User login
Tom Collins is a freelance writer in South Florida who has written about medical topics from nasty infections to ethical dilemmas, runaway tumors to tornado-chasing doctors. He travels the globe gathering conference health news and lives in West Palm Beach.
LISTEN NOW: Hospitalist Chris Spoja discusses his decision to pursue a MMM degree
Listen to Chris Spoja, MD, a hospitalist with Sound Physicians, explain his decision to pursue a Master’s of Medical Management (MMM) degree.
Listen to Chris Spoja, MD, a hospitalist with Sound Physicians, explain his decision to pursue a Master’s of Medical Management (MMM) degree.
Listen to Chris Spoja, MD, a hospitalist with Sound Physicians, explain his decision to pursue a Master’s of Medical Management (MMM) degree.
New Job Isn’t Focus of Everyone Seeking Advanced Management Degrees
Many hospitalists might get an advanced degree in management because they covet a specific job, but that might not be the only reason.
Kevan Pickrel, MD, MHM, a regional chief medical officer for Sound Physicians in Southern California, says his decision to get a master’s in healthcare management from the University of Texas at Dallas came down to credibility.
“I got the additional degree for one reason: a seat at the table,” Dr. Pickrel says. “Physicians complain a lot about all the change and the autonomy they have lost but do little about it beyond grumbling at lunch. I believe in hospital medicine as a discipline and believe in the value of the specialty. I wanted to be sure my specialty had a voice, and the only way to set myself apart from ‘just another whining doc’ was to add the letters.”
Making it happen was not a simple task, he says.
“Finding the time wasn’t easy,” he says. “I burned vacation time and leaned on my colleagues a lot. There are any number of physician- or executive-targeted programs offered that make it possible. Possible, but not easy.”
Chris Spoja, DO, a Sound hospitalist in Idaho, says he’d like to prepare himself for a chief medical officer job. He is planning to get his Master of Medical Management (MMM) from the University of Southern California (USC) next year, after he participates in a local leadership program in Idaho, which will allow him to network with people in his area.
“I would like to position myself to at least have that option,” he says, noting that the USC program will allow him to do most of his coursework online, participating in group discussions over Skype or doing work on his own. But he’ll have to visit the campus in Los Angeles for three days once a month.
“It’s not a small commitment,” he says. “But it’s doable.” TH
Tom Collins is a freelance writer in South Florida.
Many hospitalists might get an advanced degree in management because they covet a specific job, but that might not be the only reason.
Kevan Pickrel, MD, MHM, a regional chief medical officer for Sound Physicians in Southern California, says his decision to get a master’s in healthcare management from the University of Texas at Dallas came down to credibility.
“I got the additional degree for one reason: a seat at the table,” Dr. Pickrel says. “Physicians complain a lot about all the change and the autonomy they have lost but do little about it beyond grumbling at lunch. I believe in hospital medicine as a discipline and believe in the value of the specialty. I wanted to be sure my specialty had a voice, and the only way to set myself apart from ‘just another whining doc’ was to add the letters.”
Making it happen was not a simple task, he says.
“Finding the time wasn’t easy,” he says. “I burned vacation time and leaned on my colleagues a lot. There are any number of physician- or executive-targeted programs offered that make it possible. Possible, but not easy.”
Chris Spoja, DO, a Sound hospitalist in Idaho, says he’d like to prepare himself for a chief medical officer job. He is planning to get his Master of Medical Management (MMM) from the University of Southern California (USC) next year, after he participates in a local leadership program in Idaho, which will allow him to network with people in his area.
“I would like to position myself to at least have that option,” he says, noting that the USC program will allow him to do most of his coursework online, participating in group discussions over Skype or doing work on his own. But he’ll have to visit the campus in Los Angeles for three days once a month.
“It’s not a small commitment,” he says. “But it’s doable.” TH
Tom Collins is a freelance writer in South Florida.
Many hospitalists might get an advanced degree in management because they covet a specific job, but that might not be the only reason.
Kevan Pickrel, MD, MHM, a regional chief medical officer for Sound Physicians in Southern California, says his decision to get a master’s in healthcare management from the University of Texas at Dallas came down to credibility.
“I got the additional degree for one reason: a seat at the table,” Dr. Pickrel says. “Physicians complain a lot about all the change and the autonomy they have lost but do little about it beyond grumbling at lunch. I believe in hospital medicine as a discipline and believe in the value of the specialty. I wanted to be sure my specialty had a voice, and the only way to set myself apart from ‘just another whining doc’ was to add the letters.”
Making it happen was not a simple task, he says.
“Finding the time wasn’t easy,” he says. “I burned vacation time and leaned on my colleagues a lot. There are any number of physician- or executive-targeted programs offered that make it possible. Possible, but not easy.”
Chris Spoja, DO, a Sound hospitalist in Idaho, says he’d like to prepare himself for a chief medical officer job. He is planning to get his Master of Medical Management (MMM) from the University of Southern California (USC) next year, after he participates in a local leadership program in Idaho, which will allow him to network with people in his area.
“I would like to position myself to at least have that option,” he says, noting that the USC program will allow him to do most of his coursework online, participating in group discussions over Skype or doing work on his own. But he’ll have to visit the campus in Los Angeles for three days once a month.
“It’s not a small commitment,” he says. “But it’s doable.” TH
Tom Collins is a freelance writer in South Florida.
Advanced Management Degrees: What Hospitalists Should Consider Before Pursuing One
“That was kind of on-the-job training,” he says. “Just because you’re wearing a higher rank than somebody else doesn’t necessarily mean that you’re going to be able to effectively motivate them to work within the team and do their job more effectively and help you do your job more effectively.
“That probably was my first time that I was desiring formalized leadership training.”
Dr. Spoja, now 40 and a chief hospitalist in Nampa, Idaho, and regional medical director for Sound Physicians, has made the decision to pursue a Master of Medical Management (MMM) degree—a choice that will mean even crazier hours than he already has now, more hard work, and regular trips from Idaho to Los Angeles. Not exactly a snap to pull off for someone who’s married and has four kids.
But it makes sense for him, because he would like the option of pursuing a chief medical officer position eventually, he says.
“You’re going to get to interact with professors,” he says. “It shows a level of commitment, I think, to leadership.”
A Great Debate
The question of getting an advanced management degree—such as an MMM, a Master of Business Administration (MBA), a Master of Public Health (MPH), or a Master of Hospital Administration (MHA)—poses a great dilemma for many hospitalists.
Job experience and exposure to so many facets of hospital operations make hospitalists good candidates for administrative posts.
But that experience, some hospitalists find, is really only enough to place them into a gray area. Hospitalists’ experience and managerial abilities lay the groundwork for moving up the hospital ladder to the C-suite and might pique their interest in doing so; however, the question remains whether that experience alone is enough. And how to go about deciding whether to get an advanced management degree—and then where and how to pursue it—sets up a complex choice with lots of variables.
Key recommendations from educators, career counselors, and physicians who have gone through the decision process include the following:
- Seek advice from those in the positions you seek;
- Use resources like the American College of Physician Executives (ACPE); and
- Hone your leadership skills through in-house programs before embarking on an expensive and time-consuming formal degree.
Advanced degrees can cost as much as $40,000 per year, just for tuition, and can take a year or two to complete. Options range from an on-campus program to online programs to a combination of the two. The choice of which degree to pursue might be difficult for some, ranging from the traditional MBA to the more quality improvement-focused MMM.
Michael Guthrie, MD, MBA, executive-in-residence at the University of Colorado-Denver School of Business, says making the choice requires thorough consideration.
“Here’s something that could cost you $75,000, maybe more, depending on what you pick,” says Dr. Guthrie, a frequent speaker on the topic at SHM annual meetings. Plus, “time, energy, distraction, and time away from family. There are significant issues about cost, not just financial. And you have to really have a sense of what’s the return on investment.”
Those with degrees generally do make more money than those without, according to the 2011 Cejka Executive Search and ACPE Physician Executive Compensation Survey. Physician CEOs with an MBA made $24,000 more in 2011 than those without an advanced degree; CMOs with the degree made $44,000 more.
But having a management degree doesn’t automatically translate to more money in every executive position. Physician CEOs with an MMM made $37,000 less than those without a degree; CMOs with an MMM made $51,000 more than those without a degree—a difference based partially on the reality that an MMM often is a degree pursued by aspiring CMOs.

—Rebekah Apple, MA, senior manager of physician services and support, career counselor, American College of Physician Executives
Mission C
One of the most fundamental questions facing hospitalists with advancement aspirations is “Can I get to the C-suite without that extra degree?”
In some cases, the answer is “no.”
At Banner Health, a system with facilities throughout the western U.S., all C-suite executives have to have an advanced degree of some kind, generally an MBA or MHA, says Kathy Bollinger, president of the Arizona West Region at Banner. She recently hired former hospitalist Steve Narang, MD, MHCM, FAAP, MBA, as CEO of Banner Good Samaritan Medical Center in Phoenix.
It wasn’t merely Dr. Narang’s MBA that earned him the position. Bollinger says his knowledge, experience, and her own confidence in him during a transitional period in the U.S. healthcare landscape played key roles in the decision.
But the degree rule is in place, she notes, because at Banner, the degree is seen as so crucial to cultivating the kind of knowledge and person capable of being a good hospital administrator.
“His business degree is clearly part of him and part of his effectiveness,” Bollinger says. “So I’m not sure that I could have observed in Steve the things that I observed in Steve had not he not been more globally trained, if you will.”
Doctors and administrators, she says, tend not to think alike.
“I would say physicians, medical staff members of a hospital, and administrators of a hospital historically, in a stereotyped way, have been predisposed to be at odds with one another,” she says. The formal education is a way to expand a physician’s way of thinking, she adds.
“The business thinking and financial aptitude that is required at our big hospitals is such that it would be a stretch for somebody who didn’t either have a degree or was deep into it from an experience standpoint,” she says. “For me, that was very significant.”
When the Cleveland Clinic was looking for a new CEO at South Pointe Hospital in 2012, they tapped a doctor without a management degree—Brian Harte, MD, SFHM, a hospitalist who had been chief operating officer at another hospital within the system. At the time of Dr. Harte’s promotion, Cleveland Clinic Regional Hospitals President David Bronson, MD, who also does not have an advanced management degree, praised Dr. Harte’s experience.
“His expertise in quality will help South Pointe Hospital continue to provide the best experience for patients,” Dr. Bronson said in a news release at the time.
What can’t be denied, however, is that many physicians in executive roles do, in fact, have post-graduate degrees. According to the ACPE’s survey, 40% of the doctors surveyed had an MBA, an MMM, an MPH, or an MHA. Of those, 52% had an MBA. The survey includes everyone from CEOs to associate professors.
Even so, an advanced degree is not a magic wand.
“The MBA doesn’t get you a job,” Dr. Guthrie says. “People are looking at what you can do and what you’ve done and not at how smart and schooled you are. It’s helpful. It’s useful. I believe that the current terminology is ‘preferred ‘ or ‘encouraged,’ but it isn’t essential.”
Due Diligence
Robert Zipper, MD, MMM, SFHM, chief medical officer of Sound Physicians’ West Region and chair of SHM’s Leadership Committee, earned his business degree at Carnegie Mellon in Pittsburgh. He says it’s important that hospitalists have experience before pursuing the degree. This will help them “see the business side through a clinician’s eyes first.”
“There were some people in my cohort at Carnegie Mellon who didn’t have enough experience to make the programmatic elements all that relevant to their practice, to their world,” he says. “You want to be able to reflect on the mistakes that you’ve made and the things that you’ve done really well and have a deeper understanding of what worked and what didn’t if you want to get the most out of it.”
That said, he acknowledges that those circumstances apparently aren’t a requirement for success—one of his Carnegie Mellon classmates is a CEO.
Which kind of degree to pursue is a whole other question. Experts say that while getting the degree will give you a leg up to some extent, certain degrees will be preferable over others depending on what you want to do. For someone who wants to run a start-up medical company, an MBA might be best. For someone who wants to work in quality improvement, the MMM might be best.
An online degree—or at least one that’s completed partially online—might be more practical for a doctor who wants to continue with practice. Some programs require students to be on campus for every class, and some require occasional on-campus work, while others never require a doctor to set foot on a campus.
“The issue becomes, what are the individual’s degrees of freedom?” Dr. Guthrie says. “Individuals’ personal circumstances really drive which kind of program they look at. And then where they’re located may have a lot to do with what they choose.”
Rebekah Apple, MA, senior manager of physician services and support at the ACPE and the primary career counselor there, says that when doctors ask her about getting an advanced management degree, she starts by asking them what they want to be doing in three to five years. If the answer is not realistic, she helps them revise those goals. Once that’s settled, she helps them figure out whether the degree makes sense.
From that point, she says, there is no hard-and-fast rule.
“It’s very driven by the individual,” she says.
Plunging into management training probably isn’t best suited for those fresh out of residency with little leadership exposure at their institution or for those only a few years from retirement.
She tries to open physicians’ eyes to the wide range of C-suite positions available, including some they might not have heard of. Chief medical officer is traditionally what doctors think of when they consider executive positions, but other positions, such as chief information technology officer or chief patient experience officer, should be considered.
“The conversations are changing very much,” Apple says. “There are a lot of other emerging roles. I think sometimes that the varied opportunities that exist, whether or not people know about them at the beginning of our conversation, can really color the decisions that people make later.”
A love of learning should be a main motivator. Dr. Guthrie emphasizes the importance of pursuing a degree that you’re interested in. Without that interest, he says, a hospitalist might want to reconsider.
“It goes by very quickly—it’s also fun,” he says. “Physicians are great students usually, and by the time they get into it, [they] realize, ‘You know, this is really kind of a hoot.’”
Tom Collins is a freelance writer living in South Florida.
“That was kind of on-the-job training,” he says. “Just because you’re wearing a higher rank than somebody else doesn’t necessarily mean that you’re going to be able to effectively motivate them to work within the team and do their job more effectively and help you do your job more effectively.
“That probably was my first time that I was desiring formalized leadership training.”
Dr. Spoja, now 40 and a chief hospitalist in Nampa, Idaho, and regional medical director for Sound Physicians, has made the decision to pursue a Master of Medical Management (MMM) degree—a choice that will mean even crazier hours than he already has now, more hard work, and regular trips from Idaho to Los Angeles. Not exactly a snap to pull off for someone who’s married and has four kids.
But it makes sense for him, because he would like the option of pursuing a chief medical officer position eventually, he says.
“You’re going to get to interact with professors,” he says. “It shows a level of commitment, I think, to leadership.”
A Great Debate
The question of getting an advanced management degree—such as an MMM, a Master of Business Administration (MBA), a Master of Public Health (MPH), or a Master of Hospital Administration (MHA)—poses a great dilemma for many hospitalists.
Job experience and exposure to so many facets of hospital operations make hospitalists good candidates for administrative posts.
But that experience, some hospitalists find, is really only enough to place them into a gray area. Hospitalists’ experience and managerial abilities lay the groundwork for moving up the hospital ladder to the C-suite and might pique their interest in doing so; however, the question remains whether that experience alone is enough. And how to go about deciding whether to get an advanced management degree—and then where and how to pursue it—sets up a complex choice with lots of variables.
Key recommendations from educators, career counselors, and physicians who have gone through the decision process include the following:
- Seek advice from those in the positions you seek;
- Use resources like the American College of Physician Executives (ACPE); and
- Hone your leadership skills through in-house programs before embarking on an expensive and time-consuming formal degree.
Advanced degrees can cost as much as $40,000 per year, just for tuition, and can take a year or two to complete. Options range from an on-campus program to online programs to a combination of the two. The choice of which degree to pursue might be difficult for some, ranging from the traditional MBA to the more quality improvement-focused MMM.
Michael Guthrie, MD, MBA, executive-in-residence at the University of Colorado-Denver School of Business, says making the choice requires thorough consideration.
“Here’s something that could cost you $75,000, maybe more, depending on what you pick,” says Dr. Guthrie, a frequent speaker on the topic at SHM annual meetings. Plus, “time, energy, distraction, and time away from family. There are significant issues about cost, not just financial. And you have to really have a sense of what’s the return on investment.”
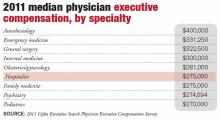
Those with degrees generally do make more money than those without, according to the 2011 Cejka Executive Search and ACPE Physician Executive Compensation Survey. Physician CEOs with an MBA made $24,000 more in 2011 than those without an advanced degree; CMOs with the degree made $44,000 more.
But having a management degree doesn’t automatically translate to more money in every executive position. Physician CEOs with an MMM made $37,000 less than those without a degree; CMOs with an MMM made $51,000 more than those without a degree—a difference based partially on the reality that an MMM often is a degree pursued by aspiring CMOs.

—Rebekah Apple, MA, senior manager of physician services and support, career counselor, American College of Physician Executives
Mission C
One of the most fundamental questions facing hospitalists with advancement aspirations is “Can I get to the C-suite without that extra degree?”
In some cases, the answer is “no.”
At Banner Health, a system with facilities throughout the western U.S., all C-suite executives have to have an advanced degree of some kind, generally an MBA or MHA, says Kathy Bollinger, president of the Arizona West Region at Banner. She recently hired former hospitalist Steve Narang, MD, MHCM, FAAP, MBA, as CEO of Banner Good Samaritan Medical Center in Phoenix.
It wasn’t merely Dr. Narang’s MBA that earned him the position. Bollinger says his knowledge, experience, and her own confidence in him during a transitional period in the U.S. healthcare landscape played key roles in the decision.
But the degree rule is in place, she notes, because at Banner, the degree is seen as so crucial to cultivating the kind of knowledge and person capable of being a good hospital administrator.
“His business degree is clearly part of him and part of his effectiveness,” Bollinger says. “So I’m not sure that I could have observed in Steve the things that I observed in Steve had not he not been more globally trained, if you will.”
Doctors and administrators, she says, tend not to think alike.
“I would say physicians, medical staff members of a hospital, and administrators of a hospital historically, in a stereotyped way, have been predisposed to be at odds with one another,” she says. The formal education is a way to expand a physician’s way of thinking, she adds.
“The business thinking and financial aptitude that is required at our big hospitals is such that it would be a stretch for somebody who didn’t either have a degree or was deep into it from an experience standpoint,” she says. “For me, that was very significant.”
When the Cleveland Clinic was looking for a new CEO at South Pointe Hospital in 2012, they tapped a doctor without a management degree—Brian Harte, MD, SFHM, a hospitalist who had been chief operating officer at another hospital within the system. At the time of Dr. Harte’s promotion, Cleveland Clinic Regional Hospitals President David Bronson, MD, who also does not have an advanced management degree, praised Dr. Harte’s experience.
“His expertise in quality will help South Pointe Hospital continue to provide the best experience for patients,” Dr. Bronson said in a news release at the time.
What can’t be denied, however, is that many physicians in executive roles do, in fact, have post-graduate degrees. According to the ACPE’s survey, 40% of the doctors surveyed had an MBA, an MMM, an MPH, or an MHA. Of those, 52% had an MBA. The survey includes everyone from CEOs to associate professors.
Even so, an advanced degree is not a magic wand.
“The MBA doesn’t get you a job,” Dr. Guthrie says. “People are looking at what you can do and what you’ve done and not at how smart and schooled you are. It’s helpful. It’s useful. I believe that the current terminology is ‘preferred ‘ or ‘encouraged,’ but it isn’t essential.”
Due Diligence
Robert Zipper, MD, MMM, SFHM, chief medical officer of Sound Physicians’ West Region and chair of SHM’s Leadership Committee, earned his business degree at Carnegie Mellon in Pittsburgh. He says it’s important that hospitalists have experience before pursuing the degree. This will help them “see the business side through a clinician’s eyes first.”
“There were some people in my cohort at Carnegie Mellon who didn’t have enough experience to make the programmatic elements all that relevant to their practice, to their world,” he says. “You want to be able to reflect on the mistakes that you’ve made and the things that you’ve done really well and have a deeper understanding of what worked and what didn’t if you want to get the most out of it.”
That said, he acknowledges that those circumstances apparently aren’t a requirement for success—one of his Carnegie Mellon classmates is a CEO.
Which kind of degree to pursue is a whole other question. Experts say that while getting the degree will give you a leg up to some extent, certain degrees will be preferable over others depending on what you want to do. For someone who wants to run a start-up medical company, an MBA might be best. For someone who wants to work in quality improvement, the MMM might be best.
An online degree—or at least one that’s completed partially online—might be more practical for a doctor who wants to continue with practice. Some programs require students to be on campus for every class, and some require occasional on-campus work, while others never require a doctor to set foot on a campus.
“The issue becomes, what are the individual’s degrees of freedom?” Dr. Guthrie says. “Individuals’ personal circumstances really drive which kind of program they look at. And then where they’re located may have a lot to do with what they choose.”
Rebekah Apple, MA, senior manager of physician services and support at the ACPE and the primary career counselor there, says that when doctors ask her about getting an advanced management degree, she starts by asking them what they want to be doing in three to five years. If the answer is not realistic, she helps them revise those goals. Once that’s settled, she helps them figure out whether the degree makes sense.
From that point, she says, there is no hard-and-fast rule.
“It’s very driven by the individual,” she says.
Plunging into management training probably isn’t best suited for those fresh out of residency with little leadership exposure at their institution or for those only a few years from retirement.
She tries to open physicians’ eyes to the wide range of C-suite positions available, including some they might not have heard of. Chief medical officer is traditionally what doctors think of when they consider executive positions, but other positions, such as chief information technology officer or chief patient experience officer, should be considered.
“The conversations are changing very much,” Apple says. “There are a lot of other emerging roles. I think sometimes that the varied opportunities that exist, whether or not people know about them at the beginning of our conversation, can really color the decisions that people make later.”
A love of learning should be a main motivator. Dr. Guthrie emphasizes the importance of pursuing a degree that you’re interested in. Without that interest, he says, a hospitalist might want to reconsider.
“It goes by very quickly—it’s also fun,” he says. “Physicians are great students usually, and by the time they get into it, [they] realize, ‘You know, this is really kind of a hoot.’”
Tom Collins is a freelance writer living in South Florida.
“That was kind of on-the-job training,” he says. “Just because you’re wearing a higher rank than somebody else doesn’t necessarily mean that you’re going to be able to effectively motivate them to work within the team and do their job more effectively and help you do your job more effectively.
“That probably was my first time that I was desiring formalized leadership training.”
Dr. Spoja, now 40 and a chief hospitalist in Nampa, Idaho, and regional medical director for Sound Physicians, has made the decision to pursue a Master of Medical Management (MMM) degree—a choice that will mean even crazier hours than he already has now, more hard work, and regular trips from Idaho to Los Angeles. Not exactly a snap to pull off for someone who’s married and has four kids.
But it makes sense for him, because he would like the option of pursuing a chief medical officer position eventually, he says.
“You’re going to get to interact with professors,” he says. “It shows a level of commitment, I think, to leadership.”
A Great Debate
The question of getting an advanced management degree—such as an MMM, a Master of Business Administration (MBA), a Master of Public Health (MPH), or a Master of Hospital Administration (MHA)—poses a great dilemma for many hospitalists.
Job experience and exposure to so many facets of hospital operations make hospitalists good candidates for administrative posts.
But that experience, some hospitalists find, is really only enough to place them into a gray area. Hospitalists’ experience and managerial abilities lay the groundwork for moving up the hospital ladder to the C-suite and might pique their interest in doing so; however, the question remains whether that experience alone is enough. And how to go about deciding whether to get an advanced management degree—and then where and how to pursue it—sets up a complex choice with lots of variables.
Key recommendations from educators, career counselors, and physicians who have gone through the decision process include the following:
- Seek advice from those in the positions you seek;
- Use resources like the American College of Physician Executives (ACPE); and
- Hone your leadership skills through in-house programs before embarking on an expensive and time-consuming formal degree.
Advanced degrees can cost as much as $40,000 per year, just for tuition, and can take a year or two to complete. Options range from an on-campus program to online programs to a combination of the two. The choice of which degree to pursue might be difficult for some, ranging from the traditional MBA to the more quality improvement-focused MMM.
Michael Guthrie, MD, MBA, executive-in-residence at the University of Colorado-Denver School of Business, says making the choice requires thorough consideration.
“Here’s something that could cost you $75,000, maybe more, depending on what you pick,” says Dr. Guthrie, a frequent speaker on the topic at SHM annual meetings. Plus, “time, energy, distraction, and time away from family. There are significant issues about cost, not just financial. And you have to really have a sense of what’s the return on investment.”
Those with degrees generally do make more money than those without, according to the 2011 Cejka Executive Search and ACPE Physician Executive Compensation Survey. Physician CEOs with an MBA made $24,000 more in 2011 than those without an advanced degree; CMOs with the degree made $44,000 more.
But having a management degree doesn’t automatically translate to more money in every executive position. Physician CEOs with an MMM made $37,000 less than those without a degree; CMOs with an MMM made $51,000 more than those without a degree—a difference based partially on the reality that an MMM often is a degree pursued by aspiring CMOs.

—Rebekah Apple, MA, senior manager of physician services and support, career counselor, American College of Physician Executives
Mission C
One of the most fundamental questions facing hospitalists with advancement aspirations is “Can I get to the C-suite without that extra degree?”
In some cases, the answer is “no.”
At Banner Health, a system with facilities throughout the western U.S., all C-suite executives have to have an advanced degree of some kind, generally an MBA or MHA, says Kathy Bollinger, president of the Arizona West Region at Banner. She recently hired former hospitalist Steve Narang, MD, MHCM, FAAP, MBA, as CEO of Banner Good Samaritan Medical Center in Phoenix.
It wasn’t merely Dr. Narang’s MBA that earned him the position. Bollinger says his knowledge, experience, and her own confidence in him during a transitional period in the U.S. healthcare landscape played key roles in the decision.
But the degree rule is in place, she notes, because at Banner, the degree is seen as so crucial to cultivating the kind of knowledge and person capable of being a good hospital administrator.
“His business degree is clearly part of him and part of his effectiveness,” Bollinger says. “So I’m not sure that I could have observed in Steve the things that I observed in Steve had not he not been more globally trained, if you will.”
Doctors and administrators, she says, tend not to think alike.
“I would say physicians, medical staff members of a hospital, and administrators of a hospital historically, in a stereotyped way, have been predisposed to be at odds with one another,” she says. The formal education is a way to expand a physician’s way of thinking, she adds.
“The business thinking and financial aptitude that is required at our big hospitals is such that it would be a stretch for somebody who didn’t either have a degree or was deep into it from an experience standpoint,” she says. “For me, that was very significant.”
When the Cleveland Clinic was looking for a new CEO at South Pointe Hospital in 2012, they tapped a doctor without a management degree—Brian Harte, MD, SFHM, a hospitalist who had been chief operating officer at another hospital within the system. At the time of Dr. Harte’s promotion, Cleveland Clinic Regional Hospitals President David Bronson, MD, who also does not have an advanced management degree, praised Dr. Harte’s experience.
“His expertise in quality will help South Pointe Hospital continue to provide the best experience for patients,” Dr. Bronson said in a news release at the time.
What can’t be denied, however, is that many physicians in executive roles do, in fact, have post-graduate degrees. According to the ACPE’s survey, 40% of the doctors surveyed had an MBA, an MMM, an MPH, or an MHA. Of those, 52% had an MBA. The survey includes everyone from CEOs to associate professors.
Even so, an advanced degree is not a magic wand.
“The MBA doesn’t get you a job,” Dr. Guthrie says. “People are looking at what you can do and what you’ve done and not at how smart and schooled you are. It’s helpful. It’s useful. I believe that the current terminology is ‘preferred ‘ or ‘encouraged,’ but it isn’t essential.”
Due Diligence
Robert Zipper, MD, MMM, SFHM, chief medical officer of Sound Physicians’ West Region and chair of SHM’s Leadership Committee, earned his business degree at Carnegie Mellon in Pittsburgh. He says it’s important that hospitalists have experience before pursuing the degree. This will help them “see the business side through a clinician’s eyes first.”
“There were some people in my cohort at Carnegie Mellon who didn’t have enough experience to make the programmatic elements all that relevant to their practice, to their world,” he says. “You want to be able to reflect on the mistakes that you’ve made and the things that you’ve done really well and have a deeper understanding of what worked and what didn’t if you want to get the most out of it.”
That said, he acknowledges that those circumstances apparently aren’t a requirement for success—one of his Carnegie Mellon classmates is a CEO.
Which kind of degree to pursue is a whole other question. Experts say that while getting the degree will give you a leg up to some extent, certain degrees will be preferable over others depending on what you want to do. For someone who wants to run a start-up medical company, an MBA might be best. For someone who wants to work in quality improvement, the MMM might be best.
An online degree—or at least one that’s completed partially online—might be more practical for a doctor who wants to continue with practice. Some programs require students to be on campus for every class, and some require occasional on-campus work, while others never require a doctor to set foot on a campus.
“The issue becomes, what are the individual’s degrees of freedom?” Dr. Guthrie says. “Individuals’ personal circumstances really drive which kind of program they look at. And then where they’re located may have a lot to do with what they choose.”
Rebekah Apple, MA, senior manager of physician services and support at the ACPE and the primary career counselor there, says that when doctors ask her about getting an advanced management degree, she starts by asking them what they want to be doing in three to five years. If the answer is not realistic, she helps them revise those goals. Once that’s settled, she helps them figure out whether the degree makes sense.
From that point, she says, there is no hard-and-fast rule.
“It’s very driven by the individual,” she says.
Plunging into management training probably isn’t best suited for those fresh out of residency with little leadership exposure at their institution or for those only a few years from retirement.
She tries to open physicians’ eyes to the wide range of C-suite positions available, including some they might not have heard of. Chief medical officer is traditionally what doctors think of when they consider executive positions, but other positions, such as chief information technology officer or chief patient experience officer, should be considered.
“The conversations are changing very much,” Apple says. “There are a lot of other emerging roles. I think sometimes that the varied opportunities that exist, whether or not people know about them at the beginning of our conversation, can really color the decisions that people make later.”
A love of learning should be a main motivator. Dr. Guthrie emphasizes the importance of pursuing a degree that you’re interested in. Without that interest, he says, a hospitalist might want to reconsider.
“It goes by very quickly—it’s also fun,” he says. “Physicians are great students usually, and by the time they get into it, [they] realize, ‘You know, this is really kind of a hoot.’”
Tom Collins is a freelance writer living in South Florida.
LISTEN NOW: M.D. Anderson hospitalists discuss caring for cancer patients
Josiah Halm, MD, and Sahitya Gadiraju, DO, assistant professors of general internal medicine at M.D. Anderson Cancer Center in Houston, discuss the breadth of care provided to cancer patients, a risk assessment being developed there on readmission risk, and factors in care that go beyond the medical.
Josiah Halm, MD, and Sahitya Gadiraju, DO, assistant professors of general internal medicine at M.D. Anderson Cancer Center in Houston, discuss the breadth of care provided to cancer patients, a risk assessment being developed there on readmission risk, and factors in care that go beyond the medical.
Josiah Halm, MD, and Sahitya Gadiraju, DO, assistant professors of general internal medicine at M.D. Anderson Cancer Center in Houston, discuss the breadth of care provided to cancer patients, a risk assessment being developed there on readmission risk, and factors in care that go beyond the medical.
10 Things Oncologists Think Hospitalists Need to Know
Things you need to know
An occasional series providing specialty-specific advice for hospitalists from experts in the field.
COMING UP: 10 Things Endocrinologists Want HM to Know Archived: @the-hospitalist.org
- 10 Things Infectious Disease
- 12 Things Cardiology
- 12 Things Nephrology
- 12 Things Billing & Coding
Cancer patients can be some of the most complicated and high-stakes patients who come into a hospitalist’s care.
The issues faced by such patients are three-pronged: Besides the effects of the cancer itself, these often elderly patients also grapple with the side effects of treatment and other medical issues.
The Hospitalist sought tips for caring for hospitalized cancer patients from a half-dozen experts in hematology and oncology. Here are the 10 most common pieces of advice they had for hospitalists caring for cancer patients.
1 Know the History
This includes the subtleties of the patient history, which can be quite involved, says Fadlo R. Khuri, MD, FACP, deputy director of the Winship Cancer Institute of Emory University and chair of hematology and medical oncology at the Emory University School of Medicine in Atlanta.
“Part of that history may be obtained from the patient and the patient’s family, but if the treatment has been evolving over time, you need to get in touch with the treating physician or at least have access to the records of the patient’s treatment,” he says. “The arsenal of drugs that we use against cancer has expanded dramatically and in different directions. Now we have tremendous technological innovations with very focused radiation or very refined surgery, and not just novel chemotherapy but also targeted therapies that can target a specific Achilles heel of cancer.”
Basically, it is important for hospitalists to know exactly “what you are dealing with.”
“That’s a lot of information that the hospitalist needs to know. Whom do I contact? Whom do I need to access, not just on the web, but in person, to understand what this patient is going through?” he adds.
With many patients, time is of the essence. This is part of the reason why it’s so important to get a complete history and full picture of a patient’s treatment right away, Dr. Khuri says.
“The patient with cancer often presents in worse shape than patients with other diseases,” he says. “Therefore, with patients with cancer or patients with other really life-threatening illness, you generally have less time to figure out what is going on.”
2 Communication Is Paramount
“The reason that communication is important is to convey the right message to the patient,” says Suresh Ramalingam, MD, professor and director of medical oncology and the lung cancer program at the Emory School of Medicine. “An oncologist who’s been following a patient for a year and a half…I would think has some insight that he or she can provide the hospitalist to manage the acute illness that the patient is admitted with.
“The other thing is many times a patient comes in the hospital and the first question they have is, ‘Does this mean my cancer is getting worse? What is the next option for me? And am I going to die right away?’ And they’re going to ask this question of whomever they see first. Having the oncologist’s thoughts on the patient’s overall status of cancer is important to address such issues.”
Dr. Ramalingam says that a situation that used to occur, but is now less frequent, is frantic calls from a patient in a hospital bed saying, “The hospitalist just walked in, and he said I’m going to die in three weeks. You never told me about that.”
When that happens, “we have to go back and talk to the patient and reassure the patient that that’s not the case,” Dr. Ramalingam says.
3 Treating Cancer Is More Than Treating Cancer
At the MD Anderson Cancer Center in Houston, where a pilot hospitalist program that began six years ago has grown into a permanent part of the center, treatment comes from all angles, not just medical, says Josiah Halm, MD, MS, FACP, FHM, CMQ, and Sahitya Gadiraju, DO, assistant professors of general internal medicine at the center.
“I think the biggest thing is to understand that a cancer patient is very complex and there’s much more than the physical component,” says Dr. Gadiraju, one of nine hospitalists at MD Anderson. “There’s an emotional component. There’s a mental component. There’s the family that’s involved.
“One of the biggest things that we do is not just support the patient physically and medically but also emotionally and mentally. And we provide very good family support working as part of an interdisciplinary team.”
4 Know the Baseline
Dr. Khuri says hospitalists should start by seeking answers to some simple questions.
“What kind of situation were they in when they began to deteriorate? Was this patient walking, talking, healthy, eating, working? And is this an acute deterioration, or is this a gradual deterioration?” he says.
The hospitalist caring for a patient with an acute decline might play a major role in the outcome.
“Some of these acute, precipitating events may be treatable, and the hospitalist may be—forgive my language—Johnny-on-the-spot—and may be able to make a major difference in turning that patient around,” he says.
5 Fight for DVT prophylaxis
When patients should be given prophylaxis for DVT, do not be deterred from doing so by the treating oncologist, says Efrén Manjarrez, MD, SFHM, assistant professor of medicine and interim chief of the division of hospital medicine and patient safety officer for the Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine. For patients undergoing chemotherapy, oncologists might be concerned about the potential for bleeding events, but it’s important to “get with the guidelines,” Dr. Manjarrez says.
“Oftentimes, hospitalists can be undermined by the oncologists that they’re managing their patients with,” he says. “Make sure that you stick to your guns and make sure that you’re strong about giving DVT prophylaxis to these patients, unless they truly meet exclusion criteria for that prophylaxis.
“Sometimes, hematologists or oncologists might actually cancel your order.”
6 ‘More Is Better’ for Genome Analysis
With a fine-needle biopsy, there might not be enough specimen left for molecular analysis, Dr. Ramalingam explains.
“The purpose of the biopsy is no longer just diagnostic; it has significant therapeutic implications. Therefore, getting as much tissue [as possible] during that initial diagnostic biopsy is very helpful, because we conduct detailed molecular studies on these specimens,” he says. “If you don’t get enough specimen in the first biopsy, but you just have enough to make a diagnosis of the type of cancer, then you have to resort to a second biopsy. So, more is better when it comes to tissue.”
7 Consider Pediatric Test Tubes for Pancytopenic Patients
Using smaller test tubes will lower the potential for anemia caused by frequent blood draws, Dr. Manjarrez says. Recent evidence suggests that hospital-acquired anemia prolongs hospital costs, length of stay, and mortality risk—all directly proportional to the level of anemia.1
“We’re causing [patients] to be more anemic with blood draws,” he says. “When you have cancer patients who get chemotherapy, their bone marrow is wiped out by the chemotherapy. So what happens is that you end up in the cycle where you have to keep transfusing these patients. The more blood draws that you get from them, the more we’re exacerbating it.”
8 Respect Your Turf, Their Turf
Dr. Manjarrez says the best way to ensure the hem-onc specialists respect the hospitalist’s turf, and vice versa, is to discuss the treatment parameters ahead of time.
“Try and negotiate comanagement deals with your hematologist-oncologist colleagues before you enter into comanagement relationships with them,” he says.
One particularly sticky situation is when a patient is admitted with the expectation that the hospitalist will be caring for acute issues like infection or cancer-related pain, but then the hospitalization is extended because the oncologist wants to start chemotherapy.
“That can be a problem,” he says. “Agree with your hematology-oncology colleagues what you’re going to do in advance, as much as you can.”

“Oftentimes, hospitalists can be undermined by the oncologists that they’re managing their patients with. Make sure that you stick to your guns and make sure that you’re strong about giving DVT prophylaxis to these patients, unless they truly meet exclusion criteria for that prophylaxis.”
—Efrén Manjarrez, MD, SFHM, assistant professor of medicine, interim chief, division of hospital medicine, patient safety officer, Sylvester Comprehensive Cancer Center, University of Miami Miller School of Medicine.
9 Be Cautious in Using Granulocyte Colony-Stimulating Factor (GCSF)
The medication is used to stimulate the body to produce more white blood cells, which sometimes is needed after chemotherapy. They are good for certain situations but should be handled with care, says Lowell Schnipper, MD, clinical director of the Beth Israel Deaconess Medical Center Cancer Center in Boston.
“Because it’s unnecessary and very expensive,” says Dr. Schnipper, who is chair of the American Society of Clinical Oncology’s Value of Care Task Force. “If this is a chemotherapy regimen that has a risk of fever and neutropenia in the context of the chemotherapy, [and] the odds of having that complication are 20% percent or higher with a chemotherapy regimen, we suggest using GCSF.”
If not, then GCSF should be avoided, he says.
Such decisions likely will fall to the treating oncologist, but Dr. Schnipper says it is a topic with which hospitalists should be familiar.
10 Rethink Imaging
“If you get a PET scan in the hospital and a patient is admitted for a different diagnosis, there’s a good likelihood that it’s not going to be reimbursed,” Dr. Ramalingam says.
Plus, he says, a scan done in the hospital could cloud the radiographic findings used to make decisions.
“For instance, for someone with pneumonia, the infiltrate might be difficult to differentiate from cancer,” he says.
Tom Collins is a freelance author in South Florida and longtime contributor to The Hospitalist.
Reference
Things you need to know
An occasional series providing specialty-specific advice for hospitalists from experts in the field.
COMING UP: 10 Things Endocrinologists Want HM to Know Archived: @the-hospitalist.org
- 10 Things Infectious Disease
- 12 Things Cardiology
- 12 Things Nephrology
- 12 Things Billing & Coding
Cancer patients can be some of the most complicated and high-stakes patients who come into a hospitalist’s care.
The issues faced by such patients are three-pronged: Besides the effects of the cancer itself, these often elderly patients also grapple with the side effects of treatment and other medical issues.
The Hospitalist sought tips for caring for hospitalized cancer patients from a half-dozen experts in hematology and oncology. Here are the 10 most common pieces of advice they had for hospitalists caring for cancer patients.
1 Know the History
This includes the subtleties of the patient history, which can be quite involved, says Fadlo R. Khuri, MD, FACP, deputy director of the Winship Cancer Institute of Emory University and chair of hematology and medical oncology at the Emory University School of Medicine in Atlanta.
“Part of that history may be obtained from the patient and the patient’s family, but if the treatment has been evolving over time, you need to get in touch with the treating physician or at least have access to the records of the patient’s treatment,” he says. “The arsenal of drugs that we use against cancer has expanded dramatically and in different directions. Now we have tremendous technological innovations with very focused radiation or very refined surgery, and not just novel chemotherapy but also targeted therapies that can target a specific Achilles heel of cancer.”
Basically, it is important for hospitalists to know exactly “what you are dealing with.”
“That’s a lot of information that the hospitalist needs to know. Whom do I contact? Whom do I need to access, not just on the web, but in person, to understand what this patient is going through?” he adds.
With many patients, time is of the essence. This is part of the reason why it’s so important to get a complete history and full picture of a patient’s treatment right away, Dr. Khuri says.
“The patient with cancer often presents in worse shape than patients with other diseases,” he says. “Therefore, with patients with cancer or patients with other really life-threatening illness, you generally have less time to figure out what is going on.”
2 Communication Is Paramount
“The reason that communication is important is to convey the right message to the patient,” says Suresh Ramalingam, MD, professor and director of medical oncology and the lung cancer program at the Emory School of Medicine. “An oncologist who’s been following a patient for a year and a half…I would think has some insight that he or she can provide the hospitalist to manage the acute illness that the patient is admitted with.
“The other thing is many times a patient comes in the hospital and the first question they have is, ‘Does this mean my cancer is getting worse? What is the next option for me? And am I going to die right away?’ And they’re going to ask this question of whomever they see first. Having the oncologist’s thoughts on the patient’s overall status of cancer is important to address such issues.”
Dr. Ramalingam says that a situation that used to occur, but is now less frequent, is frantic calls from a patient in a hospital bed saying, “The hospitalist just walked in, and he said I’m going to die in three weeks. You never told me about that.”
When that happens, “we have to go back and talk to the patient and reassure the patient that that’s not the case,” Dr. Ramalingam says.
3 Treating Cancer Is More Than Treating Cancer
At the MD Anderson Cancer Center in Houston, where a pilot hospitalist program that began six years ago has grown into a permanent part of the center, treatment comes from all angles, not just medical, says Josiah Halm, MD, MS, FACP, FHM, CMQ, and Sahitya Gadiraju, DO, assistant professors of general internal medicine at the center.
“I think the biggest thing is to understand that a cancer patient is very complex and there’s much more than the physical component,” says Dr. Gadiraju, one of nine hospitalists at MD Anderson. “There’s an emotional component. There’s a mental component. There’s the family that’s involved.
“One of the biggest things that we do is not just support the patient physically and medically but also emotionally and mentally. And we provide very good family support working as part of an interdisciplinary team.”
4 Know the Baseline
Dr. Khuri says hospitalists should start by seeking answers to some simple questions.
“What kind of situation were they in when they began to deteriorate? Was this patient walking, talking, healthy, eating, working? And is this an acute deterioration, or is this a gradual deterioration?” he says.
The hospitalist caring for a patient with an acute decline might play a major role in the outcome.
“Some of these acute, precipitating events may be treatable, and the hospitalist may be—forgive my language—Johnny-on-the-spot—and may be able to make a major difference in turning that patient around,” he says.
5 Fight for DVT prophylaxis
When patients should be given prophylaxis for DVT, do not be deterred from doing so by the treating oncologist, says Efrén Manjarrez, MD, SFHM, assistant professor of medicine and interim chief of the division of hospital medicine and patient safety officer for the Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine. For patients undergoing chemotherapy, oncologists might be concerned about the potential for bleeding events, but it’s important to “get with the guidelines,” Dr. Manjarrez says.
“Oftentimes, hospitalists can be undermined by the oncologists that they’re managing their patients with,” he says. “Make sure that you stick to your guns and make sure that you’re strong about giving DVT prophylaxis to these patients, unless they truly meet exclusion criteria for that prophylaxis.
“Sometimes, hematologists or oncologists might actually cancel your order.”
6 ‘More Is Better’ for Genome Analysis
With a fine-needle biopsy, there might not be enough specimen left for molecular analysis, Dr. Ramalingam explains.
“The purpose of the biopsy is no longer just diagnostic; it has significant therapeutic implications. Therefore, getting as much tissue [as possible] during that initial diagnostic biopsy is very helpful, because we conduct detailed molecular studies on these specimens,” he says. “If you don’t get enough specimen in the first biopsy, but you just have enough to make a diagnosis of the type of cancer, then you have to resort to a second biopsy. So, more is better when it comes to tissue.”
7 Consider Pediatric Test Tubes for Pancytopenic Patients
Using smaller test tubes will lower the potential for anemia caused by frequent blood draws, Dr. Manjarrez says. Recent evidence suggests that hospital-acquired anemia prolongs hospital costs, length of stay, and mortality risk—all directly proportional to the level of anemia.1
“We’re causing [patients] to be more anemic with blood draws,” he says. “When you have cancer patients who get chemotherapy, their bone marrow is wiped out by the chemotherapy. So what happens is that you end up in the cycle where you have to keep transfusing these patients. The more blood draws that you get from them, the more we’re exacerbating it.”
8 Respect Your Turf, Their Turf
Dr. Manjarrez says the best way to ensure the hem-onc specialists respect the hospitalist’s turf, and vice versa, is to discuss the treatment parameters ahead of time.
“Try and negotiate comanagement deals with your hematologist-oncologist colleagues before you enter into comanagement relationships with them,” he says.
One particularly sticky situation is when a patient is admitted with the expectation that the hospitalist will be caring for acute issues like infection or cancer-related pain, but then the hospitalization is extended because the oncologist wants to start chemotherapy.
“That can be a problem,” he says. “Agree with your hematology-oncology colleagues what you’re going to do in advance, as much as you can.”

“Oftentimes, hospitalists can be undermined by the oncologists that they’re managing their patients with. Make sure that you stick to your guns and make sure that you’re strong about giving DVT prophylaxis to these patients, unless they truly meet exclusion criteria for that prophylaxis.”
—Efrén Manjarrez, MD, SFHM, assistant professor of medicine, interim chief, division of hospital medicine, patient safety officer, Sylvester Comprehensive Cancer Center, University of Miami Miller School of Medicine.
9 Be Cautious in Using Granulocyte Colony-Stimulating Factor (GCSF)
The medication is used to stimulate the body to produce more white blood cells, which sometimes is needed after chemotherapy. They are good for certain situations but should be handled with care, says Lowell Schnipper, MD, clinical director of the Beth Israel Deaconess Medical Center Cancer Center in Boston.
“Because it’s unnecessary and very expensive,” says Dr. Schnipper, who is chair of the American Society of Clinical Oncology’s Value of Care Task Force. “If this is a chemotherapy regimen that has a risk of fever and neutropenia in the context of the chemotherapy, [and] the odds of having that complication are 20% percent or higher with a chemotherapy regimen, we suggest using GCSF.”
If not, then GCSF should be avoided, he says.
Such decisions likely will fall to the treating oncologist, but Dr. Schnipper says it is a topic with which hospitalists should be familiar.
10 Rethink Imaging
“If you get a PET scan in the hospital and a patient is admitted for a different diagnosis, there’s a good likelihood that it’s not going to be reimbursed,” Dr. Ramalingam says.
Plus, he says, a scan done in the hospital could cloud the radiographic findings used to make decisions.
“For instance, for someone with pneumonia, the infiltrate might be difficult to differentiate from cancer,” he says.
Tom Collins is a freelance author in South Florida and longtime contributor to The Hospitalist.
Reference
Things you need to know
An occasional series providing specialty-specific advice for hospitalists from experts in the field.
COMING UP: 10 Things Endocrinologists Want HM to Know Archived: @the-hospitalist.org
- 10 Things Infectious Disease
- 12 Things Cardiology
- 12 Things Nephrology
- 12 Things Billing & Coding
Cancer patients can be some of the most complicated and high-stakes patients who come into a hospitalist’s care.
The issues faced by such patients are three-pronged: Besides the effects of the cancer itself, these often elderly patients also grapple with the side effects of treatment and other medical issues.
The Hospitalist sought tips for caring for hospitalized cancer patients from a half-dozen experts in hematology and oncology. Here are the 10 most common pieces of advice they had for hospitalists caring for cancer patients.
1 Know the History
This includes the subtleties of the patient history, which can be quite involved, says Fadlo R. Khuri, MD, FACP, deputy director of the Winship Cancer Institute of Emory University and chair of hematology and medical oncology at the Emory University School of Medicine in Atlanta.
“Part of that history may be obtained from the patient and the patient’s family, but if the treatment has been evolving over time, you need to get in touch with the treating physician or at least have access to the records of the patient’s treatment,” he says. “The arsenal of drugs that we use against cancer has expanded dramatically and in different directions. Now we have tremendous technological innovations with very focused radiation or very refined surgery, and not just novel chemotherapy but also targeted therapies that can target a specific Achilles heel of cancer.”
Basically, it is important for hospitalists to know exactly “what you are dealing with.”
“That’s a lot of information that the hospitalist needs to know. Whom do I contact? Whom do I need to access, not just on the web, but in person, to understand what this patient is going through?” he adds.
With many patients, time is of the essence. This is part of the reason why it’s so important to get a complete history and full picture of a patient’s treatment right away, Dr. Khuri says.
“The patient with cancer often presents in worse shape than patients with other diseases,” he says. “Therefore, with patients with cancer or patients with other really life-threatening illness, you generally have less time to figure out what is going on.”
2 Communication Is Paramount
“The reason that communication is important is to convey the right message to the patient,” says Suresh Ramalingam, MD, professor and director of medical oncology and the lung cancer program at the Emory School of Medicine. “An oncologist who’s been following a patient for a year and a half…I would think has some insight that he or she can provide the hospitalist to manage the acute illness that the patient is admitted with.
“The other thing is many times a patient comes in the hospital and the first question they have is, ‘Does this mean my cancer is getting worse? What is the next option for me? And am I going to die right away?’ And they’re going to ask this question of whomever they see first. Having the oncologist’s thoughts on the patient’s overall status of cancer is important to address such issues.”
Dr. Ramalingam says that a situation that used to occur, but is now less frequent, is frantic calls from a patient in a hospital bed saying, “The hospitalist just walked in, and he said I’m going to die in three weeks. You never told me about that.”
When that happens, “we have to go back and talk to the patient and reassure the patient that that’s not the case,” Dr. Ramalingam says.
3 Treating Cancer Is More Than Treating Cancer
At the MD Anderson Cancer Center in Houston, where a pilot hospitalist program that began six years ago has grown into a permanent part of the center, treatment comes from all angles, not just medical, says Josiah Halm, MD, MS, FACP, FHM, CMQ, and Sahitya Gadiraju, DO, assistant professors of general internal medicine at the center.
“I think the biggest thing is to understand that a cancer patient is very complex and there’s much more than the physical component,” says Dr. Gadiraju, one of nine hospitalists at MD Anderson. “There’s an emotional component. There’s a mental component. There’s the family that’s involved.
“One of the biggest things that we do is not just support the patient physically and medically but also emotionally and mentally. And we provide very good family support working as part of an interdisciplinary team.”
4 Know the Baseline
Dr. Khuri says hospitalists should start by seeking answers to some simple questions.
“What kind of situation were they in when they began to deteriorate? Was this patient walking, talking, healthy, eating, working? And is this an acute deterioration, or is this a gradual deterioration?” he says.
The hospitalist caring for a patient with an acute decline might play a major role in the outcome.
“Some of these acute, precipitating events may be treatable, and the hospitalist may be—forgive my language—Johnny-on-the-spot—and may be able to make a major difference in turning that patient around,” he says.
5 Fight for DVT prophylaxis
When patients should be given prophylaxis for DVT, do not be deterred from doing so by the treating oncologist, says Efrén Manjarrez, MD, SFHM, assistant professor of medicine and interim chief of the division of hospital medicine and patient safety officer for the Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine. For patients undergoing chemotherapy, oncologists might be concerned about the potential for bleeding events, but it’s important to “get with the guidelines,” Dr. Manjarrez says.
“Oftentimes, hospitalists can be undermined by the oncologists that they’re managing their patients with,” he says. “Make sure that you stick to your guns and make sure that you’re strong about giving DVT prophylaxis to these patients, unless they truly meet exclusion criteria for that prophylaxis.
“Sometimes, hematologists or oncologists might actually cancel your order.”
6 ‘More Is Better’ for Genome Analysis
With a fine-needle biopsy, there might not be enough specimen left for molecular analysis, Dr. Ramalingam explains.
“The purpose of the biopsy is no longer just diagnostic; it has significant therapeutic implications. Therefore, getting as much tissue [as possible] during that initial diagnostic biopsy is very helpful, because we conduct detailed molecular studies on these specimens,” he says. “If you don’t get enough specimen in the first biopsy, but you just have enough to make a diagnosis of the type of cancer, then you have to resort to a second biopsy. So, more is better when it comes to tissue.”
7 Consider Pediatric Test Tubes for Pancytopenic Patients
Using smaller test tubes will lower the potential for anemia caused by frequent blood draws, Dr. Manjarrez says. Recent evidence suggests that hospital-acquired anemia prolongs hospital costs, length of stay, and mortality risk—all directly proportional to the level of anemia.1
“We’re causing [patients] to be more anemic with blood draws,” he says. “When you have cancer patients who get chemotherapy, their bone marrow is wiped out by the chemotherapy. So what happens is that you end up in the cycle where you have to keep transfusing these patients. The more blood draws that you get from them, the more we’re exacerbating it.”
8 Respect Your Turf, Their Turf
Dr. Manjarrez says the best way to ensure the hem-onc specialists respect the hospitalist’s turf, and vice versa, is to discuss the treatment parameters ahead of time.
“Try and negotiate comanagement deals with your hematologist-oncologist colleagues before you enter into comanagement relationships with them,” he says.
One particularly sticky situation is when a patient is admitted with the expectation that the hospitalist will be caring for acute issues like infection or cancer-related pain, but then the hospitalization is extended because the oncologist wants to start chemotherapy.
“That can be a problem,” he says. “Agree with your hematology-oncology colleagues what you’re going to do in advance, as much as you can.”

“Oftentimes, hospitalists can be undermined by the oncologists that they’re managing their patients with. Make sure that you stick to your guns and make sure that you’re strong about giving DVT prophylaxis to these patients, unless they truly meet exclusion criteria for that prophylaxis.”
—Efrén Manjarrez, MD, SFHM, assistant professor of medicine, interim chief, division of hospital medicine, patient safety officer, Sylvester Comprehensive Cancer Center, University of Miami Miller School of Medicine.
9 Be Cautious in Using Granulocyte Colony-Stimulating Factor (GCSF)
The medication is used to stimulate the body to produce more white blood cells, which sometimes is needed after chemotherapy. They are good for certain situations but should be handled with care, says Lowell Schnipper, MD, clinical director of the Beth Israel Deaconess Medical Center Cancer Center in Boston.
“Because it’s unnecessary and very expensive,” says Dr. Schnipper, who is chair of the American Society of Clinical Oncology’s Value of Care Task Force. “If this is a chemotherapy regimen that has a risk of fever and neutropenia in the context of the chemotherapy, [and] the odds of having that complication are 20% percent or higher with a chemotherapy regimen, we suggest using GCSF.”
If not, then GCSF should be avoided, he says.
Such decisions likely will fall to the treating oncologist, but Dr. Schnipper says it is a topic with which hospitalists should be familiar.
10 Rethink Imaging
“If you get a PET scan in the hospital and a patient is admitted for a different diagnosis, there’s a good likelihood that it’s not going to be reimbursed,” Dr. Ramalingam says.
Plus, he says, a scan done in the hospital could cloud the radiographic findings used to make decisions.
“For instance, for someone with pneumonia, the infiltrate might be difficult to differentiate from cancer,” he says.
Tom Collins is a freelance author in South Florida and longtime contributor to The Hospitalist.
Reference
Palliative Care Patient Transitions Challenging For Hospitalists, Oncologists
When should treating a cancer patient become more about controlling symptoms and making the patient comfortable than about trying to slow the cancer itself?
Hospitalists, who often care for patients in the worst stages of health, regularly make important observations that result in a patient transitioning to hospice care. When such a case is suspected, careful discussions with the treating oncologist, the patient, and the patient’s family should be held.
Determining how and when to have those discussions can be tricky, experts say.
“You have to understand the family dynamic before anything else,” Dr. Sahitya Gadiraju, DO, says. “You have to understand the patient, how mentally and emotionally ready they are to have that conversation. And how ready [the family] is to have that conversation.”

“The best treatment, regardless of anything else, is really symptom control, palliative care, taking care of the anxiety, the pain, the sleep, the constipation, the nausea. When you do those things well, everything falls in place.”—Dr. Halm
One treatment course to question, according to the American Society of Clinical Oncology’s Choosing Wisely list, is the use of cancer treatments at the end of life. The society recommends that patients with advanced, solid tumors be shifted to palliative care when previous treatments haven’t worked and no additional, evidence-based treatments are available; when patients can’t care for themselves and spend most of their time in a chair or a bed; and when they aren’t eligible for a clinical trial.
Dr. Lowell Schnipper, MD, who led the group that created the list, says this guidance can be helpful to hospitalists. He says hospitalists should be aware of the patient’s “trajectory” and should only call in consultants when “something clearly suggests that this situation is reversible.”
Dr. Suresh Ramalingam, MD says conferring with the oncologist before talking to a patient about hospice care is crucial, because new treatments are available that can bring about remarkable turnarounds, even in patients in dire condition.
“For certain subsets of patients with cancer, there are specific, molecularly targeted therapies that produce so-called ‘Lazarus responses,’ he explains. “They are bed-bound, totally crippled one day, and a few days after you give them the drug, they’re like a new person walking into your clinic.”
Dr. Josiah Halm, MD, says that, working at a comprehensive cancer center like M.D. Anderson Cancer Center in Houston, he sometimes sees patients who won’t accept the initial determination that aggressive treatment is not a good option when they have poor performance status. They sometimes still demand “small chemo,” or “a little chemo,” from their oncologist.
“Sometimes these patients would have gone elsewhere. They’ve been told, ‘Look, what you need is hospice; there’s nothing else we can do.’ And they’ll come here,” he says. “Either we’re telling them the same thing and that’s when they accept it or [they are] still demanding treatment. Sometimes they may be eligible for cancer treatment after being reviewed by our oncologists.
“The best treatment, regardless of anything else, is really symptom control, palliative care, taking care of the anxiety, the pain, the sleep, the constipation, the nausea,” he adds. “When you do those things well, everything falls in place.”
Dr. Halm sometimes asks patients what he can do to make them feel better “today,” with emphasis on the moment. In this way, he gets patients to focus on one main symptom that is causing them the most discomfort.
When patients don’t want to accept palliative-only care, Dr. Gadiraju says, it’s helpful to get them to realize they are still getting treatment, even if the nature of the treatment is different.
“We don’t want the patient to ever feel like we’re giving up on them,” he says.
When should treating a cancer patient become more about controlling symptoms and making the patient comfortable than about trying to slow the cancer itself?
Hospitalists, who often care for patients in the worst stages of health, regularly make important observations that result in a patient transitioning to hospice care. When such a case is suspected, careful discussions with the treating oncologist, the patient, and the patient’s family should be held.
Determining how and when to have those discussions can be tricky, experts say.
“You have to understand the family dynamic before anything else,” Dr. Sahitya Gadiraju, DO, says. “You have to understand the patient, how mentally and emotionally ready they are to have that conversation. And how ready [the family] is to have that conversation.”

“The best treatment, regardless of anything else, is really symptom control, palliative care, taking care of the anxiety, the pain, the sleep, the constipation, the nausea. When you do those things well, everything falls in place.”—Dr. Halm
One treatment course to question, according to the American Society of Clinical Oncology’s Choosing Wisely list, is the use of cancer treatments at the end of life. The society recommends that patients with advanced, solid tumors be shifted to palliative care when previous treatments haven’t worked and no additional, evidence-based treatments are available; when patients can’t care for themselves and spend most of their time in a chair or a bed; and when they aren’t eligible for a clinical trial.
Dr. Lowell Schnipper, MD, who led the group that created the list, says this guidance can be helpful to hospitalists. He says hospitalists should be aware of the patient’s “trajectory” and should only call in consultants when “something clearly suggests that this situation is reversible.”
Dr. Suresh Ramalingam, MD says conferring with the oncologist before talking to a patient about hospice care is crucial, because new treatments are available that can bring about remarkable turnarounds, even in patients in dire condition.
“For certain subsets of patients with cancer, there are specific, molecularly targeted therapies that produce so-called ‘Lazarus responses,’ he explains. “They are bed-bound, totally crippled one day, and a few days after you give them the drug, they’re like a new person walking into your clinic.”
Dr. Josiah Halm, MD, says that, working at a comprehensive cancer center like M.D. Anderson Cancer Center in Houston, he sometimes sees patients who won’t accept the initial determination that aggressive treatment is not a good option when they have poor performance status. They sometimes still demand “small chemo,” or “a little chemo,” from their oncologist.
“Sometimes these patients would have gone elsewhere. They’ve been told, ‘Look, what you need is hospice; there’s nothing else we can do.’ And they’ll come here,” he says. “Either we’re telling them the same thing and that’s when they accept it or [they are] still demanding treatment. Sometimes they may be eligible for cancer treatment after being reviewed by our oncologists.
“The best treatment, regardless of anything else, is really symptom control, palliative care, taking care of the anxiety, the pain, the sleep, the constipation, the nausea,” he adds. “When you do those things well, everything falls in place.”
Dr. Halm sometimes asks patients what he can do to make them feel better “today,” with emphasis on the moment. In this way, he gets patients to focus on one main symptom that is causing them the most discomfort.
When patients don’t want to accept palliative-only care, Dr. Gadiraju says, it’s helpful to get them to realize they are still getting treatment, even if the nature of the treatment is different.
“We don’t want the patient to ever feel like we’re giving up on them,” he says.
When should treating a cancer patient become more about controlling symptoms and making the patient comfortable than about trying to slow the cancer itself?
Hospitalists, who often care for patients in the worst stages of health, regularly make important observations that result in a patient transitioning to hospice care. When such a case is suspected, careful discussions with the treating oncologist, the patient, and the patient’s family should be held.
Determining how and when to have those discussions can be tricky, experts say.
“You have to understand the family dynamic before anything else,” Dr. Sahitya Gadiraju, DO, says. “You have to understand the patient, how mentally and emotionally ready they are to have that conversation. And how ready [the family] is to have that conversation.”

“The best treatment, regardless of anything else, is really symptom control, palliative care, taking care of the anxiety, the pain, the sleep, the constipation, the nausea. When you do those things well, everything falls in place.”—Dr. Halm
One treatment course to question, according to the American Society of Clinical Oncology’s Choosing Wisely list, is the use of cancer treatments at the end of life. The society recommends that patients with advanced, solid tumors be shifted to palliative care when previous treatments haven’t worked and no additional, evidence-based treatments are available; when patients can’t care for themselves and spend most of their time in a chair or a bed; and when they aren’t eligible for a clinical trial.
Dr. Lowell Schnipper, MD, who led the group that created the list, says this guidance can be helpful to hospitalists. He says hospitalists should be aware of the patient’s “trajectory” and should only call in consultants when “something clearly suggests that this situation is reversible.”
Dr. Suresh Ramalingam, MD says conferring with the oncologist before talking to a patient about hospice care is crucial, because new treatments are available that can bring about remarkable turnarounds, even in patients in dire condition.
“For certain subsets of patients with cancer, there are specific, molecularly targeted therapies that produce so-called ‘Lazarus responses,’ he explains. “They are bed-bound, totally crippled one day, and a few days after you give them the drug, they’re like a new person walking into your clinic.”
Dr. Josiah Halm, MD, says that, working at a comprehensive cancer center like M.D. Anderson Cancer Center in Houston, he sometimes sees patients who won’t accept the initial determination that aggressive treatment is not a good option when they have poor performance status. They sometimes still demand “small chemo,” or “a little chemo,” from their oncologist.
“Sometimes these patients would have gone elsewhere. They’ve been told, ‘Look, what you need is hospice; there’s nothing else we can do.’ And they’ll come here,” he says. “Either we’re telling them the same thing and that’s when they accept it or [they are] still demanding treatment. Sometimes they may be eligible for cancer treatment after being reviewed by our oncologists.
“The best treatment, regardless of anything else, is really symptom control, palliative care, taking care of the anxiety, the pain, the sleep, the constipation, the nausea,” he adds. “When you do those things well, everything falls in place.”
Dr. Halm sometimes asks patients what he can do to make them feel better “today,” with emphasis on the moment. In this way, he gets patients to focus on one main symptom that is causing them the most discomfort.
When patients don’t want to accept palliative-only care, Dr. Gadiraju says, it’s helpful to get them to realize they are still getting treatment, even if the nature of the treatment is different.
“We don’t want the patient to ever feel like we’re giving up on them,” he says.
Listen Now! Patrick Torcson, MD, MMM, SFHM, discusses how being a hospitalist prepared him for the C-suite
Click here to listen to more of our interview with Dr. Torcson
Click here to listen to more of our interview with Dr. Torcson
Click here to listen to more of our interview with Dr. Torcson
Four Hospitalists Retrace Path to C-Suite Executive Ranks

Dr. Steve Narang
CEO, Banner Health’s Good Samaritan Medical Center, Phoenix
Path to the C-suite: Medical school at Northwestern University; residency at Johns Hopkins; pediatric hospitalist at Children’s Hospital of New Orleans; medical director of Pediatric Hospitalists of Louisiana; master’s in healthcare management from Harvard; chief medical officer at Banner Health’s Cardon Children’s Medical Center
As a resident at Johns Hopkins in pediatrics, Dr. Narang wasn’t always pleased by what he saw—too many process errors and patient safety gaps, and too much waste. Healthcare resources were not being spent in the right way, he discovered.
“I was struck by [the fact] that we spent a lot of our resources in publishing more articles about what’s new, and what the coolest drug is,” he says. “I saw very little of that [relating to] what does this mean in terms of value?”
He became a hospitalist because he saw it as a role in which he could “really touch everything” if he chose to do so and work within the system to improve it.
“The hospital could use a partner,” he says. “One of the biggest challenges we have in healthcare is hospitals and physicians are often not working together to add value, and they’re subtracting from value, and they’re competing with each other.”
If doctors make the effort to learn the management aspects of working in a hospital, they can put themselves in a great position to take on big leadership roles, Dr. Narang says. He says hospitals are seeing the value in having physicians in those roles.
“If you can find the right leader and it happens to be a physician, if it happens to be a physician who can speak that language—and find a sweet spot for independent physicians, employed physicians, and hospitalists to deliver value, which we have to now I think it’s the best way to go,” he says. “I think you’re going to see a trend moving forward to this as more physicians become more interested in this track.” —TC
Being a hospitalist was a key strength of my background. Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
—Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix

Dr. Brian Harte
President, South Pointe Hospital, Warrenville Heights, Ohio
Path to the C-suite: Resident at University of California San Francisco; private practice hospitalist in Marin County, near San Francisco; hospitalist at Cleveland Clinic; program director of hospital medicine at Cleveland Clinic’s Euclid Hospital; chief operating officer at Cleveland Clinic’s Hillcrest Hospital For about two hours a day, Dr. Harte makes his way through South Pointe Hospital—to see and to be seen. Before he started doing this as president of the hospital, he underestimated how important it was to stay visible to everyone—nurses, doctors, housekeeping, and so on.
“The impression that makes surprised me,” he says.
He’ll ask what people need to do their jobs better. He’ll also pop into patients’ rooms, introduce himself, and ask how their experiences have been. Then he takes that feedback and incorporates it into his planning.
Dr. Harte says he likes to have an “open and transparent” relationship with physicians and lists his credibility, both as a physician and a person, as a top attribute for a leader. For those embarking on leadership roles in a hospital, he says it’s a must to have a “strong mentor that you can go to.”
He also says a supportive environment is critical.
“You must work in an organization that is a resource to help you succeed, because when you move out of the purely clinical or clinical administrative jobs like division chair, department chair, program director, even CMO or VPMA [vice president of medical affairs], those are doctor jobs,” he says. “When you really become a doctor doing administrative work, unless it’s in your background and in your skill set, I think it’s important to work in an organization that is going to support you in your continued growth.
“Because these are jobs that I think you grow into.” —TC
I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment. You have pockets of enormous expertise that sometimes function like silos. Being a hospitalist actually trains you well for those things.
—Brian Harte, MD, SFHM, president, South Pointe Hospital, Warrenville Heights, Ohio, SHM board member

Dr. Nasim Afsar
Associate Chief Medical Officer, UCLA Hospitals, Los Angeles
Path to the C-suite: Residency at UCLA; advanced training program in quality improvement at Intermountain Healthcare Dr. Afsar wasn’t aiming for a top administrative job in a hospital. But, during her time spent working as a hospitalist, she started noticing trouble within the system. Eventually, she wanted to try to solve problems in a way that would have a ripple effect. Inspired, she ventured into quality improvement.
“I’m very passionate about helping the patient in front of me, whether it’s helping them get better or helping them during a really challenging time of their life,” she says. “But there’s something about feeling that the improvements that you make will not just impact the person in front of you, but the thousands of patients that come after them.”
Part of her job is instilling in other healthcare providers the sense that they themselves are agents of change. One big difference in her administrative job and clinical work is how to gauge success.
“The job is a lot harder than it seems. In our clinical world, I know what constitutes a good job. I know that when I’m on service, I get up early in the morning, I come in, I pre-round on my patients extensively, I read up on a couple of different things, I go out onto the wards with my team,” she explains. “This type of leadership role, I think, is more challenging. Initiatives that you do to improve care in one area could have detrimental or challenging impacts on another set of stakeholders or care area. You’re constantly navigating the system.” —TC
By nature when you’re a hospitalist, you are a problem solver. You don’t shy away from problems that you don’t understand.
—Nasim Afsar, MD, SFHM, associate chief medical officer, UCLA Hospitals, Los Angeles, SHM board member

Dr. Patrick Torcson
Chief Integration Officer, St. Tammany Parish Hospital, Covington, La.
Path to the C-Suite: Residency at Ochsner Clinic in New Orleans; private internist; director of hospital medicine at St. Tammany Parish Hospital Dr. Torcson recently became his hospital’s first chief integration officer, a job in which he promotes clinical quality and service quality using information technology.
But it was never about a promotion, he says.
“It’s really been more about just trying to provide quality care and make contributions to fixing a broken healthcare system,” he says. “Staying focused on that personal journey has really brought me to where I am.”
A good leader within a hospital is a “systems-level thinker,” not one focusing on a specific agenda. And, prioritizing important items is crucial to success, he notes.
“We all have a limited amount of energy. If you can pick three to five things that are really important and prioritize them and they turn out to be important, that’s going to facilitate your success,” he says.
He can’t emphasize “clinical credibility” enough. That’s where it all begins, he says.
“Your leadership is facilitated if you’re seen as someone that takes good care of your patients,” being the doctor that other doctors would want themselves and their families to go to. “That’s huge.”
Also, he says, running out and getting a master’s degree in business management and then applying for positions around the country is probably not the best approach to seeking out leadership positions, he says.
“I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something,” he points out. “Leadership is home-grown, and you work your way up.” —TC
I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something. Leadership is home-grown, and you work your way up.
—Patrick Torcson, MD, MMM, FACP, SFHM, vice president and chief integration officer, St. Tammany Parish Hospital, Covington, La., SHM board member

Dr. Steve Narang
CEO, Banner Health’s Good Samaritan Medical Center, Phoenix
Path to the C-suite: Medical school at Northwestern University; residency at Johns Hopkins; pediatric hospitalist at Children’s Hospital of New Orleans; medical director of Pediatric Hospitalists of Louisiana; master’s in healthcare management from Harvard; chief medical officer at Banner Health’s Cardon Children’s Medical Center
As a resident at Johns Hopkins in pediatrics, Dr. Narang wasn’t always pleased by what he saw—too many process errors and patient safety gaps, and too much waste. Healthcare resources were not being spent in the right way, he discovered.
“I was struck by [the fact] that we spent a lot of our resources in publishing more articles about what’s new, and what the coolest drug is,” he says. “I saw very little of that [relating to] what does this mean in terms of value?”
He became a hospitalist because he saw it as a role in which he could “really touch everything” if he chose to do so and work within the system to improve it.
“The hospital could use a partner,” he says. “One of the biggest challenges we have in healthcare is hospitals and physicians are often not working together to add value, and they’re subtracting from value, and they’re competing with each other.”
If doctors make the effort to learn the management aspects of working in a hospital, they can put themselves in a great position to take on big leadership roles, Dr. Narang says. He says hospitals are seeing the value in having physicians in those roles.
“If you can find the right leader and it happens to be a physician, if it happens to be a physician who can speak that language—and find a sweet spot for independent physicians, employed physicians, and hospitalists to deliver value, which we have to now I think it’s the best way to go,” he says. “I think you’re going to see a trend moving forward to this as more physicians become more interested in this track.” —TC
Being a hospitalist was a key strength of my background. Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
—Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix

Dr. Brian Harte
President, South Pointe Hospital, Warrenville Heights, Ohio
Path to the C-suite: Resident at University of California San Francisco; private practice hospitalist in Marin County, near San Francisco; hospitalist at Cleveland Clinic; program director of hospital medicine at Cleveland Clinic’s Euclid Hospital; chief operating officer at Cleveland Clinic’s Hillcrest Hospital For about two hours a day, Dr. Harte makes his way through South Pointe Hospital—to see and to be seen. Before he started doing this as president of the hospital, he underestimated how important it was to stay visible to everyone—nurses, doctors, housekeeping, and so on.
“The impression that makes surprised me,” he says.
He’ll ask what people need to do their jobs better. He’ll also pop into patients’ rooms, introduce himself, and ask how their experiences have been. Then he takes that feedback and incorporates it into his planning.
Dr. Harte says he likes to have an “open and transparent” relationship with physicians and lists his credibility, both as a physician and a person, as a top attribute for a leader. For those embarking on leadership roles in a hospital, he says it’s a must to have a “strong mentor that you can go to.”
He also says a supportive environment is critical.
“You must work in an organization that is a resource to help you succeed, because when you move out of the purely clinical or clinical administrative jobs like division chair, department chair, program director, even CMO or VPMA [vice president of medical affairs], those are doctor jobs,” he says. “When you really become a doctor doing administrative work, unless it’s in your background and in your skill set, I think it’s important to work in an organization that is going to support you in your continued growth.
“Because these are jobs that I think you grow into.” —TC
I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment. You have pockets of enormous expertise that sometimes function like silos. Being a hospitalist actually trains you well for those things.
—Brian Harte, MD, SFHM, president, South Pointe Hospital, Warrenville Heights, Ohio, SHM board member

Dr. Nasim Afsar
Associate Chief Medical Officer, UCLA Hospitals, Los Angeles
Path to the C-suite: Residency at UCLA; advanced training program in quality improvement at Intermountain Healthcare Dr. Afsar wasn’t aiming for a top administrative job in a hospital. But, during her time spent working as a hospitalist, she started noticing trouble within the system. Eventually, she wanted to try to solve problems in a way that would have a ripple effect. Inspired, she ventured into quality improvement.
“I’m very passionate about helping the patient in front of me, whether it’s helping them get better or helping them during a really challenging time of their life,” she says. “But there’s something about feeling that the improvements that you make will not just impact the person in front of you, but the thousands of patients that come after them.”
Part of her job is instilling in other healthcare providers the sense that they themselves are agents of change. One big difference in her administrative job and clinical work is how to gauge success.
“The job is a lot harder than it seems. In our clinical world, I know what constitutes a good job. I know that when I’m on service, I get up early in the morning, I come in, I pre-round on my patients extensively, I read up on a couple of different things, I go out onto the wards with my team,” she explains. “This type of leadership role, I think, is more challenging. Initiatives that you do to improve care in one area could have detrimental or challenging impacts on another set of stakeholders or care area. You’re constantly navigating the system.” —TC
By nature when you’re a hospitalist, you are a problem solver. You don’t shy away from problems that you don’t understand.
—Nasim Afsar, MD, SFHM, associate chief medical officer, UCLA Hospitals, Los Angeles, SHM board member

Dr. Patrick Torcson
Chief Integration Officer, St. Tammany Parish Hospital, Covington, La.
Path to the C-Suite: Residency at Ochsner Clinic in New Orleans; private internist; director of hospital medicine at St. Tammany Parish Hospital Dr. Torcson recently became his hospital’s first chief integration officer, a job in which he promotes clinical quality and service quality using information technology.
But it was never about a promotion, he says.
“It’s really been more about just trying to provide quality care and make contributions to fixing a broken healthcare system,” he says. “Staying focused on that personal journey has really brought me to where I am.”
A good leader within a hospital is a “systems-level thinker,” not one focusing on a specific agenda. And, prioritizing important items is crucial to success, he notes.
“We all have a limited amount of energy. If you can pick three to five things that are really important and prioritize them and they turn out to be important, that’s going to facilitate your success,” he says.
He can’t emphasize “clinical credibility” enough. That’s where it all begins, he says.
“Your leadership is facilitated if you’re seen as someone that takes good care of your patients,” being the doctor that other doctors would want themselves and their families to go to. “That’s huge.”
Also, he says, running out and getting a master’s degree in business management and then applying for positions around the country is probably not the best approach to seeking out leadership positions, he says.
“I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something,” he points out. “Leadership is home-grown, and you work your way up.” —TC
I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something. Leadership is home-grown, and you work your way up.
—Patrick Torcson, MD, MMM, FACP, SFHM, vice president and chief integration officer, St. Tammany Parish Hospital, Covington, La., SHM board member

Dr. Steve Narang
CEO, Banner Health’s Good Samaritan Medical Center, Phoenix
Path to the C-suite: Medical school at Northwestern University; residency at Johns Hopkins; pediatric hospitalist at Children’s Hospital of New Orleans; medical director of Pediatric Hospitalists of Louisiana; master’s in healthcare management from Harvard; chief medical officer at Banner Health’s Cardon Children’s Medical Center
As a resident at Johns Hopkins in pediatrics, Dr. Narang wasn’t always pleased by what he saw—too many process errors and patient safety gaps, and too much waste. Healthcare resources were not being spent in the right way, he discovered.
“I was struck by [the fact] that we spent a lot of our resources in publishing more articles about what’s new, and what the coolest drug is,” he says. “I saw very little of that [relating to] what does this mean in terms of value?”
He became a hospitalist because he saw it as a role in which he could “really touch everything” if he chose to do so and work within the system to improve it.
“The hospital could use a partner,” he says. “One of the biggest challenges we have in healthcare is hospitals and physicians are often not working together to add value, and they’re subtracting from value, and they’re competing with each other.”
If doctors make the effort to learn the management aspects of working in a hospital, they can put themselves in a great position to take on big leadership roles, Dr. Narang says. He says hospitals are seeing the value in having physicians in those roles.
“If you can find the right leader and it happens to be a physician, if it happens to be a physician who can speak that language—and find a sweet spot for independent physicians, employed physicians, and hospitalists to deliver value, which we have to now I think it’s the best way to go,” he says. “I think you’re going to see a trend moving forward to this as more physicians become more interested in this track.” —TC
Being a hospitalist was a key strength of my background. Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
—Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix

Dr. Brian Harte
President, South Pointe Hospital, Warrenville Heights, Ohio
Path to the C-suite: Resident at University of California San Francisco; private practice hospitalist in Marin County, near San Francisco; hospitalist at Cleveland Clinic; program director of hospital medicine at Cleveland Clinic’s Euclid Hospital; chief operating officer at Cleveland Clinic’s Hillcrest Hospital For about two hours a day, Dr. Harte makes his way through South Pointe Hospital—to see and to be seen. Before he started doing this as president of the hospital, he underestimated how important it was to stay visible to everyone—nurses, doctors, housekeeping, and so on.
“The impression that makes surprised me,” he says.
He’ll ask what people need to do their jobs better. He’ll also pop into patients’ rooms, introduce himself, and ask how their experiences have been. Then he takes that feedback and incorporates it into his planning.
Dr. Harte says he likes to have an “open and transparent” relationship with physicians and lists his credibility, both as a physician and a person, as a top attribute for a leader. For those embarking on leadership roles in a hospital, he says it’s a must to have a “strong mentor that you can go to.”
He also says a supportive environment is critical.
“You must work in an organization that is a resource to help you succeed, because when you move out of the purely clinical or clinical administrative jobs like division chair, department chair, program director, even CMO or VPMA [vice president of medical affairs], those are doctor jobs,” he says. “When you really become a doctor doing administrative work, unless it’s in your background and in your skill set, I think it’s important to work in an organization that is going to support you in your continued growth.
“Because these are jobs that I think you grow into.” —TC
I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment. You have pockets of enormous expertise that sometimes function like silos. Being a hospitalist actually trains you well for those things.
—Brian Harte, MD, SFHM, president, South Pointe Hospital, Warrenville Heights, Ohio, SHM board member

Dr. Nasim Afsar
Associate Chief Medical Officer, UCLA Hospitals, Los Angeles
Path to the C-suite: Residency at UCLA; advanced training program in quality improvement at Intermountain Healthcare Dr. Afsar wasn’t aiming for a top administrative job in a hospital. But, during her time spent working as a hospitalist, she started noticing trouble within the system. Eventually, she wanted to try to solve problems in a way that would have a ripple effect. Inspired, she ventured into quality improvement.
“I’m very passionate about helping the patient in front of me, whether it’s helping them get better or helping them during a really challenging time of their life,” she says. “But there’s something about feeling that the improvements that you make will not just impact the person in front of you, but the thousands of patients that come after them.”
Part of her job is instilling in other healthcare providers the sense that they themselves are agents of change. One big difference in her administrative job and clinical work is how to gauge success.
“The job is a lot harder than it seems. In our clinical world, I know what constitutes a good job. I know that when I’m on service, I get up early in the morning, I come in, I pre-round on my patients extensively, I read up on a couple of different things, I go out onto the wards with my team,” she explains. “This type of leadership role, I think, is more challenging. Initiatives that you do to improve care in one area could have detrimental or challenging impacts on another set of stakeholders or care area. You’re constantly navigating the system.” —TC
By nature when you’re a hospitalist, you are a problem solver. You don’t shy away from problems that you don’t understand.
—Nasim Afsar, MD, SFHM, associate chief medical officer, UCLA Hospitals, Los Angeles, SHM board member

Dr. Patrick Torcson
Chief Integration Officer, St. Tammany Parish Hospital, Covington, La.
Path to the C-Suite: Residency at Ochsner Clinic in New Orleans; private internist; director of hospital medicine at St. Tammany Parish Hospital Dr. Torcson recently became his hospital’s first chief integration officer, a job in which he promotes clinical quality and service quality using information technology.
But it was never about a promotion, he says.
“It’s really been more about just trying to provide quality care and make contributions to fixing a broken healthcare system,” he says. “Staying focused on that personal journey has really brought me to where I am.”
A good leader within a hospital is a “systems-level thinker,” not one focusing on a specific agenda. And, prioritizing important items is crucial to success, he notes.
“We all have a limited amount of energy. If you can pick three to five things that are really important and prioritize them and they turn out to be important, that’s going to facilitate your success,” he says.
He can’t emphasize “clinical credibility” enough. That’s where it all begins, he says.
“Your leadership is facilitated if you’re seen as someone that takes good care of your patients,” being the doctor that other doctors would want themselves and their families to go to. “That’s huge.”
Also, he says, running out and getting a master’s degree in business management and then applying for positions around the country is probably not the best approach to seeking out leadership positions, he says.
“I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something,” he points out. “Leadership is home-grown, and you work your way up.” —TC
I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something. Leadership is home-grown, and you work your way up.
—Patrick Torcson, MD, MMM, FACP, SFHM, vice president and chief integration officer, St. Tammany Parish Hospital, Covington, La., SHM board member
Hospitalists’ Skill Sets, Work Experience Perfect for Hospitals' C-Suite Positions
Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix, was attending a leadership summit where all of Banner’s top officials were gathered. It was his third day in his new job.
Banner’s President, Peter Fine, gave a presentation in the future of healthcare and asked for questions. Dr. Narang stepped up to the microphone, asked a question, and made remarks about how the organization needed to ready itself for the changing landscape. Kathy Bollinger, president of the Arizona West Region of Banner, was struck by those remarks. Less than two years later, she made Dr. Narang the CEO at Arizona’s largest teaching hospital, Good Samaritan Medical Center.
His hospitalist background was an important ingredient in the kind of leader Dr. Narang has become, she says.
“The correlation is that hospitalists are leading teams; they are quarterbacking care,” Bollinger adds. “A good hospitalist brings the team together.”
Physicians with a background in hospital medicine are no strangers to C-suite level positions at hospitals. In April, Brian Harte, MD, SFHM, was named president of South Pointe Hospital in Warrenville Heights, Ohio, a center within the Cleveland Clinic system. In January, Patrick Cawley, MD, MBA, MHM, a former SHM president, was named CEO at the Medical University of South Carolina Medical Center in Charleston.
Other recent C-suite arrivals include Nasim Afsar, MD, SFHM, an SHM board member who is associate CMO at UCLA Hospitals in Los Angeles, and Patrick Torcson, MD, MMM, FACP, SFHM, another SHM board member, vice president, and chief integration officer at St. Tammany Parish Hospital in Covington, La.
Although their paths to the C-suite have differed, each agrees that their experience in hospital medicine gave them the knowledge of the system that was required to begin an ascent to the highest levels of leadership. Just as important, or maybe more so, their exposure to the inner workings of a hospital awakened within them a desire to see the system function better. And the necessity of working with all types of healthcare providers within the complicated hospital setting helped them recognize—or at least get others to recognize—their potential for leadership, and helped hone the teamwork skills that are vital in top administrative roles.
They also say that, when they were starting out, they never aspired to high leadership positions. Rather, it was simply following their own interests that ultimately led them there.
By the time Dr. Narang stepped up to the microphone that day in Phoenix, he had more than a dozen years under his belt working as a hospitalist for a children’s hospital and as part of a group that created a pediatric hospitalist company in Louisiana.
And that work helped lay the foundation for him, he says.
“Being a hospitalist was a key strength of my background,” Dr. Narang explains. “Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
“At the end of the day, it’s about leadership. And I learned that from day one as a hospitalist.”
His confidence and sense of the big picture were not lost on Bollinger that day at the leadership summit.
“I thought that took a fair amount of courage,” she says, “on Day 3, to stand up to the mic and have [a] specific conversation with the president of the company. In my mind, he was very enlightened. His comments were very enlightened.”
Firm Foundation
Robert Zipper, MD, MMM, SFHM, chair of SHM’s Leadership Committee, and CMO of Sound Physicians’ West Region, says it’s probably not realistic for a hospitalist to vault up immediately to a chief executive officer position. Pursuing lower-level leadership roles would be a good starting point for hospitalists with C-suite aspirations, he says.
“For those just starting out, I would recommend that they seek out opportunities to lead or be a part of managing change in their hospitals. The right opportunities should feel like a bit of a stretch, but not overwhelming. This might be work in quality, medical staff leadership, etc.,” Dr. Zipper says.
For hospitalists with leadership experience, CMO and vice president of medical affairs have the closest translation, he adds. He also says jobs like chief informatics officer and roles in quality improvement are highly suitable for hospitalists.
According to the 2011 Cejka Executive Search Physician Executive Compensation Survey, a survey of the American College of Physician Executives’ membership of physicians in management, the median salary of physicians in CEO positions was $393,152. That figure was $343,334 for CMO and $307,500 for chief quality and patient safety officer. The median for all physician executive positions was $305,000. Compensation was typically higher in academic medical centers and lower for hospitals and multi-specialty groups.
Hospitalists in executive positions had a 2011 median income of $275,000, according to the survey.
The survey also showed a wide range of compensation, typically dependent on the size of the institution. Some hospitalist leaders with more than 75% of their full-time-equivalent hours worked clinically “might actually take a small pay cut to make a move,” Dr. Zipper says.
Natural Progression
The hospitalist executives interviewed, for the most part, were emphatic that C-suite level leadership was not something that they imagined for themselves when they began their medical careers.
“In 2007, I could never imagine doing anything less than 100 percent clinical hospitalist work,” UCLA Hospitals’ Dr. Afsar says. “But once I started working and doing my hospitalist job day in and day out, I realized that there were many aspects of our care where I knew we could do better.”
Dr. Harte, president of South Pointe Hospital in Cleveland, says he never really thought about hospital administration as a career ambition. But, “opportunities presented themselves.”
Dr. Torcson says he was so firmly disinterested in administrative positions that when he was asked to join the Medical Executive Committee at his hospital, his first thought was “no way … I’m a doctor, not an administrator.” But after talking to some senior colleagues about it, they reminded him that he was basically obliged to say “yes.” And it ended up being a crucial component in his ascent through the ranks.
Dr. Narang imagined having a career that impacted value fairly early on, after making observations during his pediatric residency. But even he was surprised when he got the call to be CEO, after less than two years on the job.
Now, in retrospect, they all see their years working as a rank-and-file hospitalist as formative.
As a leader in a hospital, you have to be good at recruiting physicians, retaining them and developing them professionally, Dr. Harte says. That requires having clinical credibility, being a decent mentor, being a good role model, and “wearing your integrity on your sleeve.”
“I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment,” Dr. Harte notes. “You have pockets of enormous expertise that sometimes function like silos.
“Being a hospitalist actually trains you well for those things. By nature of what we do, we tend to be folks who do multi-disciplinary rounds. We can sit around a table or walk rounds with nurses, case managers, physical therapists, respiratory therapists, and the like, and actually develop a plan of care that recognizes the expertise of the other individuals within that group. That is a very good incubator for that kind of thinking.”
Hospital leaders also have to know how everything works together within the hospital.
“Hospital medicine has this overlap with that domain as it is,” Dr. Harte continues. “We work in hospitals. It is not such a stretch then, to think that we could be running a hospital.”
Golden Opportunity
Dr. Torcson says the opportunities to lead in the hospital setting abound. A former internist, he says hospitalists are primed to “improve quality and service at the hospital level because of the system-based approach to hospital care.”
Dealing with incomplete information and uncertainty are important challenges for hospital leaders, something Dr. Afsar says are daily hurdles for hospitalists.
“By nature when you’re a hospitalist, you are a problem solver,” she says. “You don’t shy away from problems that you don’t understand.”
That problem-solver outlook is what prompted Neil Martin, MD, chief of neurosurgery at UCLA, to ask Dr. Afsar to join a quality improvement program within the department—first as a participant and then as its leader.
“She was always one of the most active and vocal and solution-oriented people on the committees that I was participating in,” Dr. Martin says. “She was not the kind of person who would describe all of the problems and leave it at that. But, rather, [she] would help identify problems and then propose solutions and then help follow through to implement solutions.”
Hospitalist C-suiters describe days dominated by meetings with executive teams, staff, and individual physicians or groups. Meetings are a necessity, as executives are tasked with crafting a vision, constantly assessing progress, and refining the approach when necessary.
Continuing at least some clinical work is important, Dr. Harte says. It depends on the organization, but he says he sees benefits that help him in his administrative duties.
“It changes the dynamic of the interaction with some of the naysayers on the medical staff,” he says. “That’s still something that I enjoy doing. I think it’s important for me, it’s important for the credibility of my job, and particularly for the organization that I work at.”
A lot of C-suiters sought out formal training in administrative areas—though not necessarily an MBA—once they realized they had an interest in administration.
Dr. Torcson says getting a master’s in medical management degree was “absolutely invaluable.”
“It was obvious to me that I had some needs to develop some additional competencies and capabilities, a different skill set than I gained in medical school and residency,” he says. “The same skill set that makes one a successful or quality physician isn’t necessarily the same skill set that you need to be an effective manager or administrator.”
Dr. Afsar completed an advanced quality improvement training program at Intermountain Healthcare, and Dr. Narang received a master’s in healthcare management from Harvard.
Dr. Harte, who does not have an advanced management degree, says that at some institutions, such as Cleveland Clinic, you can learn on the job the non-clinical areas needed to be a top leader in a hospital, including finance and strategy.
Dr. Zipper says a related degree can be a big leg up.
“If one is specifically looking to enter the C-suite, an advanced business or management degree will make that barrier a lot lower,” he says. Whether that degree is a master’s in business administration, healthcare administration, medical management, or a similar degree doesn’t seem to matter much, he adds.
When she was looking for a new CEO for Good Samaritan Medical Center, Bollinger says that she preferred to hire a physician. That candidate, she says, had to have certain leadership qualities, including the ability to create a suitable vision, curiosity, an “executive presence,” and a “tolerance of ambiguity.”
As it turns out, the value of having a physician CEO has been “probably three times what I anticipated,” she says.
If you’re a hospitalist and have an interest in rising up the leadership ladder, getting involved and getting exposure to areas of interest is where it begins.
“I would say go for it,” Dr. Afsar says. “Raising your hand and being willing to take on responsibility are kind of the first steps in getting involved. I think it’s just as much making sure that you’re the right fit for that type of work, as it is to excel and do well. Not everyone, I think, will thrive and enjoy this type of work. So I think having the opportunity to get exposed to it and see if it’s something that you enjoy is a critical piece.”
Tom Collins is a freelance writer in Florida.
Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix, was attending a leadership summit where all of Banner’s top officials were gathered. It was his third day in his new job.
Banner’s President, Peter Fine, gave a presentation in the future of healthcare and asked for questions. Dr. Narang stepped up to the microphone, asked a question, and made remarks about how the organization needed to ready itself for the changing landscape. Kathy Bollinger, president of the Arizona West Region of Banner, was struck by those remarks. Less than two years later, she made Dr. Narang the CEO at Arizona’s largest teaching hospital, Good Samaritan Medical Center.
His hospitalist background was an important ingredient in the kind of leader Dr. Narang has become, she says.
“The correlation is that hospitalists are leading teams; they are quarterbacking care,” Bollinger adds. “A good hospitalist brings the team together.”
Physicians with a background in hospital medicine are no strangers to C-suite level positions at hospitals. In April, Brian Harte, MD, SFHM, was named president of South Pointe Hospital in Warrenville Heights, Ohio, a center within the Cleveland Clinic system. In January, Patrick Cawley, MD, MBA, MHM, a former SHM president, was named CEO at the Medical University of South Carolina Medical Center in Charleston.
Other recent C-suite arrivals include Nasim Afsar, MD, SFHM, an SHM board member who is associate CMO at UCLA Hospitals in Los Angeles, and Patrick Torcson, MD, MMM, FACP, SFHM, another SHM board member, vice president, and chief integration officer at St. Tammany Parish Hospital in Covington, La.
Although their paths to the C-suite have differed, each agrees that their experience in hospital medicine gave them the knowledge of the system that was required to begin an ascent to the highest levels of leadership. Just as important, or maybe more so, their exposure to the inner workings of a hospital awakened within them a desire to see the system function better. And the necessity of working with all types of healthcare providers within the complicated hospital setting helped them recognize—or at least get others to recognize—their potential for leadership, and helped hone the teamwork skills that are vital in top administrative roles.
They also say that, when they were starting out, they never aspired to high leadership positions. Rather, it was simply following their own interests that ultimately led them there.
By the time Dr. Narang stepped up to the microphone that day in Phoenix, he had more than a dozen years under his belt working as a hospitalist for a children’s hospital and as part of a group that created a pediatric hospitalist company in Louisiana.
And that work helped lay the foundation for him, he says.
“Being a hospitalist was a key strength of my background,” Dr. Narang explains. “Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
“At the end of the day, it’s about leadership. And I learned that from day one as a hospitalist.”
His confidence and sense of the big picture were not lost on Bollinger that day at the leadership summit.
“I thought that took a fair amount of courage,” she says, “on Day 3, to stand up to the mic and have [a] specific conversation with the president of the company. In my mind, he was very enlightened. His comments were very enlightened.”
Firm Foundation
Robert Zipper, MD, MMM, SFHM, chair of SHM’s Leadership Committee, and CMO of Sound Physicians’ West Region, says it’s probably not realistic for a hospitalist to vault up immediately to a chief executive officer position. Pursuing lower-level leadership roles would be a good starting point for hospitalists with C-suite aspirations, he says.
“For those just starting out, I would recommend that they seek out opportunities to lead or be a part of managing change in their hospitals. The right opportunities should feel like a bit of a stretch, but not overwhelming. This might be work in quality, medical staff leadership, etc.,” Dr. Zipper says.
For hospitalists with leadership experience, CMO and vice president of medical affairs have the closest translation, he adds. He also says jobs like chief informatics officer and roles in quality improvement are highly suitable for hospitalists.
According to the 2011 Cejka Executive Search Physician Executive Compensation Survey, a survey of the American College of Physician Executives’ membership of physicians in management, the median salary of physicians in CEO positions was $393,152. That figure was $343,334 for CMO and $307,500 for chief quality and patient safety officer. The median for all physician executive positions was $305,000. Compensation was typically higher in academic medical centers and lower for hospitals and multi-specialty groups.
Hospitalists in executive positions had a 2011 median income of $275,000, according to the survey.
The survey also showed a wide range of compensation, typically dependent on the size of the institution. Some hospitalist leaders with more than 75% of their full-time-equivalent hours worked clinically “might actually take a small pay cut to make a move,” Dr. Zipper says.
Natural Progression
The hospitalist executives interviewed, for the most part, were emphatic that C-suite level leadership was not something that they imagined for themselves when they began their medical careers.
“In 2007, I could never imagine doing anything less than 100 percent clinical hospitalist work,” UCLA Hospitals’ Dr. Afsar says. “But once I started working and doing my hospitalist job day in and day out, I realized that there were many aspects of our care where I knew we could do better.”
Dr. Harte, president of South Pointe Hospital in Cleveland, says he never really thought about hospital administration as a career ambition. But, “opportunities presented themselves.”
Dr. Torcson says he was so firmly disinterested in administrative positions that when he was asked to join the Medical Executive Committee at his hospital, his first thought was “no way … I’m a doctor, not an administrator.” But after talking to some senior colleagues about it, they reminded him that he was basically obliged to say “yes.” And it ended up being a crucial component in his ascent through the ranks.
Dr. Narang imagined having a career that impacted value fairly early on, after making observations during his pediatric residency. But even he was surprised when he got the call to be CEO, after less than two years on the job.
Now, in retrospect, they all see their years working as a rank-and-file hospitalist as formative.
As a leader in a hospital, you have to be good at recruiting physicians, retaining them and developing them professionally, Dr. Harte says. That requires having clinical credibility, being a decent mentor, being a good role model, and “wearing your integrity on your sleeve.”
“I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment,” Dr. Harte notes. “You have pockets of enormous expertise that sometimes function like silos.
“Being a hospitalist actually trains you well for those things. By nature of what we do, we tend to be folks who do multi-disciplinary rounds. We can sit around a table or walk rounds with nurses, case managers, physical therapists, respiratory therapists, and the like, and actually develop a plan of care that recognizes the expertise of the other individuals within that group. That is a very good incubator for that kind of thinking.”
Hospital leaders also have to know how everything works together within the hospital.
“Hospital medicine has this overlap with that domain as it is,” Dr. Harte continues. “We work in hospitals. It is not such a stretch then, to think that we could be running a hospital.”
Golden Opportunity
Dr. Torcson says the opportunities to lead in the hospital setting abound. A former internist, he says hospitalists are primed to “improve quality and service at the hospital level because of the system-based approach to hospital care.”
Dealing with incomplete information and uncertainty are important challenges for hospital leaders, something Dr. Afsar says are daily hurdles for hospitalists.
“By nature when you’re a hospitalist, you are a problem solver,” she says. “You don’t shy away from problems that you don’t understand.”
That problem-solver outlook is what prompted Neil Martin, MD, chief of neurosurgery at UCLA, to ask Dr. Afsar to join a quality improvement program within the department—first as a participant and then as its leader.
“She was always one of the most active and vocal and solution-oriented people on the committees that I was participating in,” Dr. Martin says. “She was not the kind of person who would describe all of the problems and leave it at that. But, rather, [she] would help identify problems and then propose solutions and then help follow through to implement solutions.”
Hospitalist C-suiters describe days dominated by meetings with executive teams, staff, and individual physicians or groups. Meetings are a necessity, as executives are tasked with crafting a vision, constantly assessing progress, and refining the approach when necessary.
Continuing at least some clinical work is important, Dr. Harte says. It depends on the organization, but he says he sees benefits that help him in his administrative duties.
“It changes the dynamic of the interaction with some of the naysayers on the medical staff,” he says. “That’s still something that I enjoy doing. I think it’s important for me, it’s important for the credibility of my job, and particularly for the organization that I work at.”
A lot of C-suiters sought out formal training in administrative areas—though not necessarily an MBA—once they realized they had an interest in administration.
Dr. Torcson says getting a master’s in medical management degree was “absolutely invaluable.”
“It was obvious to me that I had some needs to develop some additional competencies and capabilities, a different skill set than I gained in medical school and residency,” he says. “The same skill set that makes one a successful or quality physician isn’t necessarily the same skill set that you need to be an effective manager or administrator.”
Dr. Afsar completed an advanced quality improvement training program at Intermountain Healthcare, and Dr. Narang received a master’s in healthcare management from Harvard.
Dr. Harte, who does not have an advanced management degree, says that at some institutions, such as Cleveland Clinic, you can learn on the job the non-clinical areas needed to be a top leader in a hospital, including finance and strategy.
Dr. Zipper says a related degree can be a big leg up.
“If one is specifically looking to enter the C-suite, an advanced business or management degree will make that barrier a lot lower,” he says. Whether that degree is a master’s in business administration, healthcare administration, medical management, or a similar degree doesn’t seem to matter much, he adds.
When she was looking for a new CEO for Good Samaritan Medical Center, Bollinger says that she preferred to hire a physician. That candidate, she says, had to have certain leadership qualities, including the ability to create a suitable vision, curiosity, an “executive presence,” and a “tolerance of ambiguity.”
As it turns out, the value of having a physician CEO has been “probably three times what I anticipated,” she says.
If you’re a hospitalist and have an interest in rising up the leadership ladder, getting involved and getting exposure to areas of interest is where it begins.
“I would say go for it,” Dr. Afsar says. “Raising your hand and being willing to take on responsibility are kind of the first steps in getting involved. I think it’s just as much making sure that you’re the right fit for that type of work, as it is to excel and do well. Not everyone, I think, will thrive and enjoy this type of work. So I think having the opportunity to get exposed to it and see if it’s something that you enjoy is a critical piece.”
Tom Collins is a freelance writer in Florida.
Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix, was attending a leadership summit where all of Banner’s top officials were gathered. It was his third day in his new job.
Banner’s President, Peter Fine, gave a presentation in the future of healthcare and asked for questions. Dr. Narang stepped up to the microphone, asked a question, and made remarks about how the organization needed to ready itself for the changing landscape. Kathy Bollinger, president of the Arizona West Region of Banner, was struck by those remarks. Less than two years later, she made Dr. Narang the CEO at Arizona’s largest teaching hospital, Good Samaritan Medical Center.
His hospitalist background was an important ingredient in the kind of leader Dr. Narang has become, she says.
“The correlation is that hospitalists are leading teams; they are quarterbacking care,” Bollinger adds. “A good hospitalist brings the team together.”
Physicians with a background in hospital medicine are no strangers to C-suite level positions at hospitals. In April, Brian Harte, MD, SFHM, was named president of South Pointe Hospital in Warrenville Heights, Ohio, a center within the Cleveland Clinic system. In January, Patrick Cawley, MD, MBA, MHM, a former SHM president, was named CEO at the Medical University of South Carolina Medical Center in Charleston.
Other recent C-suite arrivals include Nasim Afsar, MD, SFHM, an SHM board member who is associate CMO at UCLA Hospitals in Los Angeles, and Patrick Torcson, MD, MMM, FACP, SFHM, another SHM board member, vice president, and chief integration officer at St. Tammany Parish Hospital in Covington, La.
Although their paths to the C-suite have differed, each agrees that their experience in hospital medicine gave them the knowledge of the system that was required to begin an ascent to the highest levels of leadership. Just as important, or maybe more so, their exposure to the inner workings of a hospital awakened within them a desire to see the system function better. And the necessity of working with all types of healthcare providers within the complicated hospital setting helped them recognize—or at least get others to recognize—their potential for leadership, and helped hone the teamwork skills that are vital in top administrative roles.
They also say that, when they were starting out, they never aspired to high leadership positions. Rather, it was simply following their own interests that ultimately led them there.
By the time Dr. Narang stepped up to the microphone that day in Phoenix, he had more than a dozen years under his belt working as a hospitalist for a children’s hospital and as part of a group that created a pediatric hospitalist company in Louisiana.
And that work helped lay the foundation for him, he says.
“Being a hospitalist was a key strength of my background,” Dr. Narang explains. “Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
“At the end of the day, it’s about leadership. And I learned that from day one as a hospitalist.”
His confidence and sense of the big picture were not lost on Bollinger that day at the leadership summit.
“I thought that took a fair amount of courage,” she says, “on Day 3, to stand up to the mic and have [a] specific conversation with the president of the company. In my mind, he was very enlightened. His comments were very enlightened.”
Firm Foundation
Robert Zipper, MD, MMM, SFHM, chair of SHM’s Leadership Committee, and CMO of Sound Physicians’ West Region, says it’s probably not realistic for a hospitalist to vault up immediately to a chief executive officer position. Pursuing lower-level leadership roles would be a good starting point for hospitalists with C-suite aspirations, he says.
“For those just starting out, I would recommend that they seek out opportunities to lead or be a part of managing change in their hospitals. The right opportunities should feel like a bit of a stretch, but not overwhelming. This might be work in quality, medical staff leadership, etc.,” Dr. Zipper says.
For hospitalists with leadership experience, CMO and vice president of medical affairs have the closest translation, he adds. He also says jobs like chief informatics officer and roles in quality improvement are highly suitable for hospitalists.
According to the 2011 Cejka Executive Search Physician Executive Compensation Survey, a survey of the American College of Physician Executives’ membership of physicians in management, the median salary of physicians in CEO positions was $393,152. That figure was $343,334 for CMO and $307,500 for chief quality and patient safety officer. The median for all physician executive positions was $305,000. Compensation was typically higher in academic medical centers and lower for hospitals and multi-specialty groups.
Hospitalists in executive positions had a 2011 median income of $275,000, according to the survey.
The survey also showed a wide range of compensation, typically dependent on the size of the institution. Some hospitalist leaders with more than 75% of their full-time-equivalent hours worked clinically “might actually take a small pay cut to make a move,” Dr. Zipper says.
Natural Progression
The hospitalist executives interviewed, for the most part, were emphatic that C-suite level leadership was not something that they imagined for themselves when they began their medical careers.
“In 2007, I could never imagine doing anything less than 100 percent clinical hospitalist work,” UCLA Hospitals’ Dr. Afsar says. “But once I started working and doing my hospitalist job day in and day out, I realized that there were many aspects of our care where I knew we could do better.”
Dr. Harte, president of South Pointe Hospital in Cleveland, says he never really thought about hospital administration as a career ambition. But, “opportunities presented themselves.”
Dr. Torcson says he was so firmly disinterested in administrative positions that when he was asked to join the Medical Executive Committee at his hospital, his first thought was “no way … I’m a doctor, not an administrator.” But after talking to some senior colleagues about it, they reminded him that he was basically obliged to say “yes.” And it ended up being a crucial component in his ascent through the ranks.
Dr. Narang imagined having a career that impacted value fairly early on, after making observations during his pediatric residency. But even he was surprised when he got the call to be CEO, after less than two years on the job.
Now, in retrospect, they all see their years working as a rank-and-file hospitalist as formative.
As a leader in a hospital, you have to be good at recruiting physicians, retaining them and developing them professionally, Dr. Harte says. That requires having clinical credibility, being a decent mentor, being a good role model, and “wearing your integrity on your sleeve.”
“I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment,” Dr. Harte notes. “You have pockets of enormous expertise that sometimes function like silos.
“Being a hospitalist actually trains you well for those things. By nature of what we do, we tend to be folks who do multi-disciplinary rounds. We can sit around a table or walk rounds with nurses, case managers, physical therapists, respiratory therapists, and the like, and actually develop a plan of care that recognizes the expertise of the other individuals within that group. That is a very good incubator for that kind of thinking.”
Hospital leaders also have to know how everything works together within the hospital.
“Hospital medicine has this overlap with that domain as it is,” Dr. Harte continues. “We work in hospitals. It is not such a stretch then, to think that we could be running a hospital.”
Golden Opportunity
Dr. Torcson says the opportunities to lead in the hospital setting abound. A former internist, he says hospitalists are primed to “improve quality and service at the hospital level because of the system-based approach to hospital care.”
Dealing with incomplete information and uncertainty are important challenges for hospital leaders, something Dr. Afsar says are daily hurdles for hospitalists.
“By nature when you’re a hospitalist, you are a problem solver,” she says. “You don’t shy away from problems that you don’t understand.”
That problem-solver outlook is what prompted Neil Martin, MD, chief of neurosurgery at UCLA, to ask Dr. Afsar to join a quality improvement program within the department—first as a participant and then as its leader.
“She was always one of the most active and vocal and solution-oriented people on the committees that I was participating in,” Dr. Martin says. “She was not the kind of person who would describe all of the problems and leave it at that. But, rather, [she] would help identify problems and then propose solutions and then help follow through to implement solutions.”
Hospitalist C-suiters describe days dominated by meetings with executive teams, staff, and individual physicians or groups. Meetings are a necessity, as executives are tasked with crafting a vision, constantly assessing progress, and refining the approach when necessary.
Continuing at least some clinical work is important, Dr. Harte says. It depends on the organization, but he says he sees benefits that help him in his administrative duties.
“It changes the dynamic of the interaction with some of the naysayers on the medical staff,” he says. “That’s still something that I enjoy doing. I think it’s important for me, it’s important for the credibility of my job, and particularly for the organization that I work at.”
A lot of C-suiters sought out formal training in administrative areas—though not necessarily an MBA—once they realized they had an interest in administration.
Dr. Torcson says getting a master’s in medical management degree was “absolutely invaluable.”
“It was obvious to me that I had some needs to develop some additional competencies and capabilities, a different skill set than I gained in medical school and residency,” he says. “The same skill set that makes one a successful or quality physician isn’t necessarily the same skill set that you need to be an effective manager or administrator.”
Dr. Afsar completed an advanced quality improvement training program at Intermountain Healthcare, and Dr. Narang received a master’s in healthcare management from Harvard.
Dr. Harte, who does not have an advanced management degree, says that at some institutions, such as Cleveland Clinic, you can learn on the job the non-clinical areas needed to be a top leader in a hospital, including finance and strategy.
Dr. Zipper says a related degree can be a big leg up.
“If one is specifically looking to enter the C-suite, an advanced business or management degree will make that barrier a lot lower,” he says. Whether that degree is a master’s in business administration, healthcare administration, medical management, or a similar degree doesn’t seem to matter much, he adds.
When she was looking for a new CEO for Good Samaritan Medical Center, Bollinger says that she preferred to hire a physician. That candidate, she says, had to have certain leadership qualities, including the ability to create a suitable vision, curiosity, an “executive presence,” and a “tolerance of ambiguity.”
As it turns out, the value of having a physician CEO has been “probably three times what I anticipated,” she says.
If you’re a hospitalist and have an interest in rising up the leadership ladder, getting involved and getting exposure to areas of interest is where it begins.
“I would say go for it,” Dr. Afsar says. “Raising your hand and being willing to take on responsibility are kind of the first steps in getting involved. I think it’s just as much making sure that you’re the right fit for that type of work, as it is to excel and do well. Not everyone, I think, will thrive and enjoy this type of work. So I think having the opportunity to get exposed to it and see if it’s something that you enjoy is a critical piece.”
Tom Collins is a freelance writer in Florida.
Two Major Studies Show Benefits of CAUTI Reduction Measures
Conscientious handling of urinary catheters is one of the main responsibilities hospitalists have in caring for patients with urological disorders—and, of course, anyone else with a urinary catheter.
Treatment of patients with urological disorders often involves special circumstances requiring physician discretion when deciding whether to remove a catheter or leave it in—removing it too soon could cause problems far worse than an infection. But two compelling studies, nationwide in scope, point to the benefits of systems that help ensure prompt removal of urinary catheters when appropriate.
One, published in 2010, was a review of interventional studies that used reminders to physicians or nurses that a urinary catheter was in use or stop orders to trigger catheter removal in hospitalized adults.
Researchers found that the rate of catheter-associated urinary tract infections, measured as episodes per 1,000 catheter-days, was reduced by 52% (P<0.001) with use of a reminder or stop order. The average duration of catheterization decreased by 37%. That amounted to 2.61 fewer days of catheterization per patient in the intervention compared to control groups.
In a 2013 study published in JAMA Internal Medicine, researchers surveyed infection prevention specialists at a sample of hospitals across the U.S.—and at all hospitals in Michigan, home to a statewide CAUTI-prevention initiative started in 2007. They asked about CAUTI prevention practices and standardized infection ratios on CAUTI.
Michigan hospitals, compared with those elsewhere in the U.S., more frequently participated in collaboratives to reduce healthcare-associated infection—94% to 67%. They also used bladder scanners to measure bladder volume more frequently (53% to 39%), along with catheter reminders or stop orders and/or nurse-initiated discontinuation (44% to 23%).
CAUTI rates in the state of Michigan saw a 25% reduction, significantly greater than the 6% decrease observed in the rest of the U.S.
Sanjay Saint, MD, MPH, a hospitalist and professor of internal medicine at the University of Michigan, says the study verifies how important it is for hospitalists to remove urinary catheters early.
"The data will set us free," he says. "It’s probably better to remove a few of these catheters prematurely and then have to reinsert them than keep all catheters in long past their due date." TH
Tom Collins is a freelance author in South Florida.
Conscientious handling of urinary catheters is one of the main responsibilities hospitalists have in caring for patients with urological disorders—and, of course, anyone else with a urinary catheter.
Treatment of patients with urological disorders often involves special circumstances requiring physician discretion when deciding whether to remove a catheter or leave it in—removing it too soon could cause problems far worse than an infection. But two compelling studies, nationwide in scope, point to the benefits of systems that help ensure prompt removal of urinary catheters when appropriate.
One, published in 2010, was a review of interventional studies that used reminders to physicians or nurses that a urinary catheter was in use or stop orders to trigger catheter removal in hospitalized adults.
Researchers found that the rate of catheter-associated urinary tract infections, measured as episodes per 1,000 catheter-days, was reduced by 52% (P<0.001) with use of a reminder or stop order. The average duration of catheterization decreased by 37%. That amounted to 2.61 fewer days of catheterization per patient in the intervention compared to control groups.
In a 2013 study published in JAMA Internal Medicine, researchers surveyed infection prevention specialists at a sample of hospitals across the U.S.—and at all hospitals in Michigan, home to a statewide CAUTI-prevention initiative started in 2007. They asked about CAUTI prevention practices and standardized infection ratios on CAUTI.
Michigan hospitals, compared with those elsewhere in the U.S., more frequently participated in collaboratives to reduce healthcare-associated infection—94% to 67%. They also used bladder scanners to measure bladder volume more frequently (53% to 39%), along with catheter reminders or stop orders and/or nurse-initiated discontinuation (44% to 23%).
CAUTI rates in the state of Michigan saw a 25% reduction, significantly greater than the 6% decrease observed in the rest of the U.S.
Sanjay Saint, MD, MPH, a hospitalist and professor of internal medicine at the University of Michigan, says the study verifies how important it is for hospitalists to remove urinary catheters early.
"The data will set us free," he says. "It’s probably better to remove a few of these catheters prematurely and then have to reinsert them than keep all catheters in long past their due date." TH
Tom Collins is a freelance author in South Florida.
Conscientious handling of urinary catheters is one of the main responsibilities hospitalists have in caring for patients with urological disorders—and, of course, anyone else with a urinary catheter.
Treatment of patients with urological disorders often involves special circumstances requiring physician discretion when deciding whether to remove a catheter or leave it in—removing it too soon could cause problems far worse than an infection. But two compelling studies, nationwide in scope, point to the benefits of systems that help ensure prompt removal of urinary catheters when appropriate.
One, published in 2010, was a review of interventional studies that used reminders to physicians or nurses that a urinary catheter was in use or stop orders to trigger catheter removal in hospitalized adults.
Researchers found that the rate of catheter-associated urinary tract infections, measured as episodes per 1,000 catheter-days, was reduced by 52% (P<0.001) with use of a reminder or stop order. The average duration of catheterization decreased by 37%. That amounted to 2.61 fewer days of catheterization per patient in the intervention compared to control groups.
In a 2013 study published in JAMA Internal Medicine, researchers surveyed infection prevention specialists at a sample of hospitals across the U.S.—and at all hospitals in Michigan, home to a statewide CAUTI-prevention initiative started in 2007. They asked about CAUTI prevention practices and standardized infection ratios on CAUTI.
Michigan hospitals, compared with those elsewhere in the U.S., more frequently participated in collaboratives to reduce healthcare-associated infection—94% to 67%. They also used bladder scanners to measure bladder volume more frequently (53% to 39%), along with catheter reminders or stop orders and/or nurse-initiated discontinuation (44% to 23%).
CAUTI rates in the state of Michigan saw a 25% reduction, significantly greater than the 6% decrease observed in the rest of the U.S.
Sanjay Saint, MD, MPH, a hospitalist and professor of internal medicine at the University of Michigan, says the study verifies how important it is for hospitalists to remove urinary catheters early.
"The data will set us free," he says. "It’s probably better to remove a few of these catheters prematurely and then have to reinsert them than keep all catheters in long past their due date." TH
Tom Collins is a freelance author in South Florida.