User login
Defining incisional hernia risk in IBD surgery
Open surgery for inflammatory bowel disease (IBD) has been known to carry a high risk of incisional hernia, but the risk factors have not been well understood.
A review of 1,000 operations performed over nearly 40 years at a high-volume, nationally recognized center has identified five patient factors that can raise the risk of incisional hernia in these operations by 50% or more, according to a study published in the Annals of Surgery.
The study followed the patients for an average of 8 years after their operations, which were performed between January 1976 and December 2014 at Mount Sinai Medical Center in New York. The overall incidence of incisional hernia was 20%-21% for patients with ulcerative colitis and 20% for those with Crohn’s disease.
Half of these patients developed an incisional hernia less than 2 years after the index surgery and 75% in less than 4 years.
The researchers identified the following statistically significant risk factors for incisional hernia: wound infection (hazard ratio, 3.66; P less than .001); hypoalbuminemia (HR, 2.02; P = .002); previous bowel resection (HR, 1.6; P = .003); ileostomy created at time of procedure (HR, 1.53; P = .01); and a history of smoking (HR, 1.52; P less than .013). Other risk factors to lesser degrees are body mass index at time of surgery (HR, 1.036; P = .009); age at time of surgery (HR, 1.021; P less than .001), and age at disease onset (HR, 1.018; P less than .001).
Lead author Tomas Heimann, MD, and his coauthors pointed out that this study population had severe levels of disease. Almost half of the patients had severe intractable disease that had resisted medical treatment. More than a quarter of these patients had received preoperative steroid therapy within 6 weeks, and 15% had received recent immunosuppressive therapy. Almost 80% were either anemic or had hypoalbuminemia or both. The average duration of disease was 12 years. More than half had undergone previous bowel surgery – “often lengthy and difficult” – with many patients suffering from fistulae, abscesses, and dense adhesions. “These factors were more likely to predispose patients to develop wound infections and delayed healing resulting in incisional hernia in one-fifth of our patients,” Dr. Heimann and his coauthors noted.
A somewhat unexpected finding was that immunosuppressive therapy and steroids were not linked to incisional hernia in these patients.
Prophylactic mesh placement in patients with IBD is impractical because of the risk of infection it carries, Dr. Heimann and his coauthors said.
Dr. Heimann and his coauthors reported having no financial disclosures.
SOURCE: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
Open surgery for inflammatory bowel disease (IBD) has been known to carry a high risk of incisional hernia, but the risk factors have not been well understood.
A review of 1,000 operations performed over nearly 40 years at a high-volume, nationally recognized center has identified five patient factors that can raise the risk of incisional hernia in these operations by 50% or more, according to a study published in the Annals of Surgery.
The study followed the patients for an average of 8 years after their operations, which were performed between January 1976 and December 2014 at Mount Sinai Medical Center in New York. The overall incidence of incisional hernia was 20%-21% for patients with ulcerative colitis and 20% for those with Crohn’s disease.
Half of these patients developed an incisional hernia less than 2 years after the index surgery and 75% in less than 4 years.
The researchers identified the following statistically significant risk factors for incisional hernia: wound infection (hazard ratio, 3.66; P less than .001); hypoalbuminemia (HR, 2.02; P = .002); previous bowel resection (HR, 1.6; P = .003); ileostomy created at time of procedure (HR, 1.53; P = .01); and a history of smoking (HR, 1.52; P less than .013). Other risk factors to lesser degrees are body mass index at time of surgery (HR, 1.036; P = .009); age at time of surgery (HR, 1.021; P less than .001), and age at disease onset (HR, 1.018; P less than .001).
Lead author Tomas Heimann, MD, and his coauthors pointed out that this study population had severe levels of disease. Almost half of the patients had severe intractable disease that had resisted medical treatment. More than a quarter of these patients had received preoperative steroid therapy within 6 weeks, and 15% had received recent immunosuppressive therapy. Almost 80% were either anemic or had hypoalbuminemia or both. The average duration of disease was 12 years. More than half had undergone previous bowel surgery – “often lengthy and difficult” – with many patients suffering from fistulae, abscesses, and dense adhesions. “These factors were more likely to predispose patients to develop wound infections and delayed healing resulting in incisional hernia in one-fifth of our patients,” Dr. Heimann and his coauthors noted.
A somewhat unexpected finding was that immunosuppressive therapy and steroids were not linked to incisional hernia in these patients.
Prophylactic mesh placement in patients with IBD is impractical because of the risk of infection it carries, Dr. Heimann and his coauthors said.
Dr. Heimann and his coauthors reported having no financial disclosures.
SOURCE: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
Open surgery for inflammatory bowel disease (IBD) has been known to carry a high risk of incisional hernia, but the risk factors have not been well understood.
A review of 1,000 operations performed over nearly 40 years at a high-volume, nationally recognized center has identified five patient factors that can raise the risk of incisional hernia in these operations by 50% or more, according to a study published in the Annals of Surgery.
The study followed the patients for an average of 8 years after their operations, which were performed between January 1976 and December 2014 at Mount Sinai Medical Center in New York. The overall incidence of incisional hernia was 20%-21% for patients with ulcerative colitis and 20% for those with Crohn’s disease.
Half of these patients developed an incisional hernia less than 2 years after the index surgery and 75% in less than 4 years.
The researchers identified the following statistically significant risk factors for incisional hernia: wound infection (hazard ratio, 3.66; P less than .001); hypoalbuminemia (HR, 2.02; P = .002); previous bowel resection (HR, 1.6; P = .003); ileostomy created at time of procedure (HR, 1.53; P = .01); and a history of smoking (HR, 1.52; P less than .013). Other risk factors to lesser degrees are body mass index at time of surgery (HR, 1.036; P = .009); age at time of surgery (HR, 1.021; P less than .001), and age at disease onset (HR, 1.018; P less than .001).
Lead author Tomas Heimann, MD, and his coauthors pointed out that this study population had severe levels of disease. Almost half of the patients had severe intractable disease that had resisted medical treatment. More than a quarter of these patients had received preoperative steroid therapy within 6 weeks, and 15% had received recent immunosuppressive therapy. Almost 80% were either anemic or had hypoalbuminemia or both. The average duration of disease was 12 years. More than half had undergone previous bowel surgery – “often lengthy and difficult” – with many patients suffering from fistulae, abscesses, and dense adhesions. “These factors were more likely to predispose patients to develop wound infections and delayed healing resulting in incisional hernia in one-fifth of our patients,” Dr. Heimann and his coauthors noted.
A somewhat unexpected finding was that immunosuppressive therapy and steroids were not linked to incisional hernia in these patients.
Prophylactic mesh placement in patients with IBD is impractical because of the risk of infection it carries, Dr. Heimann and his coauthors said.
Dr. Heimann and his coauthors reported having no financial disclosures.
SOURCE: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
FROM ANNALS OF SURGERY
Key clinical point: Patients with IBD have a high incidence of incisional hernia after open bowel resection.
Major finding: The overall incidence of incisional hernia after open bowel resection was 20%.
Data source: One thousand patients who had undergone open bowel surgery for IBD at Mount Sinai Medical Center, New York, between January 1976 and December 2014.
Disclosures: Dr. Heimann and his coauthors reported having no financial disclosures.
Source: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
Parental leave not available to all academic surgeons
Paid parental leave policies have been unevenly adopted among academic medical centers, according to a study published in the Journal of Surgical Research. These policies, or their lack, may have important ramifications for recruiting and specialty selection by surgeons, and for women of child-rearing age in particular.
Parental leave for surgeons has been championed by the American College of Surgeons, among other professional societies, in formal statements and supportive policies in recent years.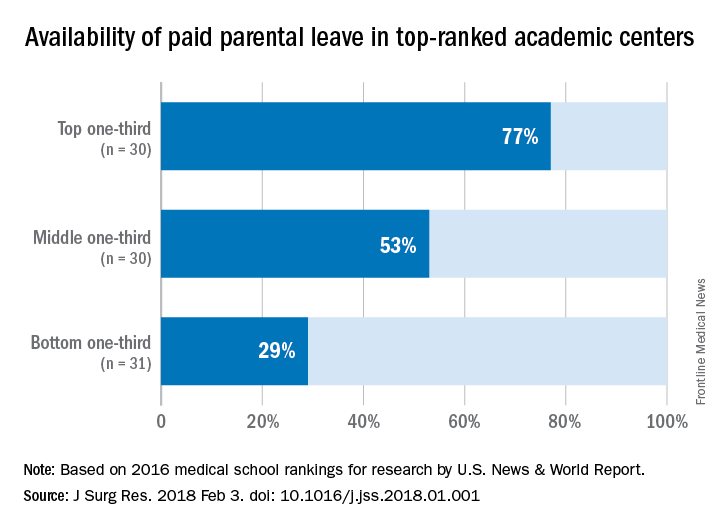
Dina S. Itum, MD, a fifth-year resident in the department of surgery, University of Texas Southwestern Medical Center, Houston, and a research team looked into how widespread parental leave is for surgeons in US medical centers. Their sample was the 91 top-ranked academic medical centers identified by U.S. News & World Report in 2016. The method used by U.S. News & World Report for ranking medical centers is based on student selectivity, dean and residency directors’ peer assessment of national institutions, faculty to student ratio, and the dollar amount in NIH research grants received.
“Parental leave” was defined by the research team as any leave dedicated to new mothers, fathers and/or primary caregivers after childbirth or adoption. “Paid leave” was defined as some protected leave with salary without mandated use of sick leave or vacation leave.
The study found that among the top-ranked 91 institutions, 48 (53%) offered some form of paid parental leave to faculty surgeons. The higher the rating, the more likely the institution offered paid parental leave: 77% of those in the top third of rankings vs. 53% in the middle third and 29% in the bottom third. Private institutions were more likely to offer paid leave of 6 weeks or longer; 67% vs. 33% of public institutions.
The investigators posed a question: Did these institutions implement the policy to attract the top talent, or did the policy improve faculty morale and productivity leading to a higher ranking? The study does not answer the question, but the investigators consider it an important issue for further study.
The investigators also suggested that surgeons of child-rearing age use parental leave information their in their own employment negotiations. “As physicians, we are aware of the health care benefits associated with parental leave, and as leaders within our communities, we should be at the forefront of supporting further advancement of this benefit,” the investigators wrote.
The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
Paid parental leave policies have been unevenly adopted among academic medical centers, according to a study published in the Journal of Surgical Research. These policies, or their lack, may have important ramifications for recruiting and specialty selection by surgeons, and for women of child-rearing age in particular.
Parental leave for surgeons has been championed by the American College of Surgeons, among other professional societies, in formal statements and supportive policies in recent years.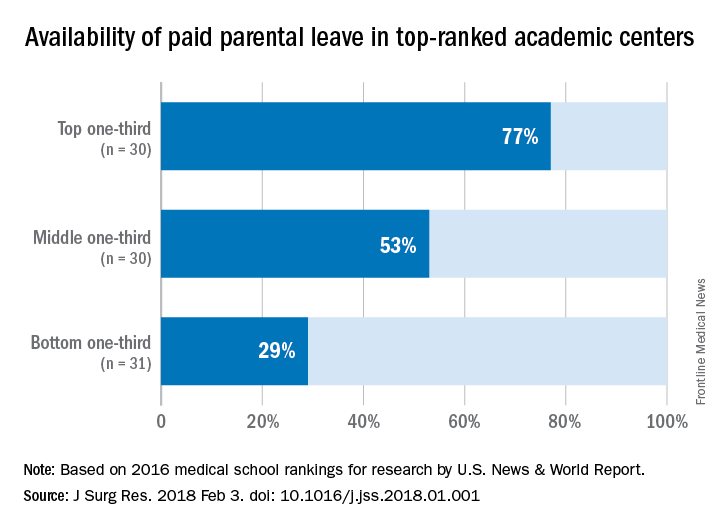
Dina S. Itum, MD, a fifth-year resident in the department of surgery, University of Texas Southwestern Medical Center, Houston, and a research team looked into how widespread parental leave is for surgeons in US medical centers. Their sample was the 91 top-ranked academic medical centers identified by U.S. News & World Report in 2016. The method used by U.S. News & World Report for ranking medical centers is based on student selectivity, dean and residency directors’ peer assessment of national institutions, faculty to student ratio, and the dollar amount in NIH research grants received.
“Parental leave” was defined by the research team as any leave dedicated to new mothers, fathers and/or primary caregivers after childbirth or adoption. “Paid leave” was defined as some protected leave with salary without mandated use of sick leave or vacation leave.
The study found that among the top-ranked 91 institutions, 48 (53%) offered some form of paid parental leave to faculty surgeons. The higher the rating, the more likely the institution offered paid parental leave: 77% of those in the top third of rankings vs. 53% in the middle third and 29% in the bottom third. Private institutions were more likely to offer paid leave of 6 weeks or longer; 67% vs. 33% of public institutions.
The investigators posed a question: Did these institutions implement the policy to attract the top talent, or did the policy improve faculty morale and productivity leading to a higher ranking? The study does not answer the question, but the investigators consider it an important issue for further study.
The investigators also suggested that surgeons of child-rearing age use parental leave information their in their own employment negotiations. “As physicians, we are aware of the health care benefits associated with parental leave, and as leaders within our communities, we should be at the forefront of supporting further advancement of this benefit,” the investigators wrote.
The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
Paid parental leave policies have been unevenly adopted among academic medical centers, according to a study published in the Journal of Surgical Research. These policies, or their lack, may have important ramifications for recruiting and specialty selection by surgeons, and for women of child-rearing age in particular.
Parental leave for surgeons has been championed by the American College of Surgeons, among other professional societies, in formal statements and supportive policies in recent years.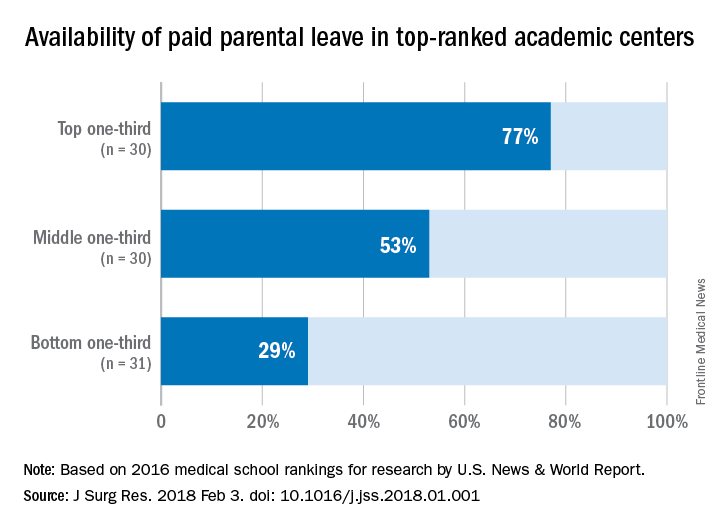
Dina S. Itum, MD, a fifth-year resident in the department of surgery, University of Texas Southwestern Medical Center, Houston, and a research team looked into how widespread parental leave is for surgeons in US medical centers. Their sample was the 91 top-ranked academic medical centers identified by U.S. News & World Report in 2016. The method used by U.S. News & World Report for ranking medical centers is based on student selectivity, dean and residency directors’ peer assessment of national institutions, faculty to student ratio, and the dollar amount in NIH research grants received.
“Parental leave” was defined by the research team as any leave dedicated to new mothers, fathers and/or primary caregivers after childbirth or adoption. “Paid leave” was defined as some protected leave with salary without mandated use of sick leave or vacation leave.
The study found that among the top-ranked 91 institutions, 48 (53%) offered some form of paid parental leave to faculty surgeons. The higher the rating, the more likely the institution offered paid parental leave: 77% of those in the top third of rankings vs. 53% in the middle third and 29% in the bottom third. Private institutions were more likely to offer paid leave of 6 weeks or longer; 67% vs. 33% of public institutions.
The investigators posed a question: Did these institutions implement the policy to attract the top talent, or did the policy improve faculty morale and productivity leading to a higher ranking? The study does not answer the question, but the investigators consider it an important issue for further study.
The investigators also suggested that surgeons of child-rearing age use parental leave information their in their own employment negotiations. “As physicians, we are aware of the health care benefits associated with parental leave, and as leaders within our communities, we should be at the forefront of supporting further advancement of this benefit,” the investigators wrote.
The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: Parental leave policies have been unevenly adopted by U.S. medical schools.
Major finding: Among the top 91 ranked medical schools, 53% offer paid parental leave.
Data source: Survey of 91 top academic medical centers identified in U.S. News & World Report 2016 listing.
Disclosures: The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
How real is resident burnout?
JACKSONVILLE, FLA. – Burnout is commonly ascribed to surgical residents, but reliable estimates of the numbers involved and a clear, comparable definition of burnout remain elusive.
A large study of general surgery residents has found that almost one in four have at least one symptom of burnout daily and more than two in five report poor psychiatric well-being, according to results of a survey reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Twenty-two percent of general surgery residents report at least one symptom of burnout daily,” said Daniel “Brock” Hewitt, MD, a research fellow in the Surgical Outcomes and Quality Improvement Center in the department of surgery, Feinberg School of Medicine, Northwestern University, Chicago. “Poor resident wellness is associated with more duty-hour violations, feeling unprepared for residency, and an increase in self-reported medical errors. However, burnout is not associated with worse surgical outcomes.”
The study, undertaken with grant support from The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality, provided three significant insights into resident wellness, Dr. Hewitt said. “When measuring the level of burnout, careful consideration should be given to how burnout is defined,” he said. “Secondly, wellness interventions with attention to preparedness for residency and duty-hour restrictions may help alleviate burnout. And finally, with the significant impact it does have on the individual physician, we believe that burnout needs to be addressed regardless of its impact on patient outcomes.”
The study drew on a questionnaire given to residents immediately following the 2017 American Board of Surgery In-Training Examination (ABSITE), which 3,789 general surgery residents from 115 general surgery programs completed. The survey had a 99.3% response rate. The survey evaluated two factors associated with resident wellness: burnout and poor psychiatric well-being. “Poor wellness is prevalent among physicians and trainees and is associated with depression, suicidal ideation, attrition, and absenteeism,” Dr. Hewitt said.
But to measure burnout, the researchers had to first define it. The instrument Dr. Hewitt and coauthors used is the Maslach Burnout Inventory, named for University of California at Berkley psychology professor Christina Maslach, PhD. It quantifies three different factors for burnout: emotional exhaustion; depersonalization or cynicism; and a low sense of personal accomplishment. This study defined “burnout” as having feelings of both emotional exhaustion and depersonalization, and dismissed the third measure of burnout because physicians rarely posses a low sense of personal accomplishment.
Overall, 22.3% reported one sign or symptom of burnout daily, and 56.5% did so on a weekly basis, Dr. Hewitt said.
However, Dr. Hewitt noted, burnout measurement thresholds can vary “because burnout itself is not an actual diagnosis.” Studies have calculated the burnout rate among surgeons at 28% to 69% (J Am Coll Surg. 2016:222:1230-9). A recent systematic review found up to eight different cutoffs used to define “high burnout” (Cogent Med. 2016 7 Oct; doi.org/10.1080/2331205X.2016.1237605; J Am Coll Surg, 2016:223:440-51)
How studies of physician burnout establish cutoffs and which Maslach Burnout Inventory subscales they measure has an impact on the rates of burnout they report, Dr. Hewitt said. For this study, the researchers used the Maslach scores in the top quartile in both emotional exhaustion and depersonalization to define burnout. “Burnout is probably best defined as a continuum from engagement on the one end and burnout on the other, so there’s some combination of the [Maslach] subscales that lead to burnout,” he said.
Among survey respondents, 19.5% reported high Maslach scores for emotional exhaustion and 9% of depersonalization on a daily basis (6.2% reported both)--22.3% reported at least one daily. On a weekly basis, 54.2% reported high scores for emotional exhaustion and 25.6% high scores for depersonalization, with 56.5% reporting at least one and 22.4% reporting both.
To evaluate residents’ sense of psychiatric well-being, the study used the General Health Questionnaire (Psychol Med. 1998;28:915-21). Among survey respondents, 43% met criteria for poor psychiatric well-being.
Burnout rates among men and women were identical, but a significantly higher percentage of women had poor psychiatric well-being: 48.4% to 39.7% of men.
Burnout and psychiatric well-being scores also varied depending on post-graduate year. Second- and third-year residents were significantly more likely to report burnout, compared to first-year residents, Dr. Hewitt said. Rates of poor psychiatric well-being were lowest for fourth- and fifth-year residents.
Most pronounced was the impact of 80-hour duty week violations had on residents’ sense of burnout and poor psychiatric well-being. Burnout rates were 8.4% for those who reported no monthly duty-hour violations, but doubled and quadrupled with more frequent monthly duty-hour violations: 16.1% for those who reported one to four violations a month; and 35% for those who reported five or more. Dr. Hewitt also noted wellness rates for those in the standard and flexible policy groups in Flexibility In duty hour Requirements for Surgical Trainees Trial (FIRST Trial) programs were similar.
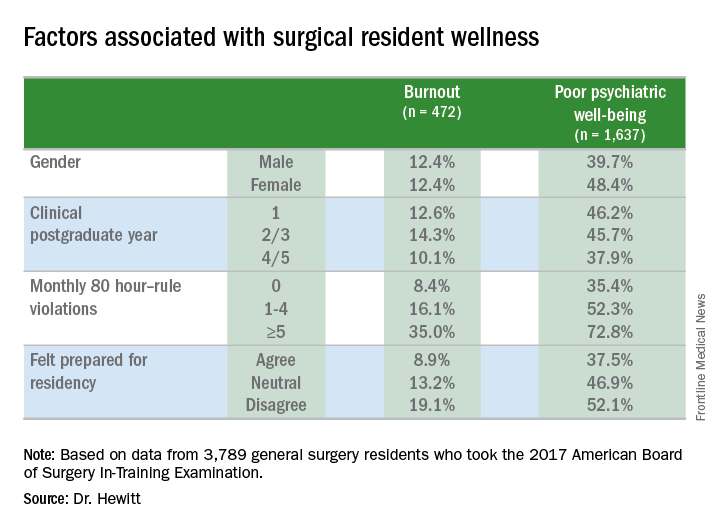
Another factor that contributed to burnout and poor psychiatric well-being was a sense of unpreparedness for residency, Dr. Hewitt said. Burnout rates for those who felt prepared were 8.9% vs. 19.1% for those who didn’t feel prepared. The disparity was less drastic, but nonetheless significant, for poor psychiatric well-being: 37.5% for those who felt prepared and 52.1% for those who didn’t.
With regard to outcomes, Dr. Hewitt said, “Residents in the highest quartile of burnout and the highest quartile of poor psychiatric well-being were significantly more likely to report a near miss or harmful medical error.” Among the burnout group, highest quartile rates were 39.3% for a near miss and 14.4% for a harmful medical error vs. 11.1% and 2.4%, respectively, for the lowest quartile. Among surgical residents who reported poor psychiatric well-being, highest quartile rates were 31.9% for a near miss and 13.2% for a harmful medical error vs. 12.5% and 2.1%, respectively, for those in the lowest quartile.
The study also analyzed outcomes for 134,877 surgical patients and found no association of overall morbidity and death or serious morbidity with resident wellness. “However,” Dr. Hewitt said, “when we look at mortality and failure to rescue, we can see an association with burnout, specifically in programs that have high levels of burnout; these patients have significantly lower odds of mortality and failure to rescue.” Each has an adjusted odds ratios of 0.81.
Among the study limitations Dr. Hewitt noted were its cross-sectional nature that led to inferences of association, not identification of causation; residents completing the survey after the ABSITE may have influenced their answers; and the fact it did not account for certain intermediate factors such as physician or nursing burnout or institutional quality measures.
The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
SOURCE: Hewitt B et al. abstract 21.01
JACKSONVILLE, FLA. – Burnout is commonly ascribed to surgical residents, but reliable estimates of the numbers involved and a clear, comparable definition of burnout remain elusive.
A large study of general surgery residents has found that almost one in four have at least one symptom of burnout daily and more than two in five report poor psychiatric well-being, according to results of a survey reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Twenty-two percent of general surgery residents report at least one symptom of burnout daily,” said Daniel “Brock” Hewitt, MD, a research fellow in the Surgical Outcomes and Quality Improvement Center in the department of surgery, Feinberg School of Medicine, Northwestern University, Chicago. “Poor resident wellness is associated with more duty-hour violations, feeling unprepared for residency, and an increase in self-reported medical errors. However, burnout is not associated with worse surgical outcomes.”
The study, undertaken with grant support from The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality, provided three significant insights into resident wellness, Dr. Hewitt said. “When measuring the level of burnout, careful consideration should be given to how burnout is defined,” he said. “Secondly, wellness interventions with attention to preparedness for residency and duty-hour restrictions may help alleviate burnout. And finally, with the significant impact it does have on the individual physician, we believe that burnout needs to be addressed regardless of its impact on patient outcomes.”
The study drew on a questionnaire given to residents immediately following the 2017 American Board of Surgery In-Training Examination (ABSITE), which 3,789 general surgery residents from 115 general surgery programs completed. The survey had a 99.3% response rate. The survey evaluated two factors associated with resident wellness: burnout and poor psychiatric well-being. “Poor wellness is prevalent among physicians and trainees and is associated with depression, suicidal ideation, attrition, and absenteeism,” Dr. Hewitt said.
But to measure burnout, the researchers had to first define it. The instrument Dr. Hewitt and coauthors used is the Maslach Burnout Inventory, named for University of California at Berkley psychology professor Christina Maslach, PhD. It quantifies three different factors for burnout: emotional exhaustion; depersonalization or cynicism; and a low sense of personal accomplishment. This study defined “burnout” as having feelings of both emotional exhaustion and depersonalization, and dismissed the third measure of burnout because physicians rarely posses a low sense of personal accomplishment.
Overall, 22.3% reported one sign or symptom of burnout daily, and 56.5% did so on a weekly basis, Dr. Hewitt said.
However, Dr. Hewitt noted, burnout measurement thresholds can vary “because burnout itself is not an actual diagnosis.” Studies have calculated the burnout rate among surgeons at 28% to 69% (J Am Coll Surg. 2016:222:1230-9). A recent systematic review found up to eight different cutoffs used to define “high burnout” (Cogent Med. 2016 7 Oct; doi.org/10.1080/2331205X.2016.1237605; J Am Coll Surg, 2016:223:440-51)
How studies of physician burnout establish cutoffs and which Maslach Burnout Inventory subscales they measure has an impact on the rates of burnout they report, Dr. Hewitt said. For this study, the researchers used the Maslach scores in the top quartile in both emotional exhaustion and depersonalization to define burnout. “Burnout is probably best defined as a continuum from engagement on the one end and burnout on the other, so there’s some combination of the [Maslach] subscales that lead to burnout,” he said.
Among survey respondents, 19.5% reported high Maslach scores for emotional exhaustion and 9% of depersonalization on a daily basis (6.2% reported both)--22.3% reported at least one daily. On a weekly basis, 54.2% reported high scores for emotional exhaustion and 25.6% high scores for depersonalization, with 56.5% reporting at least one and 22.4% reporting both.
To evaluate residents’ sense of psychiatric well-being, the study used the General Health Questionnaire (Psychol Med. 1998;28:915-21). Among survey respondents, 43% met criteria for poor psychiatric well-being.
Burnout rates among men and women were identical, but a significantly higher percentage of women had poor psychiatric well-being: 48.4% to 39.7% of men.
Burnout and psychiatric well-being scores also varied depending on post-graduate year. Second- and third-year residents were significantly more likely to report burnout, compared to first-year residents, Dr. Hewitt said. Rates of poor psychiatric well-being were lowest for fourth- and fifth-year residents.
Most pronounced was the impact of 80-hour duty week violations had on residents’ sense of burnout and poor psychiatric well-being. Burnout rates were 8.4% for those who reported no monthly duty-hour violations, but doubled and quadrupled with more frequent monthly duty-hour violations: 16.1% for those who reported one to four violations a month; and 35% for those who reported five or more. Dr. Hewitt also noted wellness rates for those in the standard and flexible policy groups in Flexibility In duty hour Requirements for Surgical Trainees Trial (FIRST Trial) programs were similar.
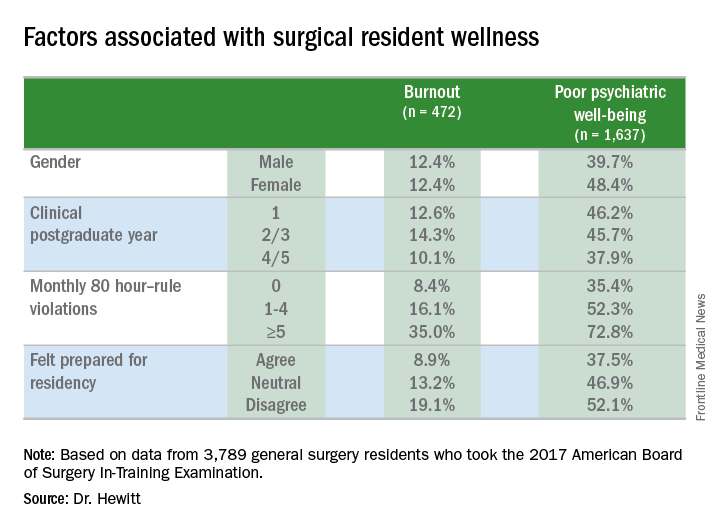
Another factor that contributed to burnout and poor psychiatric well-being was a sense of unpreparedness for residency, Dr. Hewitt said. Burnout rates for those who felt prepared were 8.9% vs. 19.1% for those who didn’t feel prepared. The disparity was less drastic, but nonetheless significant, for poor psychiatric well-being: 37.5% for those who felt prepared and 52.1% for those who didn’t.
With regard to outcomes, Dr. Hewitt said, “Residents in the highest quartile of burnout and the highest quartile of poor psychiatric well-being were significantly more likely to report a near miss or harmful medical error.” Among the burnout group, highest quartile rates were 39.3% for a near miss and 14.4% for a harmful medical error vs. 11.1% and 2.4%, respectively, for the lowest quartile. Among surgical residents who reported poor psychiatric well-being, highest quartile rates were 31.9% for a near miss and 13.2% for a harmful medical error vs. 12.5% and 2.1%, respectively, for those in the lowest quartile.
The study also analyzed outcomes for 134,877 surgical patients and found no association of overall morbidity and death or serious morbidity with resident wellness. “However,” Dr. Hewitt said, “when we look at mortality and failure to rescue, we can see an association with burnout, specifically in programs that have high levels of burnout; these patients have significantly lower odds of mortality and failure to rescue.” Each has an adjusted odds ratios of 0.81.
Among the study limitations Dr. Hewitt noted were its cross-sectional nature that led to inferences of association, not identification of causation; residents completing the survey after the ABSITE may have influenced their answers; and the fact it did not account for certain intermediate factors such as physician or nursing burnout or institutional quality measures.
The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
SOURCE: Hewitt B et al. abstract 21.01
JACKSONVILLE, FLA. – Burnout is commonly ascribed to surgical residents, but reliable estimates of the numbers involved and a clear, comparable definition of burnout remain elusive.
A large study of general surgery residents has found that almost one in four have at least one symptom of burnout daily and more than two in five report poor psychiatric well-being, according to results of a survey reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Twenty-two percent of general surgery residents report at least one symptom of burnout daily,” said Daniel “Brock” Hewitt, MD, a research fellow in the Surgical Outcomes and Quality Improvement Center in the department of surgery, Feinberg School of Medicine, Northwestern University, Chicago. “Poor resident wellness is associated with more duty-hour violations, feeling unprepared for residency, and an increase in self-reported medical errors. However, burnout is not associated with worse surgical outcomes.”
The study, undertaken with grant support from The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality, provided three significant insights into resident wellness, Dr. Hewitt said. “When measuring the level of burnout, careful consideration should be given to how burnout is defined,” he said. “Secondly, wellness interventions with attention to preparedness for residency and duty-hour restrictions may help alleviate burnout. And finally, with the significant impact it does have on the individual physician, we believe that burnout needs to be addressed regardless of its impact on patient outcomes.”
The study drew on a questionnaire given to residents immediately following the 2017 American Board of Surgery In-Training Examination (ABSITE), which 3,789 general surgery residents from 115 general surgery programs completed. The survey had a 99.3% response rate. The survey evaluated two factors associated with resident wellness: burnout and poor psychiatric well-being. “Poor wellness is prevalent among physicians and trainees and is associated with depression, suicidal ideation, attrition, and absenteeism,” Dr. Hewitt said.
But to measure burnout, the researchers had to first define it. The instrument Dr. Hewitt and coauthors used is the Maslach Burnout Inventory, named for University of California at Berkley psychology professor Christina Maslach, PhD. It quantifies three different factors for burnout: emotional exhaustion; depersonalization or cynicism; and a low sense of personal accomplishment. This study defined “burnout” as having feelings of both emotional exhaustion and depersonalization, and dismissed the third measure of burnout because physicians rarely posses a low sense of personal accomplishment.
Overall, 22.3% reported one sign or symptom of burnout daily, and 56.5% did so on a weekly basis, Dr. Hewitt said.
However, Dr. Hewitt noted, burnout measurement thresholds can vary “because burnout itself is not an actual diagnosis.” Studies have calculated the burnout rate among surgeons at 28% to 69% (J Am Coll Surg. 2016:222:1230-9). A recent systematic review found up to eight different cutoffs used to define “high burnout” (Cogent Med. 2016 7 Oct; doi.org/10.1080/2331205X.2016.1237605; J Am Coll Surg, 2016:223:440-51)
How studies of physician burnout establish cutoffs and which Maslach Burnout Inventory subscales they measure has an impact on the rates of burnout they report, Dr. Hewitt said. For this study, the researchers used the Maslach scores in the top quartile in both emotional exhaustion and depersonalization to define burnout. “Burnout is probably best defined as a continuum from engagement on the one end and burnout on the other, so there’s some combination of the [Maslach] subscales that lead to burnout,” he said.
Among survey respondents, 19.5% reported high Maslach scores for emotional exhaustion and 9% of depersonalization on a daily basis (6.2% reported both)--22.3% reported at least one daily. On a weekly basis, 54.2% reported high scores for emotional exhaustion and 25.6% high scores for depersonalization, with 56.5% reporting at least one and 22.4% reporting both.
To evaluate residents’ sense of psychiatric well-being, the study used the General Health Questionnaire (Psychol Med. 1998;28:915-21). Among survey respondents, 43% met criteria for poor psychiatric well-being.
Burnout rates among men and women were identical, but a significantly higher percentage of women had poor psychiatric well-being: 48.4% to 39.7% of men.
Burnout and psychiatric well-being scores also varied depending on post-graduate year. Second- and third-year residents were significantly more likely to report burnout, compared to first-year residents, Dr. Hewitt said. Rates of poor psychiatric well-being were lowest for fourth- and fifth-year residents.
Most pronounced was the impact of 80-hour duty week violations had on residents’ sense of burnout and poor psychiatric well-being. Burnout rates were 8.4% for those who reported no monthly duty-hour violations, but doubled and quadrupled with more frequent monthly duty-hour violations: 16.1% for those who reported one to four violations a month; and 35% for those who reported five or more. Dr. Hewitt also noted wellness rates for those in the standard and flexible policy groups in Flexibility In duty hour Requirements for Surgical Trainees Trial (FIRST Trial) programs were similar.
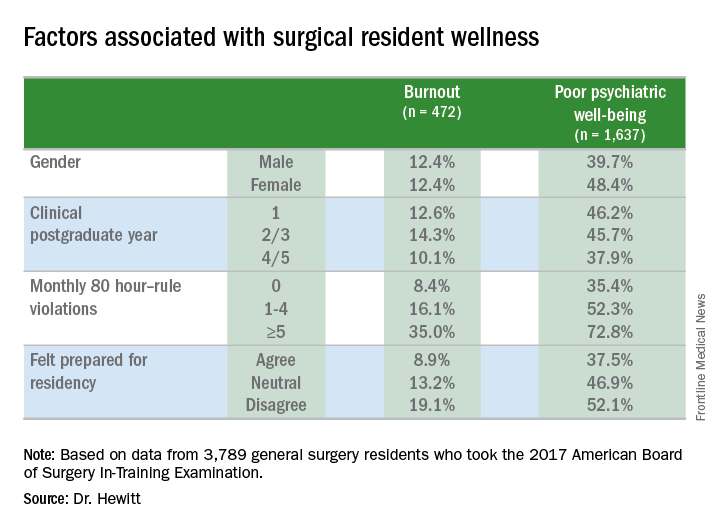
Another factor that contributed to burnout and poor psychiatric well-being was a sense of unpreparedness for residency, Dr. Hewitt said. Burnout rates for those who felt prepared were 8.9% vs. 19.1% for those who didn’t feel prepared. The disparity was less drastic, but nonetheless significant, for poor psychiatric well-being: 37.5% for those who felt prepared and 52.1% for those who didn’t.
With regard to outcomes, Dr. Hewitt said, “Residents in the highest quartile of burnout and the highest quartile of poor psychiatric well-being were significantly more likely to report a near miss or harmful medical error.” Among the burnout group, highest quartile rates were 39.3% for a near miss and 14.4% for a harmful medical error vs. 11.1% and 2.4%, respectively, for the lowest quartile. Among surgical residents who reported poor psychiatric well-being, highest quartile rates were 31.9% for a near miss and 13.2% for a harmful medical error vs. 12.5% and 2.1%, respectively, for those in the lowest quartile.
The study also analyzed outcomes for 134,877 surgical patients and found no association of overall morbidity and death or serious morbidity with resident wellness. “However,” Dr. Hewitt said, “when we look at mortality and failure to rescue, we can see an association with burnout, specifically in programs that have high levels of burnout; these patients have significantly lower odds of mortality and failure to rescue.” Each has an adjusted odds ratios of 0.81.
Among the study limitations Dr. Hewitt noted were its cross-sectional nature that led to inferences of association, not identification of causation; residents completing the survey after the ABSITE may have influenced their answers; and the fact it did not account for certain intermediate factors such as physician or nursing burnout or institutional quality measures.
The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
SOURCE: Hewitt B et al. abstract 21.01
AT THE ANNUAL ACADEMIC SURGICAL CONGRESS
Key clinical point: Almost one in four surgical residents manifest a daily symptom of burnout.
Major finding: Overall 22.8% of daily and 44.3% had poor psychiatric well-being scores.
Study details: Surveys completed by 3,789 general surgery residents during the American Board of Surgery In-Training Examination in January 2017.
Disclosures: The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
Source: Hewitt B et al. abstract 21.01
Study pinpoints link between ERAS and acute kidney injury
JACKSONVILLE, FLA. – Surgeons at the University of Alabama at Birmingham embraced the enhanced recovery pathway for elective colorectal surgery, but after they initiated the program, they noted high rates of postoperative acute kidney injury. They set about tweaking their approach to bring their results into line with national averages, according to a report presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Their response is an example of how surgery departments can use American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) data to monitor and improve their outcomes.
The rate of acute kidney injury (AKI) before ERAS was 7.1% ,compared with 13.6% after ERAS (P less than .01). After researchers adjusted for significant covariates, “ERAS patients were 2.3 times more likely to develop postoperative acute kidney injury,” Mr. Wiener said (P less than .01). That led the researchers to conclude that the ERAS protocol was independently associated with AKI following colorectal surgery. Average hospital stays for the ERAS group were less than half of those for the non-ERAS group, Wiener said: 3 days for the former vs. 7 days for the latter (P less than .01).
He noted that when UAB implemented ERAS for colorectal surgery, it also adopted the PDSA – Plan, Do, Study, Act – a cyclical quality improvement tool. “So we had done the study,” he said. “How do we act?”
Further investigation revealed the surgeons were using a stacked dosing of ketorolac with one dose at the end of the case and the next dose with initiation of the postoperative order set. “We eliminated the last intraoperative ketorolac dose to avoid the stacked dosing,” Wiener said. “Furthermore, we educated our residents to use ERAS as a guideline, but to always remember to treat the patient individually first.”
After that change, the subsequent semiannual ACS NSQIP report showed that UAB’s outcomes had improved. “We were able to go from the 10th decile for kidney failure after colorectal surgery to the first decile,” Wiener said.
“Moving forward, we will continue to monitor protocol outcomes in our ERAS patients and customize a pathway based on individual preoperative risk,” he said. That includes identifying optimal perioperative IV fluid management and refining multimodal pain management.
Mr. Wiener and coauthors had no financial relationships to disclose.
SOURCE: Wiener JG et al. Abstract 76.03
JACKSONVILLE, FLA. – Surgeons at the University of Alabama at Birmingham embraced the enhanced recovery pathway for elective colorectal surgery, but after they initiated the program, they noted high rates of postoperative acute kidney injury. They set about tweaking their approach to bring their results into line with national averages, according to a report presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Their response is an example of how surgery departments can use American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) data to monitor and improve their outcomes.
The rate of acute kidney injury (AKI) before ERAS was 7.1% ,compared with 13.6% after ERAS (P less than .01). After researchers adjusted for significant covariates, “ERAS patients were 2.3 times more likely to develop postoperative acute kidney injury,” Mr. Wiener said (P less than .01). That led the researchers to conclude that the ERAS protocol was independently associated with AKI following colorectal surgery. Average hospital stays for the ERAS group were less than half of those for the non-ERAS group, Wiener said: 3 days for the former vs. 7 days for the latter (P less than .01).
He noted that when UAB implemented ERAS for colorectal surgery, it also adopted the PDSA – Plan, Do, Study, Act – a cyclical quality improvement tool. “So we had done the study,” he said. “How do we act?”
Further investigation revealed the surgeons were using a stacked dosing of ketorolac with one dose at the end of the case and the next dose with initiation of the postoperative order set. “We eliminated the last intraoperative ketorolac dose to avoid the stacked dosing,” Wiener said. “Furthermore, we educated our residents to use ERAS as a guideline, but to always remember to treat the patient individually first.”
After that change, the subsequent semiannual ACS NSQIP report showed that UAB’s outcomes had improved. “We were able to go from the 10th decile for kidney failure after colorectal surgery to the first decile,” Wiener said.
“Moving forward, we will continue to monitor protocol outcomes in our ERAS patients and customize a pathway based on individual preoperative risk,” he said. That includes identifying optimal perioperative IV fluid management and refining multimodal pain management.
Mr. Wiener and coauthors had no financial relationships to disclose.
SOURCE: Wiener JG et al. Abstract 76.03
JACKSONVILLE, FLA. – Surgeons at the University of Alabama at Birmingham embraced the enhanced recovery pathway for elective colorectal surgery, but after they initiated the program, they noted high rates of postoperative acute kidney injury. They set about tweaking their approach to bring their results into line with national averages, according to a report presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Their response is an example of how surgery departments can use American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) data to monitor and improve their outcomes.
The rate of acute kidney injury (AKI) before ERAS was 7.1% ,compared with 13.6% after ERAS (P less than .01). After researchers adjusted for significant covariates, “ERAS patients were 2.3 times more likely to develop postoperative acute kidney injury,” Mr. Wiener said (P less than .01). That led the researchers to conclude that the ERAS protocol was independently associated with AKI following colorectal surgery. Average hospital stays for the ERAS group were less than half of those for the non-ERAS group, Wiener said: 3 days for the former vs. 7 days for the latter (P less than .01).
He noted that when UAB implemented ERAS for colorectal surgery, it also adopted the PDSA – Plan, Do, Study, Act – a cyclical quality improvement tool. “So we had done the study,” he said. “How do we act?”
Further investigation revealed the surgeons were using a stacked dosing of ketorolac with one dose at the end of the case and the next dose with initiation of the postoperative order set. “We eliminated the last intraoperative ketorolac dose to avoid the stacked dosing,” Wiener said. “Furthermore, we educated our residents to use ERAS as a guideline, but to always remember to treat the patient individually first.”
After that change, the subsequent semiannual ACS NSQIP report showed that UAB’s outcomes had improved. “We were able to go from the 10th decile for kidney failure after colorectal surgery to the first decile,” Wiener said.
“Moving forward, we will continue to monitor protocol outcomes in our ERAS patients and customize a pathway based on individual preoperative risk,” he said. That includes identifying optimal perioperative IV fluid management and refining multimodal pain management.
Mr. Wiener and coauthors had no financial relationships to disclose.
SOURCE: Wiener JG et al. Abstract 76.03
REPORTING FROM THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Implementation of the ERAS protocol for colorectal surgery was independently associated with acute kidney injury.
Major finding: After elective colorectal surgery, 13.6% of those in the ERAS protocol had acute kidney failure vs. 7.1 % of those who had surgery preprotocol (P less than .01).
Study details: Single-institution retrospective study of a prospectively maintained database containing 480 patients in the pre-ERAS group and 572 in the ERAS group.
Disclosures: The investigators reported having no financial disclosures.
Source: Wiener JG et al. Abstract 76.03.
Morbid, super obesity raises laparoscopic VHR risk
JACKSONVILLE, FLA. – Super-obese patients who have laparoscopic repair for ventral hernias have complications at a rate more than twice that for overweight individuals undergoing the same operation, according to an analysis of 10-year data presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Patients with a body mass index of 40 kg/m2 or greater were found to be significantly more likely to have a complication following laparoscopic ventral hernia repair,” said Robert A. Swendiman, MD, of the University of Pennsylvania, Philadelphia.
Dr. Swendiman and his colleagues analyzed outcomes of 57,957 patients in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database who had laparoscopic ventral hernia repair (VHR) from 2005 to 2015. The dataset was stratified into seven different BMI classes, and by hernia type (reducible or strangulated) and time of repair (initial or recurrent).
The overall complication rate for the study population was 4%, ranging from 3% in overweight patients (BMI of 25-29.99 kg/m2) to 6.9% for the super obese (BMI of 50 kg/m2 or greater); 61.4% of the study population was obese. “Initial repair and reducible hernias had lower complication rates than recurrent and incarcerated/strangulated hernias,” Dr. Swendiman said. The study considered 1 of 19 different complications within 30 days of the operation.
Three weight groups had the highest odds ratios (OR) for complications: underweight patients (less than 18.5 kg/m2, OR 1.46, P = .283); morbidly obese (40-50 kg/m2, OR 1.28, P = .014); and super obese (greater than or equal to 50 kg/m2, OR 1.76, P = less than .0001). However, Dr. Swendiman noted, “Overweight patients had a lower rate of overall complications compared to normal-weight individuals.”
These findings were consistent with a prior analysis the group did that found patients with BMI greater than 30 kg/m2 was associated with increased risk of complications after open VHR, Dr. Swendiman noted (Surgery. 2017;162[6]:1320-9).
“Future studies should be considered to evaluate the role of weight reduction prior to hernia repair as a method to reduce patient risk,” Dr. Swendiman said. Laparoscopic repair may be preferable to open VHR in obese patients, depending on the clinical context, he said.
Dr. Swendiman and coauthors reported having no financial disclosures.
SOURCE: Academic Surgical Congress. Abstract 50.02.
JACKSONVILLE, FLA. – Super-obese patients who have laparoscopic repair for ventral hernias have complications at a rate more than twice that for overweight individuals undergoing the same operation, according to an analysis of 10-year data presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Patients with a body mass index of 40 kg/m2 or greater were found to be significantly more likely to have a complication following laparoscopic ventral hernia repair,” said Robert A. Swendiman, MD, of the University of Pennsylvania, Philadelphia.
Dr. Swendiman and his colleagues analyzed outcomes of 57,957 patients in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database who had laparoscopic ventral hernia repair (VHR) from 2005 to 2015. The dataset was stratified into seven different BMI classes, and by hernia type (reducible or strangulated) and time of repair (initial or recurrent).
The overall complication rate for the study population was 4%, ranging from 3% in overweight patients (BMI of 25-29.99 kg/m2) to 6.9% for the super obese (BMI of 50 kg/m2 or greater); 61.4% of the study population was obese. “Initial repair and reducible hernias had lower complication rates than recurrent and incarcerated/strangulated hernias,” Dr. Swendiman said. The study considered 1 of 19 different complications within 30 days of the operation.
Three weight groups had the highest odds ratios (OR) for complications: underweight patients (less than 18.5 kg/m2, OR 1.46, P = .283); morbidly obese (40-50 kg/m2, OR 1.28, P = .014); and super obese (greater than or equal to 50 kg/m2, OR 1.76, P = less than .0001). However, Dr. Swendiman noted, “Overweight patients had a lower rate of overall complications compared to normal-weight individuals.”
These findings were consistent with a prior analysis the group did that found patients with BMI greater than 30 kg/m2 was associated with increased risk of complications after open VHR, Dr. Swendiman noted (Surgery. 2017;162[6]:1320-9).
“Future studies should be considered to evaluate the role of weight reduction prior to hernia repair as a method to reduce patient risk,” Dr. Swendiman said. Laparoscopic repair may be preferable to open VHR in obese patients, depending on the clinical context, he said.
Dr. Swendiman and coauthors reported having no financial disclosures.
SOURCE: Academic Surgical Congress. Abstract 50.02.
JACKSONVILLE, FLA. – Super-obese patients who have laparoscopic repair for ventral hernias have complications at a rate more than twice that for overweight individuals undergoing the same operation, according to an analysis of 10-year data presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Patients with a body mass index of 40 kg/m2 or greater were found to be significantly more likely to have a complication following laparoscopic ventral hernia repair,” said Robert A. Swendiman, MD, of the University of Pennsylvania, Philadelphia.
Dr. Swendiman and his colleagues analyzed outcomes of 57,957 patients in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database who had laparoscopic ventral hernia repair (VHR) from 2005 to 2015. The dataset was stratified into seven different BMI classes, and by hernia type (reducible or strangulated) and time of repair (initial or recurrent).
The overall complication rate for the study population was 4%, ranging from 3% in overweight patients (BMI of 25-29.99 kg/m2) to 6.9% for the super obese (BMI of 50 kg/m2 or greater); 61.4% of the study population was obese. “Initial repair and reducible hernias had lower complication rates than recurrent and incarcerated/strangulated hernias,” Dr. Swendiman said. The study considered 1 of 19 different complications within 30 days of the operation.
Three weight groups had the highest odds ratios (OR) for complications: underweight patients (less than 18.5 kg/m2, OR 1.46, P = .283); morbidly obese (40-50 kg/m2, OR 1.28, P = .014); and super obese (greater than or equal to 50 kg/m2, OR 1.76, P = less than .0001). However, Dr. Swendiman noted, “Overweight patients had a lower rate of overall complications compared to normal-weight individuals.”
These findings were consistent with a prior analysis the group did that found patients with BMI greater than 30 kg/m2 was associated with increased risk of complications after open VHR, Dr. Swendiman noted (Surgery. 2017;162[6]:1320-9).
“Future studies should be considered to evaluate the role of weight reduction prior to hernia repair as a method to reduce patient risk,” Dr. Swendiman said. Laparoscopic repair may be preferable to open VHR in obese patients, depending on the clinical context, he said.
Dr. Swendiman and coauthors reported having no financial disclosures.
SOURCE: Academic Surgical Congress. Abstract 50.02.
REPORTING FROM THE ANNUAL ACADEMIC SURGICAL CONGRESS
Key clinical point: Laparoscopic ventral hernia repair is associated with a significantly increased risk of complications in the morbidly and super obese.
Major finding: Individuals with a body mass index in the overweight range (BMI 25 to 29.99 kg/m2) had a complication rate of 3% vs. 6.9% for those with BMI greater than or equal to 50 kg/m2.
Story details: A retrospective analysis of 57,957 patients in the NSQIP database who had laparoscopic ventral hernia repair between 2005 and 2015.
Disclosures: Dr. Swendiman and coauthors reported having no financial disclosures.
Source: Academic Surgical Congress. Abstract 50.02.
Poor health literacy raises readmission risk
JACKSONVILLE, FLA. – Low health literacy is a common problem in Veterans Affairs health systems, and patients with low health literacy scores are 50% more likely to return to the hospital within 30 days of discharge after surgery than patients with high health literacy, investigators found in a study of surgery patients at VA medical centers.
“Low health literacy is prevalent among VA surgery patients and is associated with surgical readmissions,” said Samantha Baker, MD, of the University of Alabama at Birmingham and the VA Birmingham Healthcare System. She presented the findings at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
This study used an instrument developed by Lisa Chew, MD, at the University of Washington to determine health literacy scores (Fam Med. 2004;36:588-94). The instrument uses three questions: how often patients have someone else help them read hospital materials; whether they have problems learning about a medical condition because they have difficulty understanding written information; and how confident they are in filling out their own medical forms. Answers are given on a scale of 0-4, with 12 points being the highest score for poor health literacy. This study considered adequate health literacy to be a score of 0-3, and 4-12 as “possibly inadequate health literacy.”
“Of the 722 patients who took the survey, 39.2% had a score of 0; 33.2% had a score of 4 or more,” Dr. Baker said.
The adequate health literacy group had significantly lower rates of unplanned readmissions and a trend toward lower emergency department visits than the possibly inadequate health literacy group, 11.7% vs. 22.5% (P = .003) for the former and 18.7% vs. 24.2% (P = .08) for the latter, Dr. Baker said.
She noted that the ethnic makeup of the groups was similar and the differences in health literacy among the ethnic groups were not statistically significant.
She also mentioned that those with adequate health literacy tended to be younger – 64 vs. 66.9 years – and more likely to be women (“but our number is low for females in the VA,” Dr. Baker said). She added that married patients tended to have lower heath literacy than did single patients.”
The 30-day surgical readmission rate was 13.7% for patients with high health literacy and 22.5% for those with low health literacy. Patients with inadequate health literacy were 53% more likely to be readmitted to the hospital within 30 days of their index operation, she said. Each one-unit increase in health literacy scores – meaning an increase in inadequate health literacy – increased an individual’s risk of readmission by about 6% on an adjusted basis, Dr. Baker said.
“Future work is going to be focused on identifying these patients and developing the interventions to educate and empower this vulnerable population before they are discharged,” Dr. Baker said.
Dr. Baker and coauthors reported having no financial disclosures.
SOURCE: Baker S et al. Academic Surgical Congress.
JACKSONVILLE, FLA. – Low health literacy is a common problem in Veterans Affairs health systems, and patients with low health literacy scores are 50% more likely to return to the hospital within 30 days of discharge after surgery than patients with high health literacy, investigators found in a study of surgery patients at VA medical centers.
“Low health literacy is prevalent among VA surgery patients and is associated with surgical readmissions,” said Samantha Baker, MD, of the University of Alabama at Birmingham and the VA Birmingham Healthcare System. She presented the findings at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
This study used an instrument developed by Lisa Chew, MD, at the University of Washington to determine health literacy scores (Fam Med. 2004;36:588-94). The instrument uses three questions: how often patients have someone else help them read hospital materials; whether they have problems learning about a medical condition because they have difficulty understanding written information; and how confident they are in filling out their own medical forms. Answers are given on a scale of 0-4, with 12 points being the highest score for poor health literacy. This study considered adequate health literacy to be a score of 0-3, and 4-12 as “possibly inadequate health literacy.”
“Of the 722 patients who took the survey, 39.2% had a score of 0; 33.2% had a score of 4 or more,” Dr. Baker said.
The adequate health literacy group had significantly lower rates of unplanned readmissions and a trend toward lower emergency department visits than the possibly inadequate health literacy group, 11.7% vs. 22.5% (P = .003) for the former and 18.7% vs. 24.2% (P = .08) for the latter, Dr. Baker said.
She noted that the ethnic makeup of the groups was similar and the differences in health literacy among the ethnic groups were not statistically significant.
She also mentioned that those with adequate health literacy tended to be younger – 64 vs. 66.9 years – and more likely to be women (“but our number is low for females in the VA,” Dr. Baker said). She added that married patients tended to have lower heath literacy than did single patients.”
The 30-day surgical readmission rate was 13.7% for patients with high health literacy and 22.5% for those with low health literacy. Patients with inadequate health literacy were 53% more likely to be readmitted to the hospital within 30 days of their index operation, she said. Each one-unit increase in health literacy scores – meaning an increase in inadequate health literacy – increased an individual’s risk of readmission by about 6% on an adjusted basis, Dr. Baker said.
“Future work is going to be focused on identifying these patients and developing the interventions to educate and empower this vulnerable population before they are discharged,” Dr. Baker said.
Dr. Baker and coauthors reported having no financial disclosures.
SOURCE: Baker S et al. Academic Surgical Congress.
JACKSONVILLE, FLA. – Low health literacy is a common problem in Veterans Affairs health systems, and patients with low health literacy scores are 50% more likely to return to the hospital within 30 days of discharge after surgery than patients with high health literacy, investigators found in a study of surgery patients at VA medical centers.
“Low health literacy is prevalent among VA surgery patients and is associated with surgical readmissions,” said Samantha Baker, MD, of the University of Alabama at Birmingham and the VA Birmingham Healthcare System. She presented the findings at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
This study used an instrument developed by Lisa Chew, MD, at the University of Washington to determine health literacy scores (Fam Med. 2004;36:588-94). The instrument uses three questions: how often patients have someone else help them read hospital materials; whether they have problems learning about a medical condition because they have difficulty understanding written information; and how confident they are in filling out their own medical forms. Answers are given on a scale of 0-4, with 12 points being the highest score for poor health literacy. This study considered adequate health literacy to be a score of 0-3, and 4-12 as “possibly inadequate health literacy.”
“Of the 722 patients who took the survey, 39.2% had a score of 0; 33.2% had a score of 4 or more,” Dr. Baker said.
The adequate health literacy group had significantly lower rates of unplanned readmissions and a trend toward lower emergency department visits than the possibly inadequate health literacy group, 11.7% vs. 22.5% (P = .003) for the former and 18.7% vs. 24.2% (P = .08) for the latter, Dr. Baker said.
She noted that the ethnic makeup of the groups was similar and the differences in health literacy among the ethnic groups were not statistically significant.
She also mentioned that those with adequate health literacy tended to be younger – 64 vs. 66.9 years – and more likely to be women (“but our number is low for females in the VA,” Dr. Baker said). She added that married patients tended to have lower heath literacy than did single patients.”
The 30-day surgical readmission rate was 13.7% for patients with high health literacy and 22.5% for those with low health literacy. Patients with inadequate health literacy were 53% more likely to be readmitted to the hospital within 30 days of their index operation, she said. Each one-unit increase in health literacy scores – meaning an increase in inadequate health literacy – increased an individual’s risk of readmission by about 6% on an adjusted basis, Dr. Baker said.
“Future work is going to be focused on identifying these patients and developing the interventions to educate and empower this vulnerable population before they are discharged,” Dr. Baker said.
Dr. Baker and coauthors reported having no financial disclosures.
SOURCE: Baker S et al. Academic Surgical Congress.
REPORTING FROM THE ACADEMIC SURGICAL CONGRESS
Key clinical point:
Major finding: The 30-day surgical readmission rate was 13.7% for patients with high health literacy and 22.5% for those with low health literacy.
Data source: Analysis of 722 patients who had general, vascular, or thoracic surgery at four VA Medical Centers from August 2015 to June 2017.
Disclosures: Dr. Baker and coauthors reported having no financial disclosures.
Source: Baker S et al. Academic Surgical Congress.
Laparoscopic procedure safer for SBO in elderly patients
JACKSONVILLE, FLA. – Octogenarians with small-bowel obstruction are about seven times more likely to have open than laparoscopic surgery, but the minimally invasive approach in these patients has been found to reduce their hospital stays and risk of pneumonia afterward, according to results of an observational study of data from the American College of Surgeons National Surgical Quality Improvement Program database.
Dr. Chang said, “Our study was able to show that age and the presence of preoperative sepsis are associated with mortality rather than procedure type, and that there are procedure-type risks associated with open procedures.”
The observational study analyzed 103 laparoscopic and 692 open operations for small-bowel obstruction (SBO) in patients 80 and older from 2006 to 2014. Characteristics of the open and laparoscopic group – age, gender, body mass index, and race – were similar, although the open group had higher American Society of Anesthesiologists classification and incidence of preoperative sepsis, Dr. Chang said.
“Unadjusted outcomes showed longer length of stay [and] higher postoperative mortality and rates of postoperative pneumonia in the open cases vs. laparoscopic,” she said. “But after we made adjustments for preoperative risk variables, age and the presence of preoperative sepsis were associated with mortality, not the operative approach.” Length of stay was 4 days for the laparoscopic patients vs. 8 days for open (P less than .0001).
The researchers performed logistical regression analysis and found that mortality risk rose slightly with age (odds ratio, 1.11; P = .0311) but almost quadrupled with preoperative sepsis (OR, 3.77; P = .0287) regardless of open or laparoscopic approach. For postoperative pneumonia, risk factors were male gender (OR, 2.68; P = .0003) and open procedure (OR, 5.03; P = .0282).
“Our study elucidates that the octogenarian with small-bowel obstruction due to adhesive disease may benefit from an initial laparoscopic approach,” Dr. Change said. “Further prospective studies are warranted.”
Dr. Chang and coauthors reported having no financial disclosures.
SOURCE: Chang E et al. Academic Surgical Congress.
JACKSONVILLE, FLA. – Octogenarians with small-bowel obstruction are about seven times more likely to have open than laparoscopic surgery, but the minimally invasive approach in these patients has been found to reduce their hospital stays and risk of pneumonia afterward, according to results of an observational study of data from the American College of Surgeons National Surgical Quality Improvement Program database.
Dr. Chang said, “Our study was able to show that age and the presence of preoperative sepsis are associated with mortality rather than procedure type, and that there are procedure-type risks associated with open procedures.”
The observational study analyzed 103 laparoscopic and 692 open operations for small-bowel obstruction (SBO) in patients 80 and older from 2006 to 2014. Characteristics of the open and laparoscopic group – age, gender, body mass index, and race – were similar, although the open group had higher American Society of Anesthesiologists classification and incidence of preoperative sepsis, Dr. Chang said.
“Unadjusted outcomes showed longer length of stay [and] higher postoperative mortality and rates of postoperative pneumonia in the open cases vs. laparoscopic,” she said. “But after we made adjustments for preoperative risk variables, age and the presence of preoperative sepsis were associated with mortality, not the operative approach.” Length of stay was 4 days for the laparoscopic patients vs. 8 days for open (P less than .0001).
The researchers performed logistical regression analysis and found that mortality risk rose slightly with age (odds ratio, 1.11; P = .0311) but almost quadrupled with preoperative sepsis (OR, 3.77; P = .0287) regardless of open or laparoscopic approach. For postoperative pneumonia, risk factors were male gender (OR, 2.68; P = .0003) and open procedure (OR, 5.03; P = .0282).
“Our study elucidates that the octogenarian with small-bowel obstruction due to adhesive disease may benefit from an initial laparoscopic approach,” Dr. Change said. “Further prospective studies are warranted.”
Dr. Chang and coauthors reported having no financial disclosures.
SOURCE: Chang E et al. Academic Surgical Congress.
JACKSONVILLE, FLA. – Octogenarians with small-bowel obstruction are about seven times more likely to have open than laparoscopic surgery, but the minimally invasive approach in these patients has been found to reduce their hospital stays and risk of pneumonia afterward, according to results of an observational study of data from the American College of Surgeons National Surgical Quality Improvement Program database.
Dr. Chang said, “Our study was able to show that age and the presence of preoperative sepsis are associated with mortality rather than procedure type, and that there are procedure-type risks associated with open procedures.”
The observational study analyzed 103 laparoscopic and 692 open operations for small-bowel obstruction (SBO) in patients 80 and older from 2006 to 2014. Characteristics of the open and laparoscopic group – age, gender, body mass index, and race – were similar, although the open group had higher American Society of Anesthesiologists classification and incidence of preoperative sepsis, Dr. Chang said.
“Unadjusted outcomes showed longer length of stay [and] higher postoperative mortality and rates of postoperative pneumonia in the open cases vs. laparoscopic,” she said. “But after we made adjustments for preoperative risk variables, age and the presence of preoperative sepsis were associated with mortality, not the operative approach.” Length of stay was 4 days for the laparoscopic patients vs. 8 days for open (P less than .0001).
The researchers performed logistical regression analysis and found that mortality risk rose slightly with age (odds ratio, 1.11; P = .0311) but almost quadrupled with preoperative sepsis (OR, 3.77; P = .0287) regardless of open or laparoscopic approach. For postoperative pneumonia, risk factors were male gender (OR, 2.68; P = .0003) and open procedure (OR, 5.03; P = .0282).
“Our study elucidates that the octogenarian with small-bowel obstruction due to adhesive disease may benefit from an initial laparoscopic approach,” Dr. Change said. “Further prospective studies are warranted.”
Dr. Chang and coauthors reported having no financial disclosures.
SOURCE: Chang E et al. Academic Surgical Congress.
REPORTING FROM THE ACADEMIC SURGICAL CONGRESS
Key clinical point: and older.
Major finding: The open procedure had an odds ratio five times greater than laparoscopic surgery for risk of pneumonia after the operation in this age group (OR, 5.03; P =.0282).
Data source: Observational study of 103 laparoscopic and 692 open cases of surgery for SBO in the ACS NSQIP database from 2006 to 2014.
Disclosures: Dr. Chang and coauthors reported having no financial disclosures.
Source: Chang E et al. Academic Surgical Congress.
The case for closing robotic surgery port sites
JACKSONVILLE, FLA. – Findings from a retrospective chart review of robotic operations performed over 6 years has identified situations in which surgeons may consider closing 8-mm port sites after robotic surgery, according to a presentation at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.

“Although the incidence of hernia through the 8-mm port sites was low, it’s still important because it’s a significant cause of morbidity in these patients,” Dr. Diez-Barroso said. Two of the three 8-mm port-site hernias required emergency surgery for small bowel incarceration.
“Both of the hernias occurred in the left lower quadrant in the lateral most port, near the anterior superior iliac spine,” he said. “The nearest site of muscle insertions was where the abdominal wall muscle layers have a limited ability to slide over one another during insufflation and desufflation and therefore have a lack of ability to seal off the port site correctly.”
These results have caused surgeons in his group to take a closer look at their own practices, Dr. Diez-Barroso said. “In our practice, now we’re considering closure of the ports in that location in the presence of known risk factors for hernia formation,” he said.
Dr. Diez-Barroso noted other scenarios when surgeons might consider closing 8-mm port sites, for example, after a prolonged operation, when significant torque has been placed on the port site, and in obese patients. The two cases of emergency surgery for port-site hernias involved obese patients: a female with a body mass index of 33 kg/m2 who had an abdominoperineal resection and a male with a BMI of 34 kg/m2 who had a right-sided ventral hernia repair.
The study had a number of limitations, Dr. Diez-Barroso said: its small sample size, retrospective nature, and short follow-up. “Moving forward, to understand better the true incidence of port-site hernias, we want further investigation with longer follow-up times and a larger sample size,” he said.
During questions, moderator Lesly Ann Dossett, MD, FACS, of the University of Michigan, Ann Arbor, asked whether there were other steps surgeons could take, such as where to place the ports or how much torque they apply, besides closing the ports.
“We’ve always placed ports with the standard approach: inserting them perpendicular to the abdominal wall,” Dr. Diez-Barroso said. “Others have theorized that the lateral sites undergo more torque, but I think that also needs further investigation.”
Dr. Diez-Barroso and coauthors reported having no financial disclosures.
Source: Diez-Barroso R. Academic Surgical Congress 2018.
JACKSONVILLE, FLA. – Findings from a retrospective chart review of robotic operations performed over 6 years has identified situations in which surgeons may consider closing 8-mm port sites after robotic surgery, according to a presentation at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.

“Although the incidence of hernia through the 8-mm port sites was low, it’s still important because it’s a significant cause of morbidity in these patients,” Dr. Diez-Barroso said. Two of the three 8-mm port-site hernias required emergency surgery for small bowel incarceration.
“Both of the hernias occurred in the left lower quadrant in the lateral most port, near the anterior superior iliac spine,” he said. “The nearest site of muscle insertions was where the abdominal wall muscle layers have a limited ability to slide over one another during insufflation and desufflation and therefore have a lack of ability to seal off the port site correctly.”
These results have caused surgeons in his group to take a closer look at their own practices, Dr. Diez-Barroso said. “In our practice, now we’re considering closure of the ports in that location in the presence of known risk factors for hernia formation,” he said.
Dr. Diez-Barroso noted other scenarios when surgeons might consider closing 8-mm port sites, for example, after a prolonged operation, when significant torque has been placed on the port site, and in obese patients. The two cases of emergency surgery for port-site hernias involved obese patients: a female with a body mass index of 33 kg/m2 who had an abdominoperineal resection and a male with a BMI of 34 kg/m2 who had a right-sided ventral hernia repair.
The study had a number of limitations, Dr. Diez-Barroso said: its small sample size, retrospective nature, and short follow-up. “Moving forward, to understand better the true incidence of port-site hernias, we want further investigation with longer follow-up times and a larger sample size,” he said.
During questions, moderator Lesly Ann Dossett, MD, FACS, of the University of Michigan, Ann Arbor, asked whether there were other steps surgeons could take, such as where to place the ports or how much torque they apply, besides closing the ports.
“We’ve always placed ports with the standard approach: inserting them perpendicular to the abdominal wall,” Dr. Diez-Barroso said. “Others have theorized that the lateral sites undergo more torque, but I think that also needs further investigation.”
Dr. Diez-Barroso and coauthors reported having no financial disclosures.
Source: Diez-Barroso R. Academic Surgical Congress 2018.
JACKSONVILLE, FLA. – Findings from a retrospective chart review of robotic operations performed over 6 years has identified situations in which surgeons may consider closing 8-mm port sites after robotic surgery, according to a presentation at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.

“Although the incidence of hernia through the 8-mm port sites was low, it’s still important because it’s a significant cause of morbidity in these patients,” Dr. Diez-Barroso said. Two of the three 8-mm port-site hernias required emergency surgery for small bowel incarceration.
“Both of the hernias occurred in the left lower quadrant in the lateral most port, near the anterior superior iliac spine,” he said. “The nearest site of muscle insertions was where the abdominal wall muscle layers have a limited ability to slide over one another during insufflation and desufflation and therefore have a lack of ability to seal off the port site correctly.”
These results have caused surgeons in his group to take a closer look at their own practices, Dr. Diez-Barroso said. “In our practice, now we’re considering closure of the ports in that location in the presence of known risk factors for hernia formation,” he said.
Dr. Diez-Barroso noted other scenarios when surgeons might consider closing 8-mm port sites, for example, after a prolonged operation, when significant torque has been placed on the port site, and in obese patients. The two cases of emergency surgery for port-site hernias involved obese patients: a female with a body mass index of 33 kg/m2 who had an abdominoperineal resection and a male with a BMI of 34 kg/m2 who had a right-sided ventral hernia repair.
The study had a number of limitations, Dr. Diez-Barroso said: its small sample size, retrospective nature, and short follow-up. “Moving forward, to understand better the true incidence of port-site hernias, we want further investigation with longer follow-up times and a larger sample size,” he said.
During questions, moderator Lesly Ann Dossett, MD, FACS, of the University of Michigan, Ann Arbor, asked whether there were other steps surgeons could take, such as where to place the ports or how much torque they apply, besides closing the ports.
“We’ve always placed ports with the standard approach: inserting them perpendicular to the abdominal wall,” Dr. Diez-Barroso said. “Others have theorized that the lateral sites undergo more torque, but I think that also needs further investigation.”
Dr. Diez-Barroso and coauthors reported having no financial disclosures.
Source: Diez-Barroso R. Academic Surgical Congress 2018.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Some 8-mm robotic port sites may warrant closure under certain circumstances.
Major finding: Of 178 patients, 3 had complications caused by 8-mm robotic port sites that were not closed, 2 of which required emergency reoperation for small bowel incarceration.
Data source: Retrospective chart review of 178 patients who had robotic general and oncologic surgical procedures between July 2010 and December 2016.
Disclosures: Dr. Diez-Barroso and coauthors reported having no financial disclosures.
Source: Diez-Barroso R. Academic Surgical Congress 2018.
No link found between OR skullcaps and infection
JACKSONVILLE, FLA. – Surgeons who choose to wear a skullcap in the OR can point to yet another study with evidence to bolster their preference.
Two major hospital and nursing credentialing organizations have recommended that hospitals ban skullcaps from the operating room as a practice to control surgical site infections, but a study of almost 2,000 operations at an academic medical center has found that strictly enforcing the ban had no impact on infection rates, according to results of a study presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The study, conducted at Thomas Jefferson University in Philadelphia, showed that rates of surgical site infections (SSIs) were almost identical in the year before and the year after the institution implemented the skullcap ban. “The overall surgical site infection rate was 5.4%, and there were no differences in surgical site infections before or after the headwear policy was adopted,” said Arturo J. Rios-Diaz, MD. The Joint Commission and the Association of periOperative Registered Nurses recommend against the use of skullcaps.
The study reviewed American College of Surgeons National Surgical Quality Improvement Program data on 1,901 patients who had 1,950 clean or clean-contaminated general surgery procedures in 2015, the year before the ban was implemented, and in 2016 (767 in 2015 and 1,183 in 2016). The most common procedures were colectomy (18.2%), pancreatectomy (13.5%), and ventral hernia repair (9.9%). The study excluded orthopedic and vascular operations and any cases with sepsis or an active infection at the time of surgery.
There were some differences between the pre- and postban patient groups. The preban group was younger (median age, 57.91 years vs. 59.75, P = .01) but had more patients who were obese, measured as body mass index above 30 kg/m2 (42.37% vs. 35.23%, P less than .01), and smokers (16.18% vs. 12.27%, P = .02). Wound classification also differed: clean, 38.55% before vs. 43.91% after; and clean-contaminated, 61.45% vs. 56.09% (P = .02). All other demographic and clinical characteristics were similar between the two groups.
“In multivariate logistic regression models controlling for these confounders, there was no association of the banning of skullcaps with decreased surgical site infection rates,” Dr. Rios-Diaz said.
“The adoption of guidelines targeted to optimize patient care should always be welcomed by surgeons,” he said. “However, if they’re going to be implemented on a national level, these policies must be based on higher levels of evidence, so further studies are warranted to assess the validity of the [Joint Commission] headwear guidelines.” According to Dr. Rios-Diaz, the recommendations from the Association of periOperative Registered Nurses are based on two case series from the 1960s and 1970s.
Thomas Jefferson University once again allows skullcaps in the OR, he said.
Dr. Rios-Diaz and his coauthors had no financial relationships to disclose.
SOURCE: Rios-Diaz AJ et al. Annual Academic Surgical Congress. Abstract 09.11.
JACKSONVILLE, FLA. – Surgeons who choose to wear a skullcap in the OR can point to yet another study with evidence to bolster their preference.
Two major hospital and nursing credentialing organizations have recommended that hospitals ban skullcaps from the operating room as a practice to control surgical site infections, but a study of almost 2,000 operations at an academic medical center has found that strictly enforcing the ban had no impact on infection rates, according to results of a study presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The study, conducted at Thomas Jefferson University in Philadelphia, showed that rates of surgical site infections (SSIs) were almost identical in the year before and the year after the institution implemented the skullcap ban. “The overall surgical site infection rate was 5.4%, and there were no differences in surgical site infections before or after the headwear policy was adopted,” said Arturo J. Rios-Diaz, MD. The Joint Commission and the Association of periOperative Registered Nurses recommend against the use of skullcaps.
The study reviewed American College of Surgeons National Surgical Quality Improvement Program data on 1,901 patients who had 1,950 clean or clean-contaminated general surgery procedures in 2015, the year before the ban was implemented, and in 2016 (767 in 2015 and 1,183 in 2016). The most common procedures were colectomy (18.2%), pancreatectomy (13.5%), and ventral hernia repair (9.9%). The study excluded orthopedic and vascular operations and any cases with sepsis or an active infection at the time of surgery.
There were some differences between the pre- and postban patient groups. The preban group was younger (median age, 57.91 years vs. 59.75, P = .01) but had more patients who were obese, measured as body mass index above 30 kg/m2 (42.37% vs. 35.23%, P less than .01), and smokers (16.18% vs. 12.27%, P = .02). Wound classification also differed: clean, 38.55% before vs. 43.91% after; and clean-contaminated, 61.45% vs. 56.09% (P = .02). All other demographic and clinical characteristics were similar between the two groups.
“In multivariate logistic regression models controlling for these confounders, there was no association of the banning of skullcaps with decreased surgical site infection rates,” Dr. Rios-Diaz said.
“The adoption of guidelines targeted to optimize patient care should always be welcomed by surgeons,” he said. “However, if they’re going to be implemented on a national level, these policies must be based on higher levels of evidence, so further studies are warranted to assess the validity of the [Joint Commission] headwear guidelines.” According to Dr. Rios-Diaz, the recommendations from the Association of periOperative Registered Nurses are based on two case series from the 1960s and 1970s.
Thomas Jefferson University once again allows skullcaps in the OR, he said.
Dr. Rios-Diaz and his coauthors had no financial relationships to disclose.
SOURCE: Rios-Diaz AJ et al. Annual Academic Surgical Congress. Abstract 09.11.
JACKSONVILLE, FLA. – Surgeons who choose to wear a skullcap in the OR can point to yet another study with evidence to bolster their preference.
Two major hospital and nursing credentialing organizations have recommended that hospitals ban skullcaps from the operating room as a practice to control surgical site infections, but a study of almost 2,000 operations at an academic medical center has found that strictly enforcing the ban had no impact on infection rates, according to results of a study presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The study, conducted at Thomas Jefferson University in Philadelphia, showed that rates of surgical site infections (SSIs) were almost identical in the year before and the year after the institution implemented the skullcap ban. “The overall surgical site infection rate was 5.4%, and there were no differences in surgical site infections before or after the headwear policy was adopted,” said Arturo J. Rios-Diaz, MD. The Joint Commission and the Association of periOperative Registered Nurses recommend against the use of skullcaps.
The study reviewed American College of Surgeons National Surgical Quality Improvement Program data on 1,901 patients who had 1,950 clean or clean-contaminated general surgery procedures in 2015, the year before the ban was implemented, and in 2016 (767 in 2015 and 1,183 in 2016). The most common procedures were colectomy (18.2%), pancreatectomy (13.5%), and ventral hernia repair (9.9%). The study excluded orthopedic and vascular operations and any cases with sepsis or an active infection at the time of surgery.
There were some differences between the pre- and postban patient groups. The preban group was younger (median age, 57.91 years vs. 59.75, P = .01) but had more patients who were obese, measured as body mass index above 30 kg/m2 (42.37% vs. 35.23%, P less than .01), and smokers (16.18% vs. 12.27%, P = .02). Wound classification also differed: clean, 38.55% before vs. 43.91% after; and clean-contaminated, 61.45% vs. 56.09% (P = .02). All other demographic and clinical characteristics were similar between the two groups.
“In multivariate logistic regression models controlling for these confounders, there was no association of the banning of skullcaps with decreased surgical site infection rates,” Dr. Rios-Diaz said.
“The adoption of guidelines targeted to optimize patient care should always be welcomed by surgeons,” he said. “However, if they’re going to be implemented on a national level, these policies must be based on higher levels of evidence, so further studies are warranted to assess the validity of the [Joint Commission] headwear guidelines.” According to Dr. Rios-Diaz, the recommendations from the Association of periOperative Registered Nurses are based on two case series from the 1960s and 1970s.
Thomas Jefferson University once again allows skullcaps in the OR, he said.
Dr. Rios-Diaz and his coauthors had no financial relationships to disclose.
SOURCE: Rios-Diaz AJ et al. Annual Academic Surgical Congress. Abstract 09.11.
REPORTING FROM THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Findings of this study do not support the ban on surgical skullcaps.
Major finding: No association was found between the skullcap ban and decreased surgical site infection.
Study details: Analysis of ACS NSQIP data on 1,950 surgical cases from before and after the skullcap ban.
Disclosures: The investigators had no financial relationships to disclose.
Source: Rios-Diaz AJ et al. Annual Academic Surgical Congress. Abstract 09.11.
ERAS pathway can cut postdischarge opioid use
JACKSONVILLE, FLA. – An but also to reduce postdischarge opioid prescriptions.
The results of the enhanced recovery after surgery (ERAS) study were reported at the Association for Academic Surgical/Society of Academic Surgeons Academic Congress by Kathryn Hudak, a fourth-year medical student at the University of Alabama at Birmingham (UAB).
The researchers compared outcomes of 197 patients in the ERAS database at the institution who had colorectal surgery in 2015 with 198 patients who had surgery in 2013 and 2014 before the ERAS protocol was put in place.
Overall, the ERAS program had successes. “Using ERAS, we have shown a reduction in hospital length of stay and reduction in postoperative complications, [and] a reduction in hospital costs without any increase in readmissions or mortality,” Ms. Hudak said. Average length of stay decreased by 2 days and postoperative complications by 30%, study results showed.
“One purpose of ERAS is to control pain with as little need for opioids as possible,” she said. Pain management in the ERAS protocol used at UAB involved celecoxib, gabapentin, and acetaminophen before surgery; ketorolac and lidocaine during the operation; and alternating acetaminophen with other nonsteroidal anti-inflammatory drugs and oral oxycodone as needed after surgery. “If ERAS uses multimodal analgesia to avoid opioid use in the hospital, we wanted to know if we could see any effect in the use of opioids outside of the hospital,” Ms. Hudak said.
ERAS patients had more minimally invasive surgery (43.4% vs. 32.5%), more ostomies (38.9% vs. 25.9%), and lower rates of baseline opioid use (15.2% vs. 29.4%). So these patients would be expected to have a lower need for postdischarge pain medications.
For the study overall, 89.6% of patients in both groups were discharged with an opioid prescription but, Ms. Hudak said, “more of our ERAS patients were discharged without a prescription for an opioid – 14.1% vs. 7% in the pre-ERAS patients. “In our ERAS patients, we found a significantly different makeup in those discharge medications,” she said. “Many more patients were discharged on tramadol or a combination of tramadol and oxycodone or hydrocodone – again, using more of those low-potency opioids.”
The study revealed one unexpected finding, Ms. Hudak said. “We found that ERAS patients had a higher number of pills prescribed and OMEs [oral morphine equivalents], and we were surprised by this because we were expecting the opposite,” she said. Among those discharged with opioids, ERAS patients had an average oral morphine equivalent of 403 and 60.6 pills vs. 343 OMEs and 46.9 pills pre-ERAS (P less than .03). However, per-pill OME ratios were lower for the ERAS group: 6.9 vs. 7.6, Ms. Hudak said.
The study also followed up with patients a year after discharge, and found that 34% of ERAS patients needed an additional prescription while 44% of pre-ERAS patients required additional high-potency opioids, Hudak said.
“ERAS does seem to modify postdischarge opioid utilization, but we definitely need to work toward better standardization of opioid prescribing,” Ms. Hudak said. The UAB has since implemented a standardized protocol for residents to prescribe opioids after surgery based on a patient’s risk for postoperative pain, she said.
Ms. Hudak and her coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – An but also to reduce postdischarge opioid prescriptions.
The results of the enhanced recovery after surgery (ERAS) study were reported at the Association for Academic Surgical/Society of Academic Surgeons Academic Congress by Kathryn Hudak, a fourth-year medical student at the University of Alabama at Birmingham (UAB).
The researchers compared outcomes of 197 patients in the ERAS database at the institution who had colorectal surgery in 2015 with 198 patients who had surgery in 2013 and 2014 before the ERAS protocol was put in place.
Overall, the ERAS program had successes. “Using ERAS, we have shown a reduction in hospital length of stay and reduction in postoperative complications, [and] a reduction in hospital costs without any increase in readmissions or mortality,” Ms. Hudak said. Average length of stay decreased by 2 days and postoperative complications by 30%, study results showed.
“One purpose of ERAS is to control pain with as little need for opioids as possible,” she said. Pain management in the ERAS protocol used at UAB involved celecoxib, gabapentin, and acetaminophen before surgery; ketorolac and lidocaine during the operation; and alternating acetaminophen with other nonsteroidal anti-inflammatory drugs and oral oxycodone as needed after surgery. “If ERAS uses multimodal analgesia to avoid opioid use in the hospital, we wanted to know if we could see any effect in the use of opioids outside of the hospital,” Ms. Hudak said.
ERAS patients had more minimally invasive surgery (43.4% vs. 32.5%), more ostomies (38.9% vs. 25.9%), and lower rates of baseline opioid use (15.2% vs. 29.4%). So these patients would be expected to have a lower need for postdischarge pain medications.
For the study overall, 89.6% of patients in both groups were discharged with an opioid prescription but, Ms. Hudak said, “more of our ERAS patients were discharged without a prescription for an opioid – 14.1% vs. 7% in the pre-ERAS patients. “In our ERAS patients, we found a significantly different makeup in those discharge medications,” she said. “Many more patients were discharged on tramadol or a combination of tramadol and oxycodone or hydrocodone – again, using more of those low-potency opioids.”
The study revealed one unexpected finding, Ms. Hudak said. “We found that ERAS patients had a higher number of pills prescribed and OMEs [oral morphine equivalents], and we were surprised by this because we were expecting the opposite,” she said. Among those discharged with opioids, ERAS patients had an average oral morphine equivalent of 403 and 60.6 pills vs. 343 OMEs and 46.9 pills pre-ERAS (P less than .03). However, per-pill OME ratios were lower for the ERAS group: 6.9 vs. 7.6, Ms. Hudak said.
The study also followed up with patients a year after discharge, and found that 34% of ERAS patients needed an additional prescription while 44% of pre-ERAS patients required additional high-potency opioids, Hudak said.
“ERAS does seem to modify postdischarge opioid utilization, but we definitely need to work toward better standardization of opioid prescribing,” Ms. Hudak said. The UAB has since implemented a standardized protocol for residents to prescribe opioids after surgery based on a patient’s risk for postoperative pain, she said.
Ms. Hudak and her coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – An but also to reduce postdischarge opioid prescriptions.
The results of the enhanced recovery after surgery (ERAS) study were reported at the Association for Academic Surgical/Society of Academic Surgeons Academic Congress by Kathryn Hudak, a fourth-year medical student at the University of Alabama at Birmingham (UAB).
The researchers compared outcomes of 197 patients in the ERAS database at the institution who had colorectal surgery in 2015 with 198 patients who had surgery in 2013 and 2014 before the ERAS protocol was put in place.
Overall, the ERAS program had successes. “Using ERAS, we have shown a reduction in hospital length of stay and reduction in postoperative complications, [and] a reduction in hospital costs without any increase in readmissions or mortality,” Ms. Hudak said. Average length of stay decreased by 2 days and postoperative complications by 30%, study results showed.
“One purpose of ERAS is to control pain with as little need for opioids as possible,” she said. Pain management in the ERAS protocol used at UAB involved celecoxib, gabapentin, and acetaminophen before surgery; ketorolac and lidocaine during the operation; and alternating acetaminophen with other nonsteroidal anti-inflammatory drugs and oral oxycodone as needed after surgery. “If ERAS uses multimodal analgesia to avoid opioid use in the hospital, we wanted to know if we could see any effect in the use of opioids outside of the hospital,” Ms. Hudak said.
ERAS patients had more minimally invasive surgery (43.4% vs. 32.5%), more ostomies (38.9% vs. 25.9%), and lower rates of baseline opioid use (15.2% vs. 29.4%). So these patients would be expected to have a lower need for postdischarge pain medications.
For the study overall, 89.6% of patients in both groups were discharged with an opioid prescription but, Ms. Hudak said, “more of our ERAS patients were discharged without a prescription for an opioid – 14.1% vs. 7% in the pre-ERAS patients. “In our ERAS patients, we found a significantly different makeup in those discharge medications,” she said. “Many more patients were discharged on tramadol or a combination of tramadol and oxycodone or hydrocodone – again, using more of those low-potency opioids.”
The study revealed one unexpected finding, Ms. Hudak said. “We found that ERAS patients had a higher number of pills prescribed and OMEs [oral morphine equivalents], and we were surprised by this because we were expecting the opposite,” she said. Among those discharged with opioids, ERAS patients had an average oral morphine equivalent of 403 and 60.6 pills vs. 343 OMEs and 46.9 pills pre-ERAS (P less than .03). However, per-pill OME ratios were lower for the ERAS group: 6.9 vs. 7.6, Ms. Hudak said.
The study also followed up with patients a year after discharge, and found that 34% of ERAS patients needed an additional prescription while 44% of pre-ERAS patients required additional high-potency opioids, Hudak said.
“ERAS does seem to modify postdischarge opioid utilization, but we definitely need to work toward better standardization of opioid prescribing,” Ms. Hudak said. The UAB has since implemented a standardized protocol for residents to prescribe opioids after surgery based on a patient’s risk for postoperative pain, she said.
Ms. Hudak and her coauthors had no financial relationships to disclose.
REPORTING FROM THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Use of the enhanced recovery after surgery (ERAS) pathway reduces discharge prescriptions for opioids after colorectal surgery.
Major finding: 14.2% of ERAS patients were discharged without an opioid prescription vs. 7% for pre-ERAS patients.
Data source: An analysis of a single-institution ERAS database of 197 ERAS patients, compared with 198 patients who did not follow the ERAS pathway.
Disclosures: Ms. Hudak reported having no relevant financial disclosures.