelination, subpial cortical demyelination, and an absence of cerebral white-matter demyelination,” Dr. Trapp and colleagues wrote. “Our findings indicate that abnormal cerebral white-matter T2-T1-MTR regions of interest are not always demyelinated, and this pathologic evidence suggests that cerebral white-matter demyelination and cortical neuronal degeneration can be independent events in myelocortical MS.”
The authors acknowledged that one limitation of their study may have been selection bias, as all the patients in the study died from complications of advanced MS. They suggested that it was therefore not appropriate to conclude that the prevalence of myelocortical MS seen in their sample would be similar across the entire MS population, nor were the findings likely to apply to pateints with earlier stage disease.
The study received funding from the NIH and the National MS Society. One author is an employee of Renovo Neural, and three authors are employees of Biogen. One author declared a pending patent related to automated lesion segmentation from MRI images, and four authors declared funding, fees, and nonfinancial support from pharmaceutical companies.
—Bianca Nogrady
Suggested Reading
Trapp BD, Vignos M, Dudman J, et al. Cortical neuronal densities and cerebral white matter demyelination in multiple sclerosis: a retrospective study. Lancet Neurol. 2018 Aug 21 [Epub ahead of print].
A new subtype of multiple sclerosis (MS) called myelocortical MS is characterized by demyelination only in the spinal cord and cerebral cortex and not in the cerebral white matter, according to a study published online ahead of print August 21 in Lancet Neurology. The findings are based on an examination of the brains and spinal cords of 100 patients who died of MS.
Bruce D. Trapp, PhD, the Morris R. and Ruth V. Graham Endowed Chair in Biomedical Research at the Lerner Research Institute at the Cleveland Clinic in Ohio, and his coauthors said that while the demyelination of cerebral white matter is a pathologic hallmark of MS, previous research has found that only around half of cerebral T2-weighted hyperintense white matter lesions are demyelinated, and these lesions account for less than a third of variance in the rate of brain atrophy.
“In the absence of specific MRI metrics for demyelination, the relationship between cerebral white-matter demyelination and neurodegeneration remains speculative,” they said.
In this study, researchers scanned the brains with MRI before autopsy, then took centimeter-thick hemispheric slices to study the white-matter lesions. They identified 12 individuals as having what they describe as myelocortical MS, characterized by the absence of areas of cerebral white-matter discoloration indicative of demyelinated lesions.
The authors then compared these individuals with 12 individuals with typical MS matched by age, sex, MRI protocol, MS disease subtype, disease duration, and Expanded Disability Status Scale score.
Not Typical MS
They found that while individuals with myelocortical MS did not have demyelinated lesions in the cerebral white matter, they had areas of demyelinated lesions in the cerebral cortex similar to those of individuals with typical MS (median 4.45% vs 9.74%, respectively). However, the individuals with myelocortical MS had a significantly smaller area of spinal cord demyelination (median 3.81% vs 13.81%).
Individuals with myelocortical MS also had significantly lower mean cortical neuronal densities, compared with healthy control brains, in layer III, layer V, and layer VI. But individuals with typical MS only had a lower cortical neuronal density in layer V when compared with controls.
Dr. Trapp and colleagues also saw that in typical MS, neuronal density decreased as the area of brain white-matter demyelination increased. However, this negative linear correlation was not seen in myelocortical MS.
On MRI, researchers were still able to see abnormalities in the cerebral white matter in individuals with myelocortical MS, in T2-weighted, T1-weighted, and magnetization transfer ratios (MTR) images. They also found similar total T2-weighted and T1-weighted lesion volumes in individuals with myelocortical MS and those with typical MS, although individuals with typical MS had significantly greater MTR lesion volumes.
The Hallmarks of Myelocortical MS
“We propose that myelocortical MS is characterized by spinal cord demyelination, subpial cortical demyelination, and an absence of cerebral white-matter demyelination,” Dr. Trapp and colleagues wrote. “Our findings indicate that abnormal cerebral white-matter T2-T1-MTR regions of interest are not always demyelinated, and this pathologic evidence suggests that cerebral white-matter demyelination and cortical neuronal degeneration can be independent events in myelocortical MS.”
The authors acknowledged that one limitation of their study may have been selection bias, as all the patients in the study died from complications of advanced MS. They suggested that it was therefore not appropriate to conclude that the prevalence of myelocortical MS seen in their sample would be similar across the entire MS population, nor were the findings likely to apply to pateints with earlier stage disease.
The study received funding from the NIH and the National MS Society. One author is an employee of Renovo Neural, and three authors are employees of Biogen. One author declared a pending patent related to automated lesion segmentation from MRI images, and four authors declared funding, fees, and nonfinancial support from pharmaceutical companies.
—Bianca Nogrady
Suggested Reading
Trapp BD, Vignos M, Dudman J, et al. Cortical neuronal densities and cerebral white matter demyelination in multiple sclerosis: a retrospective study. Lancet Neurol. 2018 Aug 21 [Epub ahead of print].
A new subtype of multiple sclerosis (MS) called myelocortical MS is characterized by demyelination only in the spinal cord and cerebral cortex and not in the cerebral white matter, according to a study published online ahead of print August 21 in Lancet Neurology. The findings are based on an examination of the brains and spinal cords of 100 patients who died of MS.
Bruce D. Trapp, PhD, the Morris R. and Ruth V. Graham Endowed Chair in Biomedical Research at the Lerner Research Institute at the Cleveland Clinic in Ohio, and his coauthors said that while the demyelination of cerebral white matter is a pathologic hallmark of MS, previous research has found that only around half of cerebral T2-weighted hyperintense white matter lesions are demyelinated, and these lesions account for less than a third of variance in the rate of brain atrophy.
“In the absence of specific MRI metrics for demyelination, the relationship between cerebral white-matter demyelination and neurodegeneration remains speculative,” they said.
In this study, researchers scanned the brains with MRI before autopsy, then took centimeter-thick hemispheric slices to study the white-matter lesions. They identified 12 individuals as having what they describe as myelocortical MS, characterized by the absence of areas of cerebral white-matter discoloration indicative of demyelinated lesions.
The authors then compared these individuals with 12 individuals with typical MS matched by age, sex, MRI protocol, MS disease subtype, disease duration, and Expanded Disability Status Scale score.
Not Typical MS
They found that while individuals with myelocortical MS did not have demyelinated lesions in the cerebral white matter, they had areas of demyelinated lesions in the cerebral cortex similar to those of individuals with typical MS (median 4.45% vs 9.74%, respectively). However, the individuals with myelocortical MS had a significantly smaller area of spinal cord demyelination (median 3.81% vs 13.81%).
Individuals with myelocortical MS also had significantly lower mean cortical neuronal densities, compared with healthy control brains, in layer III, layer V, and layer VI. But individuals with typical MS only had a lower cortical neuronal density in layer V when compared with controls.
Dr. Trapp and colleagues also saw that in typical MS, neuronal density decreased as the area of brain white-matter demyelination increased. However, this negative linear correlation was not seen in myelocortical MS.
On MRI, researchers were still able to see abnormalities in the cerebral white matter in individuals with myelocortical MS, in T2-weighted, T1-weighted, and magnetization transfer ratios (MTR) images. They also found similar total T2-weighted and T1-weighted lesion volumes in individuals with myelocortical MS and those with typical MS, although individuals with typical MS had significantly greater MTR lesion volumes.
The Hallmarks of Myelocortical MS
“We propose that myelocortical MS is characterized by spinal cord demyelination, subpial cortical demyelination, and an absence of cerebral white-matter demyelination,” Dr. Trapp and colleagues wrote. “Our findings indicate that abnormal cerebral white-matter T2-T1-MTR regions of interest are not always demyelinated, and this pathologic evidence suggests that cerebral white-matter demyelination and cortical neuronal degeneration can be independent events in myelocortical MS.”
The authors acknowledged that one limitation of their study may have been selection bias, as all the patients in the study died from complications of advanced MS. They suggested that it was therefore not appropriate to conclude that the prevalence of myelocortical MS seen in their sample would be similar across the entire MS population, nor were the findings likely to apply to pateints with earlier stage disease.
The study received funding from the NIH and the National MS Society. One author is an employee of Renovo Neural, and three authors are employees of Biogen. One author declared a pending patent related to automated lesion segmentation from MRI images, and four authors declared funding, fees, and nonfinancial support from pharmaceutical companies.
—Bianca Nogrady
Suggested Reading
Trapp BD, Vignos M, Dudman J, et al. Cortical neuronal densities and cerebral white matter demyelination in multiple sclerosis: a retrospective study. Lancet Neurol. 2018 Aug 21 [Epub ahead of print].
Cardiovascular Health and Cognitive Decline: What Is the Connection?
Maintaining cardiovascular health may reduce white matter hyperintensities and decrease the risk of dementia.
Optimal measures of cardiovascular health are associated with brain health in adults, according to two studies published in the August 21 issue of JAMA.
In a French population-based cohort study, adults ages 65 and older with more cardiovascular health measures at ideal levels had a lower risk of dementia and lower rates of cognitive decline than did those with fewer optimal cardiovascular measures, such as blood pressure and physical activity.
In addition, a preliminary, cross-sectional study of younger adults found that the number of modifiable cardiovascular risk factors at recommended levels was associated with brain vessel structure and function and the number of white matter hyperintensities.
“These two studies convey an immediately actionable message to clinicians, policy makers, and patients,” said Jeffrey L. Saver, MD, and Mary Cushman, MD, in an accompanying editorial. “Available evidence indicates that to achieve a lifetime of robust brain health free of dementia, it is never too early or too late to strive for attainment of ideal cardiovascular health.” Dr. Saver is a Professor of Neurology and Director of the Stroke Center at the University of California, Los Angeles. Dr. Cushman is a Professor of Medicine and Pathology at Larner College of Medicine at the University of Vermont in Burlington.
Cardiovascular Health in Older Age
Vascular dementia is the second most common neuropathologic basis of dementia, after Alzheimer’s disease, and “most cases of dementia arise from a combination of [Alzheimer’s disease] and cerebrovascular pathology,” the editorialists noted. Studies have suggested a connection between cardiovascular health and dementia, but the evidence is limited.
Cécilia Samieri, PhD, a Senior Researcher at the Bordeaux Population Health Research Center at the Université de Bordeaux in France, and colleagues studied people age 65 and older from Bordeaux, Dijon, and Montpellier, France, to examine the association between cardiovascular health level and risk of dementia and cognitive decline in older adults.
The study included 6,626 people without a history of cardiovascular disease or dementia at baseline. Participants underwent in-person neuropsychologic testing between January 1999 and July 2016 and systematic detection of incident dementia. Participants had a mean age of 73.7, and 63.4% were women.
The investigators defined cardiovascular health using a seven-item tool from the American Heart Association (AHA). They determined the number of the AHA’s Life’s Simple Seven metrics that were at recommended levels (ie, nonsmoking, BMI < 25, regular physical activity, eating fish at least twice per week and fruits and vegetables at least three times per day, cholesterol < 200 mg/dL [untreated], fasting glucose < 100 mg/dL [untreated], and blood pressure < 120/80 mm Hg [untreated]).
Approximately 36.5% of the cohort had zero, one, or two optimal health metrics, 57.1% had three or four optimal health metrics, and 6.5% had five, six, or seven optimal health metrics.
During an average follow-up of 8.5 years, 745 participants developed dementia. Among participants with zero or one health metrics at optimal levels at baseline, the incidence rate of dementia was 1.76 per 100 person-years. Compared with this rate, the incidence rate per 100 person-years was 0.26 lower for participants with two optimal health metrics, 0.59 lower for participants with three optimal health metrics, 0.43 lower for participants with four optimal health metrics, 0.93 lower for participants with five optimal health metrics, and 0.96 lower for participants with six or seven optimal health metrics.
“In multivariable models, the hazard ratios for dementia were 0.90 per additional optimal metric,” the investigators said. “The study results support the recent recommendations of the AHA and the American Stroke Association for the promotion of the Life’s Simple Seven tool.”
Cerebrovascular Structure and Function in Young Adults
Wilby Williamson, BMBS
The researchers assessed patients’ cerebral vessel density, caliber, and tortuosity and brain white matter hyperintensity lesion count. In a subgroup of 52 participants, they assessed cerebral blood flow.
The researchers determined for each participant how many of eight modifiable risk factors were at recommended levels (ie, BMI < 25, highest tertile of cardiovascular fitness or physical activity, alcohol consumption < eight drinks per week, nonsmoker for more than six months, blood pressure on awake ambulatory monitoring < 130/80 mm Hg, a nonhypertensive diastolic response to exercise [ie, peak diastolic blood pressure < 90 mm Hg], total cholesterol < 200 mg/dL, and fasting glucose < 100 mg/dL).
On average, participants had six of the eight modifiable cardiovascular risk factors at recommended levels.
In multivariable models, cardiovascular risk factors were associated with cerebrovascular structure and the number of white matter hyperintensities. “For each additional modifiable risk factor categorized as healthy, vessel density was greater by 0.3 vessels/cm3, vessel caliber was greater by 8 μm, and white matter hyperintensity lesions were fewer by 1.6 lesions. Among the 52 participants with available data, cerebral blood flow varied with vessel density and was 2.5 mL/100 g/min higher for each healthier category of a modifiable risk factor,” Dr. Williamson and colleagues said.
The findings suggest that “some individuals may be starting to diverge to different risk trajectories for brain vascular health in early adulthood,” the researchers said. The study was exploratory, however, and follow-up studies are needed to determine the clinical significance of these findings, they said.
“The magnitude of changes was generally much less than would be expected to produce clinical symptoms such as cognitive impairment or gait difficulty,” said Drs. Saver and Cushman. The changes, however, “may portend more substantial abnormalities later in life,” they said. “Even during the late-life period, when septuagenarians become octogenarians, cardiovascular health is associated with substantial differences in cognitive trajectory and dementia onset.”
—Jake Remaly
Suggested Reading
Samieri C, Perier MC, Gaye B, et al. Association of cardiovascular health level in older age with cognitive decline and incident dementia. JAMA. 2018;320(7):657-664.
Saver JL, Cushman M. Striving for ideal cardiovascular and brain health: It is never too early or too late. JAMA. 2018; 320(7):645-647.
Williamson W, Lewandowski AJ, Forkert ND, et al. Association of cardiovascular risk factors with MRI indices of cerebrovascular structure and function and white matter hyperintensities in young adults. JAMA. 2018;320(7):665-673.
Maintaining cardiovascular health may reduce white matter hyperintensities and decrease the risk of dementia.
Maintaining cardiovascular health may reduce white matter hyperintensities and decrease the risk of dementia.
Optimal measures of cardiovascular health are associated with brain health in adults, according to two studies published in the August 21 issue of JAMA.
In a French population-based cohort study, adults ages 65 and older with more cardiovascular health measures at ideal levels had a lower risk of dementia and lower rates of cognitive decline than did those with fewer optimal cardiovascular measures, such as blood pressure and physical activity.
In addition, a preliminary, cross-sectional study of younger adults found that the number of modifiable cardiovascular risk factors at recommended levels was associated with brain vessel structure and function and the number of white matter hyperintensities.
“These two studies convey an immediately actionable message to clinicians, policy makers, and patients,” said Jeffrey L. Saver, MD, and Mary Cushman, MD, in an accompanying editorial. “Available evidence indicates that to achieve a lifetime of robust brain health free of dementia, it is never too early or too late to strive for attainment of ideal cardiovascular health.” Dr. Saver is a Professor of Neurology and Director of the Stroke Center at the University of California, Los Angeles. Dr. Cushman is a Professor of Medicine and Pathology at Larner College of Medicine at the University of Vermont in Burlington.
Cardiovascular Health in Older Age
Vascular dementia is the second most common neuropathologic basis of dementia, after Alzheimer’s disease, and “most cases of dementia arise from a combination of [Alzheimer’s disease] and cerebrovascular pathology,” the editorialists noted. Studies have suggested a connection between cardiovascular health and dementia, but the evidence is limited.
Cécilia Samieri, PhD, a Senior Researcher at the Bordeaux Population Health Research Center at the Université de Bordeaux in France, and colleagues studied people age 65 and older from Bordeaux, Dijon, and Montpellier, France, to examine the association between cardiovascular health level and risk of dementia and cognitive decline in older adults.
The study included 6,626 people without a history of cardiovascular disease or dementia at baseline. Participants underwent in-person neuropsychologic testing between January 1999 and July 2016 and systematic detection of incident dementia. Participants had a mean age of 73.7, and 63.4% were women.
The investigators defined cardiovascular health using a seven-item tool from the American Heart Association (AHA). They determined the number of the AHA’s Life’s Simple Seven metrics that were at recommended levels (ie, nonsmoking, BMI < 25, regular physical activity, eating fish at least twice per week and fruits and vegetables at least three times per day, cholesterol < 200 mg/dL [untreated], fasting glucose < 100 mg/dL [untreated], and blood pressure < 120/80 mm Hg [untreated]).
Approximately 36.5% of the cohort had zero, one, or two optimal health metrics, 57.1% had three or four optimal health metrics, and 6.5% had five, six, or seven optimal health metrics.
During an average follow-up of 8.5 years, 745 participants developed dementia. Among participants with zero or one health metrics at optimal levels at baseline, the incidence rate of dementia was 1.76 per 100 person-years. Compared with this rate, the incidence rate per 100 person-years was 0.26 lower for participants with two optimal health metrics, 0.59 lower for participants with three optimal health metrics, 0.43 lower for participants with four optimal health metrics, 0.93 lower for participants with five optimal health metrics, and 0.96 lower for participants with six or seven optimal health metrics.
“In multivariable models, the hazard ratios for dementia were 0.90 per additional optimal metric,” the investigators said. “The study results support the recent recommendations of the AHA and the American Stroke Association for the promotion of the Life’s Simple Seven tool.”
Cerebrovascular Structure and Function in Young Adults
Wilby Williamson, BMBS
The researchers assessed patients’ cerebral vessel density, caliber, and tortuosity and brain white matter hyperintensity lesion count. In a subgroup of 52 participants, they assessed cerebral blood flow.
The researchers determined for each participant how many of eight modifiable risk factors were at recommended levels (ie, BMI < 25, highest tertile of cardiovascular fitness or physical activity, alcohol consumption < eight drinks per week, nonsmoker for more than six months, blood pressure on awake ambulatory monitoring < 130/80 mm Hg, a nonhypertensive diastolic response to exercise [ie, peak diastolic blood pressure < 90 mm Hg], total cholesterol < 200 mg/dL, and fasting glucose < 100 mg/dL).
On average, participants had six of the eight modifiable cardiovascular risk factors at recommended levels.
In multivariable models, cardiovascular risk factors were associated with cerebrovascular structure and the number of white matter hyperintensities. “For each additional modifiable risk factor categorized as healthy, vessel density was greater by 0.3 vessels/cm3, vessel caliber was greater by 8 μm, and white matter hyperintensity lesions were fewer by 1.6 lesions. Among the 52 participants with available data, cerebral blood flow varied with vessel density and was 2.5 mL/100 g/min higher for each healthier category of a modifiable risk factor,” Dr. Williamson and colleagues said.
The findings suggest that “some individuals may be starting to diverge to different risk trajectories for brain vascular health in early adulthood,” the researchers said. The study was exploratory, however, and follow-up studies are needed to determine the clinical significance of these findings, they said.
“The magnitude of changes was generally much less than would be expected to produce clinical symptoms such as cognitive impairment or gait difficulty,” said Drs. Saver and Cushman. The changes, however, “may portend more substantial abnormalities later in life,” they said. “Even during the late-life period, when septuagenarians become octogenarians, cardiovascular health is associated with substantial differences in cognitive trajectory and dementia onset.”
—Jake Remaly
Suggested Reading
Samieri C, Perier MC, Gaye B, et al. Association of cardiovascular health level in older age with cognitive decline and incident dementia. JAMA. 2018;320(7):657-664.
Saver JL, Cushman M. Striving for ideal cardiovascular and brain health: It is never too early or too late. JAMA. 2018; 320(7):645-647.
Williamson W, Lewandowski AJ, Forkert ND, et al. Association of cardiovascular risk factors with MRI indices of cerebrovascular structure and function and white matter hyperintensities in young adults. JAMA. 2018;320(7):665-673.
Optimal measures of cardiovascular health are associated with brain health in adults, according to two studies published in the August 21 issue of JAMA.
In a French population-based cohort study, adults ages 65 and older with more cardiovascular health measures at ideal levels had a lower risk of dementia and lower rates of cognitive decline than did those with fewer optimal cardiovascular measures, such as blood pressure and physical activity.
In addition, a preliminary, cross-sectional study of younger adults found that the number of modifiable cardiovascular risk factors at recommended levels was associated with brain vessel structure and function and the number of white matter hyperintensities.
“These two studies convey an immediately actionable message to clinicians, policy makers, and patients,” said Jeffrey L. Saver, MD, and Mary Cushman, MD, in an accompanying editorial. “Available evidence indicates that to achieve a lifetime of robust brain health free of dementia, it is never too early or too late to strive for attainment of ideal cardiovascular health.” Dr. Saver is a Professor of Neurology and Director of the Stroke Center at the University of California, Los Angeles. Dr. Cushman is a Professor of Medicine and Pathology at Larner College of Medicine at the University of Vermont in Burlington.
Cardiovascular Health in Older Age
Vascular dementia is the second most common neuropathologic basis of dementia, after Alzheimer’s disease, and “most cases of dementia arise from a combination of [Alzheimer’s disease] and cerebrovascular pathology,” the editorialists noted. Studies have suggested a connection between cardiovascular health and dementia, but the evidence is limited.
Cécilia Samieri, PhD, a Senior Researcher at the Bordeaux Population Health Research Center at the Université de Bordeaux in France, and colleagues studied people age 65 and older from Bordeaux, Dijon, and Montpellier, France, to examine the association between cardiovascular health level and risk of dementia and cognitive decline in older adults.
The study included 6,626 people without a history of cardiovascular disease or dementia at baseline. Participants underwent in-person neuropsychologic testing between January 1999 and July 2016 and systematic detection of incident dementia. Participants had a mean age of 73.7, and 63.4% were women.
The investigators defined cardiovascular health using a seven-item tool from the American Heart Association (AHA). They determined the number of the AHA’s Life’s Simple Seven metrics that were at recommended levels (ie, nonsmoking, BMI < 25, regular physical activity, eating fish at least twice per week and fruits and vegetables at least three times per day, cholesterol < 200 mg/dL [untreated], fasting glucose < 100 mg/dL [untreated], and blood pressure < 120/80 mm Hg [untreated]).
Approximately 36.5% of the cohort had zero, one, or two optimal health metrics, 57.1% had three or four optimal health metrics, and 6.5% had five, six, or seven optimal health metrics.
During an average follow-up of 8.5 years, 745 participants developed dementia. Among participants with zero or one health metrics at optimal levels at baseline, the incidence rate of dementia was 1.76 per 100 person-years. Compared with this rate, the incidence rate per 100 person-years was 0.26 lower for participants with two optimal health metrics, 0.59 lower for participants with three optimal health metrics, 0.43 lower for participants with four optimal health metrics, 0.93 lower for participants with five optimal health metrics, and 0.96 lower for participants with six or seven optimal health metrics.
“In multivariable models, the hazard ratios for dementia were 0.90 per additional optimal metric,” the investigators said. “The study results support the recent recommendations of the AHA and the American Stroke Association for the promotion of the Life’s Simple Seven tool.”
Cerebrovascular Structure and Function in Young Adults
Wilby Williamson, BMBS
The researchers assessed patients’ cerebral vessel density, caliber, and tortuosity and brain white matter hyperintensity lesion count. In a subgroup of 52 participants, they assessed cerebral blood flow.
The researchers determined for each participant how many of eight modifiable risk factors were at recommended levels (ie, BMI < 25, highest tertile of cardiovascular fitness or physical activity, alcohol consumption < eight drinks per week, nonsmoker for more than six months, blood pressure on awake ambulatory monitoring < 130/80 mm Hg, a nonhypertensive diastolic response to exercise [ie, peak diastolic blood pressure < 90 mm Hg], total cholesterol < 200 mg/dL, and fasting glucose < 100 mg/dL).
On average, participants had six of the eight modifiable cardiovascular risk factors at recommended levels.
In multivariable models, cardiovascular risk factors were associated with cerebrovascular structure and the number of white matter hyperintensities. “For each additional modifiable risk factor categorized as healthy, vessel density was greater by 0.3 vessels/cm3, vessel caliber was greater by 8 μm, and white matter hyperintensity lesions were fewer by 1.6 lesions. Among the 52 participants with available data, cerebral blood flow varied with vessel density and was 2.5 mL/100 g/min higher for each healthier category of a modifiable risk factor,” Dr. Williamson and colleagues said.
The findings suggest that “some individuals may be starting to diverge to different risk trajectories for brain vascular health in early adulthood,” the researchers said. The study was exploratory, however, and follow-up studies are needed to determine the clinical significance of these findings, they said.
“The magnitude of changes was generally much less than would be expected to produce clinical symptoms such as cognitive impairment or gait difficulty,” said Drs. Saver and Cushman. The changes, however, “may portend more substantial abnormalities later in life,” they said. “Even during the late-life period, when septuagenarians become octogenarians, cardiovascular health is associated with substantial differences in cognitive trajectory and dementia onset.”
—Jake Remaly
Suggested Reading
Samieri C, Perier MC, Gaye B, et al. Association of cardiovascular health level in older age with cognitive decline and incident dementia. JAMA. 2018;320(7):657-664.
Saver JL, Cushman M. Striving for ideal cardiovascular and brain health: It is never too early or too late. JAMA. 2018; 320(7):645-647.
Williamson W, Lewandowski AJ, Forkert ND, et al. Association of cardiovascular risk factors with MRI indices of cerebrovascular structure and function and white matter hyperintensities in young adults. JAMA. 2018;320(7):665-673.
Alan M. Rapoport, MD, on Medication Overuse Headache
Neurology Reviews recently shared two poll questions with our Facebook followers about treatment medication overuse headache (MOH). I was very interested to see the results of our poll. While the number of responses was somewhat low, we do get some sense of what respondents are saying. In this commentary, I will first tell you my perspective on the answers and then we will see what some other headache specialists say about the answers to these questions.
Poll Results:
Can MOH be treated with preventive medications without detoxification?
33 votes
YES, 39%
NO, 61%
Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor) without detoxification?
26 votes
YES, 38%
NO, 62%
My Commentary:
Let me explain in more detail my thoughts on the first question, “Can MOH be treated with preventive medications without detoxification?”
If a patient had the diagnosis of MOH – meaning 15 or more headache days per month for at least 3 months, with use of stronger medications (triptans, ergots, opiates, butalbital-containing medications) for 10 days per month or milder treatment (aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]) for 15 days per month – can they improve by being put on a traditional preventive medication without intentionally reducing their overused acute medications by a detoxification protocol ordered by a doctor or nurse?
Only 39% of our audience said yes. Yet some studies have shown that patients placed on onabotulinumtoxinA or topiramate might improve without them going through a detoxification of the overused medications. As a physician, I would suggest simultaneously decreasing in their acute medications. I think in some cases this approach creates additional improvement and makes the patient feel better. It would be better for their quality of life, as well as for their kidneys and possibly even their brains.
Here are my thoughts on the second question, “Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor), without detoxification?”
If a patient has MOH, can you expect them to improve after being placed on 1 of the 4 monoclonal antibodies to CGRP ligand or its receptor – all of which are either recently approved or currently in development – without suggesting that they decrease their overused acute care medications? Note that erenumab (Aimovig-aaoe) has been approved by the FDA and marketed as of the time of this writing; we expect 2 more products to be approved very soon.
Almost an identical percentage of our audience (38%) said yes. There is evidence in published clinical trials that those patients given these new medications did about as well with or without the presence of MOH, and both groups did better than the placebo patients. Note that most trials prohibited overuse of opiates and butalbital.
I am a firm believer of detoxifying patients from their overused over-the-counter (OTC) or prescription medications. I believe that opiates and butalbital-containing medications, when overused, are worse for patients than OTCs, NSAIDs, ergot and triptans, but all of these can cause MOH. There are many studies showing that both inpatient and outpatient detoxification alone can really help. However, it is difficult to detoxify patients and some refuse to try this approach.
So, what should we do as physicians? If a patient has MOH, I educate them, try to detoxify them slowly on an outpatient basis, and if I feel it will help, start them on a preventive medication, even before the detoxification begins so they can reach therapeutic levels. In the future, will I use one of the standard preventives, approved or off-label, for migraine prevention (beta blockers, topiramate and other anticonvulsants, antidepressants, angiotensin receptor blockers, onabotulinumtoxinA and others)? It remains to be seen. I am leaning towards the anti CGRP ligand and receptor monoclonal antibodies and preventive small molecule oral CGRP receptor blockers. While that might be enough to start with, I will continue explaining to my patients why they should actively begin a slow detoxification.
Let us see what some headache specialists said about both questions.
Robert Cowan, MD, FAAN:
There have been studies that show migraine can improve without the discontinuation of medication overuse. But that is not what the question asks. The question as posed is whether MOH can be treated with a preventive medication without detoxification. Since the diagnosis of MOH has, in the past, required the cessation of overuse leading to an improvement in the underlying headache, then technically, the answer would be “no.” But that being said, there is ample evidence that the number of headache days/months and other measures of headache can, in fact, improve with the introduction of a preventive, along with other measures such as lifestyle modification. The other ambiguity in the question has to do with what is meant by “detoxification.” Is this a hospital-based detox, or is a gradual decrease in the offending medicine in combination with the addition of a preventive, still considered “detoxification?” Also, does the response imply a sequential relationship between the detoxification and initiation of the preventive? Without further clarification, this response ratio to the question is very difficult to interpret.
There is animal data that suggests acute migraine medications may promote MOH in susceptible individuals through CGRP-dependent mechanisms and anti-CGRP antibodies may be useful for the MOH (Cephalalgia. 2017;37(6):560-570. doi: 10.1177/0333102416650702). While there are no published CGRP antibody studies that did not exclude MOH patients to my knowledge, an abstract by Silberstein et al at the recent AHS Scientific Meeting reported decreased use of overused medication with fremanazumab (Headache. 2018;58(S2):76-78).
Ira Turner, MD
There is clear data to suggest that it is not necessary to detoxify these patients before starting preventive therapy. This is true for the older and newer medications. In fact, not only do these preventive therapies still work in the presence of medication overuse, but they also help to reduce medication overuse. The one caveat that must be mentioned is that this may not apply to opiate overuse. Opiate over-users were excluded from these studies.
While it is of course our goal to reduce and stop acute medication overuse, it should not be done at the expense of delaying preventive therapy. In fact, it is desirable to do both simultaneously. This applies to oral preventive medications, botulinum toxin and CGRP monoclonal antibodies.
In view of this well-established data, it was quite surprising to me to see the results of the 2 polls cited. It seems as if we still have a lot of educating to do regarding migraine prevention in general and with medication overuse in migraine in particular.
Stewart Tepper, MD
Dr. Tepper did not have time to comment, but suggested we show you an abstract presented at the recent AHS meeting. It shows that erenumab-aaoe helps patients with MOH who have not been detoxified (Headache. 2018;58(S2):160-162).
###
Please write to us at Neurology Reviews Migraine Resource Center ([email protected]) with your opinions.
Alan M. Rapoport, MD
Editor-in-Chief
Migraine Resource Center
Clinical Professor of Neurology
The David Geffen School of Medicine at UCLA
Los Angeles, California
Neurology Reviews recently shared two poll questions with our Facebook followers about treatment medication overuse headache (MOH). I was very interested to see the results of our poll. While the number of responses was somewhat low, we do get some sense of what respondents are saying. In this commentary, I will first tell you my perspective on the answers and then we will see what some other headache specialists say about the answers to these questions.
Poll Results:
Can MOH be treated with preventive medications without detoxification?
33 votes
YES, 39%
NO, 61%
Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor) without detoxification?
26 votes
YES, 38%
NO, 62%
My Commentary:
Let me explain in more detail my thoughts on the first question, “Can MOH be treated with preventive medications without detoxification?”
If a patient had the diagnosis of MOH – meaning 15 or more headache days per month for at least 3 months, with use of stronger medications (triptans, ergots, opiates, butalbital-containing medications) for 10 days per month or milder treatment (aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]) for 15 days per month – can they improve by being put on a traditional preventive medication without intentionally reducing their overused acute medications by a detoxification protocol ordered by a doctor or nurse?
Only 39% of our audience said yes. Yet some studies have shown that patients placed on onabotulinumtoxinA or topiramate might improve without them going through a detoxification of the overused medications. As a physician, I would suggest simultaneously decreasing in their acute medications. I think in some cases this approach creates additional improvement and makes the patient feel better. It would be better for their quality of life, as well as for their kidneys and possibly even their brains.
Here are my thoughts on the second question, “Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor), without detoxification?”
If a patient has MOH, can you expect them to improve after being placed on 1 of the 4 monoclonal antibodies to CGRP ligand or its receptor – all of which are either recently approved or currently in development – without suggesting that they decrease their overused acute care medications? Note that erenumab (Aimovig-aaoe) has been approved by the FDA and marketed as of the time of this writing; we expect 2 more products to be approved very soon.
Almost an identical percentage of our audience (38%) said yes. There is evidence in published clinical trials that those patients given these new medications did about as well with or without the presence of MOH, and both groups did better than the placebo patients. Note that most trials prohibited overuse of opiates and butalbital.
I am a firm believer of detoxifying patients from their overused over-the-counter (OTC) or prescription medications. I believe that opiates and butalbital-containing medications, when overused, are worse for patients than OTCs, NSAIDs, ergot and triptans, but all of these can cause MOH. There are many studies showing that both inpatient and outpatient detoxification alone can really help. However, it is difficult to detoxify patients and some refuse to try this approach.
So, what should we do as physicians? If a patient has MOH, I educate them, try to detoxify them slowly on an outpatient basis, and if I feel it will help, start them on a preventive medication, even before the detoxification begins so they can reach therapeutic levels. In the future, will I use one of the standard preventives, approved or off-label, for migraine prevention (beta blockers, topiramate and other anticonvulsants, antidepressants, angiotensin receptor blockers, onabotulinumtoxinA and others)? It remains to be seen. I am leaning towards the anti CGRP ligand and receptor monoclonal antibodies and preventive small molecule oral CGRP receptor blockers. While that might be enough to start with, I will continue explaining to my patients why they should actively begin a slow detoxification.
Let us see what some headache specialists said about both questions.
Robert Cowan, MD, FAAN:
There have been studies that show migraine can improve without the discontinuation of medication overuse. But that is not what the question asks. The question as posed is whether MOH can be treated with a preventive medication without detoxification. Since the diagnosis of MOH has, in the past, required the cessation of overuse leading to an improvement in the underlying headache, then technically, the answer would be “no.” But that being said, there is ample evidence that the number of headache days/months and other measures of headache can, in fact, improve with the introduction of a preventive, along with other measures such as lifestyle modification. The other ambiguity in the question has to do with what is meant by “detoxification.” Is this a hospital-based detox, or is a gradual decrease in the offending medicine in combination with the addition of a preventive, still considered “detoxification?” Also, does the response imply a sequential relationship between the detoxification and initiation of the preventive? Without further clarification, this response ratio to the question is very difficult to interpret.
There is animal data that suggests acute migraine medications may promote MOH in susceptible individuals through CGRP-dependent mechanisms and anti-CGRP antibodies may be useful for the MOH (Cephalalgia. 2017;37(6):560-570. doi: 10.1177/0333102416650702). While there are no published CGRP antibody studies that did not exclude MOH patients to my knowledge, an abstract by Silberstein et al at the recent AHS Scientific Meeting reported decreased use of overused medication with fremanazumab (Headache. 2018;58(S2):76-78).
Ira Turner, MD
There is clear data to suggest that it is not necessary to detoxify these patients before starting preventive therapy. This is true for the older and newer medications. In fact, not only do these preventive therapies still work in the presence of medication overuse, but they also help to reduce medication overuse. The one caveat that must be mentioned is that this may not apply to opiate overuse. Opiate over-users were excluded from these studies.
While it is of course our goal to reduce and stop acute medication overuse, it should not be done at the expense of delaying preventive therapy. In fact, it is desirable to do both simultaneously. This applies to oral preventive medications, botulinum toxin and CGRP monoclonal antibodies.
In view of this well-established data, it was quite surprising to me to see the results of the 2 polls cited. It seems as if we still have a lot of educating to do regarding migraine prevention in general and with medication overuse in migraine in particular.
Stewart Tepper, MD
Dr. Tepper did not have time to comment, but suggested we show you an abstract presented at the recent AHS meeting. It shows that erenumab-aaoe helps patients with MOH who have not been detoxified (Headache. 2018;58(S2):160-162).
###
Please write to us at Neurology Reviews Migraine Resource Center ([email protected]) with your opinions.
Alan M. Rapoport, MD
Editor-in-Chief
Migraine Resource Center
Clinical Professor of Neurology
The David Geffen School of Medicine at UCLA
Los Angeles, California
Neurology Reviews recently shared two poll questions with our Facebook followers about treatment medication overuse headache (MOH). I was very interested to see the results of our poll. While the number of responses was somewhat low, we do get some sense of what respondents are saying. In this commentary, I will first tell you my perspective on the answers and then we will see what some other headache specialists say about the answers to these questions.
Poll Results:
Can MOH be treated with preventive medications without detoxification?
33 votes
YES, 39%
NO, 61%
Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor) without detoxification?
26 votes
YES, 38%
NO, 62%
My Commentary:
Let me explain in more detail my thoughts on the first question, “Can MOH be treated with preventive medications without detoxification?”
If a patient had the diagnosis of MOH – meaning 15 or more headache days per month for at least 3 months, with use of stronger medications (triptans, ergots, opiates, butalbital-containing medications) for 10 days per month or milder treatment (aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]) for 15 days per month – can they improve by being put on a traditional preventive medication without intentionally reducing their overused acute medications by a detoxification protocol ordered by a doctor or nurse?
Only 39% of our audience said yes. Yet some studies have shown that patients placed on onabotulinumtoxinA or topiramate might improve without them going through a detoxification of the overused medications. As a physician, I would suggest simultaneously decreasing in their acute medications. I think in some cases this approach creates additional improvement and makes the patient feel better. It would be better for their quality of life, as well as for their kidneys and possibly even their brains.
Here are my thoughts on the second question, “Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor), without detoxification?”
If a patient has MOH, can you expect them to improve after being placed on 1 of the 4 monoclonal antibodies to CGRP ligand or its receptor – all of which are either recently approved or currently in development – without suggesting that they decrease their overused acute care medications? Note that erenumab (Aimovig-aaoe) has been approved by the FDA and marketed as of the time of this writing; we expect 2 more products to be approved very soon.
Almost an identical percentage of our audience (38%) said yes. There is evidence in published clinical trials that those patients given these new medications did about as well with or without the presence of MOH, and both groups did better than the placebo patients. Note that most trials prohibited overuse of opiates and butalbital.
I am a firm believer of detoxifying patients from their overused over-the-counter (OTC) or prescription medications. I believe that opiates and butalbital-containing medications, when overused, are worse for patients than OTCs, NSAIDs, ergot and triptans, but all of these can cause MOH. There are many studies showing that both inpatient and outpatient detoxification alone can really help. However, it is difficult to detoxify patients and some refuse to try this approach.
So, what should we do as physicians? If a patient has MOH, I educate them, try to detoxify them slowly on an outpatient basis, and if I feel it will help, start them on a preventive medication, even before the detoxification begins so they can reach therapeutic levels. In the future, will I use one of the standard preventives, approved or off-label, for migraine prevention (beta blockers, topiramate and other anticonvulsants, antidepressants, angiotensin receptor blockers, onabotulinumtoxinA and others)? It remains to be seen. I am leaning towards the anti CGRP ligand and receptor monoclonal antibodies and preventive small molecule oral CGRP receptor blockers. While that might be enough to start with, I will continue explaining to my patients why they should actively begin a slow detoxification.
Let us see what some headache specialists said about both questions.
Robert Cowan, MD, FAAN:
There have been studies that show migraine can improve without the discontinuation of medication overuse. But that is not what the question asks. The question as posed is whether MOH can be treated with a preventive medication without detoxification. Since the diagnosis of MOH has, in the past, required the cessation of overuse leading to an improvement in the underlying headache, then technically, the answer would be “no.” But that being said, there is ample evidence that the number of headache days/months and other measures of headache can, in fact, improve with the introduction of a preventive, along with other measures such as lifestyle modification. The other ambiguity in the question has to do with what is meant by “detoxification.” Is this a hospital-based detox, or is a gradual decrease in the offending medicine in combination with the addition of a preventive, still considered “detoxification?” Also, does the response imply a sequential relationship between the detoxification and initiation of the preventive? Without further clarification, this response ratio to the question is very difficult to interpret.
There is animal data that suggests acute migraine medications may promote MOH in susceptible individuals through CGRP-dependent mechanisms and anti-CGRP antibodies may be useful for the MOH (Cephalalgia. 2017;37(6):560-570. doi: 10.1177/0333102416650702). While there are no published CGRP antibody studies that did not exclude MOH patients to my knowledge, an abstract by Silberstein et al at the recent AHS Scientific Meeting reported decreased use of overused medication with fremanazumab (Headache. 2018;58(S2):76-78).
Ira Turner, MD
There is clear data to suggest that it is not necessary to detoxify these patients before starting preventive therapy. This is true for the older and newer medications. In fact, not only do these preventive therapies still work in the presence of medication overuse, but they also help to reduce medication overuse. The one caveat that must be mentioned is that this may not apply to opiate overuse. Opiate over-users were excluded from these studies.
While it is of course our goal to reduce and stop acute medication overuse, it should not be done at the expense of delaying preventive therapy. In fact, it is desirable to do both simultaneously. This applies to oral preventive medications, botulinum toxin and CGRP monoclonal antibodies.
In view of this well-established data, it was quite surprising to me to see the results of the 2 polls cited. It seems as if we still have a lot of educating to do regarding migraine prevention in general and with medication overuse in migraine in particular.
Stewart Tepper, MD
Dr. Tepper did not have time to comment, but suggested we show you an abstract presented at the recent AHS meeting. It shows that erenumab-aaoe helps patients with MOH who have not been detoxified (Headache. 2018;58(S2):160-162).
###
Please write to us at Neurology Reviews Migraine Resource Center ([email protected]) with your opinions.
Alan M. Rapoport, MD
Editor-in-Chief
Migraine Resource Center
Clinical Professor of Neurology
The David Geffen School of Medicine at UCLA
Los Angeles, California
Prognostic factors guide mantle cell treatment decisions
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
REPORTING FROM MHM 2018
CDC Publishes Guideline for Diagnosing and Treating Pediatric mTBI
The CDC has developed a guideline for the diagnosis and management of mild traumatic brain injury (mTBI) in children. The guideline was published online ahead of print September 4 in JAMA Pediatrics. To support the “multifaceted approach” that the authors recommend for implementing the guideline, the CDC has created materials such as a screening tool, online training, fact sheets, patient discharge instructions, and symptom-based recovery tips.
The number of emergency department visits for mTBI has increased significantly during the past decade, said the authors, yet no evidence-based clinical guidelines had been drafted in the United States to guide the diagnosis, prognosis, and management of this condition. To fill this gap, the CDC established the Pediatric mTBI Guideline Workgroup, which drafted recommendations based on a systematic review of research published from January 1990 through July 2015.
Diagnosis
The first section of the guideline offers recommendations for diagnosis. Health care professionals should not routinely obtain head CT in children with suspected mTBI, say the authors. They should, however, use validated clinical decision rules to identify children with mTBI at low risk for intracranial injury in whom CT is not indicated, as well as children at higher risk for intracranial injury for whom CT may be warranted. The authors cite the Pediatric Emergency Care Applied Research Network (PECARN) decision rules as an example.
Furthermore, health care professionals should not routinely use brain MRI to evaluate suspected or diagnosed mTBI in children, according to the guideline. No study examining whether this imaging technique is appropriate met the workgroup’s inclusion criteria.
An age-appropriate, validated symptom rating scale should be one component of the diagnostic evaluation, say the authors. The Standardized Assessment of Concussion, however, “should not be exclusively used to diagnose mTBI in children aged 6 to 18,” they add. Finally, the guideline discourages the use of biomarkers (ie, serum markers) for diagnosis outside of a research setting.
Prognosis
The second section of the document provides guidance on developing a prognosis. Clinicians should advise patients and their families that most children with mTBI do not have significant difficulties that last for more than one to three months after injury, say the authors. They also should state that even though certain factors predict a child’s risk for prolonged symptoms, “each child’s recovery from mTBI is unique and will follow its own trajectory.”
Health care professionals should evaluate a child’s premorbid history as soon as possible to help determine the prognosis, say the authors. Children and families should be advised that factors such as history of mTBI, lower cognitive ability, and neurologic disorder can delay recovery from mTBI. Clinicians should screen for known risk factors for persistent symptoms and use a combination of tools (eg, validated symptom scales, cognitive testing, and balance testing) to assess recovery, according to the guideline.
Children with mTBI at high risk for persistent symptoms should be monitored closely. “For children with mTBI whose symptoms do not resolve as expected with standard care (ie, within four to six weeks), health care professionals should provide or refer for appropriate assessments and interventions,” say the authors.
Management and Treatment
The guideline’s section devoted to management and treatment begins with recommendations for returning to normal activities. Clinicians should recommend restricting physical and cognitive activity during the first several days after pediatric mTBI, according to the authors. After that point, doctors should advise patients and families “to resume a gradual schedule of activity that does not exacerbate symptoms, with close monitoring of symptom expression.” If the patient completes this step successfully, the clinician should offer an active rehabilitation program that progressively reintroduces noncontact aerobic activity that does not worsen symptoms. The number and severity of symptoms should be monitored closely throughout the patient’s recovery. A patient should resume full activity when his or her performance returns to its premorbid level, provided that he or she has no symptoms at rest or with increasing levels of exertion, according to the guideline.
“To assist children returning to school after mTBI, medical and school-based teams should counsel the student and family regarding the process of gradually increasing the duration and intensity of academic activities as tolerated, with the goal of increasing participation without significantly exacerbating symptoms,” say the authors. Return-to-school protocols should be adapted to the severity of the child’s postconcussion symptoms. School personnel should assess the need for additional educational support in students with prolonged symptoms that harm their academic performance, according to the guideline.
If a child with mTBI develops severe headache, especially if the headache is associated with other risk factors or has worsened after mTBI, emergency department professionals should observe him or her and consider obtaining a head CT to evaluate for intracranial injury, say the authors. Health care professionals should explain proper sleep hygiene to all patients with mTBI and their families to facilitate recovery.
If a child with mTBI has cognitive dysfunction, clinicians should attempt to determine its etiology within the context of other mTBI symptoms, say the authors. Treatment for cognitive dysfunction should reflect its presumed etiology, they conclude.
—Erik Greb
Suggested Reading
Lumba-Brown A, Yeates KO, Sarmiento K, et al. Centers for Disease Control and Prevention guideline on the diagnosis and management of mild traumatic brain injury among children. JAMA Pediatr. 2018 Sep 4 [Epub ahead of print].
Lumba-Brown A, Yeates KO, Sarmiento K, et al. Diagnosis and management of mild traumatic brain injury in children: a systematic review. JAMA Pediatr. 2018 Sep 4 [Epub ahead of print].
McCrea M, Manley G. State of the science on pediatric mild traumatic brain injury: progress toward clinical translation. JAMA Pediatr. 2018 Sep 4 [Epub ahead of print].
The CDC has developed a guideline for the diagnosis and management of mild traumatic brain injury (mTBI) in children. The guideline was published online ahead of print September 4 in JAMA Pediatrics. To support the “multifaceted approach” that the authors recommend for implementing the guideline, the CDC has created materials such as a screening tool, online training, fact sheets, patient discharge instructions, and symptom-based recovery tips.
The number of emergency department visits for mTBI has increased significantly during the past decade, said the authors, yet no evidence-based clinical guidelines had been drafted in the United States to guide the diagnosis, prognosis, and management of this condition. To fill this gap, the CDC established the Pediatric mTBI Guideline Workgroup, which drafted recommendations based on a systematic review of research published from January 1990 through July 2015.
Diagnosis
The first section of the guideline offers recommendations for diagnosis. Health care professionals should not routinely obtain head CT in children with suspected mTBI, say the authors. They should, however, use validated clinical decision rules to identify children with mTBI at low risk for intracranial injury in whom CT is not indicated, as well as children at higher risk for intracranial injury for whom CT may be warranted. The authors cite the Pediatric Emergency Care Applied Research Network (PECARN) decision rules as an example.
Furthermore, health care professionals should not routinely use brain MRI to evaluate suspected or diagnosed mTBI in children, according to the guideline. No study examining whether this imaging technique is appropriate met the workgroup’s inclusion criteria.
An age-appropriate, validated symptom rating scale should be one component of the diagnostic evaluation, say the authors. The Standardized Assessment of Concussion, however, “should not be exclusively used to diagnose mTBI in children aged 6 to 18,” they add. Finally, the guideline discourages the use of biomarkers (ie, serum markers) for diagnosis outside of a research setting.
Prognosis
The second section of the document provides guidance on developing a prognosis. Clinicians should advise patients and their families that most children with mTBI do not have significant difficulties that last for more than one to three months after injury, say the authors. They also should state that even though certain factors predict a child’s risk for prolonged symptoms, “each child’s recovery from mTBI is unique and will follow its own trajectory.”
Health care professionals should evaluate a child’s premorbid history as soon as possible to help determine the prognosis, say the authors. Children and families should be advised that factors such as history of mTBI, lower cognitive ability, and neurologic disorder can delay recovery from mTBI. Clinicians should screen for known risk factors for persistent symptoms and use a combination of tools (eg, validated symptom scales, cognitive testing, and balance testing) to assess recovery, according to the guideline.
Children with mTBI at high risk for persistent symptoms should be monitored closely. “For children with mTBI whose symptoms do not resolve as expected with standard care (ie, within four to six weeks), health care professionals should provide or refer for appropriate assessments and interventions,” say the authors.
Management and Treatment
The guideline’s section devoted to management and treatment begins with recommendations for returning to normal activities. Clinicians should recommend restricting physical and cognitive activity during the first several days after pediatric mTBI, according to the authors. After that point, doctors should advise patients and families “to resume a gradual schedule of activity that does not exacerbate symptoms, with close monitoring of symptom expression.” If the patient completes this step successfully, the clinician should offer an active rehabilitation program that progressively reintroduces noncontact aerobic activity that does not worsen symptoms. The number and severity of symptoms should be monitored closely throughout the patient’s recovery. A patient should resume full activity when his or her performance returns to its premorbid level, provided that he or she has no symptoms at rest or with increasing levels of exertion, according to the guideline.
“To assist children returning to school after mTBI, medical and school-based teams should counsel the student and family regarding the process of gradually increasing the duration and intensity of academic activities as tolerated, with the goal of increasing participation without significantly exacerbating symptoms,” say the authors. Return-to-school protocols should be adapted to the severity of the child’s postconcussion symptoms. School personnel should assess the need for additional educational support in students with prolonged symptoms that harm their academic performance, according to the guideline.
If a child with mTBI develops severe headache, especially if the headache is associated with other risk factors or has worsened after mTBI, emergency department professionals should observe him or her and consider obtaining a head CT to evaluate for intracranial injury, say the authors. Health care professionals should explain proper sleep hygiene to all patients with mTBI and their families to facilitate recovery.
If a child with mTBI has cognitive dysfunction, clinicians should attempt to determine its etiology within the context of other mTBI symptoms, say the authors. Treatment for cognitive dysfunction should reflect its presumed etiology, they conclude.
—Erik Greb
Suggested Reading
Lumba-Brown A, Yeates KO, Sarmiento K, et al. Centers for Disease Control and Prevention guideline on the diagnosis and management of mild traumatic brain injury among children. JAMA Pediatr. 2018 Sep 4 [Epub ahead of print].
Lumba-Brown A, Yeates KO, Sarmiento K, et al. Diagnosis and management of mild traumatic brain injury in children: a systematic review. JAMA Pediatr. 2018 Sep 4 [Epub ahead of print].
McCrea M, Manley G. State of the science on pediatric mild traumatic brain injury: progress toward clinical translation. JAMA Pediatr. 2018 Sep 4 [Epub ahead of print].
The CDC has developed a guideline for the diagnosis and management of mild traumatic brain injury (mTBI) in children. The guideline was published online ahead of print September 4 in JAMA Pediatrics. To support the “multifaceted approach” that the authors recommend for implementing the guideline, the CDC has created materials such as a screening tool, online training, fact sheets, patient discharge instructions, and symptom-based recovery tips.
The number of emergency department visits for mTBI has increased significantly during the past decade, said the authors, yet no evidence-based clinical guidelines had been drafted in the United States to guide the diagnosis, prognosis, and management of this condition. To fill this gap, the CDC established the Pediatric mTBI Guideline Workgroup, which drafted recommendations based on a systematic review of research published from January 1990 through July 2015.
Diagnosis
The first section of the guideline offers recommendations for diagnosis. Health care professionals should not routinely obtain head CT in children with suspected mTBI, say the authors. They should, however, use validated clinical decision rules to identify children with mTBI at low risk for intracranial injury in whom CT is not indicated, as well as children at higher risk for intracranial injury for whom CT may be warranted. The authors cite the Pediatric Emergency Care Applied Research Network (PECARN) decision rules as an example.
Furthermore, health care professionals should not routinely use brain MRI to evaluate suspected or diagnosed mTBI in children, according to the guideline. No study examining whether this imaging technique is appropriate met the workgroup’s inclusion criteria.
An age-appropriate, validated symptom rating scale should be one component of the diagnostic evaluation, say the authors. The Standardized Assessment of Concussion, however, “should not be exclusively used to diagnose mTBI in children aged 6 to 18,” they add. Finally, the guideline discourages the use of biomarkers (ie, serum markers) for diagnosis outside of a research setting.
Prognosis
The second section of the document provides guidance on developing a prognosis. Clinicians should advise patients and their families that most children with mTBI do not have significant difficulties that last for more than one to three months after injury, say the authors. They also should state that even though certain factors predict a child’s risk for prolonged symptoms, “each child’s recovery from mTBI is unique and will follow its own trajectory.”
Health care professionals should evaluate a child’s premorbid history as soon as possible to help determine the prognosis, say the authors. Children and families should be advised that factors such as history of mTBI, lower cognitive ability, and neurologic disorder can delay recovery from mTBI. Clinicians should screen for known risk factors for persistent symptoms and use a combination of tools (eg, validated symptom scales, cognitive testing, and balance testing) to assess recovery, according to the guideline.
Children with mTBI at high risk for persistent symptoms should be monitored closely. “For children with mTBI whose symptoms do not resolve as expected with standard care (ie, within four to six weeks), health care professionals should provide or refer for appropriate assessments and interventions,” say the authors.
Management and Treatment
The guideline’s section devoted to management and treatment begins with recommendations for returning to normal activities. Clinicians should recommend restricting physical and cognitive activity during the first several days after pediatric mTBI, according to the authors. After that point, doctors should advise patients and families “to resume a gradual schedule of activity that does not exacerbate symptoms, with close monitoring of symptom expression.” If the patient completes this step successfully, the clinician should offer an active rehabilitation program that progressively reintroduces noncontact aerobic activity that does not worsen symptoms. The number and severity of symptoms should be monitored closely throughout the patient’s recovery. A patient should resume full activity when his or her performance returns to its premorbid level, provided that he or she has no symptoms at rest or with increasing levels of exertion, according to the guideline.
“To assist children returning to school after mTBI, medical and school-based teams should counsel the student and family regarding the process of gradually increasing the duration and intensity of academic activities as tolerated, with the goal of increasing participation without significantly exacerbating symptoms,” say the authors. Return-to-school protocols should be adapted to the severity of the child’s postconcussion symptoms. School personnel should assess the need for additional educational support in students with prolonged symptoms that harm their academic performance, according to the guideline.
If a child with mTBI develops severe headache, especially if the headache is associated with other risk factors or has worsened after mTBI, emergency department professionals should observe him or her and consider obtaining a head CT to evaluate for intracranial injury, say the authors. Health care professionals should explain proper sleep hygiene to all patients with mTBI and their families to facilitate recovery.
If a child with mTBI has cognitive dysfunction, clinicians should attempt to determine its etiology within the context of other mTBI symptoms, say the authors. Treatment for cognitive dysfunction should reflect its presumed etiology, they conclude.
—Erik Greb
Suggested Reading
Lumba-Brown A, Yeates KO, Sarmiento K, et al. Centers for Disease Control and Prevention guideline on the diagnosis and management of mild traumatic brain injury among children. JAMA Pediatr. 2018 Sep 4 [Epub ahead of print].
Lumba-Brown A, Yeates KO, Sarmiento K, et al. Diagnosis and management of mild traumatic brain injury in children: a systematic review. JAMA Pediatr. 2018 Sep 4 [Epub ahead of print].
McCrea M, Manley G. State of the science on pediatric mild traumatic brain injury: progress toward clinical translation. JAMA Pediatr. 2018 Sep 4 [Epub ahead of print].
REM Sleep Behavior Disorder Predicts Rapid Motor and Cognitive Decline in Parkinson’s Disease
The disorder may have prognostic value only among patients with certain CSF results.
Among people with Parkinson’s disease, REM sleep behavior disorder (RBD) is associated with more rapid motor progression in patients with high levels of synuclein and dopaminergic pathology, according to research published online ahead of print August 8 in Neurology. RBD also indicates an increased risk of cognitive decline in patients with high degrees of synuclein and amyloid pathology.
“Our study is the first to link the predictive value of RBD symptoms to the presence of amyloid and synuclein pathology,” said Marios Politis, MD, PhD, Lily Safra Professor of Neurology and Neuroimaging, Consultant Neurologist, and the Director of the Neurodegeneration Imaging Group at King’s College London, and colleagues. “Measuring dopaminergic dysfunction and amyloid and synuclein burden in the screening of patients with RBD at an early stage of Parkinson’s disease, possibly even at the premotor phase of disease, could potentially identify the ones more likely to progress and develop dementia.”
The prevalence of RBD in patients with Parkinson’s disease ranges between 35% and 60%. Longitudinal data indicate that RBD is associated with faster development of cognitive decline and a greater risk of mild cognitive impairment and dementia in patients with Parkinson’s disease. Dr. Politis and colleagues examined the risk of motor progression and cognitive decline in patients with Parkinson’s disease and RBD who are untreated and at an early stage after disease onset.
The investigators selected 421 untreated patients with Parkinson’s disease and 196 healthy controls from the Parkinson’s Progression Markers Initiative database for their analysis. Eligible participants presented for screening at less than two years after diagnosis. Patients underwent a [123I]FP-CIT SPECT scan, CSF assessment, 3-T MRI, and thorough clinical assessments.
Among participants with Parkinson’s disease, average age was about 61 at baseline. Approximately 66% of these participants were male, and their mean disease duration was about 6.6 years. Patients with RBD had poorer olfaction, a higher burden of nonmotor symptoms, and worse scores on neuropsychologic tests. Furthermore, patients with RBD had lower CSF amyloid β42 levels and higher ratios of total tau to amyloid β42, compared with patients without RBD.
During 60 months of follow-up, RBD was associated with faster motor progression (hazard ratio [HR], 1.368) and cognitive decline (HR, 1.794). RBD predicted motor progression only in patients with Parkinson’s disease who had low α-synuclein levels and low [123I]FP-CIT uptake in the striatum (HR, 2.091). RBD predicted cognitive decline only in patients with Parkinson’s disease who had low amyloid β42 and low α-synuclein levels (HR, 2.810). RBD was not associated with cognitive decline or pathologic changes among healthy controls.
Parkinson’s disease with RBD “was previously suggested as a specific Parkinson’s disease phenotype associated with faster motor progression and characterized by reduced tremor, high frequency of falls, and a lower amplitude of response to medication dose,” said Dr. Politis and coauthors. “Our findings extend these observations and indicate that the Parkinson’s disease-RBD phenotype may vary in terms of progression of motor or cognitive symptoms, depending on underlying α-synuclein, amyloid β, and dopaminergic pathology."
—Erik Greb
Suggested Reading
Pagano G, De Micco R, Yousaf T, et al. REM behavior disorder predicts motor progression and cognitive decline in Parkinson disease. Neurology. 2018 Aug 8 [Epub ahead of print].
The disorder may have prognostic value only among patients with certain CSF results.
The disorder may have prognostic value only among patients with certain CSF results.
Among people with Parkinson’s disease, REM sleep behavior disorder (RBD) is associated with more rapid motor progression in patients with high levels of synuclein and dopaminergic pathology, according to research published online ahead of print August 8 in Neurology. RBD also indicates an increased risk of cognitive decline in patients with high degrees of synuclein and amyloid pathology.
“Our study is the first to link the predictive value of RBD symptoms to the presence of amyloid and synuclein pathology,” said Marios Politis, MD, PhD, Lily Safra Professor of Neurology and Neuroimaging, Consultant Neurologist, and the Director of the Neurodegeneration Imaging Group at King’s College London, and colleagues. “Measuring dopaminergic dysfunction and amyloid and synuclein burden in the screening of patients with RBD at an early stage of Parkinson’s disease, possibly even at the premotor phase of disease, could potentially identify the ones more likely to progress and develop dementia.”
The prevalence of RBD in patients with Parkinson’s disease ranges between 35% and 60%. Longitudinal data indicate that RBD is associated with faster development of cognitive decline and a greater risk of mild cognitive impairment and dementia in patients with Parkinson’s disease. Dr. Politis and colleagues examined the risk of motor progression and cognitive decline in patients with Parkinson’s disease and RBD who are untreated and at an early stage after disease onset.
The investigators selected 421 untreated patients with Parkinson’s disease and 196 healthy controls from the Parkinson’s Progression Markers Initiative database for their analysis. Eligible participants presented for screening at less than two years after diagnosis. Patients underwent a [123I]FP-CIT SPECT scan, CSF assessment, 3-T MRI, and thorough clinical assessments.
Among participants with Parkinson’s disease, average age was about 61 at baseline. Approximately 66% of these participants were male, and their mean disease duration was about 6.6 years. Patients with RBD had poorer olfaction, a higher burden of nonmotor symptoms, and worse scores on neuropsychologic tests. Furthermore, patients with RBD had lower CSF amyloid β42 levels and higher ratios of total tau to amyloid β42, compared with patients without RBD.
During 60 months of follow-up, RBD was associated with faster motor progression (hazard ratio [HR], 1.368) and cognitive decline (HR, 1.794). RBD predicted motor progression only in patients with Parkinson’s disease who had low α-synuclein levels and low [123I]FP-CIT uptake in the striatum (HR, 2.091). RBD predicted cognitive decline only in patients with Parkinson’s disease who had low amyloid β42 and low α-synuclein levels (HR, 2.810). RBD was not associated with cognitive decline or pathologic changes among healthy controls.
Parkinson’s disease with RBD “was previously suggested as a specific Parkinson’s disease phenotype associated with faster motor progression and characterized by reduced tremor, high frequency of falls, and a lower amplitude of response to medication dose,” said Dr. Politis and coauthors. “Our findings extend these observations and indicate that the Parkinson’s disease-RBD phenotype may vary in terms of progression of motor or cognitive symptoms, depending on underlying α-synuclein, amyloid β, and dopaminergic pathology."
—Erik Greb
Suggested Reading
Pagano G, De Micco R, Yousaf T, et al. REM behavior disorder predicts motor progression and cognitive decline in Parkinson disease. Neurology. 2018 Aug 8 [Epub ahead of print].
Among people with Parkinson’s disease, REM sleep behavior disorder (RBD) is associated with more rapid motor progression in patients with high levels of synuclein and dopaminergic pathology, according to research published online ahead of print August 8 in Neurology. RBD also indicates an increased risk of cognitive decline in patients with high degrees of synuclein and amyloid pathology.
“Our study is the first to link the predictive value of RBD symptoms to the presence of amyloid and synuclein pathology,” said Marios Politis, MD, PhD, Lily Safra Professor of Neurology and Neuroimaging, Consultant Neurologist, and the Director of the Neurodegeneration Imaging Group at King’s College London, and colleagues. “Measuring dopaminergic dysfunction and amyloid and synuclein burden in the screening of patients with RBD at an early stage of Parkinson’s disease, possibly even at the premotor phase of disease, could potentially identify the ones more likely to progress and develop dementia.”
The prevalence of RBD in patients with Parkinson’s disease ranges between 35% and 60%. Longitudinal data indicate that RBD is associated with faster development of cognitive decline and a greater risk of mild cognitive impairment and dementia in patients with Parkinson’s disease. Dr. Politis and colleagues examined the risk of motor progression and cognitive decline in patients with Parkinson’s disease and RBD who are untreated and at an early stage after disease onset.
The investigators selected 421 untreated patients with Parkinson’s disease and 196 healthy controls from the Parkinson’s Progression Markers Initiative database for their analysis. Eligible participants presented for screening at less than two years after diagnosis. Patients underwent a [123I]FP-CIT SPECT scan, CSF assessment, 3-T MRI, and thorough clinical assessments.
Among participants with Parkinson’s disease, average age was about 61 at baseline. Approximately 66% of these participants were male, and their mean disease duration was about 6.6 years. Patients with RBD had poorer olfaction, a higher burden of nonmotor symptoms, and worse scores on neuropsychologic tests. Furthermore, patients with RBD had lower CSF amyloid β42 levels and higher ratios of total tau to amyloid β42, compared with patients without RBD.
During 60 months of follow-up, RBD was associated with faster motor progression (hazard ratio [HR], 1.368) and cognitive decline (HR, 1.794). RBD predicted motor progression only in patients with Parkinson’s disease who had low α-synuclein levels and low [123I]FP-CIT uptake in the striatum (HR, 2.091). RBD predicted cognitive decline only in patients with Parkinson’s disease who had low amyloid β42 and low α-synuclein levels (HR, 2.810). RBD was not associated with cognitive decline or pathologic changes among healthy controls.
Parkinson’s disease with RBD “was previously suggested as a specific Parkinson’s disease phenotype associated with faster motor progression and characterized by reduced tremor, high frequency of falls, and a lower amplitude of response to medication dose,” said Dr. Politis and coauthors. “Our findings extend these observations and indicate that the Parkinson’s disease-RBD phenotype may vary in terms of progression of motor or cognitive symptoms, depending on underlying α-synuclein, amyloid β, and dopaminergic pathology."
—Erik Greb
Suggested Reading
Pagano G, De Micco R, Yousaf T, et al. REM behavior disorder predicts motor progression and cognitive decline in Parkinson disease. Neurology. 2018 Aug 8 [Epub ahead of print].
Multiday Seizure Cycles May Be Common
Tracking seizure cycles could facilitate personalized medicine and improve seizure reduction.
Multiday epileptic seizure cycles may occur in many individuals with epilepsy, according to a retrospective cohort study published online ahead of print September 12 in Lancet Neurology.
About 80% of patients in the study showed circadian modulation of their seizure rates, and more than 20% had strong circaseptan (ie, seven-day) rhythms, said Mark J. Cook, MD, a neurologist at St. Vincent’s Hospital in Melbourne, and colleagues.
The high prevalence of multiday seizure cycles could present an opportunity to improve treatment through the development of patient-specific chronotherapy (ie, the administration of medication when seizures are most likely). “Even without fully understanding the mechanisms of seizure cycles, temporal patterns can be incorporated into patient management plans,” said Dr. Cook.
The investigators based their study on two seizure datasets. One was a US cohort of 1,118 patients who reported at least 100 seizures through the SeizureTracker website or mobile app. The other was an Australian cohort of 12 patients with focal epilepsy who had at least 30 seizures recorded by an implanted electrocorticography device during follow-up that ranged between six months and three years.
In the US cohort, 86% of participants had at least one significant cycle in their seizure times, and 64% had more than one cycle. Most of the cycles (80%) were circadian, while 21% of people had significant circaseptan cycles in one analysis using the Hodges-Ajne test, a statistical method used to test for circular uniformity. “Many patients also showed some evidence of cycles lasting up to a month,” said the authors.
A confirmatory analysis using Monte Carlo simulation found that 7% of people, or 77 individuals, had significant circaseptan cycles. “The probability that 77 patients would randomly share a specific cycle is infinitesimal,” said the authors.
In the Australian study, 11 of 12 patients had strong rhythms at 24 hours, one had a significant cycle of exactly one week, and two others had cycles of approximately one week.
“Some people had stronger rhythms at time scales longer than 24 hours, which suggests that circadian regulation was not necessarily the strongest modulating factor of epileptic activity,” said the investigators. The cause of longer seizure cycles remains unclear, though peak seizure times might be linked to varying stress levels, seasonal changes in sleep quality, or biologic cycles such as menstruation.
—Andrew D. Bowser
Suggested Reading
Karoly PJ, Goldenholz DM, Freestone DR, et al. Circadian and circaseptan rhythms in human epilepsy: a retrospective cohort study. Lancet Neurol. 2018 Sep 12 [Epub ahead of print].
Tracking seizure cycles could facilitate personalized medicine and improve seizure reduction.
Tracking seizure cycles could facilitate personalized medicine and improve seizure reduction.
Multiday epileptic seizure cycles may occur in many individuals with epilepsy, according to a retrospective cohort study published online ahead of print September 12 in Lancet Neurology.
About 80% of patients in the study showed circadian modulation of their seizure rates, and more than 20% had strong circaseptan (ie, seven-day) rhythms, said Mark J. Cook, MD, a neurologist at St. Vincent’s Hospital in Melbourne, and colleagues.
The high prevalence of multiday seizure cycles could present an opportunity to improve treatment through the development of patient-specific chronotherapy (ie, the administration of medication when seizures are most likely). “Even without fully understanding the mechanisms of seizure cycles, temporal patterns can be incorporated into patient management plans,” said Dr. Cook.
The investigators based their study on two seizure datasets. One was a US cohort of 1,118 patients who reported at least 100 seizures through the SeizureTracker website or mobile app. The other was an Australian cohort of 12 patients with focal epilepsy who had at least 30 seizures recorded by an implanted electrocorticography device during follow-up that ranged between six months and three years.
In the US cohort, 86% of participants had at least one significant cycle in their seizure times, and 64% had more than one cycle. Most of the cycles (80%) were circadian, while 21% of people had significant circaseptan cycles in one analysis using the Hodges-Ajne test, a statistical method used to test for circular uniformity. “Many patients also showed some evidence of cycles lasting up to a month,” said the authors.
A confirmatory analysis using Monte Carlo simulation found that 7% of people, or 77 individuals, had significant circaseptan cycles. “The probability that 77 patients would randomly share a specific cycle is infinitesimal,” said the authors.
In the Australian study, 11 of 12 patients had strong rhythms at 24 hours, one had a significant cycle of exactly one week, and two others had cycles of approximately one week.
“Some people had stronger rhythms at time scales longer than 24 hours, which suggests that circadian regulation was not necessarily the strongest modulating factor of epileptic activity,” said the investigators. The cause of longer seizure cycles remains unclear, though peak seizure times might be linked to varying stress levels, seasonal changes in sleep quality, or biologic cycles such as menstruation.
—Andrew D. Bowser
Suggested Reading
Karoly PJ, Goldenholz DM, Freestone DR, et al. Circadian and circaseptan rhythms in human epilepsy: a retrospective cohort study. Lancet Neurol. 2018 Sep 12 [Epub ahead of print].
Multiday epileptic seizure cycles may occur in many individuals with epilepsy, according to a retrospective cohort study published online ahead of print September 12 in Lancet Neurology.
About 80% of patients in the study showed circadian modulation of their seizure rates, and more than 20% had strong circaseptan (ie, seven-day) rhythms, said Mark J. Cook, MD, a neurologist at St. Vincent’s Hospital in Melbourne, and colleagues.
The high prevalence of multiday seizure cycles could present an opportunity to improve treatment through the development of patient-specific chronotherapy (ie, the administration of medication when seizures are most likely). “Even without fully understanding the mechanisms of seizure cycles, temporal patterns can be incorporated into patient management plans,” said Dr. Cook.
The investigators based their study on two seizure datasets. One was a US cohort of 1,118 patients who reported at least 100 seizures through the SeizureTracker website or mobile app. The other was an Australian cohort of 12 patients with focal epilepsy who had at least 30 seizures recorded by an implanted electrocorticography device during follow-up that ranged between six months and three years.
In the US cohort, 86% of participants had at least one significant cycle in their seizure times, and 64% had more than one cycle. Most of the cycles (80%) were circadian, while 21% of people had significant circaseptan cycles in one analysis using the Hodges-Ajne test, a statistical method used to test for circular uniformity. “Many patients also showed some evidence of cycles lasting up to a month,” said the authors.
A confirmatory analysis using Monte Carlo simulation found that 7% of people, or 77 individuals, had significant circaseptan cycles. “The probability that 77 patients would randomly share a specific cycle is infinitesimal,” said the authors.
In the Australian study, 11 of 12 patients had strong rhythms at 24 hours, one had a significant cycle of exactly one week, and two others had cycles of approximately one week.
“Some people had stronger rhythms at time scales longer than 24 hours, which suggests that circadian regulation was not necessarily the strongest modulating factor of epileptic activity,” said the investigators. The cause of longer seizure cycles remains unclear, though peak seizure times might be linked to varying stress levels, seasonal changes in sleep quality, or biologic cycles such as menstruation.
—Andrew D. Bowser
Suggested Reading
Karoly PJ, Goldenholz DM, Freestone DR, et al. Circadian and circaseptan rhythms in human epilepsy: a retrospective cohort study. Lancet Neurol. 2018 Sep 12 [Epub ahead of print].