User login
Your 15-year-old patient requests an IUD without parental knowledge
CASE Adolescent seeks care without parent
A 15-year-old patient (G0) presents to the gynecology clinic requesting birth control. She reports being sexually active over the past 6 months and having several male partners over the past 2 years. She and her current male partner use condoms inconsistently. She reports being active in school sports, and her academic performance has been noteworthy. Her peers have encouraged her to seek out birth control; one of her good friends recently became pregnant and dropped out of school. She states that her best friend went to a similar clinic and received a “gynecologic encounter” that included information regarding safe sex and contraception, with no pelvic exam required for her to receive birth control pills.
The patient insists that her parents are not to know of her request for contraception due to sexual activity or that she is a patient at the clinic. The gynecologist covering the clinic is aware of the American College of Obstetricians and Gynecologists Committee on Adolescent Health Care and their many publications. The patient is counseled regarding human papillomavirus (HPV) vaccination and screened for sexually transmitted infections. In addition, the gynecologist discusses contraceptive options with the patient, ranging from oral contraceptives, vaginal rings, subdermal implants, depomedroxyprogesterone acetate, as well as intrauterine devices (IUDs). The gynecologist emphasizes safe sex and advises that her partner consider use of condoms independent of her method of birth control. The patient asks for oral contraceptives and is given information about their use and risks, and she indicates that she understands.
A few months later the patient requests an IUD, as she would like to have lighter menses and not have to remember to take a pill every day. The provider obtains informed consent for the insertion procedure; the patient signs the appropriate forms.
The IUD is inserted, with difficulty, by a resident physician in the clinic. The patient experiences severe pelvic pain during and immediately following the insertion. She is sent home and told to contact the clinic or another health care provider or proceed to the local emergency department should pain persist or if fever develops.
The patient returns 72 hours later in pain. Pelvic ultrasonography shows the IUD out of place and at risk of perforating the fundus of the uterus. Later that day the patient’s mother calls the clinic, saying that she found a statement of service with the clinic’s number on it in her daughter’s bedroom. She wants to know if her daughter is there, what is going on, and what services have been or are being provided. In passing she remarks that she has no intention of paying (or allowing her insurance to pay for) any care that was provided.
What are the provider’s obligations at this point, both medically and legally?
Medical and legal considerations
One of the most difficult and important health law questions in adolescent medicine is the ability of minors to consent to treatment and to control the health care information resulting from treatment. (“Minor” describes a child or adolescent who has not obtained the age of legal consent, generally 18 years old, to lawfully enter into a legal transaction.)
Continue to: The consent of minor patients...
The consent of minor patients
The traditional legal rule is that parents or guardians (“parent” refers to both) must consent to medical treatment for minor children. There is an exception for emergency situations but generally minors do not provide consent for medical care, a parent does.1 The parent typically is obliged to provide payment (often through insurance) for those services.
This traditional rule has some exceptions—the emergency exception already noted and the case of emancipated minors, notably an adolescent who is living almost entirely independent of her parents (for example, she is married or not relying on parents in a meaningful way). In recent times there has been increasing authority for “mature minors” to make some medical decisions.2 A mature minor is one who has sufficient understanding and judgment to appreciate the consequences, benefits, and risks of accepting proposed medical intervention.
No circumstance involving adolescent treatment has been more contentious than services related to abortion and, to a lesser degree, contraception.3 Both the law of consent to services and the rights of parents to obtain information about contraceptive and abortion services have been a matter of strong, continuing debate. The law in these areas varies greatly from state-to-state, and includes a mix of state law (statutes and court decisions) with an overlay of federal constitutional law related to reproduction-related decisions of adolescents. In addition, the law in this area of consent and information changes relatively frequently.4 Clinicians, of course, must focus on the consent laws of the state in which they practice.
STI counseling and treatment
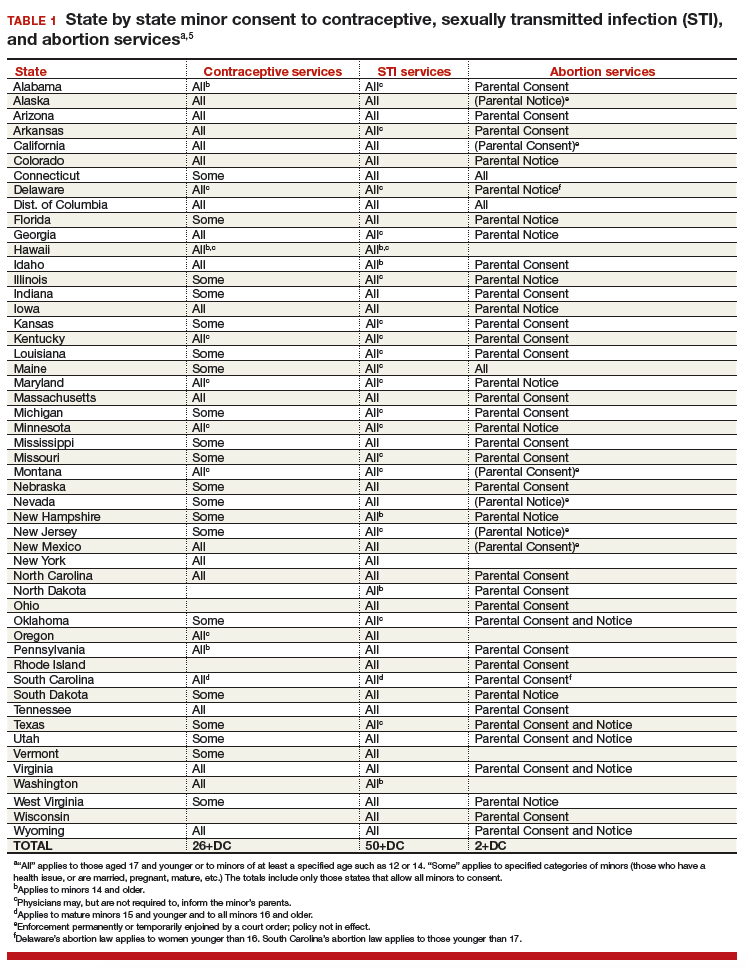
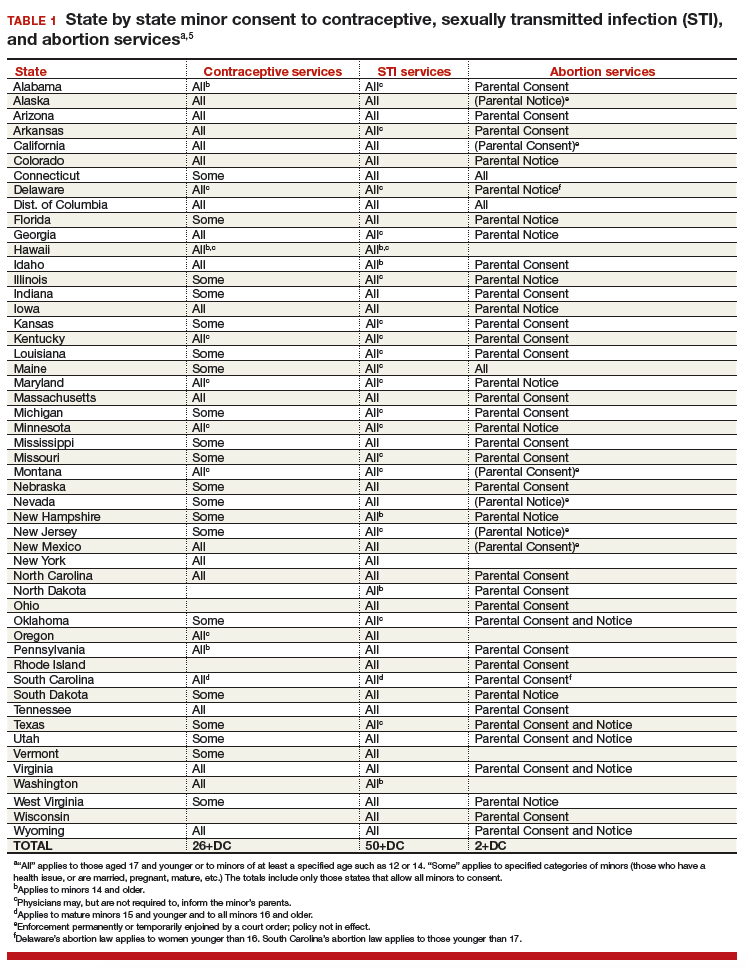
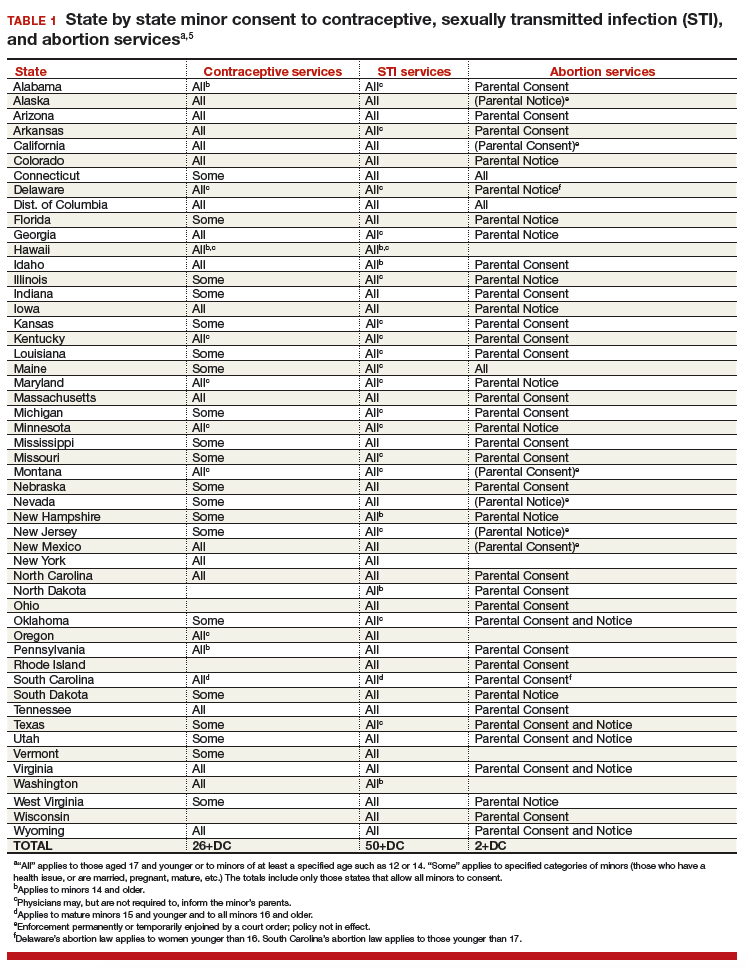
All states permit a minor patient to consent to treatment for an STI (TABLE 1).5 A number of states expressly permit, but do not require, health care providers to inform parents of treatment when a physician determines it would be in the best interest of the minor. Thus, the clinic would not be required to provide proactively the information to our case patient’s mother (regarding any STI issues) when she called.6
Contraception
Consent for contraception is more complicated. About half the states allow minors who have reached a certain age (12, 14, or 16 years) to consent to contraception. About 20 other states allow some minors to consent to contraceptive services, but the “allowed group” may be fairly narrow (eg, be married, have a health issue, or be “mature”). In 4 states there is currently no clear legal authority to provide contraceptive services to minors, yet those states do not specifically prohibit it. The US Supreme Court has held that a state cannot completely prohibit the availability of contraception to minors.7 The reach of that decision, however, is not clear and may not extend beyond what the states currently permit.
The ability of minors to consent to contraception services does not mean that there is a right to consent to all contraceptive options. As contraception becomes more irreversible, permanent, or risky, it is more problematic. For example, consent to sterilization would not ordinarily be within a minor’s recognized ability to consent. Standard, low risk, reversible contraception generally is covered by these state laws.8
In our case here, the patient likely was able to consent to contraception—initially to the oral contraception and later to the IUD. The risks and reversibility of both are probably within her ability to consent.9,10 Of course, if the care was provided in a state that does not include the patient within the groups that can give consent to contraception, it is possible that she might not have the legal authority to consent.
Continue to: General requirements of consent...
General requirements of consent
Even when adolescent consent is permitted for treatment, including in cases of contraception, it is essential that all of the legal and ethical requirements related to informed consent are met.
1. The adolescent has the capacity to consent. This means not only that the state-mandated requirements are met (age, for example) but also that the patient can and does understand the various elements of consent, and can make a sensible, informed decision.
The bottom line is “adolescent capacity is a complex process dependent upon the development of maturity of the adolescent, degree of intervention, expected benefit of the medical procedure, and the sociocultural context surrounding the decision.”11 Other items of interest include the “evolving capacity” of the child,12 which is the concept of increasing ability of the teen to process information and provide more appropriate informed consent. Central nervous system (CNS) maturation allows the adolescent to become increasingly more capable of decision making and has awareness of consequences of such decisions. Abstract thinking capabilities is a reflection of this CNS maturing process. If this competency is not established, the adolescent patient cannot give legitimate consent.
2. The patient must be given appropriate information (be “informed”). The discussion should include information relevant to the condition being treated (and the disease process if relevant). In addition, information about the treatment or intervention proposed and its risks and alternatives must be provided to the patient and in a way that is understandable.
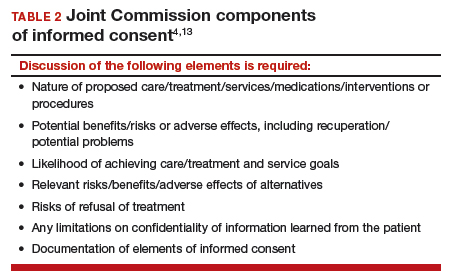
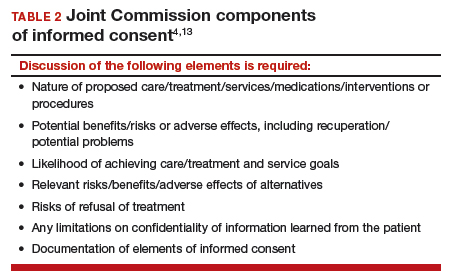
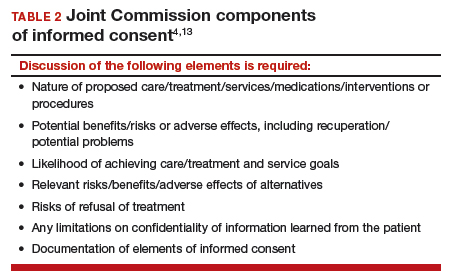
3. As with all patients, consent must be voluntary and free of coercion or manipulation. These elements of informed consent are expanded on by the Joint Commission, which has established a number of components of informed consent (TABLE 2).4,13
Confidentiality and release of information to parents and others
Similar to consent, parents historically have had the authority to obtain medical information about their minor children. This right generally continues today, with some limitations. The right to give consent generally carries with it the right to medical information. There are some times when parents may access medical information even if they have not given consent.
This right adds complexity to minor consent and is an important treatment issue and legal consideration because confidentiality for adolescents affects quality of care. Adolescents report that “confidentiality is an important factor in their decision to seek [medical] care.”14 Many parents are under the assumption that the health care provider will automatically inform them independent of whether or not the adolescent expressed precise instruction not to inform.15,16
Of course if a minor patient authorizes the physician to provide information to her parents, that is consent and the health care provider may then provide the information. If the patient instructs the provider to convey the information, the practitioner would ordinarily be expected to be proactive in providing the information to the parent. The issue of “voluntariness” of the waiver of confidentiality can be a question, and the physician may discuss that question with the patient. Ordinarily, however, once a minor has authorized disclosure to the parent, the clinician has the authority to disclose the information to the parent, but not to others.
All of the usual considerations of confidentiality in health care apply to adolescent ObGyn services and care. This includes the general obligation not to disclose information without consent and to ensure that health care information is protected from accidental release as required by the Health Insurance Portability and Accountability Act (HIPAA) and other health information privacy laws.17
It is important to emphasize that the issues of consent to abortion are much different than those for contraception and sexually transmitted infections. As our case presentation does not deal with abortion, we will address this complex but important discussion in the future--as there are an estimated 90,000 abortions in adolescent girls annually.1
Given that abortion consent and notification laws are often complex, any physician providing abortion services to any minor should have sound legal advice on the requirements of the pertinent state law. In earlier publications of this section in OBG Management we have discussed the importance of practitioners having an ongoing relationship with a health law attorney. We make this point again, as this person can provide advice on consent and the rights of parents to have information about their minor children.
Reference
- Henshaw SK. U.S. teenage pregnancy statistics with comparative statistics for women age 20-24. New York, New York: Alan Guttmacher Institute; May 2003.
Continue to: How and when to protect minor confidentiality...
How and when to protect minor confidentiality
A clinician cannot assure minors of absolute confidentiality and should not agree to do so or imply that they are doing so.18 In our hypothetical case, when the patient told the physician that her parents were not to know of any of her treatment or communications, the provider should not have acquiesced by silence. He/she might have responded along these lines: “I have a strong commitment to confidentiality of your information, and we take many steps to protect that information. The law also allows some special protection of health care information. Despite the commitment to privacy, there are circumstances in which the law requires disclosure of information—and that might even be to parents. In addition, if you want any of your care covered by insurance, we would have to disclose that. While I expect that we can do as you ask about maintaining your confidentiality, no health care provider can absolutely guarantee it.”
Proactive vs reactive disclosure. There is “proactive” disclosure of information and “reactive” disclosure. Proactive is when the provider (without being asked) contacts a parent or others and provides information. Some states require proactive information about specific kinds of treatment (especially abortion services). For the most part, in states where a minor can legally consent to treatment, health care providers are not required to proactively disclose information.19
Clinicians may be required to respond to parental requests for information, which is reactive disclosure and is reflected in our case presentation. Even in such circumstances, however, the individual providing care may seek to avoid disclosure. In many states, the law would not require the release of this information (but would permit it if it is in the best interest of the patient). In addition, there are practical ways of avoiding the release of information. For example, the health care provider might acknowledge the interest and desire of the parent to have the information, but might humbly explain that in the experience of many clinicians protecting the confidentiality of patients is very important to successful treatment and it is the policy of the office/clinic not to breach the expectation of patient confidentiality except where that is clearly in the best interest of the patient or required by law.
In response to the likely question, “Well, isn’t that required by law?” the clinician can honestly reply, “I don’t know. There are many complex factors in the law regarding disclosure of medical information and as I am not an attorney I do not know how they all apply in this instance.” In some cases the parent may push the matter or take some kind of legal action. It is in this type of situation that an attorney familiar with health law and the clinician’s practice can be invaluable.
When parents are involved in the minor’s treatment (bringing the patient to the office/clinic, for example), there is an opportunity for an understanding, or agreement, among the patient, provider, and parent about what information the parent will receive. Ordinarily the agreement should not create the expectation of detailed information for the parent. Perhaps, for example, the physician will provide information only when he or she believes that doing so will be in the best interest of the patient. Even with parental agreement, complete confidentiality cannot be assured for minor patients. There may, for example, be another parent who will not feel bound by the established understanding, and the law requires some disclosures (in the case of child abuse or a court order).20
Continue to: Accidental disclosure...
Accidental disclosure. Health care providers also should make sure that office procedures do not unnecessarily or accidentally disclose information about patients. For example, routinely gathering information about insurance coverage may well trigger the release of information to the policy holder (often a parent). Thus, there should be clear understandings about billing, insurance, and related issues before information is divulged by the patient. This should be part of the process of obtaining informed consent to treatment. It should be up front and honest. Developing a clear understanding of the legal requirements of the state is essential, so that assurance of confidentiality is on legal, solid ground.
As the pediatric and adolescent segment of gynecologic care continues to evolve, it is noteworthy that the American Board of Obstetrics and Gynecology recently has established a "Focused Practice" designation in pediatric adolescent gynecology. This allows ObGyns to have an ongoing level of professional education in this specialized area. Additional information can be obtained at www.abog.org or [email protected].
More resources for adolescent contraceptive care include:
- The American College of Obstetricians and Gynecologists (ACOG) "Birth Control (Especially for Teens)" frequently asked questions information series (https://www.acog.org/Patients/FAQs/Birth-Control-Especially-for-Teens)
- ACOG's Adolescent Healthcare Committee Opinions address adolescent pregnancy, contraception, and sexual activity (https://www.acog.org/-/media/List-of-Titles/COListOfTitles.pdf)
- ACOG statement on teen pregnancy and contraception, April 7, 2015 (https://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Teen-Pregnancy-and-Contraception?IsMobileSet=false)
- North American Society for Pediatric and Adolescent Gynecology resources for patients (https://www.naspag.org/page/patienttools)
- Society for Adolescent Health and Medicine statement regarding contraceptive access policies (https://www.adolescenthealth.org)
- The Guttmacher Institute's overview of state laws relevant to minor consent, as of January 1, 2019 (https://www.guttmacher.org/state-policy/explore/overview-minors-consent-law). It is updated frequently.
Abuse reporting obligations
All states have mandatory child abuse reporting laws. These laws require medical professionals (and others) to report known, and often suspected, abuse of children. Abuse includes physical, sexual, or emotional, and generally also includes neglect that is harming a child. When there is apparent sexual or physical abuse, the health care provider is obligated to report it to designated state authorities, generally child protective services. Reporting laws vary from state to state based on the relationship between the suspected abuser and the minor, the nature of the harm, and how strong the suspicion of abuse needs to be. The failure to make required reports is a crime in most states and also may result in civil liability or licensure discipline. Criminal charges seldom result from the failure to report, but in some cases the failure to report may have serious consequences for the professional.
An ObGyn example of the complexity of reporting laws, and variation from state to state, is in the area of “statutory rape” reporting. Those state laws, which define serious criminal offenses, set out the age below which an individual is not legally capable of consenting to sexual activity. It varies among states, but may be an absolute age of consent, the age differential between the parties, or some combination of age and age differential.21 The question of reporting is further complicated by the issue of when statutory rape must be reported—for example, the circumstances when the harm to the underage person is sufficient to require reporting.22
Laws are complex, as is practice navigation
It is apparent that navigating these issues makes it essential for an ObGyn practice to have clear policies and practices regarding reporting, yet the overall complexity is also why it is so difficult to develop those policies in the first place. Of course, they must be tailored to the state in which the practice resides. Once again, the need is clear for health care professionals to have an ongoing relationship with a health attorney who can help navigate ongoing questions.
- Benjamin L, Ishimine P, Joseph M, et al. Evaluation and treatment of minors. Ann Emerg Med. 2018;71(2):225-232.
- Coleman D, Rosoff P. The legal authority of mature minors to consent to general medical treatment. Pediatrics. 2013;13:786-793.
- American College of Obstetricians and Gynecologists. Committee Opinion No. 699. Adolescent pregnancy, contraception, and sexual activity. Obstet Gynecol. 2017;129:e142-e149.
- Tillett J. Adolescents and informed consent. J Perinat Neonat Nurs. 2005;19:112-121.
- An overview of minor's consent law. Guttmacher Institute's website. https://www.guttmacher.org/state-policy/explore/overview-minors-consent-law. Accessed February 14, 2019.
- Chelmow D, Karjane N, Ricciotti HA, et al, eds. A 16-year-old adolescent requesting confidential treatment for chlamydia exposure (understanding state laws regarding minors and resources). Office Gynecology: A Case-Based Approach. Cambridge, United Kingdom: Cambridge University Press; January 31, 2019:39.
- Carey v Population Services, 431 US 678 (1977).
- Williams RL, Meredith AH, Ott MA. Expanding adolescent access to hormonal contraception: an update on over-the-counter, pharmacist prescribing, and web-based telehealth approaches. Curr Opin Obstet Gynecol. 2018;30:458-464.
- McClellan K, Temples H, Miller L. The latest in teen pregnancy prevention: long-acting reversible contraception. J Pediatr Health Care. 2018;32:e91-e97.
- Behmer Hansen RT, Arora KS. Consenting to invasive contraceptives: an ethical analysis of adolescent decision-making authority for long-acting reversible contraception. J Med Ethics. 2018;44:585-588.
- Robertson D. Opinions in pediatric and adolescent gynecology. J Pediatr Adolesc Gynecol. 2008:21:47-51.
- Lansdown G. The evolving capacities of the child. Florence, Italy: UNICEF Innocenti Research Centre, Innocenti Insight; 2005. https://www.unicef-irc.org/publications/384-the-evolving-capacities-of-the-child.html. Accessed February 15, 2019.
- Clapp JT, Fleisher LA. What is the realistic scope of informed consent? Jt Comm J Qual Patient Saf. 2018;44(6):341-342.
- Berlan E, Bravender T. Confidentiality, consent and caring for the adolescent. Curr Opin Pediatr. 2009;21:450-456.
- Schantz K. Who Needs to Know? Confidentiality in Adolescent Sexual Health Care. Act for Youth website. http://www.actforyouth.net/resources/rf/rf_confidentiality_1118.pdf. Accessed February 14, 2019.
- Lynn A, Kodish E, Lazebnik R, et al. Understanding confidentiality: perspectives of African American adolescents and their parents. J Adolesc Health. 2006;39:261-265.
- English A, Ford CA. The HIPAA privacy rule and adolescents: legal questions and clinical challenges. Perspect Sex Reprod Health. 2004;36:80-86.
- Schapiro NA, Mejia J. Adolescent confidentiality and women's health: history, rationale, and current threats. Nurs Clin North Am. 2018;53:145-156.
- Scott NL, Alderman EM, 2018. Case of a girl with a secret. In: Adolescent Gynecology: A Clinical Casebook. New York, New York: Springer International; 2017:3-11.
- Cullitan CM. Please don't tell my mom--a minor's right to informational privacy. JL & Educ. 2011;40:417-460.
- Bierie DM, Budd KM. Romeo, Juliet, and statutory rape. Sex Abuse. 2018;30:296-321.
- Mathews B. A taxonomy of duties to report child sexual abuse: legal developments offer new ways to facilitate disclosure. Child Abuse Negl. 2019;88:337-347.
CASE Adolescent seeks care without parent
A 15-year-old patient (G0) presents to the gynecology clinic requesting birth control. She reports being sexually active over the past 6 months and having several male partners over the past 2 years. She and her current male partner use condoms inconsistently. She reports being active in school sports, and her academic performance has been noteworthy. Her peers have encouraged her to seek out birth control; one of her good friends recently became pregnant and dropped out of school. She states that her best friend went to a similar clinic and received a “gynecologic encounter” that included information regarding safe sex and contraception, with no pelvic exam required for her to receive birth control pills.
The patient insists that her parents are not to know of her request for contraception due to sexual activity or that she is a patient at the clinic. The gynecologist covering the clinic is aware of the American College of Obstetricians and Gynecologists Committee on Adolescent Health Care and their many publications. The patient is counseled regarding human papillomavirus (HPV) vaccination and screened for sexually transmitted infections. In addition, the gynecologist discusses contraceptive options with the patient, ranging from oral contraceptives, vaginal rings, subdermal implants, depomedroxyprogesterone acetate, as well as intrauterine devices (IUDs). The gynecologist emphasizes safe sex and advises that her partner consider use of condoms independent of her method of birth control. The patient asks for oral contraceptives and is given information about their use and risks, and she indicates that she understands.
A few months later the patient requests an IUD, as she would like to have lighter menses and not have to remember to take a pill every day. The provider obtains informed consent for the insertion procedure; the patient signs the appropriate forms.
The IUD is inserted, with difficulty, by a resident physician in the clinic. The patient experiences severe pelvic pain during and immediately following the insertion. She is sent home and told to contact the clinic or another health care provider or proceed to the local emergency department should pain persist or if fever develops.
The patient returns 72 hours later in pain. Pelvic ultrasonography shows the IUD out of place and at risk of perforating the fundus of the uterus. Later that day the patient’s mother calls the clinic, saying that she found a statement of service with the clinic’s number on it in her daughter’s bedroom. She wants to know if her daughter is there, what is going on, and what services have been or are being provided. In passing she remarks that she has no intention of paying (or allowing her insurance to pay for) any care that was provided.
What are the provider’s obligations at this point, both medically and legally?
Medical and legal considerations
One of the most difficult and important health law questions in adolescent medicine is the ability of minors to consent to treatment and to control the health care information resulting from treatment. (“Minor” describes a child or adolescent who has not obtained the age of legal consent, generally 18 years old, to lawfully enter into a legal transaction.)
Continue to: The consent of minor patients...
The consent of minor patients
The traditional legal rule is that parents or guardians (“parent” refers to both) must consent to medical treatment for minor children. There is an exception for emergency situations but generally minors do not provide consent for medical care, a parent does.1 The parent typically is obliged to provide payment (often through insurance) for those services.
This traditional rule has some exceptions—the emergency exception already noted and the case of emancipated minors, notably an adolescent who is living almost entirely independent of her parents (for example, she is married or not relying on parents in a meaningful way). In recent times there has been increasing authority for “mature minors” to make some medical decisions.2 A mature minor is one who has sufficient understanding and judgment to appreciate the consequences, benefits, and risks of accepting proposed medical intervention.
No circumstance involving adolescent treatment has been more contentious than services related to abortion and, to a lesser degree, contraception.3 Both the law of consent to services and the rights of parents to obtain information about contraceptive and abortion services have been a matter of strong, continuing debate. The law in these areas varies greatly from state-to-state, and includes a mix of state law (statutes and court decisions) with an overlay of federal constitutional law related to reproduction-related decisions of adolescents. In addition, the law in this area of consent and information changes relatively frequently.4 Clinicians, of course, must focus on the consent laws of the state in which they practice.
STI counseling and treatment
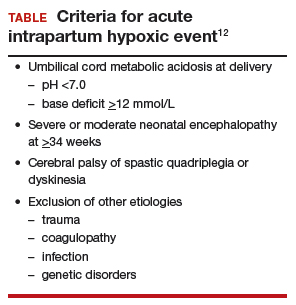
All states permit a minor patient to consent to treatment for an STI (TABLE 1).5 A number of states expressly permit, but do not require, health care providers to inform parents of treatment when a physician determines it would be in the best interest of the minor. Thus, the clinic would not be required to provide proactively the information to our case patient’s mother (regarding any STI issues) when she called.6
Contraception
Consent for contraception is more complicated. About half the states allow minors who have reached a certain age (12, 14, or 16 years) to consent to contraception. About 20 other states allow some minors to consent to contraceptive services, but the “allowed group” may be fairly narrow (eg, be married, have a health issue, or be “mature”). In 4 states there is currently no clear legal authority to provide contraceptive services to minors, yet those states do not specifically prohibit it. The US Supreme Court has held that a state cannot completely prohibit the availability of contraception to minors.7 The reach of that decision, however, is not clear and may not extend beyond what the states currently permit.
The ability of minors to consent to contraception services does not mean that there is a right to consent to all contraceptive options. As contraception becomes more irreversible, permanent, or risky, it is more problematic. For example, consent to sterilization would not ordinarily be within a minor’s recognized ability to consent. Standard, low risk, reversible contraception generally is covered by these state laws.8
In our case here, the patient likely was able to consent to contraception—initially to the oral contraception and later to the IUD. The risks and reversibility of both are probably within her ability to consent.9,10 Of course, if the care was provided in a state that does not include the patient within the groups that can give consent to contraception, it is possible that she might not have the legal authority to consent.
Continue to: General requirements of consent...
General requirements of consent
Even when adolescent consent is permitted for treatment, including in cases of contraception, it is essential that all of the legal and ethical requirements related to informed consent are met.
1. The adolescent has the capacity to consent. This means not only that the state-mandated requirements are met (age, for example) but also that the patient can and does understand the various elements of consent, and can make a sensible, informed decision.
The bottom line is “adolescent capacity is a complex process dependent upon the development of maturity of the adolescent, degree of intervention, expected benefit of the medical procedure, and the sociocultural context surrounding the decision.”11 Other items of interest include the “evolving capacity” of the child,12 which is the concept of increasing ability of the teen to process information and provide more appropriate informed consent. Central nervous system (CNS) maturation allows the adolescent to become increasingly more capable of decision making and has awareness of consequences of such decisions. Abstract thinking capabilities is a reflection of this CNS maturing process. If this competency is not established, the adolescent patient cannot give legitimate consent.
2. The patient must be given appropriate information (be “informed”). The discussion should include information relevant to the condition being treated (and the disease process if relevant). In addition, information about the treatment or intervention proposed and its risks and alternatives must be provided to the patient and in a way that is understandable.
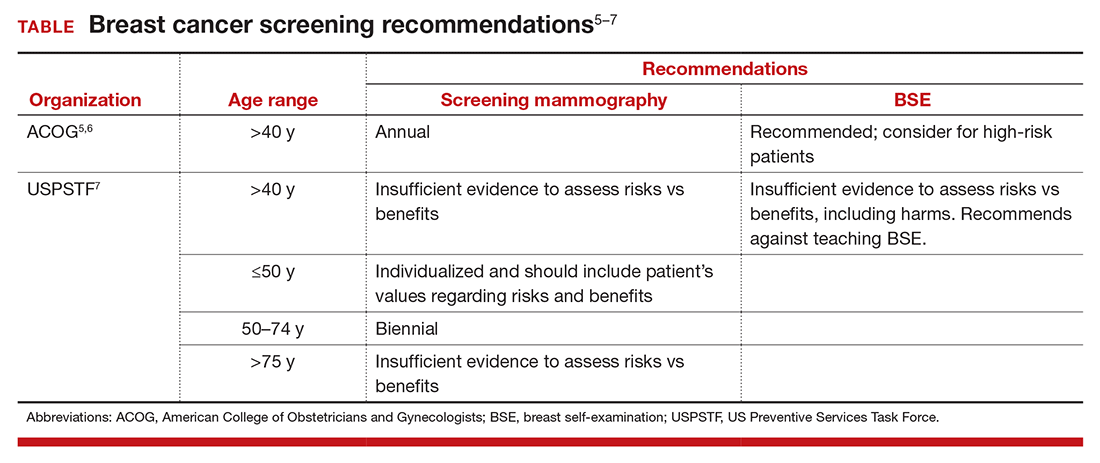
3. As with all patients, consent must be voluntary and free of coercion or manipulation. These elements of informed consent are expanded on by the Joint Commission, which has established a number of components of informed consent (TABLE 2).4,13
Confidentiality and release of information to parents and others
Similar to consent, parents historically have had the authority to obtain medical information about their minor children. This right generally continues today, with some limitations. The right to give consent generally carries with it the right to medical information. There are some times when parents may access medical information even if they have not given consent.
This right adds complexity to minor consent and is an important treatment issue and legal consideration because confidentiality for adolescents affects quality of care. Adolescents report that “confidentiality is an important factor in their decision to seek [medical] care.”14 Many parents are under the assumption that the health care provider will automatically inform them independent of whether or not the adolescent expressed precise instruction not to inform.15,16
Of course if a minor patient authorizes the physician to provide information to her parents, that is consent and the health care provider may then provide the information. If the patient instructs the provider to convey the information, the practitioner would ordinarily be expected to be proactive in providing the information to the parent. The issue of “voluntariness” of the waiver of confidentiality can be a question, and the physician may discuss that question with the patient. Ordinarily, however, once a minor has authorized disclosure to the parent, the clinician has the authority to disclose the information to the parent, but not to others.
All of the usual considerations of confidentiality in health care apply to adolescent ObGyn services and care. This includes the general obligation not to disclose information without consent and to ensure that health care information is protected from accidental release as required by the Health Insurance Portability and Accountability Act (HIPAA) and other health information privacy laws.17
It is important to emphasize that the issues of consent to abortion are much different than those for contraception and sexually transmitted infections. As our case presentation does not deal with abortion, we will address this complex but important discussion in the future--as there are an estimated 90,000 abortions in adolescent girls annually.1
Given that abortion consent and notification laws are often complex, any physician providing abortion services to any minor should have sound legal advice on the requirements of the pertinent state law. In earlier publications of this section in OBG Management we have discussed the importance of practitioners having an ongoing relationship with a health law attorney. We make this point again, as this person can provide advice on consent and the rights of parents to have information about their minor children.
Reference
- Henshaw SK. U.S. teenage pregnancy statistics with comparative statistics for women age 20-24. New York, New York: Alan Guttmacher Institute; May 2003.
Continue to: How and when to protect minor confidentiality...
How and when to protect minor confidentiality
A clinician cannot assure minors of absolute confidentiality and should not agree to do so or imply that they are doing so.18 In our hypothetical case, when the patient told the physician that her parents were not to know of any of her treatment or communications, the provider should not have acquiesced by silence. He/she might have responded along these lines: “I have a strong commitment to confidentiality of your information, and we take many steps to protect that information. The law also allows some special protection of health care information. Despite the commitment to privacy, there are circumstances in which the law requires disclosure of information—and that might even be to parents. In addition, if you want any of your care covered by insurance, we would have to disclose that. While I expect that we can do as you ask about maintaining your confidentiality, no health care provider can absolutely guarantee it.”
Proactive vs reactive disclosure. There is “proactive” disclosure of information and “reactive” disclosure. Proactive is when the provider (without being asked) contacts a parent or others and provides information. Some states require proactive information about specific kinds of treatment (especially abortion services). For the most part, in states where a minor can legally consent to treatment, health care providers are not required to proactively disclose information.19
Clinicians may be required to respond to parental requests for information, which is reactive disclosure and is reflected in our case presentation. Even in such circumstances, however, the individual providing care may seek to avoid disclosure. In many states, the law would not require the release of this information (but would permit it if it is in the best interest of the patient). In addition, there are practical ways of avoiding the release of information. For example, the health care provider might acknowledge the interest and desire of the parent to have the information, but might humbly explain that in the experience of many clinicians protecting the confidentiality of patients is very important to successful treatment and it is the policy of the office/clinic not to breach the expectation of patient confidentiality except where that is clearly in the best interest of the patient or required by law.
In response to the likely question, “Well, isn’t that required by law?” the clinician can honestly reply, “I don’t know. There are many complex factors in the law regarding disclosure of medical information and as I am not an attorney I do not know how they all apply in this instance.” In some cases the parent may push the matter or take some kind of legal action. It is in this type of situation that an attorney familiar with health law and the clinician’s practice can be invaluable.
When parents are involved in the minor’s treatment (bringing the patient to the office/clinic, for example), there is an opportunity for an understanding, or agreement, among the patient, provider, and parent about what information the parent will receive. Ordinarily the agreement should not create the expectation of detailed information for the parent. Perhaps, for example, the physician will provide information only when he or she believes that doing so will be in the best interest of the patient. Even with parental agreement, complete confidentiality cannot be assured for minor patients. There may, for example, be another parent who will not feel bound by the established understanding, and the law requires some disclosures (in the case of child abuse or a court order).20
Continue to: Accidental disclosure...
Accidental disclosure. Health care providers also should make sure that office procedures do not unnecessarily or accidentally disclose information about patients. For example, routinely gathering information about insurance coverage may well trigger the release of information to the policy holder (often a parent). Thus, there should be clear understandings about billing, insurance, and related issues before information is divulged by the patient. This should be part of the process of obtaining informed consent to treatment. It should be up front and honest. Developing a clear understanding of the legal requirements of the state is essential, so that assurance of confidentiality is on legal, solid ground.
As the pediatric and adolescent segment of gynecologic care continues to evolve, it is noteworthy that the American Board of Obstetrics and Gynecology recently has established a "Focused Practice" designation in pediatric adolescent gynecology. This allows ObGyns to have an ongoing level of professional education in this specialized area. Additional information can be obtained at www.abog.org or [email protected].
More resources for adolescent contraceptive care include:
- The American College of Obstetricians and Gynecologists (ACOG) "Birth Control (Especially for Teens)" frequently asked questions information series (https://www.acog.org/Patients/FAQs/Birth-Control-Especially-for-Teens)
- ACOG's Adolescent Healthcare Committee Opinions address adolescent pregnancy, contraception, and sexual activity (https://www.acog.org/-/media/List-of-Titles/COListOfTitles.pdf)
- ACOG statement on teen pregnancy and contraception, April 7, 2015 (https://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Teen-Pregnancy-and-Contraception?IsMobileSet=false)
- North American Society for Pediatric and Adolescent Gynecology resources for patients (https://www.naspag.org/page/patienttools)
- Society for Adolescent Health and Medicine statement regarding contraceptive access policies (https://www.adolescenthealth.org)
- The Guttmacher Institute's overview of state laws relevant to minor consent, as of January 1, 2019 (https://www.guttmacher.org/state-policy/explore/overview-minors-consent-law). It is updated frequently.
Abuse reporting obligations
All states have mandatory child abuse reporting laws. These laws require medical professionals (and others) to report known, and often suspected, abuse of children. Abuse includes physical, sexual, or emotional, and generally also includes neglect that is harming a child. When there is apparent sexual or physical abuse, the health care provider is obligated to report it to designated state authorities, generally child protective services. Reporting laws vary from state to state based on the relationship between the suspected abuser and the minor, the nature of the harm, and how strong the suspicion of abuse needs to be. The failure to make required reports is a crime in most states and also may result in civil liability or licensure discipline. Criminal charges seldom result from the failure to report, but in some cases the failure to report may have serious consequences for the professional.
An ObGyn example of the complexity of reporting laws, and variation from state to state, is in the area of “statutory rape” reporting. Those state laws, which define serious criminal offenses, set out the age below which an individual is not legally capable of consenting to sexual activity. It varies among states, but may be an absolute age of consent, the age differential between the parties, or some combination of age and age differential.21 The question of reporting is further complicated by the issue of when statutory rape must be reported—for example, the circumstances when the harm to the underage person is sufficient to require reporting.22
Laws are complex, as is practice navigation
It is apparent that navigating these issues makes it essential for an ObGyn practice to have clear policies and practices regarding reporting, yet the overall complexity is also why it is so difficult to develop those policies in the first place. Of course, they must be tailored to the state in which the practice resides. Once again, the need is clear for health care professionals to have an ongoing relationship with a health attorney who can help navigate ongoing questions.
CASE Adolescent seeks care without parent
A 15-year-old patient (G0) presents to the gynecology clinic requesting birth control. She reports being sexually active over the past 6 months and having several male partners over the past 2 years. She and her current male partner use condoms inconsistently. She reports being active in school sports, and her academic performance has been noteworthy. Her peers have encouraged her to seek out birth control; one of her good friends recently became pregnant and dropped out of school. She states that her best friend went to a similar clinic and received a “gynecologic encounter” that included information regarding safe sex and contraception, with no pelvic exam required for her to receive birth control pills.
The patient insists that her parents are not to know of her request for contraception due to sexual activity or that she is a patient at the clinic. The gynecologist covering the clinic is aware of the American College of Obstetricians and Gynecologists Committee on Adolescent Health Care and their many publications. The patient is counseled regarding human papillomavirus (HPV) vaccination and screened for sexually transmitted infections. In addition, the gynecologist discusses contraceptive options with the patient, ranging from oral contraceptives, vaginal rings, subdermal implants, depomedroxyprogesterone acetate, as well as intrauterine devices (IUDs). The gynecologist emphasizes safe sex and advises that her partner consider use of condoms independent of her method of birth control. The patient asks for oral contraceptives and is given information about their use and risks, and she indicates that she understands.
A few months later the patient requests an IUD, as she would like to have lighter menses and not have to remember to take a pill every day. The provider obtains informed consent for the insertion procedure; the patient signs the appropriate forms.
The IUD is inserted, with difficulty, by a resident physician in the clinic. The patient experiences severe pelvic pain during and immediately following the insertion. She is sent home and told to contact the clinic or another health care provider or proceed to the local emergency department should pain persist or if fever develops.
The patient returns 72 hours later in pain. Pelvic ultrasonography shows the IUD out of place and at risk of perforating the fundus of the uterus. Later that day the patient’s mother calls the clinic, saying that she found a statement of service with the clinic’s number on it in her daughter’s bedroom. She wants to know if her daughter is there, what is going on, and what services have been or are being provided. In passing she remarks that she has no intention of paying (or allowing her insurance to pay for) any care that was provided.
What are the provider’s obligations at this point, both medically and legally?
Medical and legal considerations
One of the most difficult and important health law questions in adolescent medicine is the ability of minors to consent to treatment and to control the health care information resulting from treatment. (“Minor” describes a child or adolescent who has not obtained the age of legal consent, generally 18 years old, to lawfully enter into a legal transaction.)
Continue to: The consent of minor patients...
The consent of minor patients
The traditional legal rule is that parents or guardians (“parent” refers to both) must consent to medical treatment for minor children. There is an exception for emergency situations but generally minors do not provide consent for medical care, a parent does.1 The parent typically is obliged to provide payment (often through insurance) for those services.
This traditional rule has some exceptions—the emergency exception already noted and the case of emancipated minors, notably an adolescent who is living almost entirely independent of her parents (for example, she is married or not relying on parents in a meaningful way). In recent times there has been increasing authority for “mature minors” to make some medical decisions.2 A mature minor is one who has sufficient understanding and judgment to appreciate the consequences, benefits, and risks of accepting proposed medical intervention.
No circumstance involving adolescent treatment has been more contentious than services related to abortion and, to a lesser degree, contraception.3 Both the law of consent to services and the rights of parents to obtain information about contraceptive and abortion services have been a matter of strong, continuing debate. The law in these areas varies greatly from state-to-state, and includes a mix of state law (statutes and court decisions) with an overlay of federal constitutional law related to reproduction-related decisions of adolescents. In addition, the law in this area of consent and information changes relatively frequently.4 Clinicians, of course, must focus on the consent laws of the state in which they practice.
STI counseling and treatment
All states permit a minor patient to consent to treatment for an STI (TABLE 1).5 A number of states expressly permit, but do not require, health care providers to inform parents of treatment when a physician determines it would be in the best interest of the minor. Thus, the clinic would not be required to provide proactively the information to our case patient’s mother (regarding any STI issues) when she called.6
Contraception
Consent for contraception is more complicated. About half the states allow minors who have reached a certain age (12, 14, or 16 years) to consent to contraception. About 20 other states allow some minors to consent to contraceptive services, but the “allowed group” may be fairly narrow (eg, be married, have a health issue, or be “mature”). In 4 states there is currently no clear legal authority to provide contraceptive services to minors, yet those states do not specifically prohibit it. The US Supreme Court has held that a state cannot completely prohibit the availability of contraception to minors.7 The reach of that decision, however, is not clear and may not extend beyond what the states currently permit.
The ability of minors to consent to contraception services does not mean that there is a right to consent to all contraceptive options. As contraception becomes more irreversible, permanent, or risky, it is more problematic. For example, consent to sterilization would not ordinarily be within a minor’s recognized ability to consent. Standard, low risk, reversible contraception generally is covered by these state laws.8
In our case here, the patient likely was able to consent to contraception—initially to the oral contraception and later to the IUD. The risks and reversibility of both are probably within her ability to consent.9,10 Of course, if the care was provided in a state that does not include the patient within the groups that can give consent to contraception, it is possible that she might not have the legal authority to consent.
Continue to: General requirements of consent...
General requirements of consent
Even when adolescent consent is permitted for treatment, including in cases of contraception, it is essential that all of the legal and ethical requirements related to informed consent are met.
1. The adolescent has the capacity to consent. This means not only that the state-mandated requirements are met (age, for example) but also that the patient can and does understand the various elements of consent, and can make a sensible, informed decision.
The bottom line is “adolescent capacity is a complex process dependent upon the development of maturity of the adolescent, degree of intervention, expected benefit of the medical procedure, and the sociocultural context surrounding the decision.”11 Other items of interest include the “evolving capacity” of the child,12 which is the concept of increasing ability of the teen to process information and provide more appropriate informed consent. Central nervous system (CNS) maturation allows the adolescent to become increasingly more capable of decision making and has awareness of consequences of such decisions. Abstract thinking capabilities is a reflection of this CNS maturing process. If this competency is not established, the adolescent patient cannot give legitimate consent.
2. The patient must be given appropriate information (be “informed”). The discussion should include information relevant to the condition being treated (and the disease process if relevant). In addition, information about the treatment or intervention proposed and its risks and alternatives must be provided to the patient and in a way that is understandable.
3. As with all patients, consent must be voluntary and free of coercion or manipulation. These elements of informed consent are expanded on by the Joint Commission, which has established a number of components of informed consent (TABLE 2).4,13
Confidentiality and release of information to parents and others
Similar to consent, parents historically have had the authority to obtain medical information about their minor children. This right generally continues today, with some limitations. The right to give consent generally carries with it the right to medical information. There are some times when parents may access medical information even if they have not given consent.
This right adds complexity to minor consent and is an important treatment issue and legal consideration because confidentiality for adolescents affects quality of care. Adolescents report that “confidentiality is an important factor in their decision to seek [medical] care.”14 Many parents are under the assumption that the health care provider will automatically inform them independent of whether or not the adolescent expressed precise instruction not to inform.15,16
Of course if a minor patient authorizes the physician to provide information to her parents, that is consent and the health care provider may then provide the information. If the patient instructs the provider to convey the information, the practitioner would ordinarily be expected to be proactive in providing the information to the parent. The issue of “voluntariness” of the waiver of confidentiality can be a question, and the physician may discuss that question with the patient. Ordinarily, however, once a minor has authorized disclosure to the parent, the clinician has the authority to disclose the information to the parent, but not to others.
All of the usual considerations of confidentiality in health care apply to adolescent ObGyn services and care. This includes the general obligation not to disclose information without consent and to ensure that health care information is protected from accidental release as required by the Health Insurance Portability and Accountability Act (HIPAA) and other health information privacy laws.17
It is important to emphasize that the issues of consent to abortion are much different than those for contraception and sexually transmitted infections. As our case presentation does not deal with abortion, we will address this complex but important discussion in the future--as there are an estimated 90,000 abortions in adolescent girls annually.1
Given that abortion consent and notification laws are often complex, any physician providing abortion services to any minor should have sound legal advice on the requirements of the pertinent state law. In earlier publications of this section in OBG Management we have discussed the importance of practitioners having an ongoing relationship with a health law attorney. We make this point again, as this person can provide advice on consent and the rights of parents to have information about their minor children.
Reference
- Henshaw SK. U.S. teenage pregnancy statistics with comparative statistics for women age 20-24. New York, New York: Alan Guttmacher Institute; May 2003.
Continue to: How and when to protect minor confidentiality...
How and when to protect minor confidentiality
A clinician cannot assure minors of absolute confidentiality and should not agree to do so or imply that they are doing so.18 In our hypothetical case, when the patient told the physician that her parents were not to know of any of her treatment or communications, the provider should not have acquiesced by silence. He/she might have responded along these lines: “I have a strong commitment to confidentiality of your information, and we take many steps to protect that information. The law also allows some special protection of health care information. Despite the commitment to privacy, there are circumstances in which the law requires disclosure of information—and that might even be to parents. In addition, if you want any of your care covered by insurance, we would have to disclose that. While I expect that we can do as you ask about maintaining your confidentiality, no health care provider can absolutely guarantee it.”
Proactive vs reactive disclosure. There is “proactive” disclosure of information and “reactive” disclosure. Proactive is when the provider (without being asked) contacts a parent or others and provides information. Some states require proactive information about specific kinds of treatment (especially abortion services). For the most part, in states where a minor can legally consent to treatment, health care providers are not required to proactively disclose information.19
Clinicians may be required to respond to parental requests for information, which is reactive disclosure and is reflected in our case presentation. Even in such circumstances, however, the individual providing care may seek to avoid disclosure. In many states, the law would not require the release of this information (but would permit it if it is in the best interest of the patient). In addition, there are practical ways of avoiding the release of information. For example, the health care provider might acknowledge the interest and desire of the parent to have the information, but might humbly explain that in the experience of many clinicians protecting the confidentiality of patients is very important to successful treatment and it is the policy of the office/clinic not to breach the expectation of patient confidentiality except where that is clearly in the best interest of the patient or required by law.
In response to the likely question, “Well, isn’t that required by law?” the clinician can honestly reply, “I don’t know. There are many complex factors in the law regarding disclosure of medical information and as I am not an attorney I do not know how they all apply in this instance.” In some cases the parent may push the matter or take some kind of legal action. It is in this type of situation that an attorney familiar with health law and the clinician’s practice can be invaluable.
When parents are involved in the minor’s treatment (bringing the patient to the office/clinic, for example), there is an opportunity for an understanding, or agreement, among the patient, provider, and parent about what information the parent will receive. Ordinarily the agreement should not create the expectation of detailed information for the parent. Perhaps, for example, the physician will provide information only when he or she believes that doing so will be in the best interest of the patient. Even with parental agreement, complete confidentiality cannot be assured for minor patients. There may, for example, be another parent who will not feel bound by the established understanding, and the law requires some disclosures (in the case of child abuse or a court order).20
Continue to: Accidental disclosure...
Accidental disclosure. Health care providers also should make sure that office procedures do not unnecessarily or accidentally disclose information about patients. For example, routinely gathering information about insurance coverage may well trigger the release of information to the policy holder (often a parent). Thus, there should be clear understandings about billing, insurance, and related issues before information is divulged by the patient. This should be part of the process of obtaining informed consent to treatment. It should be up front and honest. Developing a clear understanding of the legal requirements of the state is essential, so that assurance of confidentiality is on legal, solid ground.
As the pediatric and adolescent segment of gynecologic care continues to evolve, it is noteworthy that the American Board of Obstetrics and Gynecology recently has established a "Focused Practice" designation in pediatric adolescent gynecology. This allows ObGyns to have an ongoing level of professional education in this specialized area. Additional information can be obtained at www.abog.org or [email protected].
More resources for adolescent contraceptive care include:
- The American College of Obstetricians and Gynecologists (ACOG) "Birth Control (Especially for Teens)" frequently asked questions information series (https://www.acog.org/Patients/FAQs/Birth-Control-Especially-for-Teens)
- ACOG's Adolescent Healthcare Committee Opinions address adolescent pregnancy, contraception, and sexual activity (https://www.acog.org/-/media/List-of-Titles/COListOfTitles.pdf)
- ACOG statement on teen pregnancy and contraception, April 7, 2015 (https://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Teen-Pregnancy-and-Contraception?IsMobileSet=false)
- North American Society for Pediatric and Adolescent Gynecology resources for patients (https://www.naspag.org/page/patienttools)
- Society for Adolescent Health and Medicine statement regarding contraceptive access policies (https://www.adolescenthealth.org)
- The Guttmacher Institute's overview of state laws relevant to minor consent, as of January 1, 2019 (https://www.guttmacher.org/state-policy/explore/overview-minors-consent-law). It is updated frequently.
Abuse reporting obligations
All states have mandatory child abuse reporting laws. These laws require medical professionals (and others) to report known, and often suspected, abuse of children. Abuse includes physical, sexual, or emotional, and generally also includes neglect that is harming a child. When there is apparent sexual or physical abuse, the health care provider is obligated to report it to designated state authorities, generally child protective services. Reporting laws vary from state to state based on the relationship between the suspected abuser and the minor, the nature of the harm, and how strong the suspicion of abuse needs to be. The failure to make required reports is a crime in most states and also may result in civil liability or licensure discipline. Criminal charges seldom result from the failure to report, but in some cases the failure to report may have serious consequences for the professional.
An ObGyn example of the complexity of reporting laws, and variation from state to state, is in the area of “statutory rape” reporting. Those state laws, which define serious criminal offenses, set out the age below which an individual is not legally capable of consenting to sexual activity. It varies among states, but may be an absolute age of consent, the age differential between the parties, or some combination of age and age differential.21 The question of reporting is further complicated by the issue of when statutory rape must be reported—for example, the circumstances when the harm to the underage person is sufficient to require reporting.22
Laws are complex, as is practice navigation
It is apparent that navigating these issues makes it essential for an ObGyn practice to have clear policies and practices regarding reporting, yet the overall complexity is also why it is so difficult to develop those policies in the first place. Of course, they must be tailored to the state in which the practice resides. Once again, the need is clear for health care professionals to have an ongoing relationship with a health attorney who can help navigate ongoing questions.
- Benjamin L, Ishimine P, Joseph M, et al. Evaluation and treatment of minors. Ann Emerg Med. 2018;71(2):225-232.
- Coleman D, Rosoff P. The legal authority of mature minors to consent to general medical treatment. Pediatrics. 2013;13:786-793.
- American College of Obstetricians and Gynecologists. Committee Opinion No. 699. Adolescent pregnancy, contraception, and sexual activity. Obstet Gynecol. 2017;129:e142-e149.
- Tillett J. Adolescents and informed consent. J Perinat Neonat Nurs. 2005;19:112-121.
- An overview of minor's consent law. Guttmacher Institute's website. https://www.guttmacher.org/state-policy/explore/overview-minors-consent-law. Accessed February 14, 2019.
- Chelmow D, Karjane N, Ricciotti HA, et al, eds. A 16-year-old adolescent requesting confidential treatment for chlamydia exposure (understanding state laws regarding minors and resources). Office Gynecology: A Case-Based Approach. Cambridge, United Kingdom: Cambridge University Press; January 31, 2019:39.
- Carey v Population Services, 431 US 678 (1977).
- Williams RL, Meredith AH, Ott MA. Expanding adolescent access to hormonal contraception: an update on over-the-counter, pharmacist prescribing, and web-based telehealth approaches. Curr Opin Obstet Gynecol. 2018;30:458-464.
- McClellan K, Temples H, Miller L. The latest in teen pregnancy prevention: long-acting reversible contraception. J Pediatr Health Care. 2018;32:e91-e97.
- Behmer Hansen RT, Arora KS. Consenting to invasive contraceptives: an ethical analysis of adolescent decision-making authority for long-acting reversible contraception. J Med Ethics. 2018;44:585-588.
- Robertson D. Opinions in pediatric and adolescent gynecology. J Pediatr Adolesc Gynecol. 2008:21:47-51.
- Lansdown G. The evolving capacities of the child. Florence, Italy: UNICEF Innocenti Research Centre, Innocenti Insight; 2005. https://www.unicef-irc.org/publications/384-the-evolving-capacities-of-the-child.html. Accessed February 15, 2019.
- Clapp JT, Fleisher LA. What is the realistic scope of informed consent? Jt Comm J Qual Patient Saf. 2018;44(6):341-342.
- Berlan E, Bravender T. Confidentiality, consent and caring for the adolescent. Curr Opin Pediatr. 2009;21:450-456.
- Schantz K. Who Needs to Know? Confidentiality in Adolescent Sexual Health Care. Act for Youth website. http://www.actforyouth.net/resources/rf/rf_confidentiality_1118.pdf. Accessed February 14, 2019.
- Lynn A, Kodish E, Lazebnik R, et al. Understanding confidentiality: perspectives of African American adolescents and their parents. J Adolesc Health. 2006;39:261-265.
- English A, Ford CA. The HIPAA privacy rule and adolescents: legal questions and clinical challenges. Perspect Sex Reprod Health. 2004;36:80-86.
- Schapiro NA, Mejia J. Adolescent confidentiality and women's health: history, rationale, and current threats. Nurs Clin North Am. 2018;53:145-156.
- Scott NL, Alderman EM, 2018. Case of a girl with a secret. In: Adolescent Gynecology: A Clinical Casebook. New York, New York: Springer International; 2017:3-11.
- Cullitan CM. Please don't tell my mom--a minor's right to informational privacy. JL & Educ. 2011;40:417-460.
- Bierie DM, Budd KM. Romeo, Juliet, and statutory rape. Sex Abuse. 2018;30:296-321.
- Mathews B. A taxonomy of duties to report child sexual abuse: legal developments offer new ways to facilitate disclosure. Child Abuse Negl. 2019;88:337-347.
- Benjamin L, Ishimine P, Joseph M, et al. Evaluation and treatment of minors. Ann Emerg Med. 2018;71(2):225-232.
- Coleman D, Rosoff P. The legal authority of mature minors to consent to general medical treatment. Pediatrics. 2013;13:786-793.
- American College of Obstetricians and Gynecologists. Committee Opinion No. 699. Adolescent pregnancy, contraception, and sexual activity. Obstet Gynecol. 2017;129:e142-e149.
- Tillett J. Adolescents and informed consent. J Perinat Neonat Nurs. 2005;19:112-121.
- An overview of minor's consent law. Guttmacher Institute's website. https://www.guttmacher.org/state-policy/explore/overview-minors-consent-law. Accessed February 14, 2019.
- Chelmow D, Karjane N, Ricciotti HA, et al, eds. A 16-year-old adolescent requesting confidential treatment for chlamydia exposure (understanding state laws regarding minors and resources). Office Gynecology: A Case-Based Approach. Cambridge, United Kingdom: Cambridge University Press; January 31, 2019:39.
- Carey v Population Services, 431 US 678 (1977).
- Williams RL, Meredith AH, Ott MA. Expanding adolescent access to hormonal contraception: an update on over-the-counter, pharmacist prescribing, and web-based telehealth approaches. Curr Opin Obstet Gynecol. 2018;30:458-464.
- McClellan K, Temples H, Miller L. The latest in teen pregnancy prevention: long-acting reversible contraception. J Pediatr Health Care. 2018;32:e91-e97.
- Behmer Hansen RT, Arora KS. Consenting to invasive contraceptives: an ethical analysis of adolescent decision-making authority for long-acting reversible contraception. J Med Ethics. 2018;44:585-588.
- Robertson D. Opinions in pediatric and adolescent gynecology. J Pediatr Adolesc Gynecol. 2008:21:47-51.
- Lansdown G. The evolving capacities of the child. Florence, Italy: UNICEF Innocenti Research Centre, Innocenti Insight; 2005. https://www.unicef-irc.org/publications/384-the-evolving-capacities-of-the-child.html. Accessed February 15, 2019.
- Clapp JT, Fleisher LA. What is the realistic scope of informed consent? Jt Comm J Qual Patient Saf. 2018;44(6):341-342.
- Berlan E, Bravender T. Confidentiality, consent and caring for the adolescent. Curr Opin Pediatr. 2009;21:450-456.
- Schantz K. Who Needs to Know? Confidentiality in Adolescent Sexual Health Care. Act for Youth website. http://www.actforyouth.net/resources/rf/rf_confidentiality_1118.pdf. Accessed February 14, 2019.
- Lynn A, Kodish E, Lazebnik R, et al. Understanding confidentiality: perspectives of African American adolescents and their parents. J Adolesc Health. 2006;39:261-265.
- English A, Ford CA. The HIPAA privacy rule and adolescents: legal questions and clinical challenges. Perspect Sex Reprod Health. 2004;36:80-86.
- Schapiro NA, Mejia J. Adolescent confidentiality and women's health: history, rationale, and current threats. Nurs Clin North Am. 2018;53:145-156.
- Scott NL, Alderman EM, 2018. Case of a girl with a secret. In: Adolescent Gynecology: A Clinical Casebook. New York, New York: Springer International; 2017:3-11.
- Cullitan CM. Please don't tell my mom--a minor's right to informational privacy. JL & Educ. 2011;40:417-460.
- Bierie DM, Budd KM. Romeo, Juliet, and statutory rape. Sex Abuse. 2018;30:296-321.
- Mathews B. A taxonomy of duties to report child sexual abuse: legal developments offer new ways to facilitate disclosure. Child Abuse Negl. 2019;88:337-347.
Cost-conscious minimally invasive hysterectomy: A case illustration
CASE Cost-conscious benign laparoscopic hysterectomy
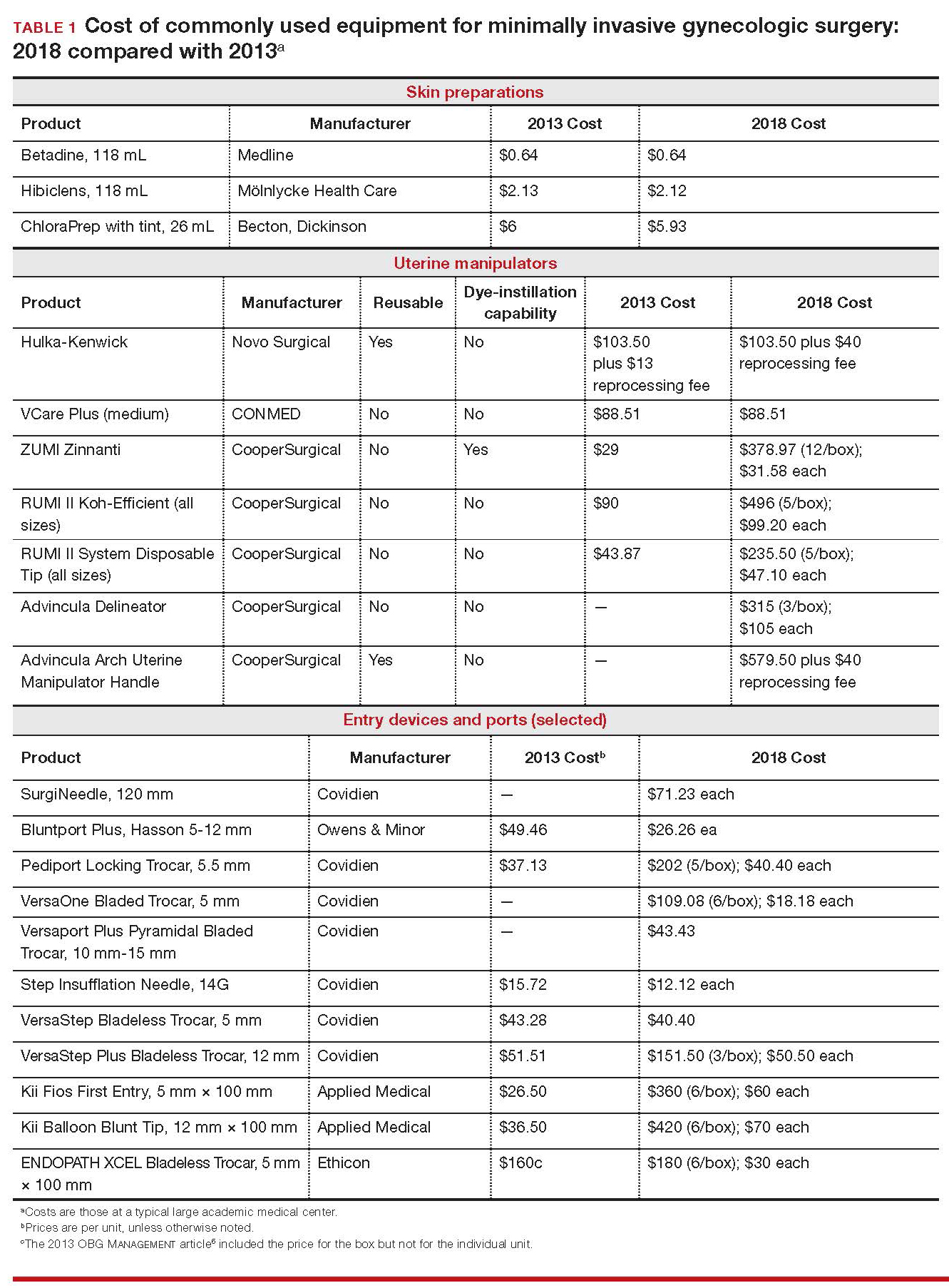
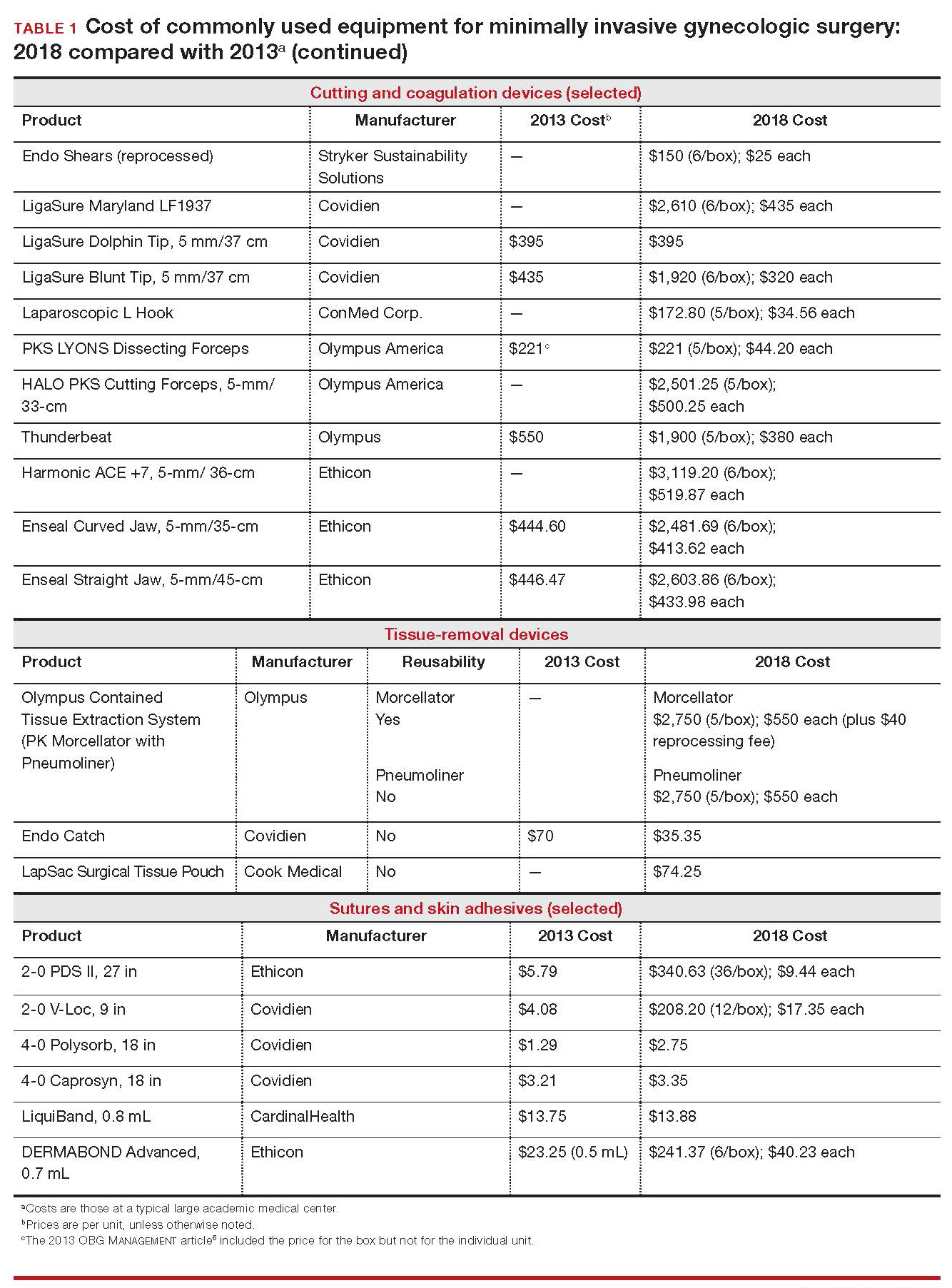
A 43-year-old woman undergoes laparoscopic hysterectomy for treatment of presumed benign uterine fibroids and menorrhagia. Once she is prepped with ChloraPrep with tint, a RUMI II uterine manipulator is placed. Laparoscopic ports include a Kii Balloon Blunt Tip system, a Versaport Plus Pyramidal Bladed Trocar, and 2 Kii Fios First Entry trocars.
The surgeon uses the Harmonic ACE +7 device (a purely ultrasonic device) to perform most of the procedure. The uterus is morcellated and removed using the US Food and Drug Administration (FDA)-approved Olympus Contained Tissue Extraction System, and the vaginal cuff is closed using a series of 2-0 PDS II sutures. Skin incisions are closed using Dermabond skin adhesive.
Total cost of the products used in this case: $1,592.40. Could different product choices have reduced this figure?
Health-care costs continue to rise faster than inflation: Total health-care expenditures account for approximately 18% of gross domestic product in the United States. Physicians therefore face increasing pressure to take cost into account in their care of patients.1 Cost-effectiveness and outcome quality continue to increase in importance as measures in many clinical trials that compare standard and alternative therapies. And women’s health—specifically, minimally invasive gynecologic surgery—invites such comparisons.
Overall, conventional laparoscopic gynecologic procedures tend to cost less than laparotomy, a consequence of shorter hospital stays, faster recovery, and fewer complications.2-5 What is not fully appreciated, however, is how choice of laparoscopic instrumentation and associated products affects surgical costs. In this article, which revisits and updates a 2013 OBG Management examination of cost-consciousness in the selection of equipment and supplies for minimally invasive gynecologic surgery,6 we review these costs in 2018. Our goal is to raise awareness of the role of cost in care among minimally invasive gynecologic surgeons.
In the sections that follow, we highlight several aspects of laparoscopic gynecologic surgery that can affect your selection of instruments and products, describing differences in cost as well as some distinctive characteristics of products. Note that our comparisons focus solely on cost—not on ease of utility, effectiveness, surgical technique, risk of complications, or any other assessment. Note also that numerous other instruments and devices are commercially available besides those we list.
Importantly, 2013 and 2018 costs are included in TABLE 1. Unless otherwise noted, costs are per unit. Changes in manufacturers and material costs and technologic advances have contributed to some, but not all, of the changes in cost between 2013 and 2018.
Continue to: Variables to keep in mind
Variables to keep in mind
Even when taking cost into consideration, tailor your selection of instruments and supplies to your capabilities and comfort, as well as to the particular characteristics of the patient and the planned procedure. Also, remember that your institution might have arrangements with companies that supply minimally invasive instruments, and that such arrangements might limit your options, to some degree. Last, be aware that reprocessed ports and instruments are now available at a reduced cost. In short, we believe that it is crucial for surgeons to be cognizant of all products available to them prior to attending a surgical case.
Skin preparation and other preop considerations
Multiple preoperative skin preparations are available (TABLE 1). Traditionally, a povidone–iodine topical antiseptic, such as Betadine, has been used for skin and vaginal preparation prior to gynecologic surgery. Hibiclens and ChloraPrep are different combinations of chlorhexidine gluconate and isopropyl alcohol that act as broad-spectrum antiseptics.
ChloraPrep is applied with a wand-like applicator and contains a much higher concentration of isopropyl alcohol than Hibiclens (70% and 4%, respectively), rendering it more flammable. It also requires longer drying time before surgery can be started. Clear and tinted ChloraPrep formulations are available.
Continue to: Uterine manipulators
Uterine manipulators
Cannulation of the cervical canal allows for uterine manipulation, increasing intraoperative traction and exposure as well as visualization of the adnexae and peritoneal surfaces.
The Hulka-Kenwick is a reusable uterine manipulator that is fairly standard and easy to apply. Specialized, single-use manipulators also are available, including the Advincula Delineator and VCare Plus uterine manipulator/elevator. The VCare Plus manipulator consists of 2 opposing cups: one cup (available in 4 sizes, small to extra-large) fits around the cervix and defines the site for colpotomy; the other helps maintain pneumoperitoneum once a colpotomy is created.
The ZUMI (Zinnanti Uterine Manipulator Injector) is a rigid, curved shaft with an intrauterine balloon to help prevent expulsion. It also has an integrated injection channel to allow for intraoperative chromotubation.
The RUMI II System fits individual patient anatomy with various tip lengths and colpotomy cup sizes. The Advincula Arch Uterine Manipulator Handle is a reusable alternative to the articulating RUMI II and works with the RUMI II System Disposable Tip (TABLE 1).
Continue to: Entry style and ports
Entry style and ports
The peritoneal cavity can be entered using either a closed (Veress needle) or open (Hasson) technique.7,8 Closed entry might allow for quicker access to the peritoneal cavity. A 2015 Cochrane review of 46 randomized, controlled trials of 7,389 patients undergoing laparoscopy compared outcomes between laparoscopic entry techniques and found no difference in major vascular or visceral injury between closed and open techniques at the umbilicus.9 However, open entry was associated with a greater likelihood of successful entry into the peritoneal cavity.9
Left upper-quadrant (Palmer’s point) entry is another option when adhesions are anticipated or abnormal anatomy is encountered at the umbilicus.
In general, complications related to laparoscopic entry are rare in gynecologic surgery, ranging from 0.18% to 0.5% of cases in studies.8,10,11 A minimally invasive surgeon might prefer one entry technique over another but should be able to perform both methods competently and recognize when a particular technique is warranted.
--
Choosing a port
Laparoscopic ports usually range from 5 mm to 12 mm and can be fixed or variable in size.
The primary port, usually placed through the umbilicus, can be a standard, blunt, 10-mm (Bluntport Plus Hasson) port, or it can be specialized to ease entry of the port or stabilize the port once it is introduced through the skin incision.
Optical trocars have a transparent tip that allows the surgeon to visualize the abdominal wall entry layer by layer using a 0° laparoscope, sometimes after pneumoperitoneum is created with a Veress needle. Other specialized ports include those that have balloons or foam collars, or both, to secure the port without traditional stay sutures on the fascia and to minimize leakage of pneumoperitoneum.
Continue to: Accessory ports
Accessory ports
When choosing an accessory port type and size, it is important to anticipate which instruments and devices, such as an Endo Catch bag, suture, or needle, will need to pass through it. Also, know whether 5-mm and 10-mm laparoscopes are available, and anticipate whether a second port with insufflation capabilities will be required.
The Pediport Locking Trocar is a user-friendly, 5-mm bladed port that deploys a mushroom-shaped stabilizer to prevent dislodgement. The Versaport bladed trocar has a spring-loaded entry shield, which slides over the blade to protect it once the peritoneal cavity is entered.
VersaStep Bladeless Trocars are introduced after a Step Insufflation Needle has been inserted. These trocars create a smaller fascial defect than conventional bladed trocars for an equivalent cannula size (TABLE 1).
Cutting and coagulating
Both monopolar and bipolar electrosurgical techniques are commonly employed in gynecologic laparoscopy. A wide variety of disposable and reusable instruments are available for monopolar energy, such as scissors, a hook, and a spatula.
Bipolar devices also can be disposable or reusable. Although bipolar electrosurgery minimizes injury to surrounding tissues by containing the current within the jaws of the forceps, it cannot cut or seal large vessels. As a result, several advanced bipolar devices with sealing and transecting capabilities have emerged (the LigaSure line of devices, Enseal). Ultrasonic devices, such as the Harmonic ACE, also can coagulate and cut at lower temperatures by converting electrical energy to mechanical energy (TABLE 1).
Continue to: Suture material
Suture material
Aspects of minimally invasive gynecologic surgery that require the use of suture include, but are not limited to, closure of the vaginal cuff, oophoropexy, and reapproximation of the ovarian cortex after cystectomy. Synthetic and delayed absorbable sutures, such as PDS II, are used frequently. The barbed suture also has gained popularity because it anchors to tissue without the need for intracorporeal or extracorporeal knots (TABLE 1).
Tissue removal
Adnexae and pathologic tissue, such as dermoid cysts, can be removed intact from the peritoneal cavity using an Endo Catch Single Use Specimen Pouch, a polyurethane sac. Careful use, with placement of the ovary with the cyst into the pouch prior to cystectomy, can contain or prevent spillage outside the bag.
A large uterus that cannot be extracted through a colpotomy can be manually morcellated. Appropriate candidates can undergo power morcellation using an FDA-approved device. (TABLE 1), allowing for the removal of smaller pieces through a small laparoscopic incision or the colpotomy.
Issues surrounding morcellation continue to require that gynecologic surgeons understand FDA recommendations. In 2014, the FDA issued a safety communication that morcellation is “contraindicated in gynecologic surgery if tissue is known or suspected to be malignant; it is contraindicated for uterine tissue removal with presumed benign fibroids in perimenopausal women.”12 A black-box warning was issued that uterine tissue might contain unsuspected cancer.
A task force created by AAGL addressed key issues in this controversy.
AAGL then provided guidelines related to morcellation13:
- Do not use morcellate in the setting of known malignancy.
- Provide appropriate preoperative evaluation with up-to-date Pap smear screening and image analysis.
- Increasing age significantly increases the risk of leiomyosarcoma, especially in a postmenopausal woman.
- Fibroid growth is not a reliable sign of malignancy.
- Do not use a morcellator if the patient is at high risk for malignancy.
- If leiomyosarcoma is the presumed pathology, await the final pathology report before proceeding with hysterectomy.
- Concomitant use of a bag might mitigate the risk of tissue spread.
- Obtain informed consent before proceeding with morcellation.
Continue to: Skin closure
Skin closure
Final subcuticular closure can be accomplished using sutures or skin adhesive. Sutures can be synthetic, absorbable monofilament (Caprosyn), or synthetic, absorbable, braided multifilament (Polysorb).
Skin adhesive closes incisions quickly, avoids inflammation related to foreign bodies, and can ease patients’ concerns that sometimes arise when absorbable suture persists postoperatively (TABLE 1).
The impact of physician experience
Physician experience has been shown to reduce cost while maintaining quality of care.14 That was the conclusion of researchers who undertook a retrospective study, addressing cost and clinical outcomes, of senior and junior attending physicians who performed laparoscopic-assisted vaginal hysterectomy on 120 patients. Studies such as these often lead to clinical pathways to facilitate cost-effective quality care.
--
CASE Same outcome at lower cost
The hypothetical 43-year-old patient in the opening case undergoes laparoscopic hysterectomy for treatment of uterine fibroids and menorrhagia. In this scenario, however, the surgeon makes the following product choices:
- The patient is prepped with Hibiclens.
- A VCare Plus uterine manipulator is placed.
- Laparoscopic ports include a VersaStep Plus Bladeless Trocar with Step Insufflation Needle; Versaport Plus Pyramidal Bladed Trocar; and 2 VersaOne Bladed trocars.
- The surgeon uses the PKS LYONS Dissecting Forceps and reprocessed Endo Shears to perform the hysterectomy.
- The uterus is enclosed in an Endo Catch bag and removed through the minilaparotomy site.
- The vaginal cuff is closed using 2-0 V-Loc barbed suture. Skin incisions are closed with 4-0 Polysorb, a polyglycolic acid absorbable suture.
The cost of this set of products? $360.44 or, roughly, $1,231.96 less than the set-up described in the case at the beginning of this article (TABLE 2).
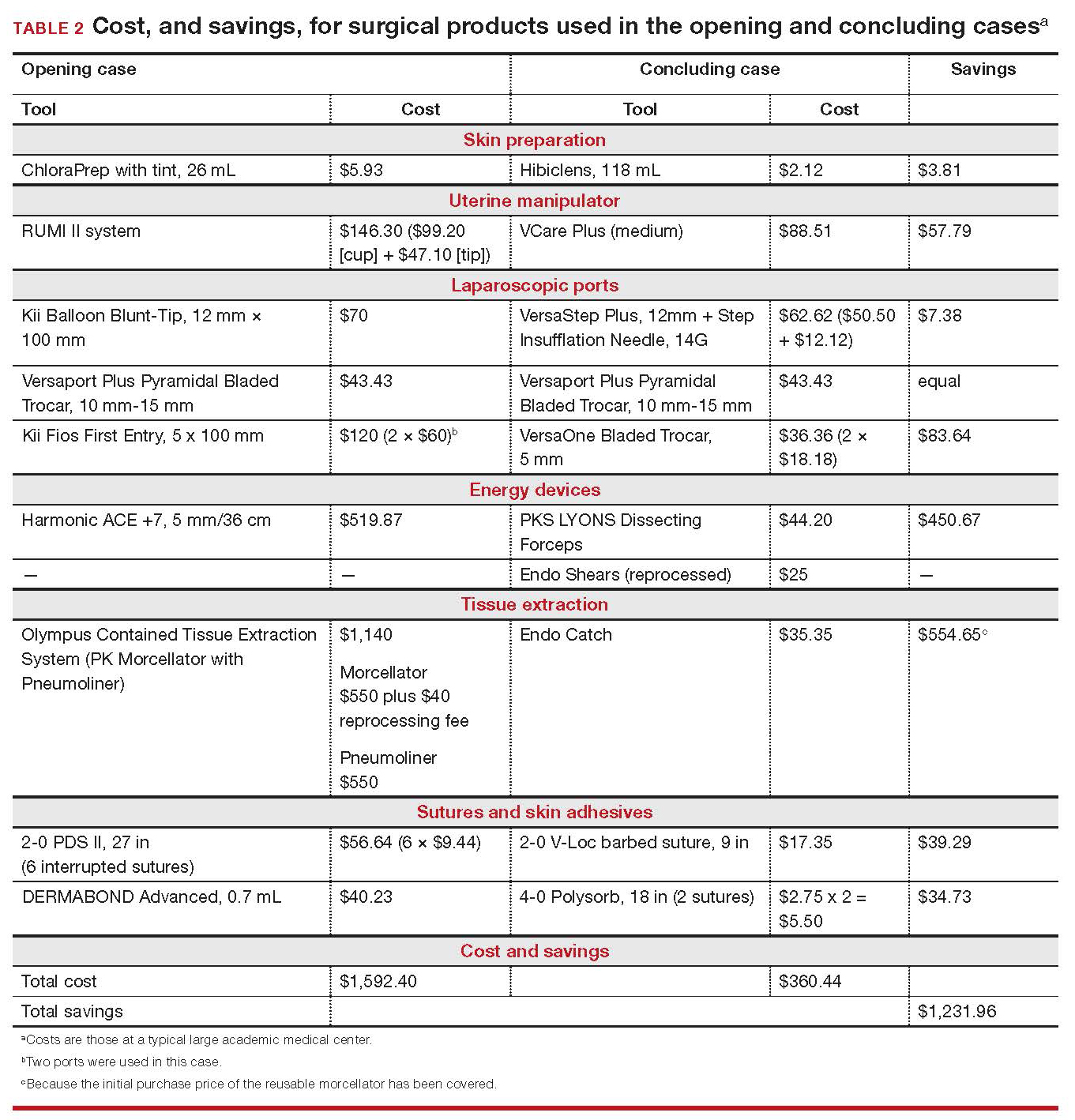
Continue to: Summing up
Summing up
Here are key points to take away from this analysis and discussion:
- As third-party payers and hospitals continue to evaluate surgeons individually and compare procedures from surgeon to surgeon, reimbursement might be stratified—thereby favoring physicians who demonstrate both quality outcomes and cost containment.
- There are many ways a minimally invasive surgeon can implement cost-conscious choices that have little or no impact on the quality of outcome.
- Surgeons who are familiar with surgical instruments and models available at their institution are better prepared to make wise cost-conscious decisions. (See “Caregivers should keep cost in mind: Here’s why,” in the Web version of this article at https://www.mdedge.com/obgyn.)
- Cost is not the only indicator of value: The surgeon must know how to apply tools correctly and be familiar with their limitations, and should choose instruments and products for their safety and ease of use. More often than not, a surgeon’s training and personal experience define—and sometimes restrict—the choice of devices.
- Last, it makes sense to have instruments and devices readily available in the operating room at the start of a case, to avoid unnecessary surgical delays. However, we recommend that you refrain from opening these tools until they are required intraoperatively. It is possible that the case will require conversion to laparotomy or that, after direct visualization of the pathology, different ports or instruments are required.
Acknowledgments
The authors would like to thank Meredith Snook, MD, who was coauthor of the original 2013 article6 and Kathleen Riordan, BSN, RN, for assistance in gathering specific cost-related information for this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Centers for Medicare & Medicaid Services. National health expenditure projections 2017-2026: Forecast summary. www.cms.gov/Research-Statistics-Data-and-Systems /Statistics-Trends-and-Reports/NationalHealthExpendData /Downloads/ForecastSummary.pdf. Accessed November 3, 2018.
- Vilos GA, Alshimmiri MM. Cost-benefit analysis of laparoscopic versus laparotomy salpingo-oophorectomy for benign tubo-ovarian disease. J Am Assoc Gynecol Laparosc. 1995;2(3):299-303.
- Gray DT, Thorburn J, Lundor P, et al. A cost-effectiveness study of a randomised trial of laparoscopy versus laparotomy for ectopic pregnancy. Lancet. 1995;345(8958):1139-1143.
- Chapron C, Fauconnier A, Goffinet F, et al. Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynaecologic pathology. Results of a metaanalysis. Hum Reprod. 2002;17(5):1334-1342.
- Benezra V, Verma U, Whitted RW. Comparison of laparoscopy versus laparotomy for the surgical treatment of ovarian dermoid cysts. Obstet Gynecol Surv. 2006;61(1): 20-21.
- Sanfilippo JS, Snook ML. Cost-conscious choices for minimally invasive gynecologic surgery. OBG Manag. 2013;25(11):40-41,44,46-48,72.
- Hasson HM. A modified instrument and method for laparoscopy. Am J Obstet Gynecol. 1971;110(6):886-887.
- Ott J, Jaeger-Lansky A, Poschalko G, et al. Entry techniques in gynecologic laparoscopy—a review. Gynecol Surg. 2012;9(2):139-146.
- Ahmad G, Gent D, Henderson D, et al. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2015;8:CD006583.
- Hasson HM, Rotman C, Rana N, et al. Open laparoscopy: 29-year experience. Obstet Gynecol. 2000;96(5 Pt 1):763-766.
- Schäfer M, Lauper M, Krähenbühl L. Trocar and Veress needle injuries during laparoscopy. Surg Endosc. 2001;15(3):275- 280.
- Immediately in effect guidance document: product labeling for laparoscopic power morcellators. Rockville, MD: US Department of Health and Human Services, Food and Drug Administration Center for Devices and Radiological Health; November 25, 2014. www.fda.gov/downloads /MedicalDevices/DeviceRegulationandGuidance /GuidanceDocuments/UCM424123.pdf. Accessed November 3, 2018.
- Tissue Extraction Task Force Members. Morcellation during uterine tissue extraction: an update. J Minim Invasive Gynecol. 2018;25(4):543-550.
- Chang WC, Li TC, Lin CC. The effect of physician experience on costs and clinical outcomes of laparoscopic-assisted vaginal hysterectomy: a multivariate analysis. J Am Assoc Gynecol Laparosc. 2003;10(3):356-359.
CASE Cost-conscious benign laparoscopic hysterectomy
A 43-year-old woman undergoes laparoscopic hysterectomy for treatment of presumed benign uterine fibroids and menorrhagia. Once she is prepped with ChloraPrep with tint, a RUMI II uterine manipulator is placed. Laparoscopic ports include a Kii Balloon Blunt Tip system, a Versaport Plus Pyramidal Bladed Trocar, and 2 Kii Fios First Entry trocars.
The surgeon uses the Harmonic ACE +7 device (a purely ultrasonic device) to perform most of the procedure. The uterus is morcellated and removed using the US Food and Drug Administration (FDA)-approved Olympus Contained Tissue Extraction System, and the vaginal cuff is closed using a series of 2-0 PDS II sutures. Skin incisions are closed using Dermabond skin adhesive.
Total cost of the products used in this case: $1,592.40. Could different product choices have reduced this figure?
Health-care costs continue to rise faster than inflation: Total health-care expenditures account for approximately 18% of gross domestic product in the United States. Physicians therefore face increasing pressure to take cost into account in their care of patients.1 Cost-effectiveness and outcome quality continue to increase in importance as measures in many clinical trials that compare standard and alternative therapies. And women’s health—specifically, minimally invasive gynecologic surgery—invites such comparisons.
Overall, conventional laparoscopic gynecologic procedures tend to cost less than laparotomy, a consequence of shorter hospital stays, faster recovery, and fewer complications.2-5 What is not fully appreciated, however, is how choice of laparoscopic instrumentation and associated products affects surgical costs. In this article, which revisits and updates a 2013 OBG Management examination of cost-consciousness in the selection of equipment and supplies for minimally invasive gynecologic surgery,6 we review these costs in 2018. Our goal is to raise awareness of the role of cost in care among minimally invasive gynecologic surgeons.
In the sections that follow, we highlight several aspects of laparoscopic gynecologic surgery that can affect your selection of instruments and products, describing differences in cost as well as some distinctive characteristics of products. Note that our comparisons focus solely on cost—not on ease of utility, effectiveness, surgical technique, risk of complications, or any other assessment. Note also that numerous other instruments and devices are commercially available besides those we list.
Importantly, 2013 and 2018 costs are included in TABLE 1. Unless otherwise noted, costs are per unit. Changes in manufacturers and material costs and technologic advances have contributed to some, but not all, of the changes in cost between 2013 and 2018.
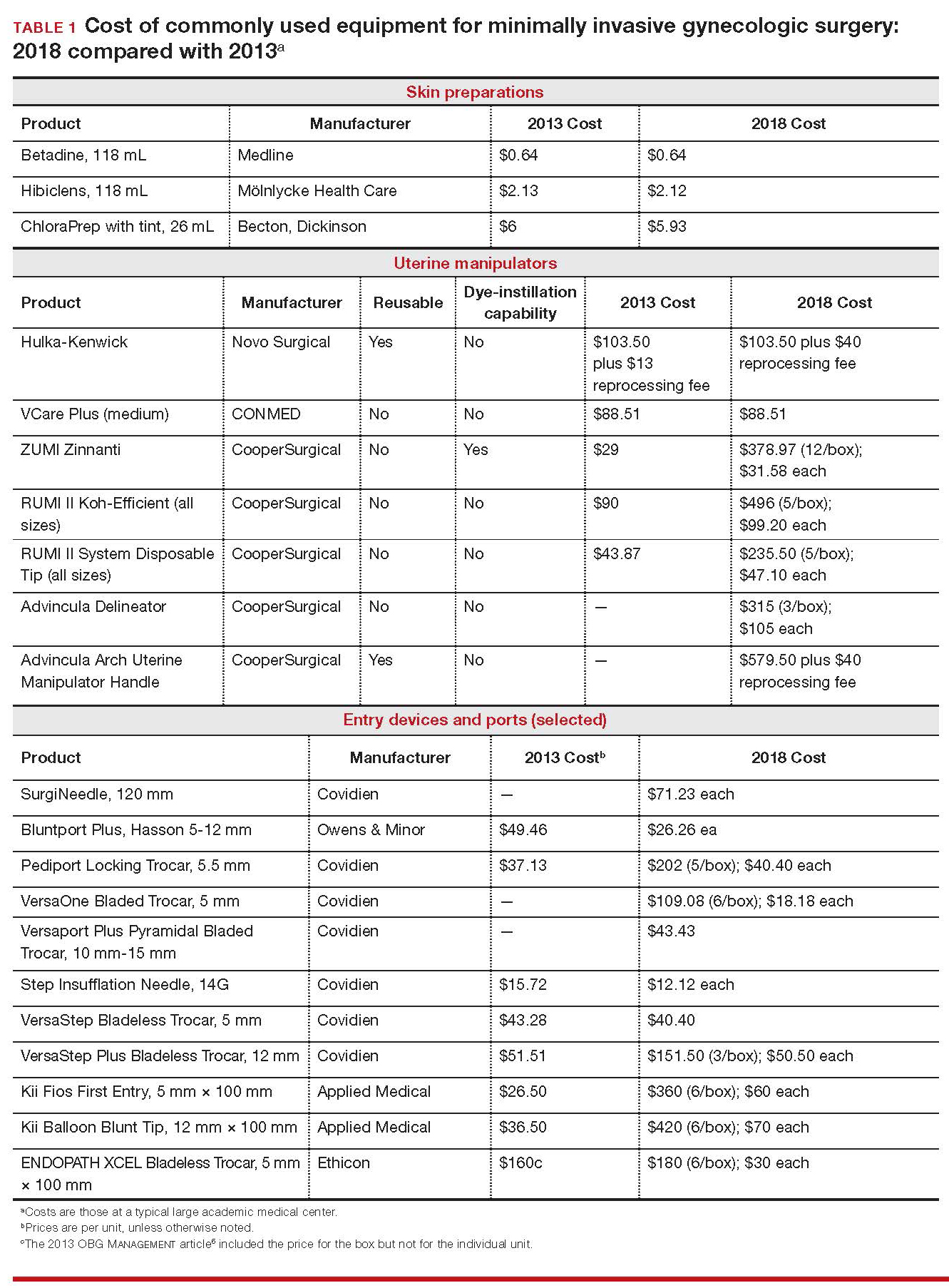
Continue to: Variables to keep in mind
Variables to keep in mind
Even when taking cost into consideration, tailor your selection of instruments and supplies to your capabilities and comfort, as well as to the particular characteristics of the patient and the planned procedure. Also, remember that your institution might have arrangements with companies that supply minimally invasive instruments, and that such arrangements might limit your options, to some degree. Last, be aware that reprocessed ports and instruments are now available at a reduced cost. In short, we believe that it is crucial for surgeons to be cognizant of all products available to them prior to attending a surgical case.
Skin preparation and other preop considerations
Multiple preoperative skin preparations are available (TABLE 1). Traditionally, a povidone–iodine topical antiseptic, such as Betadine, has been used for skin and vaginal preparation prior to gynecologic surgery. Hibiclens and ChloraPrep are different combinations of chlorhexidine gluconate and isopropyl alcohol that act as broad-spectrum antiseptics.
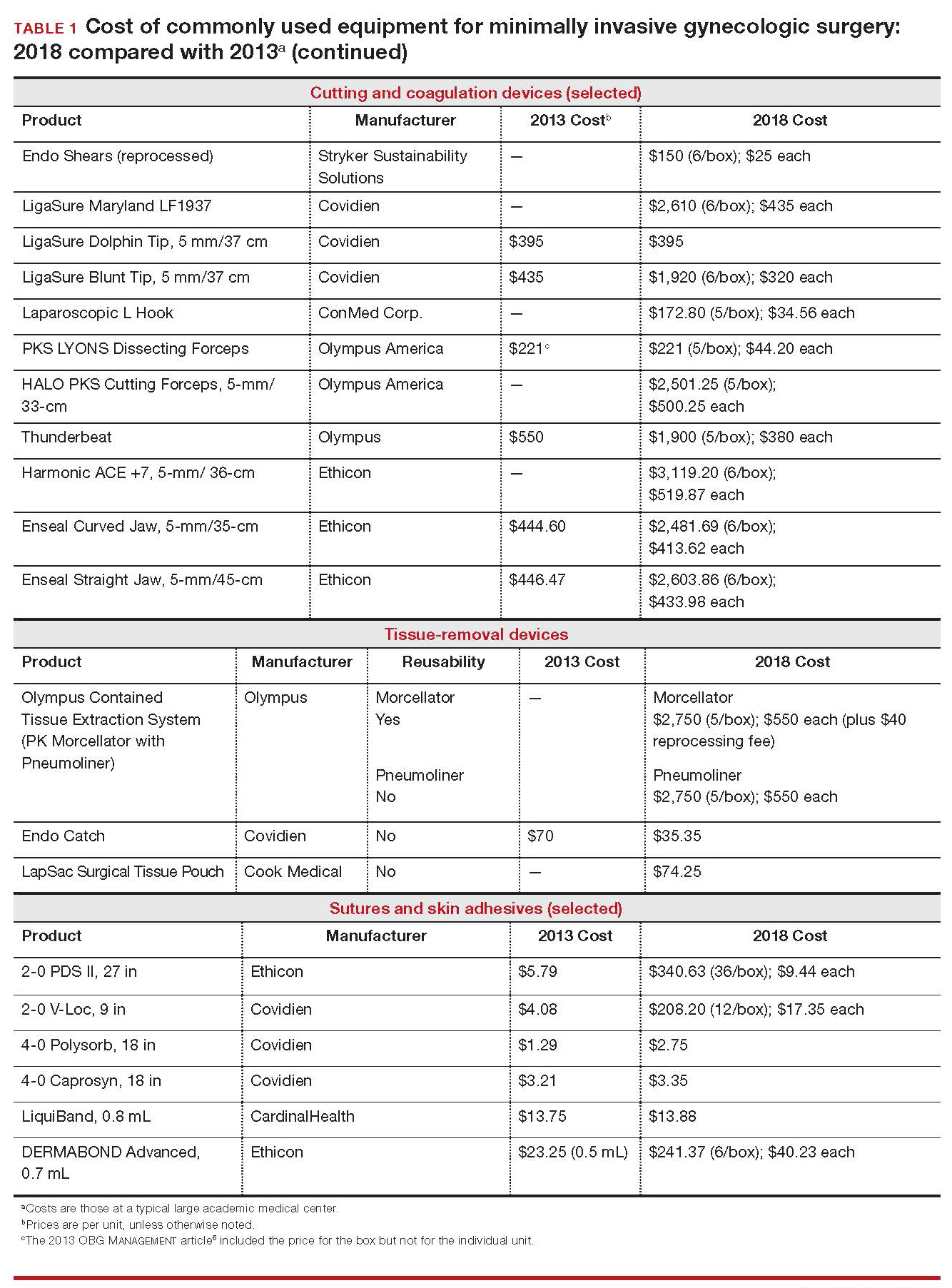
ChloraPrep is applied with a wand-like applicator and contains a much higher concentration of isopropyl alcohol than Hibiclens (70% and 4%, respectively), rendering it more flammable. It also requires longer drying time before surgery can be started. Clear and tinted ChloraPrep formulations are available.
Continue to: Uterine manipulators
Uterine manipulators
Cannulation of the cervical canal allows for uterine manipulation, increasing intraoperative traction and exposure as well as visualization of the adnexae and peritoneal surfaces.
The Hulka-Kenwick is a reusable uterine manipulator that is fairly standard and easy to apply. Specialized, single-use manipulators also are available, including the Advincula Delineator and VCare Plus uterine manipulator/elevator. The VCare Plus manipulator consists of 2 opposing cups: one cup (available in 4 sizes, small to extra-large) fits around the cervix and defines the site for colpotomy; the other helps maintain pneumoperitoneum once a colpotomy is created.
The ZUMI (Zinnanti Uterine Manipulator Injector) is a rigid, curved shaft with an intrauterine balloon to help prevent expulsion. It also has an integrated injection channel to allow for intraoperative chromotubation.
The RUMI II System fits individual patient anatomy with various tip lengths and colpotomy cup sizes. The Advincula Arch Uterine Manipulator Handle is a reusable alternative to the articulating RUMI II and works with the RUMI II System Disposable Tip (TABLE 1).
Continue to: Entry style and ports
Entry style and ports
The peritoneal cavity can be entered using either a closed (Veress needle) or open (Hasson) technique.7,8 Closed entry might allow for quicker access to the peritoneal cavity. A 2015 Cochrane review of 46 randomized, controlled trials of 7,389 patients undergoing laparoscopy compared outcomes between laparoscopic entry techniques and found no difference in major vascular or visceral injury between closed and open techniques at the umbilicus.9 However, open entry was associated with a greater likelihood of successful entry into the peritoneal cavity.9
Left upper-quadrant (Palmer’s point) entry is another option when adhesions are anticipated or abnormal anatomy is encountered at the umbilicus.
In general, complications related to laparoscopic entry are rare in gynecologic surgery, ranging from 0.18% to 0.5% of cases in studies.8,10,11 A minimally invasive surgeon might prefer one entry technique over another but should be able to perform both methods competently and recognize when a particular technique is warranted.
--
Choosing a port
Laparoscopic ports usually range from 5 mm to 12 mm and can be fixed or variable in size.
The primary port, usually placed through the umbilicus, can be a standard, blunt, 10-mm (Bluntport Plus Hasson) port, or it can be specialized to ease entry of the port or stabilize the port once it is introduced through the skin incision.
Optical trocars have a transparent tip that allows the surgeon to visualize the abdominal wall entry layer by layer using a 0° laparoscope, sometimes after pneumoperitoneum is created with a Veress needle. Other specialized ports include those that have balloons or foam collars, or both, to secure the port without traditional stay sutures on the fascia and to minimize leakage of pneumoperitoneum.
Continue to: Accessory ports
Accessory ports
When choosing an accessory port type and size, it is important to anticipate which instruments and devices, such as an Endo Catch bag, suture, or needle, will need to pass through it. Also, know whether 5-mm and 10-mm laparoscopes are available, and anticipate whether a second port with insufflation capabilities will be required.
The Pediport Locking Trocar is a user-friendly, 5-mm bladed port that deploys a mushroom-shaped stabilizer to prevent dislodgement. The Versaport bladed trocar has a spring-loaded entry shield, which slides over the blade to protect it once the peritoneal cavity is entered.
VersaStep Bladeless Trocars are introduced after a Step Insufflation Needle has been inserted. These trocars create a smaller fascial defect than conventional bladed trocars for an equivalent cannula size (TABLE 1).
Cutting and coagulating
Both monopolar and bipolar electrosurgical techniques are commonly employed in gynecologic laparoscopy. A wide variety of disposable and reusable instruments are available for monopolar energy, such as scissors, a hook, and a spatula.
Bipolar devices also can be disposable or reusable. Although bipolar electrosurgery minimizes injury to surrounding tissues by containing the current within the jaws of the forceps, it cannot cut or seal large vessels. As a result, several advanced bipolar devices with sealing and transecting capabilities have emerged (the LigaSure line of devices, Enseal). Ultrasonic devices, such as the Harmonic ACE, also can coagulate and cut at lower temperatures by converting electrical energy to mechanical energy (TABLE 1).
Continue to: Suture material
Suture material
Aspects of minimally invasive gynecologic surgery that require the use of suture include, but are not limited to, closure of the vaginal cuff, oophoropexy, and reapproximation of the ovarian cortex after cystectomy. Synthetic and delayed absorbable sutures, such as PDS II, are used frequently. The barbed suture also has gained popularity because it anchors to tissue without the need for intracorporeal or extracorporeal knots (TABLE 1).
Tissue removal
Adnexae and pathologic tissue, such as dermoid cysts, can be removed intact from the peritoneal cavity using an Endo Catch Single Use Specimen Pouch, a polyurethane sac. Careful use, with placement of the ovary with the cyst into the pouch prior to cystectomy, can contain or prevent spillage outside the bag.
A large uterus that cannot be extracted through a colpotomy can be manually morcellated. Appropriate candidates can undergo power morcellation using an FDA-approved device. (TABLE 1), allowing for the removal of smaller pieces through a small laparoscopic incision or the colpotomy.
Issues surrounding morcellation continue to require that gynecologic surgeons understand FDA recommendations. In 2014, the FDA issued a safety communication that morcellation is “contraindicated in gynecologic surgery if tissue is known or suspected to be malignant; it is contraindicated for uterine tissue removal with presumed benign fibroids in perimenopausal women.”12 A black-box warning was issued that uterine tissue might contain unsuspected cancer.
A task force created by AAGL addressed key issues in this controversy.
AAGL then provided guidelines related to morcellation13:
- Do not use morcellate in the setting of known malignancy.
- Provide appropriate preoperative evaluation with up-to-date Pap smear screening and image analysis.
- Increasing age significantly increases the risk of leiomyosarcoma, especially in a postmenopausal woman.
- Fibroid growth is not a reliable sign of malignancy.
- Do not use a morcellator if the patient is at high risk for malignancy.
- If leiomyosarcoma is the presumed pathology, await the final pathology report before proceeding with hysterectomy.
- Concomitant use of a bag might mitigate the risk of tissue spread.
- Obtain informed consent before proceeding with morcellation.
Continue to: Skin closure
Skin closure
Final subcuticular closure can be accomplished using sutures or skin adhesive. Sutures can be synthetic, absorbable monofilament (Caprosyn), or synthetic, absorbable, braided multifilament (Polysorb).
Skin adhesive closes incisions quickly, avoids inflammation related to foreign bodies, and can ease patients’ concerns that sometimes arise when absorbable suture persists postoperatively (TABLE 1).
The impact of physician experience
Physician experience has been shown to reduce cost while maintaining quality of care.14 That was the conclusion of researchers who undertook a retrospective study, addressing cost and clinical outcomes, of senior and junior attending physicians who performed laparoscopic-assisted vaginal hysterectomy on 120 patients. Studies such as these often lead to clinical pathways to facilitate cost-effective quality care.
--
CASE Same outcome at lower cost
The hypothetical 43-year-old patient in the opening case undergoes laparoscopic hysterectomy for treatment of uterine fibroids and menorrhagia. In this scenario, however, the surgeon makes the following product choices:
- The patient is prepped with Hibiclens.
- A VCare Plus uterine manipulator is placed.
- Laparoscopic ports include a VersaStep Plus Bladeless Trocar with Step Insufflation Needle; Versaport Plus Pyramidal Bladed Trocar; and 2 VersaOne Bladed trocars.
- The surgeon uses the PKS LYONS Dissecting Forceps and reprocessed Endo Shears to perform the hysterectomy.
- The uterus is enclosed in an Endo Catch bag and removed through the minilaparotomy site.
- The vaginal cuff is closed using 2-0 V-Loc barbed suture. Skin incisions are closed with 4-0 Polysorb, a polyglycolic acid absorbable suture.
The cost of this set of products? $360.44 or, roughly, $1,231.96 less than the set-up described in the case at the beginning of this article (TABLE 2).
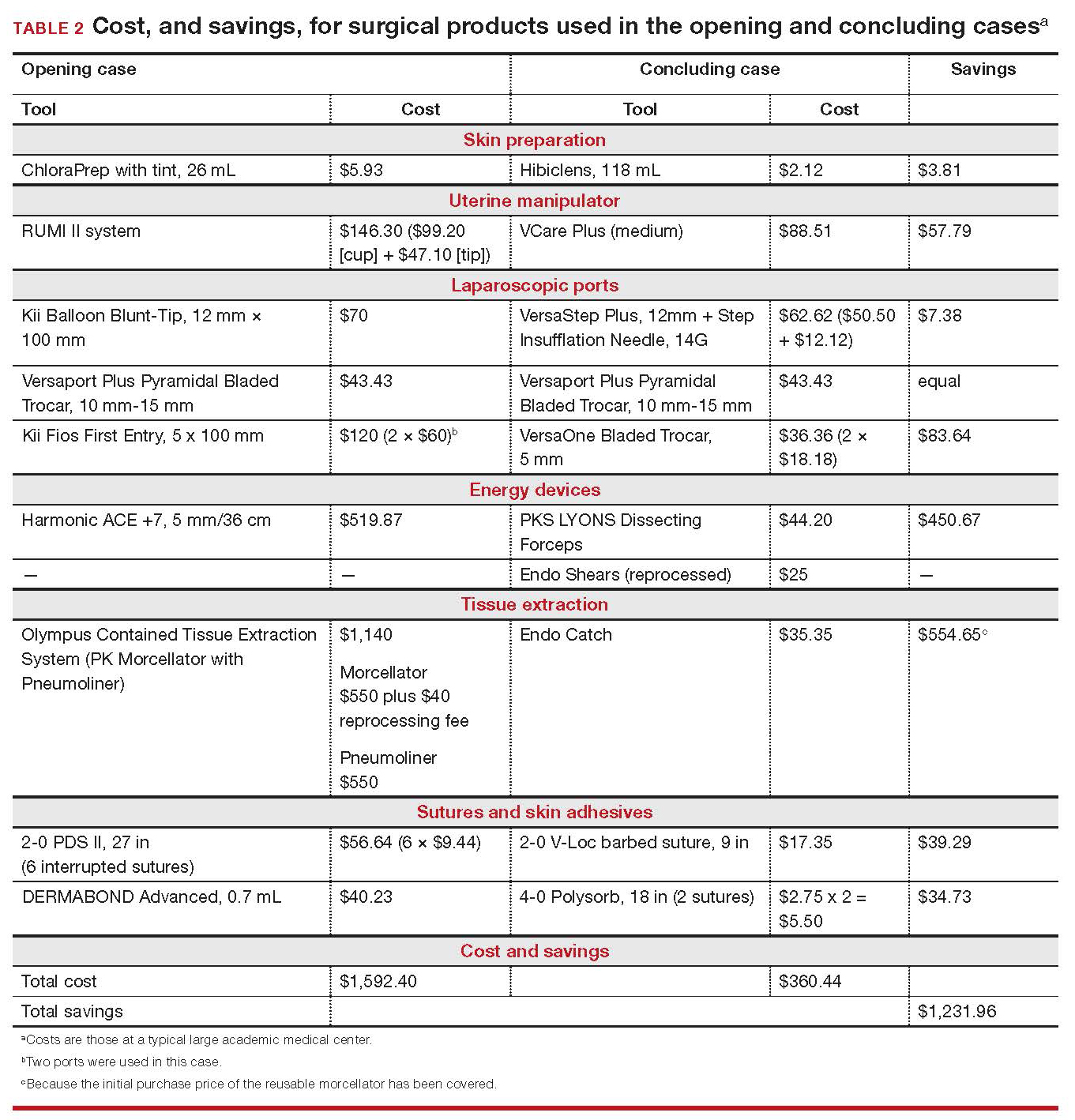
Continue to: Summing up
Summing up
Here are key points to take away from this analysis and discussion:
- As third-party payers and hospitals continue to evaluate surgeons individually and compare procedures from surgeon to surgeon, reimbursement might be stratified—thereby favoring physicians who demonstrate both quality outcomes and cost containment.
- There are many ways a minimally invasive surgeon can implement cost-conscious choices that have little or no impact on the quality of outcome.
- Surgeons who are familiar with surgical instruments and models available at their institution are better prepared to make wise cost-conscious decisions. (See “Caregivers should keep cost in mind: Here’s why,” in the Web version of this article at https://www.mdedge.com/obgyn.)
- Cost is not the only indicator of value: The surgeon must know how to apply tools correctly and be familiar with their limitations, and should choose instruments and products for their safety and ease of use. More often than not, a surgeon’s training and personal experience define—and sometimes restrict—the choice of devices.
- Last, it makes sense to have instruments and devices readily available in the operating room at the start of a case, to avoid unnecessary surgical delays. However, we recommend that you refrain from opening these tools until they are required intraoperatively. It is possible that the case will require conversion to laparotomy or that, after direct visualization of the pathology, different ports or instruments are required.
Acknowledgments
The authors would like to thank Meredith Snook, MD, who was coauthor of the original 2013 article6 and Kathleen Riordan, BSN, RN, for assistance in gathering specific cost-related information for this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE Cost-conscious benign laparoscopic hysterectomy
A 43-year-old woman undergoes laparoscopic hysterectomy for treatment of presumed benign uterine fibroids and menorrhagia. Once she is prepped with ChloraPrep with tint, a RUMI II uterine manipulator is placed. Laparoscopic ports include a Kii Balloon Blunt Tip system, a Versaport Plus Pyramidal Bladed Trocar, and 2 Kii Fios First Entry trocars.
The surgeon uses the Harmonic ACE +7 device (a purely ultrasonic device) to perform most of the procedure. The uterus is morcellated and removed using the US Food and Drug Administration (FDA)-approved Olympus Contained Tissue Extraction System, and the vaginal cuff is closed using a series of 2-0 PDS II sutures. Skin incisions are closed using Dermabond skin adhesive.
Total cost of the products used in this case: $1,592.40. Could different product choices have reduced this figure?
Health-care costs continue to rise faster than inflation: Total health-care expenditures account for approximately 18% of gross domestic product in the United States. Physicians therefore face increasing pressure to take cost into account in their care of patients.1 Cost-effectiveness and outcome quality continue to increase in importance as measures in many clinical trials that compare standard and alternative therapies. And women’s health—specifically, minimally invasive gynecologic surgery—invites such comparisons.
Overall, conventional laparoscopic gynecologic procedures tend to cost less than laparotomy, a consequence of shorter hospital stays, faster recovery, and fewer complications.2-5 What is not fully appreciated, however, is how choice of laparoscopic instrumentation and associated products affects surgical costs. In this article, which revisits and updates a 2013 OBG Management examination of cost-consciousness in the selection of equipment and supplies for minimally invasive gynecologic surgery,6 we review these costs in 2018. Our goal is to raise awareness of the role of cost in care among minimally invasive gynecologic surgeons.
In the sections that follow, we highlight several aspects of laparoscopic gynecologic surgery that can affect your selection of instruments and products, describing differences in cost as well as some distinctive characteristics of products. Note that our comparisons focus solely on cost—not on ease of utility, effectiveness, surgical technique, risk of complications, or any other assessment. Note also that numerous other instruments and devices are commercially available besides those we list.
Importantly, 2013 and 2018 costs are included in TABLE 1. Unless otherwise noted, costs are per unit. Changes in manufacturers and material costs and technologic advances have contributed to some, but not all, of the changes in cost between 2013 and 2018.
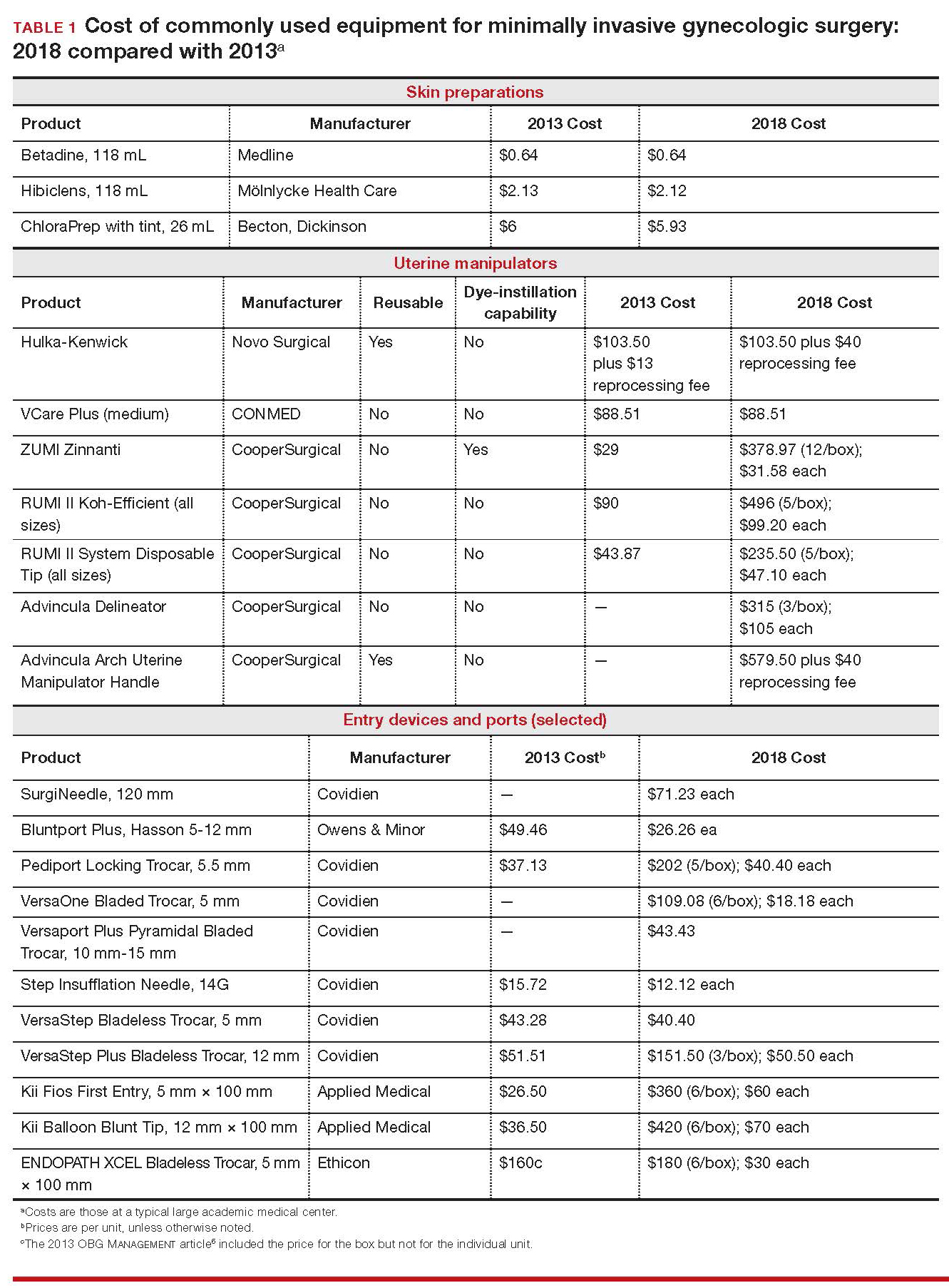
Continue to: Variables to keep in mind
Variables to keep in mind
Even when taking cost into consideration, tailor your selection of instruments and supplies to your capabilities and comfort, as well as to the particular characteristics of the patient and the planned procedure. Also, remember that your institution might have arrangements with companies that supply minimally invasive instruments, and that such arrangements might limit your options, to some degree. Last, be aware that reprocessed ports and instruments are now available at a reduced cost. In short, we believe that it is crucial for surgeons to be cognizant of all products available to them prior to attending a surgical case.
Skin preparation and other preop considerations
Multiple preoperative skin preparations are available (TABLE 1). Traditionally, a povidone–iodine topical antiseptic, such as Betadine, has been used for skin and vaginal preparation prior to gynecologic surgery. Hibiclens and ChloraPrep are different combinations of chlorhexidine gluconate and isopropyl alcohol that act as broad-spectrum antiseptics.
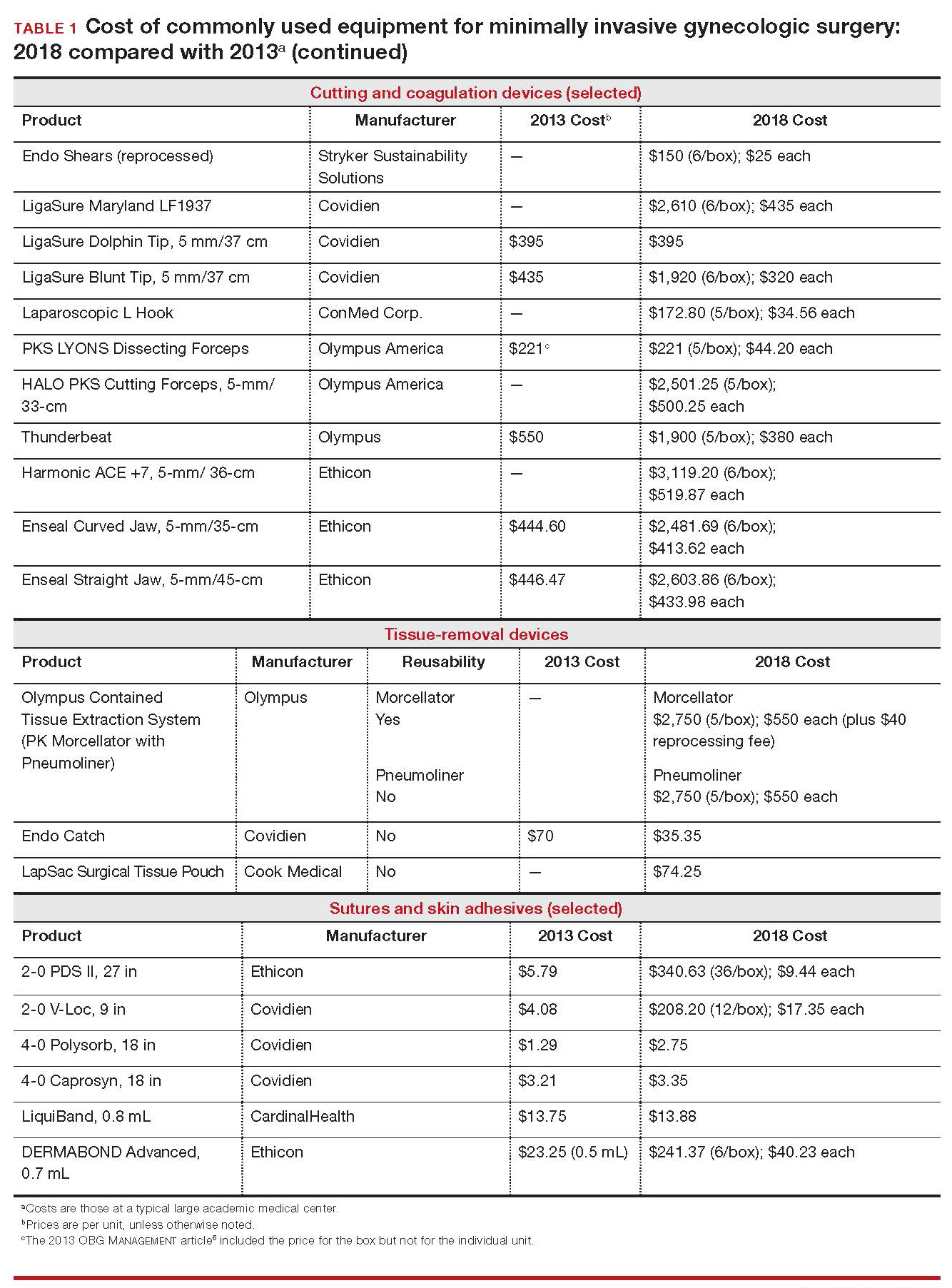
ChloraPrep is applied with a wand-like applicator and contains a much higher concentration of isopropyl alcohol than Hibiclens (70% and 4%, respectively), rendering it more flammable. It also requires longer drying time before surgery can be started. Clear and tinted ChloraPrep formulations are available.
Continue to: Uterine manipulators
Uterine manipulators
Cannulation of the cervical canal allows for uterine manipulation, increasing intraoperative traction and exposure as well as visualization of the adnexae and peritoneal surfaces.
The Hulka-Kenwick is a reusable uterine manipulator that is fairly standard and easy to apply. Specialized, single-use manipulators also are available, including the Advincula Delineator and VCare Plus uterine manipulator/elevator. The VCare Plus manipulator consists of 2 opposing cups: one cup (available in 4 sizes, small to extra-large) fits around the cervix and defines the site for colpotomy; the other helps maintain pneumoperitoneum once a colpotomy is created.
The ZUMI (Zinnanti Uterine Manipulator Injector) is a rigid, curved shaft with an intrauterine balloon to help prevent expulsion. It also has an integrated injection channel to allow for intraoperative chromotubation.
The RUMI II System fits individual patient anatomy with various tip lengths and colpotomy cup sizes. The Advincula Arch Uterine Manipulator Handle is a reusable alternative to the articulating RUMI II and works with the RUMI II System Disposable Tip (TABLE 1).
Continue to: Entry style and ports
Entry style and ports
The peritoneal cavity can be entered using either a closed (Veress needle) or open (Hasson) technique.7,8 Closed entry might allow for quicker access to the peritoneal cavity. A 2015 Cochrane review of 46 randomized, controlled trials of 7,389 patients undergoing laparoscopy compared outcomes between laparoscopic entry techniques and found no difference in major vascular or visceral injury between closed and open techniques at the umbilicus.9 However, open entry was associated with a greater likelihood of successful entry into the peritoneal cavity.9
Left upper-quadrant (Palmer’s point) entry is another option when adhesions are anticipated or abnormal anatomy is encountered at the umbilicus.
In general, complications related to laparoscopic entry are rare in gynecologic surgery, ranging from 0.18% to 0.5% of cases in studies.8,10,11 A minimally invasive surgeon might prefer one entry technique over another but should be able to perform both methods competently and recognize when a particular technique is warranted.
--
Choosing a port
Laparoscopic ports usually range from 5 mm to 12 mm and can be fixed or variable in size.
The primary port, usually placed through the umbilicus, can be a standard, blunt, 10-mm (Bluntport Plus Hasson) port, or it can be specialized to ease entry of the port or stabilize the port once it is introduced through the skin incision.
Optical trocars have a transparent tip that allows the surgeon to visualize the abdominal wall entry layer by layer using a 0° laparoscope, sometimes after pneumoperitoneum is created with a Veress needle. Other specialized ports include those that have balloons or foam collars, or both, to secure the port without traditional stay sutures on the fascia and to minimize leakage of pneumoperitoneum.
Continue to: Accessory ports
Accessory ports
When choosing an accessory port type and size, it is important to anticipate which instruments and devices, such as an Endo Catch bag, suture, or needle, will need to pass through it. Also, know whether 5-mm and 10-mm laparoscopes are available, and anticipate whether a second port with insufflation capabilities will be required.
The Pediport Locking Trocar is a user-friendly, 5-mm bladed port that deploys a mushroom-shaped stabilizer to prevent dislodgement. The Versaport bladed trocar has a spring-loaded entry shield, which slides over the blade to protect it once the peritoneal cavity is entered.
VersaStep Bladeless Trocars are introduced after a Step Insufflation Needle has been inserted. These trocars create a smaller fascial defect than conventional bladed trocars for an equivalent cannula size (TABLE 1).
Cutting and coagulating
Both monopolar and bipolar electrosurgical techniques are commonly employed in gynecologic laparoscopy. A wide variety of disposable and reusable instruments are available for monopolar energy, such as scissors, a hook, and a spatula.
Bipolar devices also can be disposable or reusable. Although bipolar electrosurgery minimizes injury to surrounding tissues by containing the current within the jaws of the forceps, it cannot cut or seal large vessels. As a result, several advanced bipolar devices with sealing and transecting capabilities have emerged (the LigaSure line of devices, Enseal). Ultrasonic devices, such as the Harmonic ACE, also can coagulate and cut at lower temperatures by converting electrical energy to mechanical energy (TABLE 1).
Continue to: Suture material
Suture material
Aspects of minimally invasive gynecologic surgery that require the use of suture include, but are not limited to, closure of the vaginal cuff, oophoropexy, and reapproximation of the ovarian cortex after cystectomy. Synthetic and delayed absorbable sutures, such as PDS II, are used frequently. The barbed suture also has gained popularity because it anchors to tissue without the need for intracorporeal or extracorporeal knots (TABLE 1).
Tissue removal
Adnexae and pathologic tissue, such as dermoid cysts, can be removed intact from the peritoneal cavity using an Endo Catch Single Use Specimen Pouch, a polyurethane sac. Careful use, with placement of the ovary with the cyst into the pouch prior to cystectomy, can contain or prevent spillage outside the bag.
A large uterus that cannot be extracted through a colpotomy can be manually morcellated. Appropriate candidates can undergo power morcellation using an FDA-approved device. (TABLE 1), allowing for the removal of smaller pieces through a small laparoscopic incision or the colpotomy.
Issues surrounding morcellation continue to require that gynecologic surgeons understand FDA recommendations. In 2014, the FDA issued a safety communication that morcellation is “contraindicated in gynecologic surgery if tissue is known or suspected to be malignant; it is contraindicated for uterine tissue removal with presumed benign fibroids in perimenopausal women.”12 A black-box warning was issued that uterine tissue might contain unsuspected cancer.
A task force created by AAGL addressed key issues in this controversy.
AAGL then provided guidelines related to morcellation13:
- Do not use morcellate in the setting of known malignancy.
- Provide appropriate preoperative evaluation with up-to-date Pap smear screening and image analysis.
- Increasing age significantly increases the risk of leiomyosarcoma, especially in a postmenopausal woman.
- Fibroid growth is not a reliable sign of malignancy.
- Do not use a morcellator if the patient is at high risk for malignancy.
- If leiomyosarcoma is the presumed pathology, await the final pathology report before proceeding with hysterectomy.
- Concomitant use of a bag might mitigate the risk of tissue spread.
- Obtain informed consent before proceeding with morcellation.
Continue to: Skin closure
Skin closure
Final subcuticular closure can be accomplished using sutures or skin adhesive. Sutures can be synthetic, absorbable monofilament (Caprosyn), or synthetic, absorbable, braided multifilament (Polysorb).
Skin adhesive closes incisions quickly, avoids inflammation related to foreign bodies, and can ease patients’ concerns that sometimes arise when absorbable suture persists postoperatively (TABLE 1).
The impact of physician experience
Physician experience has been shown to reduce cost while maintaining quality of care.14 That was the conclusion of researchers who undertook a retrospective study, addressing cost and clinical outcomes, of senior and junior attending physicians who performed laparoscopic-assisted vaginal hysterectomy on 120 patients. Studies such as these often lead to clinical pathways to facilitate cost-effective quality care.
--
CASE Same outcome at lower cost
The hypothetical 43-year-old patient in the opening case undergoes laparoscopic hysterectomy for treatment of uterine fibroids and menorrhagia. In this scenario, however, the surgeon makes the following product choices:
- The patient is prepped with Hibiclens.
- A VCare Plus uterine manipulator is placed.
- Laparoscopic ports include a VersaStep Plus Bladeless Trocar with Step Insufflation Needle; Versaport Plus Pyramidal Bladed Trocar; and 2 VersaOne Bladed trocars.
- The surgeon uses the PKS LYONS Dissecting Forceps and reprocessed Endo Shears to perform the hysterectomy.
- The uterus is enclosed in an Endo Catch bag and removed through the minilaparotomy site.
- The vaginal cuff is closed using 2-0 V-Loc barbed suture. Skin incisions are closed with 4-0 Polysorb, a polyglycolic acid absorbable suture.
The cost of this set of products? $360.44 or, roughly, $1,231.96 less than the set-up described in the case at the beginning of this article (TABLE 2).
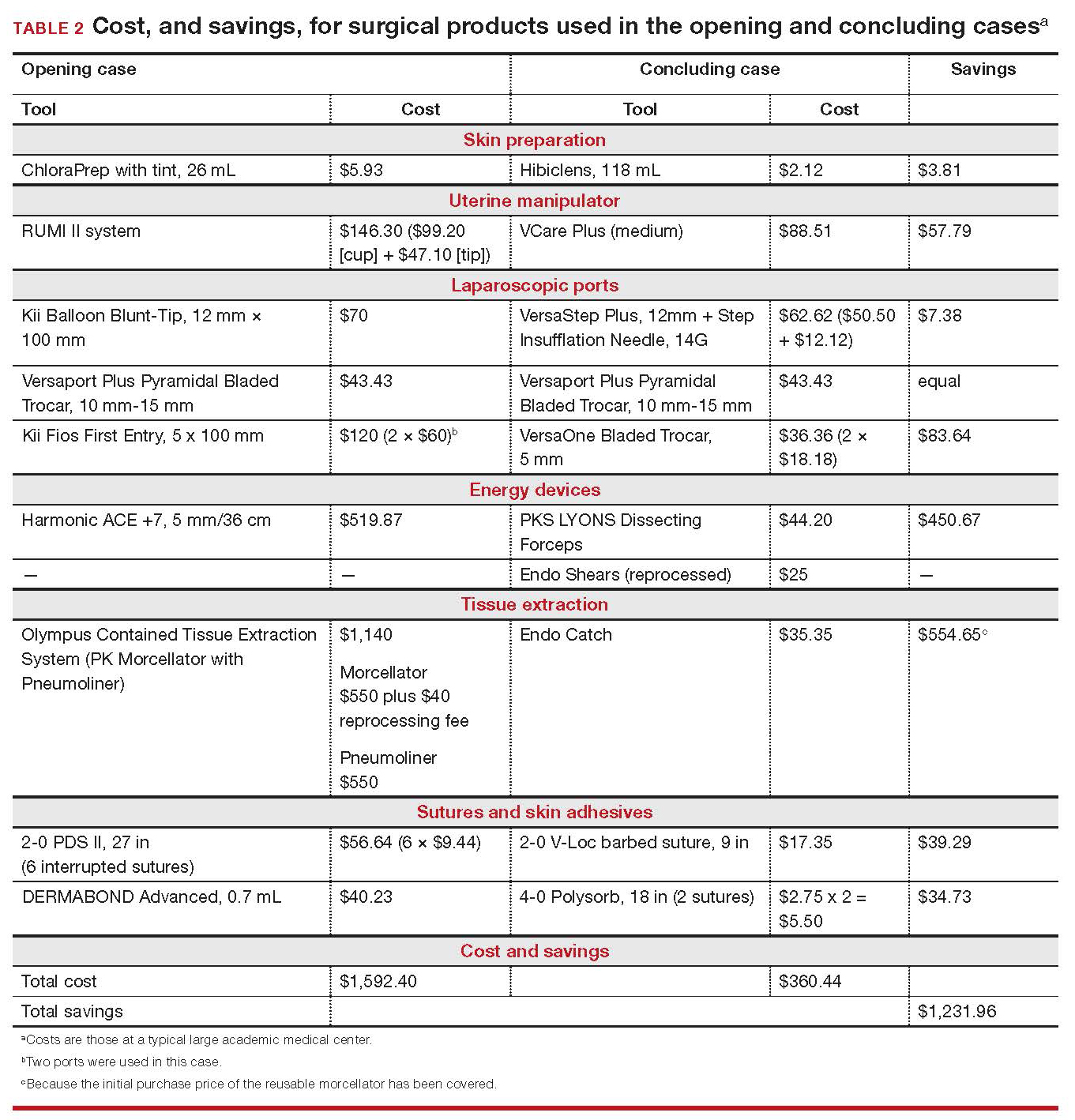
Continue to: Summing up
Summing up
Here are key points to take away from this analysis and discussion:
- As third-party payers and hospitals continue to evaluate surgeons individually and compare procedures from surgeon to surgeon, reimbursement might be stratified—thereby favoring physicians who demonstrate both quality outcomes and cost containment.
- There are many ways a minimally invasive surgeon can implement cost-conscious choices that have little or no impact on the quality of outcome.
- Surgeons who are familiar with surgical instruments and models available at their institution are better prepared to make wise cost-conscious decisions. (See “Caregivers should keep cost in mind: Here’s why,” in the Web version of this article at https://www.mdedge.com/obgyn.)
- Cost is not the only indicator of value: The surgeon must know how to apply tools correctly and be familiar with their limitations, and should choose instruments and products for their safety and ease of use. More often than not, a surgeon’s training and personal experience define—and sometimes restrict—the choice of devices.
- Last, it makes sense to have instruments and devices readily available in the operating room at the start of a case, to avoid unnecessary surgical delays. However, we recommend that you refrain from opening these tools until they are required intraoperatively. It is possible that the case will require conversion to laparotomy or that, after direct visualization of the pathology, different ports or instruments are required.
Acknowledgments
The authors would like to thank Meredith Snook, MD, who was coauthor of the original 2013 article6 and Kathleen Riordan, BSN, RN, for assistance in gathering specific cost-related information for this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Centers for Medicare & Medicaid Services. National health expenditure projections 2017-2026: Forecast summary. www.cms.gov/Research-Statistics-Data-and-Systems /Statistics-Trends-and-Reports/NationalHealthExpendData /Downloads/ForecastSummary.pdf. Accessed November 3, 2018.
- Vilos GA, Alshimmiri MM. Cost-benefit analysis of laparoscopic versus laparotomy salpingo-oophorectomy for benign tubo-ovarian disease. J Am Assoc Gynecol Laparosc. 1995;2(3):299-303.
- Gray DT, Thorburn J, Lundor P, et al. A cost-effectiveness study of a randomised trial of laparoscopy versus laparotomy for ectopic pregnancy. Lancet. 1995;345(8958):1139-1143.
- Chapron C, Fauconnier A, Goffinet F, et al. Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynaecologic pathology. Results of a metaanalysis. Hum Reprod. 2002;17(5):1334-1342.
- Benezra V, Verma U, Whitted RW. Comparison of laparoscopy versus laparotomy for the surgical treatment of ovarian dermoid cysts. Obstet Gynecol Surv. 2006;61(1): 20-21.
- Sanfilippo JS, Snook ML. Cost-conscious choices for minimally invasive gynecologic surgery. OBG Manag. 2013;25(11):40-41,44,46-48,72.
- Hasson HM. A modified instrument and method for laparoscopy. Am J Obstet Gynecol. 1971;110(6):886-887.
- Ott J, Jaeger-Lansky A, Poschalko G, et al. Entry techniques in gynecologic laparoscopy—a review. Gynecol Surg. 2012;9(2):139-146.
- Ahmad G, Gent D, Henderson D, et al. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2015;8:CD006583.
- Hasson HM, Rotman C, Rana N, et al. Open laparoscopy: 29-year experience. Obstet Gynecol. 2000;96(5 Pt 1):763-766.
- Schäfer M, Lauper M, Krähenbühl L. Trocar and Veress needle injuries during laparoscopy. Surg Endosc. 2001;15(3):275- 280.
- Immediately in effect guidance document: product labeling for laparoscopic power morcellators. Rockville, MD: US Department of Health and Human Services, Food and Drug Administration Center for Devices and Radiological Health; November 25, 2014. www.fda.gov/downloads /MedicalDevices/DeviceRegulationandGuidance /GuidanceDocuments/UCM424123.pdf. Accessed November 3, 2018.
- Tissue Extraction Task Force Members. Morcellation during uterine tissue extraction: an update. J Minim Invasive Gynecol. 2018;25(4):543-550.
- Chang WC, Li TC, Lin CC. The effect of physician experience on costs and clinical outcomes of laparoscopic-assisted vaginal hysterectomy: a multivariate analysis. J Am Assoc Gynecol Laparosc. 2003;10(3):356-359.
- Centers for Medicare & Medicaid Services. National health expenditure projections 2017-2026: Forecast summary. www.cms.gov/Research-Statistics-Data-and-Systems /Statistics-Trends-and-Reports/NationalHealthExpendData /Downloads/ForecastSummary.pdf. Accessed November 3, 2018.
- Vilos GA, Alshimmiri MM. Cost-benefit analysis of laparoscopic versus laparotomy salpingo-oophorectomy for benign tubo-ovarian disease. J Am Assoc Gynecol Laparosc. 1995;2(3):299-303.
- Gray DT, Thorburn J, Lundor P, et al. A cost-effectiveness study of a randomised trial of laparoscopy versus laparotomy for ectopic pregnancy. Lancet. 1995;345(8958):1139-1143.
- Chapron C, Fauconnier A, Goffinet F, et al. Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynaecologic pathology. Results of a metaanalysis. Hum Reprod. 2002;17(5):1334-1342.
- Benezra V, Verma U, Whitted RW. Comparison of laparoscopy versus laparotomy for the surgical treatment of ovarian dermoid cysts. Obstet Gynecol Surv. 2006;61(1): 20-21.
- Sanfilippo JS, Snook ML. Cost-conscious choices for minimally invasive gynecologic surgery. OBG Manag. 2013;25(11):40-41,44,46-48,72.
- Hasson HM. A modified instrument and method for laparoscopy. Am J Obstet Gynecol. 1971;110(6):886-887.
- Ott J, Jaeger-Lansky A, Poschalko G, et al. Entry techniques in gynecologic laparoscopy—a review. Gynecol Surg. 2012;9(2):139-146.
- Ahmad G, Gent D, Henderson D, et al. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2015;8:CD006583.
- Hasson HM, Rotman C, Rana N, et al. Open laparoscopy: 29-year experience. Obstet Gynecol. 2000;96(5 Pt 1):763-766.
- Schäfer M, Lauper M, Krähenbühl L. Trocar and Veress needle injuries during laparoscopy. Surg Endosc. 2001;15(3):275- 280.
- Immediately in effect guidance document: product labeling for laparoscopic power morcellators. Rockville, MD: US Department of Health and Human Services, Food and Drug Administration Center for Devices and Radiological Health; November 25, 2014. www.fda.gov/downloads /MedicalDevices/DeviceRegulationandGuidance /GuidanceDocuments/UCM424123.pdf. Accessed November 3, 2018.
- Tissue Extraction Task Force Members. Morcellation during uterine tissue extraction: an update. J Minim Invasive Gynecol. 2018;25(4):543-550.
- Chang WC, Li TC, Lin CC. The effect of physician experience on costs and clinical outcomes of laparoscopic-assisted vaginal hysterectomy: a multivariate analysis. J Am Assoc Gynecol Laparosc. 2003;10(3):356-359.
Abortion, the travel ban, and other top Supreme Court rulings affecting your practice
The 2017−2018 term of the Supreme Court of the United States (SCOTUS) was momentous. Justice Anthony Kennedy, who had been the deciding vote in most of the 5 to 4 cases for a generation, announced his retirement as of July 31, 2018. In addition, the Court decided a number of cases of interest to ObGyns. In this article we review some of those cases, as well as consider the future of the Court without Justice Kennedy. In selecting cases, we have given special attention to those in which national medical organizations filed amicus briefs. These “amicus curiae” or “friend of the court” briefs are filed by an entity who is not party to a case but wants to provide information or views to the court.

1. Abortion rulings

The Court decided 2 abortion cases and rejected a request to hear a third.
National Institute of Family and Life Advocates v Becerra
In this case,1 the Court struck down a California law that required pregnancy crisis centers not offering abortions (generally operated by pro-life groups) to provide special notices to clients.2
At stake. These notices would inform clients that California provides free or low-cost services, including abortions, and provide a phone number to call for those services.
There were many amicus briefs filed in this case, including those by the American College of Obstetricians and Gynecologists (ACOG) and other specialty boards,3 as well as the American Association of Pro-Life Obstetricians and Gynecologists and other pro-life organizations.4 ACOG’s brief argued that the California-required notice facilitates the goal of allowing women to receive medical services without harmful delay.
Final ruling. The Court held that the law required clinics to engage in speech with which the clinics disagreed (known as “compelled speech”). It also noted that California disclosure requirements were “wildly underinclusive” because they apply only to some clinics. The majority felt that there was no strong state interest in compelling this speech because there were other alternatives for the state to provide information about the availability of abortion and other services. The Court found that the clinics were likely to succeed on the merits of their claims of a First Amendment (free speech) violation.
Right to abortion for illegal immigrants in custody
A very unusual abortion case involved “Jane Doe,” a minor who was at 8 weeks’ gestation when she illegally crossed the border into the United States.5 She was placed in a federally-funded shelter where she requested an abortion. The facility denied that request.
At stake. Legal argument ensued about releasing her to another facility for an abortion, as the argument was made that pregnant minors who are apprehended crossing into the United States illegally and placed into the custody of federal officials should have abortion access. A lower Court of Appeals ruled against the Trump Administration’s policy of denying abortions to undocumented minors in federal custody. During the process of the federal government taking the case to the Supreme Court, the attorneys for Doe moved appointments around and, without notice, the abortion was performed. Government attorneys said that Doe’s attorneys made “what appear to be material misrepresentations and omissions” designed to “thwart [the Supreme Court’s] review” of the case.5 The government requested that the Court vacate the order of the Court of Appeals so that it could not be used as precedent.
Final ruling. The Court granted the governments request to vacate the lower court’s order because the minor was no longer pregnant and the order was therefore moot. The basic issue in this case (the right of in-custody minors to access abortions) remains unresolved. It is likely to appear before the Court in the future.
Continue to: Access to medical abortions
Access to medical abortions
An Arkansas law requires that a physician administering medical abortions contract with a physician who has admitting privileges at a hospital (a “contracted physician”).
At stake. Planned Parenthood filed suit challenging the requirement as unnecessary and harmful because it would result in the closure of 2 of the 3 abortion providers in Arkansas. ACOG filed an amicus brief urging the Supreme Court to consider the case.6 (Technically this was a petition for a Writ of Certiorari, the procedure by which the Court accepts cases. It accepts only about 1% of applications.) ACOG argued that there was no medical reason for the contracted physician requirement, and noted the harm it would do to women who would not have access to abortions.
Final ruling. On May 29, 2018, the Court declined to hear the case. This case is still active in the lower courts and may eventually return to the Supreme Court.

2. The patent system

The medical profession depends on the patent system to encourage the discovery of new patents efficiently and effectively. In 2012, Congress passed the America Invents Act7 that authorizes a petition by anyone other than the patent holder to the Patent and Trademark Office (PTO) for an “inter partes review” to assess a challenge to the patent’s legitimacy. If the PTO determines that there may be merit to the claim, the Patent Trial and Appeal Board undertakes a trial-like review process that may validate, invalidate, or amend the patent. The Board’s decision is subject to appellate court review.
At stake. This term, the inter partes review was challenged as unconstitutional on technical bases.8
Final ruling. The Court rejected this claim and approved the current administrative inter partes review process. The Court determined that once the Patent Office takes a petition challenging a patent, it must decide all of the claims against the patent, not pick and choose which elements of the challenge to evaluate.9 The Court’s decision upheld patent-review reform, but will require the Patent Office to tweak its procedures.

3. The travel ban

ACOG, the American Medical Association (AMA), the Association of American Medical Colleges, and more than 30 other health care and specialty associations filed an amicus brief regarding one of the most anticipated cases of the term—the “travel ban.”10
At stake. The essential argument of these organizations was that the US health care system depends on professionals from other countries. An efficient and fair immigration program is, therefore, important to advance the nation’s “health security.” During the 2016−2017 term, the Court considered but then removed the issue from its calendar when the Trump Administration issued a revised travel ban.11
In September 2017, President Trump’s proclamation imposed a range of entry restrictions on the citizens of 8 countries, most (but not all) of which are predominantly Muslim. The government indicated that, in a study by Homeland Security and the State Department, these countries were identified as having especially deficient information-sharing practices and presented national security concerns. Trump v Hawaii12 challenged this proclamation.
Final ruling. The majority of the Court upheld the travel ban. For the 5-Justice majority led by Chief Justice Roberts, the case came down to 3 things:
- The Constitution and the laws passed by Congress of necessity give the President great authority to engage in foreign policy, including policies regarding entry into the country.
- The courts are very reluctant to get into the substance of foreign affairs—they are not equipped to know in detail what the facts are, and things change very fast.
- If courts start tinkering with foreign policy and things turn bad, it will appear that the courts are to blame and were interfering in an area about which they are not competent.
Continue to: 4. Did a credit card case add risk to health insurance markets?

It was just a credit card case, but one in which the AMA saw a real risk to regulation of the health insurance markets.
At stake. Technically, Ohio v American Express concerned a claim that American Express (AmEx) violated antitrust laws when it prohibited merchants taking its credit card from “steering” customers to cards with lower fees.13 AmEx maintained that, because credit cards were a special kind of “2-sided” market (connecting merchants on one side and customers on the other), antitrust laws should not be strictly enforced.
The AMA noticed that special rules regarding 2-sided markets might apply to health insurance, and it submitted an amicus brief14 that noted: “dominant health insurance networks … have imposed and could further impose rules or effectively erect barriers that prohibit physicians from referring patients to certain specialists, particularly out-of-network specialists, for innovative and even necessary medical tests.”14 It concluded that the antitrust rule AmEx was suggesting would make it nearly impossible to challenge these unfair provisions in health insurance arrangements.
Final ruling. The Court, however, accepted the AmEx position, making it very difficult to develop an antitrust case against 2-sided markets. It remains to be seen the degree to which the AMA concern about health insurance markets will be realized.

5. Gay wedding and a bakeshop

At stake. In Masterpiece Cakeshop v Colorado, a cakemaker declined to design a cake for a gay wedding and had been disciplined under Colorado law for discriminating against the couple based on sexual orientation.15
Final ruling. The Court, however, found that the Colorado regulators had, ironically, shown such religious animus in the way they treated the baker that the regulators themselves had discriminated on the basis of religion. As a result, the Court reversed the sanctions against the baker.
This decision was fairly narrow. It does not, for example, stand for the proposition that there may be a general religious exception to antidiscrimination laws. The question of broader religious or free-speech objections to antidiscrimination laws remains for another time.
Amicus brief. It was interesting that the American College of Pediatricians, American Association of Pro-Life Obstetricians and Gynecologists, and others, filed an amicus brief to report with concern the “demands that individual medical professionals must perform, assist with, or facilitate abortions, without regard to the teachings of their own faiths, consciences, and convictions.”16 The brief also noted that “issues in the present case implicate the fundamental rights of health care professionals, and to respectfully urge that the Court should by no means permit any weakening or qualification of well-established protections against compelled speech, and of free exercise” of religion.16
Arbitration. The Court upheld, as it has in most recent terms, another arbitration agreement.1 This case concerned an employment agreement in which employees consented to submit to arbitration rather than file lawsuits and not use class action claims.
Search of cell-phone location. Cell phones, whenever turned on, connect with cell towers that record the phone’s location several times a minute. Cell companies store this information, creating a virtual map of where the owner is at all times. The Federal Bureau of Investigation asked a cell company for location information for several people during a 127-day period in which robberies were committed.2 The Court held that the search was illegal in the absence of a warrant.
Public employee unions. The Court held that agency (fair share) fees, in which public employees who are not union members can be required to pay dues for the bargaining and grievance activities (from which they generally benefit), violate the First Amendment. The majority held that forcing public employees to pay fees to unions requires the employees, through those fees, to engage in political activities with which they disagree.3 This is a form of compelled speech, which the Court found violates the First Amendment. Health care professionals who are public employees in positions that have union representation will probably have the opportunity to opt out of agency agreements.
Internet sales tax. The Court permitted states to charge sales tax on out-of-state Internet purchases.4 In doing so, a state may require out-of-state companies to collect taxes on sales to its residents.
References
- Epic Systems Corp. v Lewis, 584 US 16 285 (2018).
- Carpenter v United States, 585 US 16 402 (2018).
- Janus v State, County, and Municipal Employees, 585 US 16 1466 (2018).
- South Dakota v Wayfair, Inc, 585 US 17 494 (2018).
Clues to the future
During the term that ran from October 2, 2017, through June 27, 2018, the Court issued 72 decisions. An unusually high proportion of cases (26%; 19 cases) were decided on a 5 to 4 vote. Last term, the rate of 5 to 4 decisions was 10%; the 6-year average was 18%. The unanimous decision rate was 39% this term, compared with 59% last term, and 50% on average.
The rate of 5 to 4 cases provides a clue about the Court’s general direction. The number of times each Justice was in the majority in those nineteen 5 to 4 decisions included: Chief Justice Roberts, 17; and Justices Kennedy, 16; Gorsuch, 16; Thomas, 15; and Alito, 15; compared with Justices Ginsburg, 5; Breyer, 4; Sotomayor, 4; and Kagan, 3.
The Court convened on October 1, 2018. At this writing, whether the new term starts with 8 or 9 justices remains a question. President Trump nominated Brett Kavanaugh, JD, to take Justice Kennedy’s place on the Court. His professional qualifications and experience appear to make him qualified for a position on the Court, but as we have seen, there are many other elements that go into confirming a Justice’s nomination.
Justice Anthony Kennedy was the deciding vote in the overwhelming majority of the 5 to 4 decisions in 20 of his 30 years on the Court. The areas in which he had an especially important impact include1:
- Gay rights. Justice Kennedy wrote the opinions (usually 5 to 4 decisions) in a number of groundbreaking gay-rights cases, including decriminalizing homosexual conduct, striking down the Defense of Marriage Act, and finding that the Constitution requires states to recognize gay marriage.
- The death penalty. Justice Kennedy wrote decisions that prohibited states from imposing the death penalty for any crime other than murder, for defendants who were under 18 when they committed the crime, and for defendants with serious developmental disabilities. He expressed reservations about long-term solitary confinement, but did not have a case that allowed him to decide its constitutionality.
- The First Amendment. Early in his service on the Court, he held that the First Amendment protected flag burning as a form of speech. He decided many important freespeech and freedom-of-religion cases that have set a standard for protecting those fundamental freedoms.
- Use of health and social science data. Justice Kennedy was more open to mental health information and cited it more often than most other Justices.
- Abortion rights? Many commentators would add protecting the right to choose to have an abortion to the above list. Justice Kennedy was a central figure in one case that declined to back away from Roe v Wade, and joined a more recent decision that struck down a Texas law that created an undue burden on women seeking abortion. Plus, he also voted to uphold abortion restrictions, such as “partial-birth-abortion laws.” So there is a good argument for including abortion rights on the list, although he did not break new ground.
Justice Kennedy as a person
Outside the courtroom, Justice Kennedy is a person of great warmth and compassion. He is a natural teacher and spends a great deal of time with students. When asked how he would like to be remembered, Justice Kennedy once replied, “Somebody who’s decent, and honest, and fair, and who’s absolutely committed to the proposition that freedom is America’s gift to the rest of the world.” I agree with that assessment.
STEVEN R. SMITH, MS, JD
Reference
- South Dakota v Wayfair, Inc, 585 US (2018)
Next term, the Court is scheduled to hear cases regarding pharmaceutical liability, double jeopardy, sex-offender registration, expert witnesses, Social Security disability benefits, and the Age Discrimination in Employment Act. There will be at least 3 arbitration cases. Health care and reproductive rights will continue to be an important part of the Court’s docket.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- National Institute of Family and Life Advocates v Becerra, 585 US 16 1140 (2018).
- California Reproductive Freedom, Accountability, Comprehensive Care, and Transparency Act (FACT Act), Cal. Health & Safety Code Ann. §123470 et seq. (West 2018).
- Brief amici curiae of American Academy of Pediatrics, et al. in National Institute of Family and Life Advocates v Becerra, February 27, 2018.
- Brief amici curiae of American Association of Pro-Life Obstetricians & Gynecologists, et al. in National Institute of Family and Life Advocates v Becerra, January 16, 2018.
- Azar v Garza, 584 US 17 654 (2018).
- Brief amici curiae of American College of Obstetricians and Gynecologists and American Public Health Association in Planned Parenthood of Arkansas and Eastern Oklahoma v Jegley, February 1, 2018.
- Chapter 31, Inter Partes Review. United States Code. Title 35: Patents. Part III, Patents and protection of patents. 2012 Ed. 35 USC 311–319.
- Oil States Energy Services, LLC v Greene’s Energy Group, LLC, 584 US 16 712 (2018).
- SAS Institute Inc. v Iancu, 584 US 16 969 (2018).
- Brief for Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents, Trump v Hawaii. https://www.supremecourt.gov/Docket PDF/17/ 17-965/40128/20180327105855912_17-965%20Amicus%20Br.%20Proclamation.pdf. Accessed September 21, 2018.
- Smith SR, Sanfilippo JS. Supreme Court decisions in 2017 that affected your practice. OBG Manag. 2017;29(12)44–47.
- Trump v Hawaii, 585 US 17 965 (2018).
- Ohio v American Express Co, 585 US 16 1454 (2018).
- Brief amici curiae of American Medical Association and Ohio State Medical Association in Ohio v American Express, December 24, 2017.
- Masterpiece Cakeshop, Ltd. v Colorado Civil Rights Commission, 584 US 16 111 (2018).
- Brief amici curiae of American College of Pediatricians, et al. in Masterpiece Cakeshop v Colorado Civil Rights Commission, September 7, 2017.
The 2017−2018 term of the Supreme Court of the United States (SCOTUS) was momentous. Justice Anthony Kennedy, who had been the deciding vote in most of the 5 to 4 cases for a generation, announced his retirement as of July 31, 2018. In addition, the Court decided a number of cases of interest to ObGyns. In this article we review some of those cases, as well as consider the future of the Court without Justice Kennedy. In selecting cases, we have given special attention to those in which national medical organizations filed amicus briefs. These “amicus curiae” or “friend of the court” briefs are filed by an entity who is not party to a case but wants to provide information or views to the court.

1. Abortion rulings

The Court decided 2 abortion cases and rejected a request to hear a third.
National Institute of Family and Life Advocates v Becerra
In this case,1 the Court struck down a California law that required pregnancy crisis centers not offering abortions (generally operated by pro-life groups) to provide special notices to clients.2
At stake. These notices would inform clients that California provides free or low-cost services, including abortions, and provide a phone number to call for those services.
There were many amicus briefs filed in this case, including those by the American College of Obstetricians and Gynecologists (ACOG) and other specialty boards,3 as well as the American Association of Pro-Life Obstetricians and Gynecologists and other pro-life organizations.4 ACOG’s brief argued that the California-required notice facilitates the goal of allowing women to receive medical services without harmful delay.
Final ruling. The Court held that the law required clinics to engage in speech with which the clinics disagreed (known as “compelled speech”). It also noted that California disclosure requirements were “wildly underinclusive” because they apply only to some clinics. The majority felt that there was no strong state interest in compelling this speech because there were other alternatives for the state to provide information about the availability of abortion and other services. The Court found that the clinics were likely to succeed on the merits of their claims of a First Amendment (free speech) violation.
Right to abortion for illegal immigrants in custody
A very unusual abortion case involved “Jane Doe,” a minor who was at 8 weeks’ gestation when she illegally crossed the border into the United States.5 She was placed in a federally-funded shelter where she requested an abortion. The facility denied that request.
At stake. Legal argument ensued about releasing her to another facility for an abortion, as the argument was made that pregnant minors who are apprehended crossing into the United States illegally and placed into the custody of federal officials should have abortion access. A lower Court of Appeals ruled against the Trump Administration’s policy of denying abortions to undocumented minors in federal custody. During the process of the federal government taking the case to the Supreme Court, the attorneys for Doe moved appointments around and, without notice, the abortion was performed. Government attorneys said that Doe’s attorneys made “what appear to be material misrepresentations and omissions” designed to “thwart [the Supreme Court’s] review” of the case.5 The government requested that the Court vacate the order of the Court of Appeals so that it could not be used as precedent.
Final ruling. The Court granted the governments request to vacate the lower court’s order because the minor was no longer pregnant and the order was therefore moot. The basic issue in this case (the right of in-custody minors to access abortions) remains unresolved. It is likely to appear before the Court in the future.
Continue to: Access to medical abortions
Access to medical abortions
An Arkansas law requires that a physician administering medical abortions contract with a physician who has admitting privileges at a hospital (a “contracted physician”).
At stake. Planned Parenthood filed suit challenging the requirement as unnecessary and harmful because it would result in the closure of 2 of the 3 abortion providers in Arkansas. ACOG filed an amicus brief urging the Supreme Court to consider the case.6 (Technically this was a petition for a Writ of Certiorari, the procedure by which the Court accepts cases. It accepts only about 1% of applications.) ACOG argued that there was no medical reason for the contracted physician requirement, and noted the harm it would do to women who would not have access to abortions.
Final ruling. On May 29, 2018, the Court declined to hear the case. This case is still active in the lower courts and may eventually return to the Supreme Court.

2. The patent system

The medical profession depends on the patent system to encourage the discovery of new patents efficiently and effectively. In 2012, Congress passed the America Invents Act7 that authorizes a petition by anyone other than the patent holder to the Patent and Trademark Office (PTO) for an “inter partes review” to assess a challenge to the patent’s legitimacy. If the PTO determines that there may be merit to the claim, the Patent Trial and Appeal Board undertakes a trial-like review process that may validate, invalidate, or amend the patent. The Board’s decision is subject to appellate court review.
At stake. This term, the inter partes review was challenged as unconstitutional on technical bases.8
Final ruling. The Court rejected this claim and approved the current administrative inter partes review process. The Court determined that once the Patent Office takes a petition challenging a patent, it must decide all of the claims against the patent, not pick and choose which elements of the challenge to evaluate.9 The Court’s decision upheld patent-review reform, but will require the Patent Office to tweak its procedures.

3. The travel ban

ACOG, the American Medical Association (AMA), the Association of American Medical Colleges, and more than 30 other health care and specialty associations filed an amicus brief regarding one of the most anticipated cases of the term—the “travel ban.”10
At stake. The essential argument of these organizations was that the US health care system depends on professionals from other countries. An efficient and fair immigration program is, therefore, important to advance the nation’s “health security.” During the 2016−2017 term, the Court considered but then removed the issue from its calendar when the Trump Administration issued a revised travel ban.11
In September 2017, President Trump’s proclamation imposed a range of entry restrictions on the citizens of 8 countries, most (but not all) of which are predominantly Muslim. The government indicated that, in a study by Homeland Security and the State Department, these countries were identified as having especially deficient information-sharing practices and presented national security concerns. Trump v Hawaii12 challenged this proclamation.
Final ruling. The majority of the Court upheld the travel ban. For the 5-Justice majority led by Chief Justice Roberts, the case came down to 3 things:
- The Constitution and the laws passed by Congress of necessity give the President great authority to engage in foreign policy, including policies regarding entry into the country.
- The courts are very reluctant to get into the substance of foreign affairs—they are not equipped to know in detail what the facts are, and things change very fast.
- If courts start tinkering with foreign policy and things turn bad, it will appear that the courts are to blame and were interfering in an area about which they are not competent.
Continue to: 4. Did a credit card case add risk to health insurance markets?

It was just a credit card case, but one in which the AMA saw a real risk to regulation of the health insurance markets.
At stake. Technically, Ohio v American Express concerned a claim that American Express (AmEx) violated antitrust laws when it prohibited merchants taking its credit card from “steering” customers to cards with lower fees.13 AmEx maintained that, because credit cards were a special kind of “2-sided” market (connecting merchants on one side and customers on the other), antitrust laws should not be strictly enforced.
The AMA noticed that special rules regarding 2-sided markets might apply to health insurance, and it submitted an amicus brief14 that noted: “dominant health insurance networks … have imposed and could further impose rules or effectively erect barriers that prohibit physicians from referring patients to certain specialists, particularly out-of-network specialists, for innovative and even necessary medical tests.”14 It concluded that the antitrust rule AmEx was suggesting would make it nearly impossible to challenge these unfair provisions in health insurance arrangements.
Final ruling. The Court, however, accepted the AmEx position, making it very difficult to develop an antitrust case against 2-sided markets. It remains to be seen the degree to which the AMA concern about health insurance markets will be realized.

5. Gay wedding and a bakeshop

At stake. In Masterpiece Cakeshop v Colorado, a cakemaker declined to design a cake for a gay wedding and had been disciplined under Colorado law for discriminating against the couple based on sexual orientation.15
Final ruling. The Court, however, found that the Colorado regulators had, ironically, shown such religious animus in the way they treated the baker that the regulators themselves had discriminated on the basis of religion. As a result, the Court reversed the sanctions against the baker.
This decision was fairly narrow. It does not, for example, stand for the proposition that there may be a general religious exception to antidiscrimination laws. The question of broader religious or free-speech objections to antidiscrimination laws remains for another time.
Amicus brief. It was interesting that the American College of Pediatricians, American Association of Pro-Life Obstetricians and Gynecologists, and others, filed an amicus brief to report with concern the “demands that individual medical professionals must perform, assist with, or facilitate abortions, without regard to the teachings of their own faiths, consciences, and convictions.”16 The brief also noted that “issues in the present case implicate the fundamental rights of health care professionals, and to respectfully urge that the Court should by no means permit any weakening or qualification of well-established protections against compelled speech, and of free exercise” of religion.16
Arbitration. The Court upheld, as it has in most recent terms, another arbitration agreement.1 This case concerned an employment agreement in which employees consented to submit to arbitration rather than file lawsuits and not use class action claims.
Search of cell-phone location. Cell phones, whenever turned on, connect with cell towers that record the phone’s location several times a minute. Cell companies store this information, creating a virtual map of where the owner is at all times. The Federal Bureau of Investigation asked a cell company for location information for several people during a 127-day period in which robberies were committed.2 The Court held that the search was illegal in the absence of a warrant.
Public employee unions. The Court held that agency (fair share) fees, in which public employees who are not union members can be required to pay dues for the bargaining and grievance activities (from which they generally benefit), violate the First Amendment. The majority held that forcing public employees to pay fees to unions requires the employees, through those fees, to engage in political activities with which they disagree.3 This is a form of compelled speech, which the Court found violates the First Amendment. Health care professionals who are public employees in positions that have union representation will probably have the opportunity to opt out of agency agreements.
Internet sales tax. The Court permitted states to charge sales tax on out-of-state Internet purchases.4 In doing so, a state may require out-of-state companies to collect taxes on sales to its residents.
References
- Epic Systems Corp. v Lewis, 584 US 16 285 (2018).
- Carpenter v United States, 585 US 16 402 (2018).
- Janus v State, County, and Municipal Employees, 585 US 16 1466 (2018).
- South Dakota v Wayfair, Inc, 585 US 17 494 (2018).
Clues to the future
During the term that ran from October 2, 2017, through June 27, 2018, the Court issued 72 decisions. An unusually high proportion of cases (26%; 19 cases) were decided on a 5 to 4 vote. Last term, the rate of 5 to 4 decisions was 10%; the 6-year average was 18%. The unanimous decision rate was 39% this term, compared with 59% last term, and 50% on average.
The rate of 5 to 4 cases provides a clue about the Court’s general direction. The number of times each Justice was in the majority in those nineteen 5 to 4 decisions included: Chief Justice Roberts, 17; and Justices Kennedy, 16; Gorsuch, 16; Thomas, 15; and Alito, 15; compared with Justices Ginsburg, 5; Breyer, 4; Sotomayor, 4; and Kagan, 3.
The Court convened on October 1, 2018. At this writing, whether the new term starts with 8 or 9 justices remains a question. President Trump nominated Brett Kavanaugh, JD, to take Justice Kennedy’s place on the Court. His professional qualifications and experience appear to make him qualified for a position on the Court, but as we have seen, there are many other elements that go into confirming a Justice’s nomination.
Justice Anthony Kennedy was the deciding vote in the overwhelming majority of the 5 to 4 decisions in 20 of his 30 years on the Court. The areas in which he had an especially important impact include1:
- Gay rights. Justice Kennedy wrote the opinions (usually 5 to 4 decisions) in a number of groundbreaking gay-rights cases, including decriminalizing homosexual conduct, striking down the Defense of Marriage Act, and finding that the Constitution requires states to recognize gay marriage.
- The death penalty. Justice Kennedy wrote decisions that prohibited states from imposing the death penalty for any crime other than murder, for defendants who were under 18 when they committed the crime, and for defendants with serious developmental disabilities. He expressed reservations about long-term solitary confinement, but did not have a case that allowed him to decide its constitutionality.
- The First Amendment. Early in his service on the Court, he held that the First Amendment protected flag burning as a form of speech. He decided many important freespeech and freedom-of-religion cases that have set a standard for protecting those fundamental freedoms.
- Use of health and social science data. Justice Kennedy was more open to mental health information and cited it more often than most other Justices.
- Abortion rights? Many commentators would add protecting the right to choose to have an abortion to the above list. Justice Kennedy was a central figure in one case that declined to back away from Roe v Wade, and joined a more recent decision that struck down a Texas law that created an undue burden on women seeking abortion. Plus, he also voted to uphold abortion restrictions, such as “partial-birth-abortion laws.” So there is a good argument for including abortion rights on the list, although he did not break new ground.
Justice Kennedy as a person
Outside the courtroom, Justice Kennedy is a person of great warmth and compassion. He is a natural teacher and spends a great deal of time with students. When asked how he would like to be remembered, Justice Kennedy once replied, “Somebody who’s decent, and honest, and fair, and who’s absolutely committed to the proposition that freedom is America’s gift to the rest of the world.” I agree with that assessment.
STEVEN R. SMITH, MS, JD
Reference
- South Dakota v Wayfair, Inc, 585 US (2018)
Next term, the Court is scheduled to hear cases regarding pharmaceutical liability, double jeopardy, sex-offender registration, expert witnesses, Social Security disability benefits, and the Age Discrimination in Employment Act. There will be at least 3 arbitration cases. Health care and reproductive rights will continue to be an important part of the Court’s docket.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The 2017−2018 term of the Supreme Court of the United States (SCOTUS) was momentous. Justice Anthony Kennedy, who had been the deciding vote in most of the 5 to 4 cases for a generation, announced his retirement as of July 31, 2018. In addition, the Court decided a number of cases of interest to ObGyns. In this article we review some of those cases, as well as consider the future of the Court without Justice Kennedy. In selecting cases, we have given special attention to those in which national medical organizations filed amicus briefs. These “amicus curiae” or “friend of the court” briefs are filed by an entity who is not party to a case but wants to provide information or views to the court.

1. Abortion rulings

The Court decided 2 abortion cases and rejected a request to hear a third.
National Institute of Family and Life Advocates v Becerra
In this case,1 the Court struck down a California law that required pregnancy crisis centers not offering abortions (generally operated by pro-life groups) to provide special notices to clients.2
At stake. These notices would inform clients that California provides free or low-cost services, including abortions, and provide a phone number to call for those services.
There were many amicus briefs filed in this case, including those by the American College of Obstetricians and Gynecologists (ACOG) and other specialty boards,3 as well as the American Association of Pro-Life Obstetricians and Gynecologists and other pro-life organizations.4 ACOG’s brief argued that the California-required notice facilitates the goal of allowing women to receive medical services without harmful delay.
Final ruling. The Court held that the law required clinics to engage in speech with which the clinics disagreed (known as “compelled speech”). It also noted that California disclosure requirements were “wildly underinclusive” because they apply only to some clinics. The majority felt that there was no strong state interest in compelling this speech because there were other alternatives for the state to provide information about the availability of abortion and other services. The Court found that the clinics were likely to succeed on the merits of their claims of a First Amendment (free speech) violation.
Right to abortion for illegal immigrants in custody
A very unusual abortion case involved “Jane Doe,” a minor who was at 8 weeks’ gestation when she illegally crossed the border into the United States.5 She was placed in a federally-funded shelter where she requested an abortion. The facility denied that request.
At stake. Legal argument ensued about releasing her to another facility for an abortion, as the argument was made that pregnant minors who are apprehended crossing into the United States illegally and placed into the custody of federal officials should have abortion access. A lower Court of Appeals ruled against the Trump Administration’s policy of denying abortions to undocumented minors in federal custody. During the process of the federal government taking the case to the Supreme Court, the attorneys for Doe moved appointments around and, without notice, the abortion was performed. Government attorneys said that Doe’s attorneys made “what appear to be material misrepresentations and omissions” designed to “thwart [the Supreme Court’s] review” of the case.5 The government requested that the Court vacate the order of the Court of Appeals so that it could not be used as precedent.
Final ruling. The Court granted the governments request to vacate the lower court’s order because the minor was no longer pregnant and the order was therefore moot. The basic issue in this case (the right of in-custody minors to access abortions) remains unresolved. It is likely to appear before the Court in the future.
Continue to: Access to medical abortions
Access to medical abortions
An Arkansas law requires that a physician administering medical abortions contract with a physician who has admitting privileges at a hospital (a “contracted physician”).
At stake. Planned Parenthood filed suit challenging the requirement as unnecessary and harmful because it would result in the closure of 2 of the 3 abortion providers in Arkansas. ACOG filed an amicus brief urging the Supreme Court to consider the case.6 (Technically this was a petition for a Writ of Certiorari, the procedure by which the Court accepts cases. It accepts only about 1% of applications.) ACOG argued that there was no medical reason for the contracted physician requirement, and noted the harm it would do to women who would not have access to abortions.
Final ruling. On May 29, 2018, the Court declined to hear the case. This case is still active in the lower courts and may eventually return to the Supreme Court.

2. The patent system

The medical profession depends on the patent system to encourage the discovery of new patents efficiently and effectively. In 2012, Congress passed the America Invents Act7 that authorizes a petition by anyone other than the patent holder to the Patent and Trademark Office (PTO) for an “inter partes review” to assess a challenge to the patent’s legitimacy. If the PTO determines that there may be merit to the claim, the Patent Trial and Appeal Board undertakes a trial-like review process that may validate, invalidate, or amend the patent. The Board’s decision is subject to appellate court review.
At stake. This term, the inter partes review was challenged as unconstitutional on technical bases.8
Final ruling. The Court rejected this claim and approved the current administrative inter partes review process. The Court determined that once the Patent Office takes a petition challenging a patent, it must decide all of the claims against the patent, not pick and choose which elements of the challenge to evaluate.9 The Court’s decision upheld patent-review reform, but will require the Patent Office to tweak its procedures.

3. The travel ban

ACOG, the American Medical Association (AMA), the Association of American Medical Colleges, and more than 30 other health care and specialty associations filed an amicus brief regarding one of the most anticipated cases of the term—the “travel ban.”10
At stake. The essential argument of these organizations was that the US health care system depends on professionals from other countries. An efficient and fair immigration program is, therefore, important to advance the nation’s “health security.” During the 2016−2017 term, the Court considered but then removed the issue from its calendar when the Trump Administration issued a revised travel ban.11
In September 2017, President Trump’s proclamation imposed a range of entry restrictions on the citizens of 8 countries, most (but not all) of which are predominantly Muslim. The government indicated that, in a study by Homeland Security and the State Department, these countries were identified as having especially deficient information-sharing practices and presented national security concerns. Trump v Hawaii12 challenged this proclamation.
Final ruling. The majority of the Court upheld the travel ban. For the 5-Justice majority led by Chief Justice Roberts, the case came down to 3 things:
- The Constitution and the laws passed by Congress of necessity give the President great authority to engage in foreign policy, including policies regarding entry into the country.
- The courts are very reluctant to get into the substance of foreign affairs—they are not equipped to know in detail what the facts are, and things change very fast.
- If courts start tinkering with foreign policy and things turn bad, it will appear that the courts are to blame and were interfering in an area about which they are not competent.
Continue to: 4. Did a credit card case add risk to health insurance markets?

It was just a credit card case, but one in which the AMA saw a real risk to regulation of the health insurance markets.
At stake. Technically, Ohio v American Express concerned a claim that American Express (AmEx) violated antitrust laws when it prohibited merchants taking its credit card from “steering” customers to cards with lower fees.13 AmEx maintained that, because credit cards were a special kind of “2-sided” market (connecting merchants on one side and customers on the other), antitrust laws should not be strictly enforced.
The AMA noticed that special rules regarding 2-sided markets might apply to health insurance, and it submitted an amicus brief14 that noted: “dominant health insurance networks … have imposed and could further impose rules or effectively erect barriers that prohibit physicians from referring patients to certain specialists, particularly out-of-network specialists, for innovative and even necessary medical tests.”14 It concluded that the antitrust rule AmEx was suggesting would make it nearly impossible to challenge these unfair provisions in health insurance arrangements.
Final ruling. The Court, however, accepted the AmEx position, making it very difficult to develop an antitrust case against 2-sided markets. It remains to be seen the degree to which the AMA concern about health insurance markets will be realized.

5. Gay wedding and a bakeshop

At stake. In Masterpiece Cakeshop v Colorado, a cakemaker declined to design a cake for a gay wedding and had been disciplined under Colorado law for discriminating against the couple based on sexual orientation.15
Final ruling. The Court, however, found that the Colorado regulators had, ironically, shown such religious animus in the way they treated the baker that the regulators themselves had discriminated on the basis of religion. As a result, the Court reversed the sanctions against the baker.
This decision was fairly narrow. It does not, for example, stand for the proposition that there may be a general religious exception to antidiscrimination laws. The question of broader religious or free-speech objections to antidiscrimination laws remains for another time.
Amicus brief. It was interesting that the American College of Pediatricians, American Association of Pro-Life Obstetricians and Gynecologists, and others, filed an amicus brief to report with concern the “demands that individual medical professionals must perform, assist with, or facilitate abortions, without regard to the teachings of their own faiths, consciences, and convictions.”16 The brief also noted that “issues in the present case implicate the fundamental rights of health care professionals, and to respectfully urge that the Court should by no means permit any weakening or qualification of well-established protections against compelled speech, and of free exercise” of religion.16
Arbitration. The Court upheld, as it has in most recent terms, another arbitration agreement.1 This case concerned an employment agreement in which employees consented to submit to arbitration rather than file lawsuits and not use class action claims.
Search of cell-phone location. Cell phones, whenever turned on, connect with cell towers that record the phone’s location several times a minute. Cell companies store this information, creating a virtual map of where the owner is at all times. The Federal Bureau of Investigation asked a cell company for location information for several people during a 127-day period in which robberies were committed.2 The Court held that the search was illegal in the absence of a warrant.
Public employee unions. The Court held that agency (fair share) fees, in which public employees who are not union members can be required to pay dues for the bargaining and grievance activities (from which they generally benefit), violate the First Amendment. The majority held that forcing public employees to pay fees to unions requires the employees, through those fees, to engage in political activities with which they disagree.3 This is a form of compelled speech, which the Court found violates the First Amendment. Health care professionals who are public employees in positions that have union representation will probably have the opportunity to opt out of agency agreements.
Internet sales tax. The Court permitted states to charge sales tax on out-of-state Internet purchases.4 In doing so, a state may require out-of-state companies to collect taxes on sales to its residents.
References
- Epic Systems Corp. v Lewis, 584 US 16 285 (2018).
- Carpenter v United States, 585 US 16 402 (2018).
- Janus v State, County, and Municipal Employees, 585 US 16 1466 (2018).
- South Dakota v Wayfair, Inc, 585 US 17 494 (2018).
Clues to the future
During the term that ran from October 2, 2017, through June 27, 2018, the Court issued 72 decisions. An unusually high proportion of cases (26%; 19 cases) were decided on a 5 to 4 vote. Last term, the rate of 5 to 4 decisions was 10%; the 6-year average was 18%. The unanimous decision rate was 39% this term, compared with 59% last term, and 50% on average.
The rate of 5 to 4 cases provides a clue about the Court’s general direction. The number of times each Justice was in the majority in those nineteen 5 to 4 decisions included: Chief Justice Roberts, 17; and Justices Kennedy, 16; Gorsuch, 16; Thomas, 15; and Alito, 15; compared with Justices Ginsburg, 5; Breyer, 4; Sotomayor, 4; and Kagan, 3.
The Court convened on October 1, 2018. At this writing, whether the new term starts with 8 or 9 justices remains a question. President Trump nominated Brett Kavanaugh, JD, to take Justice Kennedy’s place on the Court. His professional qualifications and experience appear to make him qualified for a position on the Court, but as we have seen, there are many other elements that go into confirming a Justice’s nomination.
Justice Anthony Kennedy was the deciding vote in the overwhelming majority of the 5 to 4 decisions in 20 of his 30 years on the Court. The areas in which he had an especially important impact include1:
- Gay rights. Justice Kennedy wrote the opinions (usually 5 to 4 decisions) in a number of groundbreaking gay-rights cases, including decriminalizing homosexual conduct, striking down the Defense of Marriage Act, and finding that the Constitution requires states to recognize gay marriage.
- The death penalty. Justice Kennedy wrote decisions that prohibited states from imposing the death penalty for any crime other than murder, for defendants who were under 18 when they committed the crime, and for defendants with serious developmental disabilities. He expressed reservations about long-term solitary confinement, but did not have a case that allowed him to decide its constitutionality.
- The First Amendment. Early in his service on the Court, he held that the First Amendment protected flag burning as a form of speech. He decided many important freespeech and freedom-of-religion cases that have set a standard for protecting those fundamental freedoms.
- Use of health and social science data. Justice Kennedy was more open to mental health information and cited it more often than most other Justices.
- Abortion rights? Many commentators would add protecting the right to choose to have an abortion to the above list. Justice Kennedy was a central figure in one case that declined to back away from Roe v Wade, and joined a more recent decision that struck down a Texas law that created an undue burden on women seeking abortion. Plus, he also voted to uphold abortion restrictions, such as “partial-birth-abortion laws.” So there is a good argument for including abortion rights on the list, although he did not break new ground.
Justice Kennedy as a person
Outside the courtroom, Justice Kennedy is a person of great warmth and compassion. He is a natural teacher and spends a great deal of time with students. When asked how he would like to be remembered, Justice Kennedy once replied, “Somebody who’s decent, and honest, and fair, and who’s absolutely committed to the proposition that freedom is America’s gift to the rest of the world.” I agree with that assessment.
STEVEN R. SMITH, MS, JD
Reference
- South Dakota v Wayfair, Inc, 585 US (2018)
Next term, the Court is scheduled to hear cases regarding pharmaceutical liability, double jeopardy, sex-offender registration, expert witnesses, Social Security disability benefits, and the Age Discrimination in Employment Act. There will be at least 3 arbitration cases. Health care and reproductive rights will continue to be an important part of the Court’s docket.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- National Institute of Family and Life Advocates v Becerra, 585 US 16 1140 (2018).
- California Reproductive Freedom, Accountability, Comprehensive Care, and Transparency Act (FACT Act), Cal. Health & Safety Code Ann. §123470 et seq. (West 2018).
- Brief amici curiae of American Academy of Pediatrics, et al. in National Institute of Family and Life Advocates v Becerra, February 27, 2018.
- Brief amici curiae of American Association of Pro-Life Obstetricians & Gynecologists, et al. in National Institute of Family and Life Advocates v Becerra, January 16, 2018.
- Azar v Garza, 584 US 17 654 (2018).
- Brief amici curiae of American College of Obstetricians and Gynecologists and American Public Health Association in Planned Parenthood of Arkansas and Eastern Oklahoma v Jegley, February 1, 2018.
- Chapter 31, Inter Partes Review. United States Code. Title 35: Patents. Part III, Patents and protection of patents. 2012 Ed. 35 USC 311–319.
- Oil States Energy Services, LLC v Greene’s Energy Group, LLC, 584 US 16 712 (2018).
- SAS Institute Inc. v Iancu, 584 US 16 969 (2018).
- Brief for Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents, Trump v Hawaii. https://www.supremecourt.gov/Docket PDF/17/ 17-965/40128/20180327105855912_17-965%20Amicus%20Br.%20Proclamation.pdf. Accessed September 21, 2018.
- Smith SR, Sanfilippo JS. Supreme Court decisions in 2017 that affected your practice. OBG Manag. 2017;29(12)44–47.
- Trump v Hawaii, 585 US 17 965 (2018).
- Ohio v American Express Co, 585 US 16 1454 (2018).
- Brief amici curiae of American Medical Association and Ohio State Medical Association in Ohio v American Express, December 24, 2017.
- Masterpiece Cakeshop, Ltd. v Colorado Civil Rights Commission, 584 US 16 111 (2018).
- Brief amici curiae of American College of Pediatricians, et al. in Masterpiece Cakeshop v Colorado Civil Rights Commission, September 7, 2017.
- National Institute of Family and Life Advocates v Becerra, 585 US 16 1140 (2018).
- California Reproductive Freedom, Accountability, Comprehensive Care, and Transparency Act (FACT Act), Cal. Health & Safety Code Ann. §123470 et seq. (West 2018).
- Brief amici curiae of American Academy of Pediatrics, et al. in National Institute of Family and Life Advocates v Becerra, February 27, 2018.
- Brief amici curiae of American Association of Pro-Life Obstetricians & Gynecologists, et al. in National Institute of Family and Life Advocates v Becerra, January 16, 2018.
- Azar v Garza, 584 US 17 654 (2018).
- Brief amici curiae of American College of Obstetricians and Gynecologists and American Public Health Association in Planned Parenthood of Arkansas and Eastern Oklahoma v Jegley, February 1, 2018.
- Chapter 31, Inter Partes Review. United States Code. Title 35: Patents. Part III, Patents and protection of patents. 2012 Ed. 35 USC 311–319.
- Oil States Energy Services, LLC v Greene’s Energy Group, LLC, 584 US 16 712 (2018).
- SAS Institute Inc. v Iancu, 584 US 16 969 (2018).
- Brief for Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents, Trump v Hawaii. https://www.supremecourt.gov/Docket PDF/17/ 17-965/40128/20180327105855912_17-965%20Amicus%20Br.%20Proclamation.pdf. Accessed September 21, 2018.
- Smith SR, Sanfilippo JS. Supreme Court decisions in 2017 that affected your practice. OBG Manag. 2017;29(12)44–47.
- Trump v Hawaii, 585 US 17 965 (2018).
- Ohio v American Express Co, 585 US 16 1454 (2018).
- Brief amici curiae of American Medical Association and Ohio State Medical Association in Ohio v American Express, December 24, 2017.
- Masterpiece Cakeshop, Ltd. v Colorado Civil Rights Commission, 584 US 16 111 (2018).
- Brief amici curiae of American College of Pediatricians, et al. in Masterpiece Cakeshop v Colorado Civil Rights Commission, September 7, 2017.
Lessons from a daunting malpractice event
CASE Failure to perform cesarean delivery1–4
A 19-year-old woman (G1P0) received prenatal care at a federally funded health center. Her pregnancy was normal without complications. She presented to the hospital after spontaneous rupture of membranes (SROM). The on-call ObGyn employed by the clinic was offsite when the mother was admitted.
The mother signed a standard consent form for vaginal and cesarean deliveries and any other surgical procedure required during the course of giving birth.
The ObGyn ordered low-dose oxytocin to augment labor in light of her SROM. Oxytocin was started at 9:46
Upon delivery, the infant was flaccid and not breathing. His Apgar scores were 2, 3, and 6 at 1, 5, and 10 minutes, respectively, and the cord pH was 7. The neonatal intensive care (NICU) team provided aggressive resuscitation.
At the time of trial, the 18-month-old boy was being fed through a percutaneous endoscopic gastrostomy tube and had a tracheostomy that required periodic suctioning. The child was not able to stand, crawl, or support himself, and will require 24-hour nursing care for the rest of his life.
LAWSUIT. The parents filed a lawsuit in federal court for damages under the Federal Tort Claims Act (see “Notes about this case,”). The mother claimed that she had requested a cesarean delivery early in labor when FHR tracings showed fetal distress, and again prior to vacuum extraction; the ObGyn refused both times.
The ObGyn claimed that when he noted a category III tracing, he recommended cesarean delivery, but the patient refused. He recorded the refusal in the chart some time later, after he had noted the neonate’s appearance.
The parents’ expert testified that restarting oxytocin and using vacuum extraction multiple times were dangerous and gross deviations from acceptable practice. Prolonged and repetitive use of the vacuum extractor caused a large subgaleal hematoma that decreased blood flow to the fetal brain, resulting in irreversible central nervous system (CNS) damage secondary to hypoxic ischemic encephalopathy. An emergency cesarean delivery should have been performed at the first sign of fetal distress.
The defense expert pointed out that the ObGyn discussed the need for cesarean delivery with the patient when fetal distress occurred and that the ObGyn was bedside and monitoring the fetus and the mother. Although the mother consented to a cesarean delivery at time of admission, she refused to allow the procedure.
The labor and delivery (L&D) nurse corroborated the mother’s story that a cesarean delivery was not offered by the ObGyn, and when the patient asked for a cesarean delivery, he refused. The nurse stated that the note added to the records by the ObGyn about the mother’s refusal was a lie. If the mother had refused a cesarean, the nurse would have documented the refusal by completing a Refusal of Treatment form that would have been faxed to the risk manager. No such form was required because nothing was ever offered that the mother refused.
The nurse also testified that during the course of the latter part of labor, the ObGyn left the room several times to assist other patients, deliver another baby, and make an 8-minute phone call to his stockbroker. She reported that the ObGyn was out of the room when delivery occurred.
WHAT’S THE VERDICT?
Read about the verdict and medical considerations.
WHAT’S THE VERDICT?
The medical care and the federal-court bench trial held in front of a judge (not a jury) occurred in Florida. The verdict suggests that the ObGyn breached the standard of care by not offering or proceeding with a cesarean delivery and this management resulted in the child’s injuries. The court awarded damages in the amount of $33,813,495.91, including $29,413,495.91 for the infant; $3,300,000.00 for the plaintiff; and $1,100,000.00 for her spouse.4
Medical considerations
Refusal of medical care
Although it appears that in this case the patient did not actually refuse medical care (cesarean delivery), the case does raise the question of refusal. Refusal of medical care has been addressed by the American College of Obstetricians and Gynecologists (ACOG) predicated upon care that supports maternal and fetal wellbeing.5 There may be a fine balance between safeguarding the pregnant woman’s autonomy and optimization of fetal wellbeing. “Forced compliance,” on the other hand, is the alternative to respecting refusal of treatment. Ethical issues come into play: patient rights; respect for autonomy; violations of bodily integrity; power differentials; and gender equality.5 The use of coercion is “not only ethically impermissible but also medically inadvisable secondary to the realities of prognostic uncertainty and the limitations of medical knowledge.”5 There is an obligation to elicit the patient’s reasoning and lived experience. Perhaps most importantly, as clinicians working to achieve a resolution, consideration of the following is appropriate5:
- reliability and validity of evidence-based medicine
- severity of the prospective outcome
- degree of risk or burden placed on the patient
- patient understanding of the gravity of the situation and risks
- degree of urgency.
Much of this boils down to the obligation to discuss “risks and benefits of treatment, alternatives and consequences of refusing treatment.”6
Complications from vacuum-assisted vaginal delivery
Ghidini and associates, in a multicenter retrospective study, evaluated complications relating to vacuum-assisted delivery. They listed major primary outcomes of subgaleal hemorrhage, skull fracture, and intracranial bleeding, and minor primary outcomes of cephalohematoma, scalp laceration, and extensive skin abrasions. Secondary outcomes included a 5-minute Apgar score of <7, umbilical artery pH of <7.10, shoulder dystocia, and NICU admission.7
A retrospective study from Sweden assessing all vacuum deliveries over a 2-year period compared the use of the Kiwi OmniCup (Clinical Innovations) to use of the Malmström metal cup (Medela). No statistical differences in maternal or neonatal outcomes as well as failure rates were noted. However, the duration of the procedure was longer and the requirement for fundal pressure was higher with the Malmström device.8
Subgaleal hemorrhage. Ghidini and colleagues reported a heightened incidence of head injury related to the duration of vacuum application and birth weight.7 Specifically, vacuum delivery devices increase the risk of subgaleal hemorrhage. Blood can accumulate between the scalp’s epicranial aponeurosis and the periosteum and potentially can extend forward to the orbital margins, backward to the nuchal ridge, and laterally to the temporal fascia. As much as 260 mL of blood can get into this subaponeurotic space in term babies.9 Up to one-quarter of babies who require NICU admission for this condition die.10 This injury seldom occurs with forceps.
Shoulder dystocia. In a meta-analysisfrom Italy, the vacuum extractor was associated with increased risk of shoulder dystocia compared with spontaneous vaginal delivery.11
Intrapartum hypoxia. In 2003, the ACOG Task Force on Neonatal Encephalopathy and Cerebral Palsy defined an acute intrapartum hypoxic event (TABLE).12
Cerebral palsy (CP) is defined as “a chronic neuromuscular disability characterized by aberrant control of movement or posture appearing early in life and not the result of recognized progressive disease.”13,14
The Collaborative Perinatal Project concluded that birth trauma plays a minimal role in development of CP.15 Arrested labor, use of oxytocin, or prolonged labor did not play a role. CP can develop following significant cerebral or posterior fossa hemorrhage in term infants.16
Perinatal asphyxia is a poor and imprecise term and use of the expression should be abandoned. Overall, 90% of children with CP do not have birth asphyxia as the underlying etiology.14
Prognostic assessment can be made, in part, by using the Sarnat classification system (classification scale for hypoxic-ischemic encephalopathy of the newborn) or an electroencephalogram to stratify the severity of neonatal encephalopathy.12 Such tests are not stand-alone but a segment of assessment. At this point “a better understanding of the processes leading to neonatal encephalopathy and associated outcomes” appear to be required to understand and associate outcomes.12 “More accurate and reliable tools (are required) for prognostic forecasting.”12
Hypoxic-ischemic encephalopathy involves multisystem organ failure including renal, hepatic, hematologic, cardiac, gastrointestinal, and metabolic abnormalities. There is no correlation between the degree of CNS injury and level of other organ abnormalities.12
Differential diagnosis
When events such as those described in this case occur, develop a differential diagnosis by considering the following12:
- uterine rupture
- severe placental abruption
- umbilical cord prolapse
- amniotic fluid embolus
- maternal cardiovascular collapse
- fetal exsanguination.
Read about the legal considerations.
Legal considerations
Although ObGyns are among the specialties most likely to experience malpractice claims,17 a verdict of more than $33 million is unusual.18 Despite the failure of adequate care, and the enormous damages, the ObGyn involved probably will not be responsible for paying the verdict (see “Notes about this case”). The case presents a number of important lessons and reminders for anyone practicing obstetrics.
A procedural comment
The case in this article arose under the Federal Tort Claims Act (FTCA).1 Most government entities have sovereign immunity, meaning that they can be sued only with their consent. In the FTCA, the federal government consented to being sued for the acts of its employees. This right has a number of limitations and some technical procedures, but at its core, it permits the United States to be sued as though it was a private individual.2 Private individuals can be sued for the acts of the agents (including employees).
Although the FTCA is a federal law, and these cases are tried in federal court, the substantive law of the state applies. This case occurred in Florida, so Florida tort law, defenses, and limitation on claims applied here also. Had the events occurred in Iowa, Iowa law would have applied.
In FTCA cases, the United States is the defendant (generally it is the government, not the employee who is the defendant).3 In this case, the ObGyn was employed by a federal government entity to provide delivery services. As a result, the United States was the primary defendant, had the obligation to defend the suit, and will almost certainly be obligated to pay the verdict.
The case facts
Although this description is based on an actual case, the facts were taken from the opinion of the trial court, legal summaries and press reports and not from the full case documents.4-7 We could not independently assess the accuracy of the facts, but for the purpose of this discussion, we have assumed the facts to be correct. The government has apparently filed an appeal in the Eleventh Circuit.
References
- Federal Tort Claims Act. Vol 28 U.S.C. Pt.VI Ch.171 and 28 U.S.C. § 1346(b).
- About the Federal Tort Claims Act (FTCA). Health Resources & Services Administration: Health Center Program. https://bphc.hrsa.gov/ftca/about/index.html. Accessed May 16, 2018.
- Dowell MA, Scott CD. Federally Qualified Health Center Federal Tort Claims Act Insurance Coverage. Health Law. 2015;5:31-43.
- Chang D. Miami doctor's call to broker during baby's delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed January 11, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17-18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
Very large verdict
The extraordinary size of this verdict ($33 million without any punitive damages) is a reminder that in obstetrics, mistakes can have catastrophic consequences and very high costs.19 This fact is reflected in malpractice insurance rates.
A substantial amount of this case’s award will provide around-the-clock care for the child. This verdict was not the result of a runaway jury—it was a judge’s decision. It is also noteworthy to report that a small percentage of physicians (1%) appear responsible for a significant number (about one-third) of paid claims.20
Although the size of the verdict is unusual, the case is a fairly straightforward negligence tort. The judge found that the ObGyn had breached the duty of care for his patient. The actions that fell below the standard of care included restarting the oxytocin, using the Kiwi vacuum device 3 times, and failing to perform a cesarean delivery in light of obvious fetal distress. That negligence caused injury to the infant (and his parents).21 The judge determined that the 4 elements of negligence were present: 1) duty of care, 2) breach of that duty, 3) injury, and 4) a causal link between the breach of duty and the injury. The failure to adhere to good practice standards practically defines breach of duty.22
Multitasking
One important lesson is that multitasking, absence, and inattention can look terrible when things go wrong. Known as “hindsight bias,” the awareness that there was a disastrous result makes it easier to attribute the outcome to small mistakes that otherwise might seem trivial. This ObGyn was in and out of the room during a difficult labor. Perhaps that was understandable if it were unavoidable because of another delivery, but being absent frequently and not present for the delivery now looks very significant.23 And, of course, the 8-minute phone call to the stockbroker shines as a heartless, self-centered act of inattention.
Manipulating the record
Another lesson of this case: Do not manipulate the record. The ObGyn recorded that the patient had refused the cesarean delivery he recommended. Had that been the truth, it would have substantially improved his case. But apparently it was not the truth. Although there was circumstantial evidence (the charting of the patient’s refusal only after the newborn’s condition was obvious, failure to complete appropriate hospital forms), the most damning evidence was the direct testimony of the L&D nurse. She reported that, contrary to what the ObGyn put in the chart, the patient requested a cesarean delivery. In truth, it was the ObGyn who had refused.
A physician who is dishonest with charting—making false statements or going back or “correcting” a chart later—loses credibility and the presumption of acting in good faith. That is disastrous for the physician.24
A hidden lesson
Another lesson, more human than legal, is that it matters how patients are treated when things go wrong. According to press reports, the parents felt that the ObGyn had not recognized that he had made any errors, did not apologize, and had even blamed the mother for the outcome. It does not require graduate work in psychology to expect that this approach would make the parents angry enough to pursue legal action. True regret, respect, and apologies are not panaceas, but they are important.25 Who gets sued and why is a key question that is part of a larger risk management plan. In this case, the magnitude of the injuries made a suit very likely, which is not the case with all bad outcomes.26 Honest communication with patients in the face of bad results remains the goal.27
Pulling it all together
Clinicians must always remain cognizant that the patient comes first and of the importance of working as a team with nursing staff and other allied health professionals. Excellent communication and support staff interaction in good times and bad can make a difference in patient outcomes and, indeed, in medical malpractice verdicts.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Chang D. Miami doctor’s call to broker during baby’s delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed May 16, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17−18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
- American College of Obstetricians and Gynecologists Committee on Ethics. Committee Opinion No. 664: Refusal of medically recommended treatment during pregnancy. Obstet Gynecol. 2016;126(6):e175−e182.
- American College of Obstetricians and Gynecologists. Professional liability and risk management an essential guide for obstetrician-gynecologist. 3rd ed. Washington, DC: 2014.
- Ghidini A, Stewart D, Pezzullo J, Locatelli A. Neonatal complications in vacuum-assisted vaginal delivery: are they associated with number of pulls, cup detachments, and duration of vacuum application? Arch Gynecol Obstet. 2017;295(1):67−73.
- Turkmen S. Maternal and neonatal outcomes in vacuum-assisted delivery with the Kiwi OmniCup and Malmstrom metal cup. J Obstet Gynaecol Res. 2015;41(2):207−213.
- Davis DJ. Neonatal subgaleal hemorrhage: diagnosis and management. CMAJ. 2001;164(10):1452−1453.
- Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health. 1996;32(3):228−232.
- Dall’Asta A, Ghi T, Pedrazzi G, Frusca T. Does vacuum delivery carry a higher risk of shoulder dystocia? Review and metanalysis of the literature. Eur J Obstet Gynecol Reprod Biol. 2016;201:62−68.
- American College of Obstetricians and Gynecologists Task Force on Neonatal Encephalopathy. Neonatal Encephalopathy and Neurologic Outcomes. 2nd ed. Washington, DC: 2014.
- Nelson K, Ellenberg J. Apgar scores as predictors of chronic neurologic disability. Pediatrics. 1981;68:36−44.
- ACOG Technical Bulletin No. 163: Fetal and neonatal neurologic injury. Int J. Gynaecol Obstet. 1993;41(1):97−101.
- Nelson K, Ellenberg J. Antecedents of cerebral palsy. I. Univariate analysis of risks. Am J Dis Child. 1985;139(10):1031−1038.
- Fenichel GM, Webster D, Wong WK. Intracranial hemorrhage in the term newborn. Arch Neurol. 1984;41(1):30−34.
- Peckham C. Medscape Malpractice Report 2015: Why Ob/Gyns Get Sued. Medscape. https://www.medscape.com/features/slideshow/malpractice-report-2015/obgyn#page=1. Published January 2016. Accessed May 16, 2018.
- Bixenstine PJ, Shore AD, Mehtsun WT, Ibrahim AM, Freischlag JA, Makary MA. Catastrophic medical malpractice payouts in the United States. J Healthc Qual. 2014;36(4):43−53.
- Santos P, Ritter GA, Hefele JL, Hendrich A, McCoy CK. Decreasing intrapartum malpractice: Targeting the most injurious neonatal adverse events. J Healthc Risk Manag. 2015;34(4):20−27.
- Studdert DM, Bismark MM, Mello MM, Singh H, Spittal MJ. Prevalence and characteristics of physicians prone to malpractice claims. N Engl J Med. 2016;374(4):354−362.
- Levine AS. Legal 101: Tort law and medical malpractice for physicians. Contemp OBGYN. http://www.contem poraryobgyn.net/obstetrics-gynecology-womens-health/legal-101-tort-law-and-medical-malpractice-physicians. Published July 17, 2015. Accessed May 8, 2018.
- Smith SR, Sanfilippo JS. Applied Business Law. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:91−126.
- Glaser LM, Alvi FA, Milad MP. Trends in malpractice claims for obstetric and gynecologic procedures, 2005 through 2014. Am J Obstet Gynecol. 2017;217(3):340.e1–e6.
- Seegert L. Malpractice pitfalls: 5 strategies to reduce lawsuit threats. Medical Econ. http://www.medicaleconomics.com/medical-economics-blog/5-strategies-reduce-malpractice-lawsuit-threats. Published November 10, 2016. Accessed May 8, 2018.
- Peckham C. Malpractice and medicine: who gets sued and why? Medscape. http://www.medscape.com/viewarticle/855229. Published December 8, 2015. Accessed May 16, 2018.
- McMichael B. The failure of ‘sorry’: an empirical evaluation of apology laws, health care, and medical malpractice. Social Science Research Network. https://papers.ssrn.com/abstract=3020352. Published August 16, 2017. Accessed May 16, 2018.
- Carranza L, Lyerly AD, Lipira L, Prouty CD, Loren D, Gallagher TH. Delivering the truth: challenges and opportunities for error disclosure in obstetrics. Obstet Gynecol. 2014;123(3):656−659.
CASE Failure to perform cesarean delivery1–4
A 19-year-old woman (G1P0) received prenatal care at a federally funded health center. Her pregnancy was normal without complications. She presented to the hospital after spontaneous rupture of membranes (SROM). The on-call ObGyn employed by the clinic was offsite when the mother was admitted.
The mother signed a standard consent form for vaginal and cesarean deliveries and any other surgical procedure required during the course of giving birth.
The ObGyn ordered low-dose oxytocin to augment labor in light of her SROM. Oxytocin was started at 9:46
Upon delivery, the infant was flaccid and not breathing. His Apgar scores were 2, 3, and 6 at 1, 5, and 10 minutes, respectively, and the cord pH was 7. The neonatal intensive care (NICU) team provided aggressive resuscitation.
At the time of trial, the 18-month-old boy was being fed through a percutaneous endoscopic gastrostomy tube and had a tracheostomy that required periodic suctioning. The child was not able to stand, crawl, or support himself, and will require 24-hour nursing care for the rest of his life.
LAWSUIT. The parents filed a lawsuit in federal court for damages under the Federal Tort Claims Act (see “Notes about this case,”). The mother claimed that she had requested a cesarean delivery early in labor when FHR tracings showed fetal distress, and again prior to vacuum extraction; the ObGyn refused both times.
The ObGyn claimed that when he noted a category III tracing, he recommended cesarean delivery, but the patient refused. He recorded the refusal in the chart some time later, after he had noted the neonate’s appearance.
The parents’ expert testified that restarting oxytocin and using vacuum extraction multiple times were dangerous and gross deviations from acceptable practice. Prolonged and repetitive use of the vacuum extractor caused a large subgaleal hematoma that decreased blood flow to the fetal brain, resulting in irreversible central nervous system (CNS) damage secondary to hypoxic ischemic encephalopathy. An emergency cesarean delivery should have been performed at the first sign of fetal distress.
The defense expert pointed out that the ObGyn discussed the need for cesarean delivery with the patient when fetal distress occurred and that the ObGyn was bedside and monitoring the fetus and the mother. Although the mother consented to a cesarean delivery at time of admission, she refused to allow the procedure.
The labor and delivery (L&D) nurse corroborated the mother’s story that a cesarean delivery was not offered by the ObGyn, and when the patient asked for a cesarean delivery, he refused. The nurse stated that the note added to the records by the ObGyn about the mother’s refusal was a lie. If the mother had refused a cesarean, the nurse would have documented the refusal by completing a Refusal of Treatment form that would have been faxed to the risk manager. No such form was required because nothing was ever offered that the mother refused.
The nurse also testified that during the course of the latter part of labor, the ObGyn left the room several times to assist other patients, deliver another baby, and make an 8-minute phone call to his stockbroker. She reported that the ObGyn was out of the room when delivery occurred.
WHAT’S THE VERDICT?
Read about the verdict and medical considerations.
WHAT’S THE VERDICT?
The medical care and the federal-court bench trial held in front of a judge (not a jury) occurred in Florida. The verdict suggests that the ObGyn breached the standard of care by not offering or proceeding with a cesarean delivery and this management resulted in the child’s injuries. The court awarded damages in the amount of $33,813,495.91, including $29,413,495.91 for the infant; $3,300,000.00 for the plaintiff; and $1,100,000.00 for her spouse.4
Medical considerations
Refusal of medical care
Although it appears that in this case the patient did not actually refuse medical care (cesarean delivery), the case does raise the question of refusal. Refusal of medical care has been addressed by the American College of Obstetricians and Gynecologists (ACOG) predicated upon care that supports maternal and fetal wellbeing.5 There may be a fine balance between safeguarding the pregnant woman’s autonomy and optimization of fetal wellbeing. “Forced compliance,” on the other hand, is the alternative to respecting refusal of treatment. Ethical issues come into play: patient rights; respect for autonomy; violations of bodily integrity; power differentials; and gender equality.5 The use of coercion is “not only ethically impermissible but also medically inadvisable secondary to the realities of prognostic uncertainty and the limitations of medical knowledge.”5 There is an obligation to elicit the patient’s reasoning and lived experience. Perhaps most importantly, as clinicians working to achieve a resolution, consideration of the following is appropriate5:
- reliability and validity of evidence-based medicine
- severity of the prospective outcome
- degree of risk or burden placed on the patient
- patient understanding of the gravity of the situation and risks
- degree of urgency.
Much of this boils down to the obligation to discuss “risks and benefits of treatment, alternatives and consequences of refusing treatment.”6
Complications from vacuum-assisted vaginal delivery
Ghidini and associates, in a multicenter retrospective study, evaluated complications relating to vacuum-assisted delivery. They listed major primary outcomes of subgaleal hemorrhage, skull fracture, and intracranial bleeding, and minor primary outcomes of cephalohematoma, scalp laceration, and extensive skin abrasions. Secondary outcomes included a 5-minute Apgar score of <7, umbilical artery pH of <7.10, shoulder dystocia, and NICU admission.7
A retrospective study from Sweden assessing all vacuum deliveries over a 2-year period compared the use of the Kiwi OmniCup (Clinical Innovations) to use of the Malmström metal cup (Medela). No statistical differences in maternal or neonatal outcomes as well as failure rates were noted. However, the duration of the procedure was longer and the requirement for fundal pressure was higher with the Malmström device.8
Subgaleal hemorrhage. Ghidini and colleagues reported a heightened incidence of head injury related to the duration of vacuum application and birth weight.7 Specifically, vacuum delivery devices increase the risk of subgaleal hemorrhage. Blood can accumulate between the scalp’s epicranial aponeurosis and the periosteum and potentially can extend forward to the orbital margins, backward to the nuchal ridge, and laterally to the temporal fascia. As much as 260 mL of blood can get into this subaponeurotic space in term babies.9 Up to one-quarter of babies who require NICU admission for this condition die.10 This injury seldom occurs with forceps.
Shoulder dystocia. In a meta-analysisfrom Italy, the vacuum extractor was associated with increased risk of shoulder dystocia compared with spontaneous vaginal delivery.11
Intrapartum hypoxia. In 2003, the ACOG Task Force on Neonatal Encephalopathy and Cerebral Palsy defined an acute intrapartum hypoxic event (TABLE).12
Cerebral palsy (CP) is defined as “a chronic neuromuscular disability characterized by aberrant control of movement or posture appearing early in life and not the result of recognized progressive disease.”13,14
The Collaborative Perinatal Project concluded that birth trauma plays a minimal role in development of CP.15 Arrested labor, use of oxytocin, or prolonged labor did not play a role. CP can develop following significant cerebral or posterior fossa hemorrhage in term infants.16
Perinatal asphyxia is a poor and imprecise term and use of the expression should be abandoned. Overall, 90% of children with CP do not have birth asphyxia as the underlying etiology.14
Prognostic assessment can be made, in part, by using the Sarnat classification system (classification scale for hypoxic-ischemic encephalopathy of the newborn) or an electroencephalogram to stratify the severity of neonatal encephalopathy.12 Such tests are not stand-alone but a segment of assessment. At this point “a better understanding of the processes leading to neonatal encephalopathy and associated outcomes” appear to be required to understand and associate outcomes.12 “More accurate and reliable tools (are required) for prognostic forecasting.”12
Hypoxic-ischemic encephalopathy involves multisystem organ failure including renal, hepatic, hematologic, cardiac, gastrointestinal, and metabolic abnormalities. There is no correlation between the degree of CNS injury and level of other organ abnormalities.12
Differential diagnosis
When events such as those described in this case occur, develop a differential diagnosis by considering the following12:
- uterine rupture
- severe placental abruption
- umbilical cord prolapse
- amniotic fluid embolus
- maternal cardiovascular collapse
- fetal exsanguination.
Read about the legal considerations.
Legal considerations
Although ObGyns are among the specialties most likely to experience malpractice claims,17 a verdict of more than $33 million is unusual.18 Despite the failure of adequate care, and the enormous damages, the ObGyn involved probably will not be responsible for paying the verdict (see “Notes about this case”). The case presents a number of important lessons and reminders for anyone practicing obstetrics.
A procedural comment
The case in this article arose under the Federal Tort Claims Act (FTCA).1 Most government entities have sovereign immunity, meaning that they can be sued only with their consent. In the FTCA, the federal government consented to being sued for the acts of its employees. This right has a number of limitations and some technical procedures, but at its core, it permits the United States to be sued as though it was a private individual.2 Private individuals can be sued for the acts of the agents (including employees).
Although the FTCA is a federal law, and these cases are tried in federal court, the substantive law of the state applies. This case occurred in Florida, so Florida tort law, defenses, and limitation on claims applied here also. Had the events occurred in Iowa, Iowa law would have applied.
In FTCA cases, the United States is the defendant (generally it is the government, not the employee who is the defendant).3 In this case, the ObGyn was employed by a federal government entity to provide delivery services. As a result, the United States was the primary defendant, had the obligation to defend the suit, and will almost certainly be obligated to pay the verdict.
The case facts
Although this description is based on an actual case, the facts were taken from the opinion of the trial court, legal summaries and press reports and not from the full case documents.4-7 We could not independently assess the accuracy of the facts, but for the purpose of this discussion, we have assumed the facts to be correct. The government has apparently filed an appeal in the Eleventh Circuit.
References
- Federal Tort Claims Act. Vol 28 U.S.C. Pt.VI Ch.171 and 28 U.S.C. § 1346(b).
- About the Federal Tort Claims Act (FTCA). Health Resources & Services Administration: Health Center Program. https://bphc.hrsa.gov/ftca/about/index.html. Accessed May 16, 2018.
- Dowell MA, Scott CD. Federally Qualified Health Center Federal Tort Claims Act Insurance Coverage. Health Law. 2015;5:31-43.
- Chang D. Miami doctor's call to broker during baby's delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed January 11, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17-18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
Very large verdict
The extraordinary size of this verdict ($33 million without any punitive damages) is a reminder that in obstetrics, mistakes can have catastrophic consequences and very high costs.19 This fact is reflected in malpractice insurance rates.
A substantial amount of this case’s award will provide around-the-clock care for the child. This verdict was not the result of a runaway jury—it was a judge’s decision. It is also noteworthy to report that a small percentage of physicians (1%) appear responsible for a significant number (about one-third) of paid claims.20
Although the size of the verdict is unusual, the case is a fairly straightforward negligence tort. The judge found that the ObGyn had breached the duty of care for his patient. The actions that fell below the standard of care included restarting the oxytocin, using the Kiwi vacuum device 3 times, and failing to perform a cesarean delivery in light of obvious fetal distress. That negligence caused injury to the infant (and his parents).21 The judge determined that the 4 elements of negligence were present: 1) duty of care, 2) breach of that duty, 3) injury, and 4) a causal link between the breach of duty and the injury. The failure to adhere to good practice standards practically defines breach of duty.22
Multitasking
One important lesson is that multitasking, absence, and inattention can look terrible when things go wrong. Known as “hindsight bias,” the awareness that there was a disastrous result makes it easier to attribute the outcome to small mistakes that otherwise might seem trivial. This ObGyn was in and out of the room during a difficult labor. Perhaps that was understandable if it were unavoidable because of another delivery, but being absent frequently and not present for the delivery now looks very significant.23 And, of course, the 8-minute phone call to the stockbroker shines as a heartless, self-centered act of inattention.
Manipulating the record
Another lesson of this case: Do not manipulate the record. The ObGyn recorded that the patient had refused the cesarean delivery he recommended. Had that been the truth, it would have substantially improved his case. But apparently it was not the truth. Although there was circumstantial evidence (the charting of the patient’s refusal only after the newborn’s condition was obvious, failure to complete appropriate hospital forms), the most damning evidence was the direct testimony of the L&D nurse. She reported that, contrary to what the ObGyn put in the chart, the patient requested a cesarean delivery. In truth, it was the ObGyn who had refused.
A physician who is dishonest with charting—making false statements or going back or “correcting” a chart later—loses credibility and the presumption of acting in good faith. That is disastrous for the physician.24
A hidden lesson
Another lesson, more human than legal, is that it matters how patients are treated when things go wrong. According to press reports, the parents felt that the ObGyn had not recognized that he had made any errors, did not apologize, and had even blamed the mother for the outcome. It does not require graduate work in psychology to expect that this approach would make the parents angry enough to pursue legal action. True regret, respect, and apologies are not panaceas, but they are important.25 Who gets sued and why is a key question that is part of a larger risk management plan. In this case, the magnitude of the injuries made a suit very likely, which is not the case with all bad outcomes.26 Honest communication with patients in the face of bad results remains the goal.27
Pulling it all together
Clinicians must always remain cognizant that the patient comes first and of the importance of working as a team with nursing staff and other allied health professionals. Excellent communication and support staff interaction in good times and bad can make a difference in patient outcomes and, indeed, in medical malpractice verdicts.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE Failure to perform cesarean delivery1–4
A 19-year-old woman (G1P0) received prenatal care at a federally funded health center. Her pregnancy was normal without complications. She presented to the hospital after spontaneous rupture of membranes (SROM). The on-call ObGyn employed by the clinic was offsite when the mother was admitted.
The mother signed a standard consent form for vaginal and cesarean deliveries and any other surgical procedure required during the course of giving birth.
The ObGyn ordered low-dose oxytocin to augment labor in light of her SROM. Oxytocin was started at 9:46
Upon delivery, the infant was flaccid and not breathing. His Apgar scores were 2, 3, and 6 at 1, 5, and 10 minutes, respectively, and the cord pH was 7. The neonatal intensive care (NICU) team provided aggressive resuscitation.
At the time of trial, the 18-month-old boy was being fed through a percutaneous endoscopic gastrostomy tube and had a tracheostomy that required periodic suctioning. The child was not able to stand, crawl, or support himself, and will require 24-hour nursing care for the rest of his life.
LAWSUIT. The parents filed a lawsuit in federal court for damages under the Federal Tort Claims Act (see “Notes about this case,”). The mother claimed that she had requested a cesarean delivery early in labor when FHR tracings showed fetal distress, and again prior to vacuum extraction; the ObGyn refused both times.
The ObGyn claimed that when he noted a category III tracing, he recommended cesarean delivery, but the patient refused. He recorded the refusal in the chart some time later, after he had noted the neonate’s appearance.
The parents’ expert testified that restarting oxytocin and using vacuum extraction multiple times were dangerous and gross deviations from acceptable practice. Prolonged and repetitive use of the vacuum extractor caused a large subgaleal hematoma that decreased blood flow to the fetal brain, resulting in irreversible central nervous system (CNS) damage secondary to hypoxic ischemic encephalopathy. An emergency cesarean delivery should have been performed at the first sign of fetal distress.
The defense expert pointed out that the ObGyn discussed the need for cesarean delivery with the patient when fetal distress occurred and that the ObGyn was bedside and monitoring the fetus and the mother. Although the mother consented to a cesarean delivery at time of admission, she refused to allow the procedure.
The labor and delivery (L&D) nurse corroborated the mother’s story that a cesarean delivery was not offered by the ObGyn, and when the patient asked for a cesarean delivery, he refused. The nurse stated that the note added to the records by the ObGyn about the mother’s refusal was a lie. If the mother had refused a cesarean, the nurse would have documented the refusal by completing a Refusal of Treatment form that would have been faxed to the risk manager. No such form was required because nothing was ever offered that the mother refused.
The nurse also testified that during the course of the latter part of labor, the ObGyn left the room several times to assist other patients, deliver another baby, and make an 8-minute phone call to his stockbroker. She reported that the ObGyn was out of the room when delivery occurred.
WHAT’S THE VERDICT?
Read about the verdict and medical considerations.
WHAT’S THE VERDICT?
The medical care and the federal-court bench trial held in front of a judge (not a jury) occurred in Florida. The verdict suggests that the ObGyn breached the standard of care by not offering or proceeding with a cesarean delivery and this management resulted in the child’s injuries. The court awarded damages in the amount of $33,813,495.91, including $29,413,495.91 for the infant; $3,300,000.00 for the plaintiff; and $1,100,000.00 for her spouse.4
Medical considerations
Refusal of medical care
Although it appears that in this case the patient did not actually refuse medical care (cesarean delivery), the case does raise the question of refusal. Refusal of medical care has been addressed by the American College of Obstetricians and Gynecologists (ACOG) predicated upon care that supports maternal and fetal wellbeing.5 There may be a fine balance between safeguarding the pregnant woman’s autonomy and optimization of fetal wellbeing. “Forced compliance,” on the other hand, is the alternative to respecting refusal of treatment. Ethical issues come into play: patient rights; respect for autonomy; violations of bodily integrity; power differentials; and gender equality.5 The use of coercion is “not only ethically impermissible but also medically inadvisable secondary to the realities of prognostic uncertainty and the limitations of medical knowledge.”5 There is an obligation to elicit the patient’s reasoning and lived experience. Perhaps most importantly, as clinicians working to achieve a resolution, consideration of the following is appropriate5:
- reliability and validity of evidence-based medicine
- severity of the prospective outcome
- degree of risk or burden placed on the patient
- patient understanding of the gravity of the situation and risks
- degree of urgency.
Much of this boils down to the obligation to discuss “risks and benefits of treatment, alternatives and consequences of refusing treatment.”6
Complications from vacuum-assisted vaginal delivery
Ghidini and associates, in a multicenter retrospective study, evaluated complications relating to vacuum-assisted delivery. They listed major primary outcomes of subgaleal hemorrhage, skull fracture, and intracranial bleeding, and minor primary outcomes of cephalohematoma, scalp laceration, and extensive skin abrasions. Secondary outcomes included a 5-minute Apgar score of <7, umbilical artery pH of <7.10, shoulder dystocia, and NICU admission.7
A retrospective study from Sweden assessing all vacuum deliveries over a 2-year period compared the use of the Kiwi OmniCup (Clinical Innovations) to use of the Malmström metal cup (Medela). No statistical differences in maternal or neonatal outcomes as well as failure rates were noted. However, the duration of the procedure was longer and the requirement for fundal pressure was higher with the Malmström device.8
Subgaleal hemorrhage. Ghidini and colleagues reported a heightened incidence of head injury related to the duration of vacuum application and birth weight.7 Specifically, vacuum delivery devices increase the risk of subgaleal hemorrhage. Blood can accumulate between the scalp’s epicranial aponeurosis and the periosteum and potentially can extend forward to the orbital margins, backward to the nuchal ridge, and laterally to the temporal fascia. As much as 260 mL of blood can get into this subaponeurotic space in term babies.9 Up to one-quarter of babies who require NICU admission for this condition die.10 This injury seldom occurs with forceps.
Shoulder dystocia. In a meta-analysisfrom Italy, the vacuum extractor was associated with increased risk of shoulder dystocia compared with spontaneous vaginal delivery.11
Intrapartum hypoxia. In 2003, the ACOG Task Force on Neonatal Encephalopathy and Cerebral Palsy defined an acute intrapartum hypoxic event (TABLE).12
Cerebral palsy (CP) is defined as “a chronic neuromuscular disability characterized by aberrant control of movement or posture appearing early in life and not the result of recognized progressive disease.”13,14
The Collaborative Perinatal Project concluded that birth trauma plays a minimal role in development of CP.15 Arrested labor, use of oxytocin, or prolonged labor did not play a role. CP can develop following significant cerebral or posterior fossa hemorrhage in term infants.16
Perinatal asphyxia is a poor and imprecise term and use of the expression should be abandoned. Overall, 90% of children with CP do not have birth asphyxia as the underlying etiology.14
Prognostic assessment can be made, in part, by using the Sarnat classification system (classification scale for hypoxic-ischemic encephalopathy of the newborn) or an electroencephalogram to stratify the severity of neonatal encephalopathy.12 Such tests are not stand-alone but a segment of assessment. At this point “a better understanding of the processes leading to neonatal encephalopathy and associated outcomes” appear to be required to understand and associate outcomes.12 “More accurate and reliable tools (are required) for prognostic forecasting.”12
Hypoxic-ischemic encephalopathy involves multisystem organ failure including renal, hepatic, hematologic, cardiac, gastrointestinal, and metabolic abnormalities. There is no correlation between the degree of CNS injury and level of other organ abnormalities.12
Differential diagnosis
When events such as those described in this case occur, develop a differential diagnosis by considering the following12:
- uterine rupture
- severe placental abruption
- umbilical cord prolapse
- amniotic fluid embolus
- maternal cardiovascular collapse
- fetal exsanguination.
Read about the legal considerations.
Legal considerations
Although ObGyns are among the specialties most likely to experience malpractice claims,17 a verdict of more than $33 million is unusual.18 Despite the failure of adequate care, and the enormous damages, the ObGyn involved probably will not be responsible for paying the verdict (see “Notes about this case”). The case presents a number of important lessons and reminders for anyone practicing obstetrics.
A procedural comment
The case in this article arose under the Federal Tort Claims Act (FTCA).1 Most government entities have sovereign immunity, meaning that they can be sued only with their consent. In the FTCA, the federal government consented to being sued for the acts of its employees. This right has a number of limitations and some technical procedures, but at its core, it permits the United States to be sued as though it was a private individual.2 Private individuals can be sued for the acts of the agents (including employees).
Although the FTCA is a federal law, and these cases are tried in federal court, the substantive law of the state applies. This case occurred in Florida, so Florida tort law, defenses, and limitation on claims applied here also. Had the events occurred in Iowa, Iowa law would have applied.
In FTCA cases, the United States is the defendant (generally it is the government, not the employee who is the defendant).3 In this case, the ObGyn was employed by a federal government entity to provide delivery services. As a result, the United States was the primary defendant, had the obligation to defend the suit, and will almost certainly be obligated to pay the verdict.
The case facts
Although this description is based on an actual case, the facts were taken from the opinion of the trial court, legal summaries and press reports and not from the full case documents.4-7 We could not independently assess the accuracy of the facts, but for the purpose of this discussion, we have assumed the facts to be correct. The government has apparently filed an appeal in the Eleventh Circuit.
References
- Federal Tort Claims Act. Vol 28 U.S.C. Pt.VI Ch.171 and 28 U.S.C. § 1346(b).
- About the Federal Tort Claims Act (FTCA). Health Resources & Services Administration: Health Center Program. https://bphc.hrsa.gov/ftca/about/index.html. Accessed May 16, 2018.
- Dowell MA, Scott CD. Federally Qualified Health Center Federal Tort Claims Act Insurance Coverage. Health Law. 2015;5:31-43.
- Chang D. Miami doctor's call to broker during baby's delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed January 11, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17-18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
Very large verdict
The extraordinary size of this verdict ($33 million without any punitive damages) is a reminder that in obstetrics, mistakes can have catastrophic consequences and very high costs.19 This fact is reflected in malpractice insurance rates.
A substantial amount of this case’s award will provide around-the-clock care for the child. This verdict was not the result of a runaway jury—it was a judge’s decision. It is also noteworthy to report that a small percentage of physicians (1%) appear responsible for a significant number (about one-third) of paid claims.20
Although the size of the verdict is unusual, the case is a fairly straightforward negligence tort. The judge found that the ObGyn had breached the duty of care for his patient. The actions that fell below the standard of care included restarting the oxytocin, using the Kiwi vacuum device 3 times, and failing to perform a cesarean delivery in light of obvious fetal distress. That negligence caused injury to the infant (and his parents).21 The judge determined that the 4 elements of negligence were present: 1) duty of care, 2) breach of that duty, 3) injury, and 4) a causal link between the breach of duty and the injury. The failure to adhere to good practice standards practically defines breach of duty.22
Multitasking
One important lesson is that multitasking, absence, and inattention can look terrible when things go wrong. Known as “hindsight bias,” the awareness that there was a disastrous result makes it easier to attribute the outcome to small mistakes that otherwise might seem trivial. This ObGyn was in and out of the room during a difficult labor. Perhaps that was understandable if it were unavoidable because of another delivery, but being absent frequently and not present for the delivery now looks very significant.23 And, of course, the 8-minute phone call to the stockbroker shines as a heartless, self-centered act of inattention.
Manipulating the record
Another lesson of this case: Do not manipulate the record. The ObGyn recorded that the patient had refused the cesarean delivery he recommended. Had that been the truth, it would have substantially improved his case. But apparently it was not the truth. Although there was circumstantial evidence (the charting of the patient’s refusal only after the newborn’s condition was obvious, failure to complete appropriate hospital forms), the most damning evidence was the direct testimony of the L&D nurse. She reported that, contrary to what the ObGyn put in the chart, the patient requested a cesarean delivery. In truth, it was the ObGyn who had refused.
A physician who is dishonest with charting—making false statements or going back or “correcting” a chart later—loses credibility and the presumption of acting in good faith. That is disastrous for the physician.24
A hidden lesson
Another lesson, more human than legal, is that it matters how patients are treated when things go wrong. According to press reports, the parents felt that the ObGyn had not recognized that he had made any errors, did not apologize, and had even blamed the mother for the outcome. It does not require graduate work in psychology to expect that this approach would make the parents angry enough to pursue legal action. True regret, respect, and apologies are not panaceas, but they are important.25 Who gets sued and why is a key question that is part of a larger risk management plan. In this case, the magnitude of the injuries made a suit very likely, which is not the case with all bad outcomes.26 Honest communication with patients in the face of bad results remains the goal.27
Pulling it all together
Clinicians must always remain cognizant that the patient comes first and of the importance of working as a team with nursing staff and other allied health professionals. Excellent communication and support staff interaction in good times and bad can make a difference in patient outcomes and, indeed, in medical malpractice verdicts.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Chang D. Miami doctor’s call to broker during baby’s delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed May 16, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17−18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
- American College of Obstetricians and Gynecologists Committee on Ethics. Committee Opinion No. 664: Refusal of medically recommended treatment during pregnancy. Obstet Gynecol. 2016;126(6):e175−e182.
- American College of Obstetricians and Gynecologists. Professional liability and risk management an essential guide for obstetrician-gynecologist. 3rd ed. Washington, DC: 2014.
- Ghidini A, Stewart D, Pezzullo J, Locatelli A. Neonatal complications in vacuum-assisted vaginal delivery: are they associated with number of pulls, cup detachments, and duration of vacuum application? Arch Gynecol Obstet. 2017;295(1):67−73.
- Turkmen S. Maternal and neonatal outcomes in vacuum-assisted delivery with the Kiwi OmniCup and Malmstrom metal cup. J Obstet Gynaecol Res. 2015;41(2):207−213.
- Davis DJ. Neonatal subgaleal hemorrhage: diagnosis and management. CMAJ. 2001;164(10):1452−1453.
- Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health. 1996;32(3):228−232.
- Dall’Asta A, Ghi T, Pedrazzi G, Frusca T. Does vacuum delivery carry a higher risk of shoulder dystocia? Review and metanalysis of the literature. Eur J Obstet Gynecol Reprod Biol. 2016;201:62−68.
- American College of Obstetricians and Gynecologists Task Force on Neonatal Encephalopathy. Neonatal Encephalopathy and Neurologic Outcomes. 2nd ed. Washington, DC: 2014.
- Nelson K, Ellenberg J. Apgar scores as predictors of chronic neurologic disability. Pediatrics. 1981;68:36−44.
- ACOG Technical Bulletin No. 163: Fetal and neonatal neurologic injury. Int J. Gynaecol Obstet. 1993;41(1):97−101.
- Nelson K, Ellenberg J. Antecedents of cerebral palsy. I. Univariate analysis of risks. Am J Dis Child. 1985;139(10):1031−1038.
- Fenichel GM, Webster D, Wong WK. Intracranial hemorrhage in the term newborn. Arch Neurol. 1984;41(1):30−34.
- Peckham C. Medscape Malpractice Report 2015: Why Ob/Gyns Get Sued. Medscape. https://www.medscape.com/features/slideshow/malpractice-report-2015/obgyn#page=1. Published January 2016. Accessed May 16, 2018.
- Bixenstine PJ, Shore AD, Mehtsun WT, Ibrahim AM, Freischlag JA, Makary MA. Catastrophic medical malpractice payouts in the United States. J Healthc Qual. 2014;36(4):43−53.
- Santos P, Ritter GA, Hefele JL, Hendrich A, McCoy CK. Decreasing intrapartum malpractice: Targeting the most injurious neonatal adverse events. J Healthc Risk Manag. 2015;34(4):20−27.
- Studdert DM, Bismark MM, Mello MM, Singh H, Spittal MJ. Prevalence and characteristics of physicians prone to malpractice claims. N Engl J Med. 2016;374(4):354−362.
- Levine AS. Legal 101: Tort law and medical malpractice for physicians. Contemp OBGYN. http://www.contem poraryobgyn.net/obstetrics-gynecology-womens-health/legal-101-tort-law-and-medical-malpractice-physicians. Published July 17, 2015. Accessed May 8, 2018.
- Smith SR, Sanfilippo JS. Applied Business Law. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:91−126.
- Glaser LM, Alvi FA, Milad MP. Trends in malpractice claims for obstetric and gynecologic procedures, 2005 through 2014. Am J Obstet Gynecol. 2017;217(3):340.e1–e6.
- Seegert L. Malpractice pitfalls: 5 strategies to reduce lawsuit threats. Medical Econ. http://www.medicaleconomics.com/medical-economics-blog/5-strategies-reduce-malpractice-lawsuit-threats. Published November 10, 2016. Accessed May 8, 2018.
- Peckham C. Malpractice and medicine: who gets sued and why? Medscape. http://www.medscape.com/viewarticle/855229. Published December 8, 2015. Accessed May 16, 2018.
- McMichael B. The failure of ‘sorry’: an empirical evaluation of apology laws, health care, and medical malpractice. Social Science Research Network. https://papers.ssrn.com/abstract=3020352. Published August 16, 2017. Accessed May 16, 2018.
- Carranza L, Lyerly AD, Lipira L, Prouty CD, Loren D, Gallagher TH. Delivering the truth: challenges and opportunities for error disclosure in obstetrics. Obstet Gynecol. 2014;123(3):656−659.
- Chang D. Miami doctor’s call to broker during baby’s delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed May 16, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17−18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
- American College of Obstetricians and Gynecologists Committee on Ethics. Committee Opinion No. 664: Refusal of medically recommended treatment during pregnancy. Obstet Gynecol. 2016;126(6):e175−e182.
- American College of Obstetricians and Gynecologists. Professional liability and risk management an essential guide for obstetrician-gynecologist. 3rd ed. Washington, DC: 2014.
- Ghidini A, Stewart D, Pezzullo J, Locatelli A. Neonatal complications in vacuum-assisted vaginal delivery: are they associated with number of pulls, cup detachments, and duration of vacuum application? Arch Gynecol Obstet. 2017;295(1):67−73.
- Turkmen S. Maternal and neonatal outcomes in vacuum-assisted delivery with the Kiwi OmniCup and Malmstrom metal cup. J Obstet Gynaecol Res. 2015;41(2):207−213.
- Davis DJ. Neonatal subgaleal hemorrhage: diagnosis and management. CMAJ. 2001;164(10):1452−1453.
- Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health. 1996;32(3):228−232.
- Dall’Asta A, Ghi T, Pedrazzi G, Frusca T. Does vacuum delivery carry a higher risk of shoulder dystocia? Review and metanalysis of the literature. Eur J Obstet Gynecol Reprod Biol. 2016;201:62−68.
- American College of Obstetricians and Gynecologists Task Force on Neonatal Encephalopathy. Neonatal Encephalopathy and Neurologic Outcomes. 2nd ed. Washington, DC: 2014.
- Nelson K, Ellenberg J. Apgar scores as predictors of chronic neurologic disability. Pediatrics. 1981;68:36−44.
- ACOG Technical Bulletin No. 163: Fetal and neonatal neurologic injury. Int J. Gynaecol Obstet. 1993;41(1):97−101.
- Nelson K, Ellenberg J. Antecedents of cerebral palsy. I. Univariate analysis of risks. Am J Dis Child. 1985;139(10):1031−1038.
- Fenichel GM, Webster D, Wong WK. Intracranial hemorrhage in the term newborn. Arch Neurol. 1984;41(1):30−34.
- Peckham C. Medscape Malpractice Report 2015: Why Ob/Gyns Get Sued. Medscape. https://www.medscape.com/features/slideshow/malpractice-report-2015/obgyn#page=1. Published January 2016. Accessed May 16, 2018.
- Bixenstine PJ, Shore AD, Mehtsun WT, Ibrahim AM, Freischlag JA, Makary MA. Catastrophic medical malpractice payouts in the United States. J Healthc Qual. 2014;36(4):43−53.
- Santos P, Ritter GA, Hefele JL, Hendrich A, McCoy CK. Decreasing intrapartum malpractice: Targeting the most injurious neonatal adverse events. J Healthc Risk Manag. 2015;34(4):20−27.
- Studdert DM, Bismark MM, Mello MM, Singh H, Spittal MJ. Prevalence and characteristics of physicians prone to malpractice claims. N Engl J Med. 2016;374(4):354−362.
- Levine AS. Legal 101: Tort law and medical malpractice for physicians. Contemp OBGYN. http://www.contem poraryobgyn.net/obstetrics-gynecology-womens-health/legal-101-tort-law-and-medical-malpractice-physicians. Published July 17, 2015. Accessed May 8, 2018.
- Smith SR, Sanfilippo JS. Applied Business Law. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:91−126.
- Glaser LM, Alvi FA, Milad MP. Trends in malpractice claims for obstetric and gynecologic procedures, 2005 through 2014. Am J Obstet Gynecol. 2017;217(3):340.e1–e6.
- Seegert L. Malpractice pitfalls: 5 strategies to reduce lawsuit threats. Medical Econ. http://www.medicaleconomics.com/medical-economics-blog/5-strategies-reduce-malpractice-lawsuit-threats. Published November 10, 2016. Accessed May 8, 2018.
- Peckham C. Malpractice and medicine: who gets sued and why? Medscape. http://www.medscape.com/viewarticle/855229. Published December 8, 2015. Accessed May 16, 2018.
- McMichael B. The failure of ‘sorry’: an empirical evaluation of apology laws, health care, and medical malpractice. Social Science Research Network. https://papers.ssrn.com/abstract=3020352. Published August 16, 2017. Accessed May 16, 2018.
- Carranza L, Lyerly AD, Lipira L, Prouty CD, Loren D, Gallagher TH. Delivering the truth: challenges and opportunities for error disclosure in obstetrics. Obstet Gynecol. 2014;123(3):656−659.
Supreme Court decisions in 2017 that affected your practice
Despite being short-handed (there were only 8 justices for most of the Term), the United States Supreme Court decided a number of important cases during its most recent Term, which concluded on June 27, 2017. Among the 69 cases, several are of particular interest to ObGyns.
1. Arbitration in health care
In Kindred Nursing Centers v Clark, the Court decided an important case involving arbitration in health care.1
At stake. The families of 2 people who died after being in a long-term care facility filed lawsuits against the facility, claiming personal injury, violations of Kentucky statutes regarding long-term care facilities, and wrongful death. However, during admission to the facility, the patients (technically, their agents under a power of attorney) signed an agreement that any disputes would be taken to arbitration. The facility successfully had the lawsuits dismissed.
Final ruling. The Supreme Court agreed that the case had to go to arbitration rather than to court, even though the arbitration clause violated state law. The Federal Arbitration Act (FAA) preempts state law. The Court has been very aggressive in enforcing arbitration agreements and striking down state laws that are inconsistent with the FAA. This case emphasizes that the FAA applies in the health care context.
The case suggests both a warning and an opportunity for health care providers. The warning is that arbitration clauses will be enforced; thoughtlessly entering into arbitration for future disputes may be dangerous. Among other things, the decision of arbitrators is essentially unreviewable. Appellate courts review the decisions of lower courts, but there is no such review in arbitration. Furthermore, arbitration may be stacked in favor of commercial entities that often use arbitrators.
The opportunity for health care providers lies in that it may be possible to include arbitration clauses in agreements with patients. This should be considered only after obtaining legal advice. The agreements should, for example, be consistent with the obligations to patients (in the case of the Kentucky facility, it made clear that accepting the arbitration agreement was not necessary in order to receive care or be admitted to the facility). Because arbitration agreements are becoming ubiquitous and rigorously enforced by federal courts, arbitration is bound to have an important function in health care.
2. Pharmaceuticals
Biologics and biosimilars
Biologics play an important role in health care. Eight of the top 10 selling drugs in 2016 were biologics.2 The case of Sandoz v Amgen involved biosimilar pharmaceuticals, essentially the generics of biologic drugs.3
At stake. While biologics hold great promise in medicine, they are generally very expensive. Just as with generics, brand-name companies (generally referred to as “reference” biologics) want to keep biosimilars off the market for as long as possible, thereby extending the advantages of monopolistic pricing. This Term the Supreme Court considered the statutory rules for licensing biosimilar drugs.
Final ruling. The Court’s decision will allow biosimilar companies to speed up the licensing process by at least 180 days. This is a modest win for patients and their physicians, but the legal issues around biosimilars will need additional attention.
Class action suits
In another case, the Court made it more difficult to file class action suits against pharmaceutical companies in state courts.4 Although this is a fairly technical decision, it is likely to have a significant impact in pharmaceutical liability by limiting classactions.
3. The travel ban
The American College of Obstetricians and Gynecologists joined other medical organizations in an amicus curiae (friend of the court) brief to challenge President Trump’s “travel ban.”5
At stake. The brief argued that the United States “relies upon a significant number of health professionals and scientists who have entered the country through the immigration system.”5
Final ruling. The Court allowed most of the travel ban to stay in place, but did permit entry into the United States by foreign nationals “with a close familial relationship,” or pre-existing ties to US businesses or institutions (such as students who have been admitted to American colleges, workers who have accepted US employment, or lecturers invited to address American audiences).6 Following the Term, the Administration issued a different travel ban, so the issue was taken off the Court’s calendar for the moment. There undoubtedly will be additional chapters to come.
4. Birth certificates and same-sex marriage
In Pavan v Smith, the legal question concerned whether married same-sex couples may have both parents listed on the birth certificate of children born during the marriage.7 Two same-sex couples conceived children through anonymous sperm donation and gave birth in Arkansas. The Department of Health in Arkansas issued birth certificates listing the mother’s name, but refused to list the spouse on the birth certificate.
At stake. The couples brought suit claiming a constitutional right to have both parents listed. In particular, they noted that under Arkansas law, the woman who gives birth is deemed to be the mother. When the woman is married, the husband’s name is “entered on the certificate as the father of the child.”8 The same-sex parents argued that a 2015 decision of the Supreme Court, which held that the Constitution requires states to recognize same-sex marriages, made it clear that same-sex couples should have the benefits of marriage.9 Eventually the case wound its way to the Supreme Court.
Final ruling. The Court held that if the state ordinarily lists the names of both husband and wife on such certificates, then same-sex couples are entitled to have birth certificates listing both parents. The Court noted that laws are unconstitutional if they treat same-sex couples differently than opposite-sex couples. Based on this principle, the Court held that parental birth certificate registration is part of the “constellations of benefits” linked to marriage that the Constitution affords same-sex couples. This ruling applies as a matter of constitutional right in all states.
Read about more interesting Supreme Court decisions
5. Sexual offenders and social media
States struggle to protect children from convicted sex offenders. North Carolina, for example, made it a felony for sex offenders (who had completed their sentences) to use social media sites that “permit minor children to become members or create and maintain personal web pages.”10
At stake. In Packingham v North Carolina, the Court was asked to decide whether this statute violates the First Amendment (free speech) rights of sex offenders.11
Final ruling. The Court held that the North Carolina limitation on sex offenders’ use of social media was too broad. It noted the wide range of political, employment, news, personal, commercial, and religious websites that are off limits to sex offenders under the statute—hardly narrowly tailored. It suggested, however, that it probably would be constitutional for a state to prohibit sex offenders “from engaging in conduct that often presages a sexual crime, like contacting a minor or using a website to gather information about a minor.”11
It was important in this case that the defendant had already served his entire sentence and was “no longer subject to the supervision of the criminal justice system.”11 If he had still been in prison, the state could limit or prohibit his Internet use. Even if he had been on probation or parole (under the supervision of the criminal justice system) the restrictions may well have been permitted. In addition, the state could impose new, narrowly tailored restrictions.
This case is also a reminder that ObGyns are very important in the efforts to eliminate child sexual abuse. All states have laws that require the reporting of known or suspected sexual abuse. In addition to complying with the law, such reports are often critical to discovering and ending the abuse.
6. Transgender rights
The Court had accepted a “transgender bathroom case” in Gloucester County School Board v G.G.12
At stake. This case essentially challenged the Obama Administration’s requirement that schools allow transgender students to use the restrooms in which they feel most comfortable. It was one of the most anticipated cases of the Term, but it essentially disappeared. Following the presidential election, the Department of Education rescinded the earlier guidance on which the case was based.
Final ruling. The Court returned the case to the Fourth Circuit for reconsideration. This issue, however, may reappear before the Court in the form of a claim that the states must provide this accommodation as a matter of federal statutory right, or even Equal Protection.
- In an important First Amendment decision, the Court held that it is a violation of the Freedom of Religion to deny a church-related school access to generally available state grant funds solely because of its religious status (in this case the program funded playground surfacing grants).1
- In several cases, it was apparent that the Court is uncomfortable with the way death penalty cases are handled in some states.2
- Juries may be questioned about racial bias that was expressed during jury deliberations--a substantial change for many courts.3
- The failure of the Patent and Trademark Office (PTO) to register the trademark for the band "The Slants" was a First Amendment violation. One reason that this case was watched was because of the effort of the PTO to deregister the trademark of the Washington Redskins.4
- The Court considered 9 cases involving revoking citizenship, deportation, and cross-border liability (an extraordinary number). Two cases that could change the nature and process of deportation were held over to the next Term for reargument.
- Individualized educational plans under the federal Individuals with Disabilities Education Act (IDEA) must target more than trivial progress for the students.5
References
- Trinity Lutheran Church of Columbia, Inc. v Comer, 582 US 15 577 (2017).
- McAllister S. Death-penalty symposium: A court increasingly uncomfortable with the death penalty. SCOTUSblog.com. http://www.scotusblog.com/2017/06/death-penalty-symposium-court-increasingly-uncomfortable-death-penalty/. Published June 29, 2017. Accessed November 2, 2017.
- Pena-Rodriguez v Colorado, 580 US 15 606 (2017).
- Matal v Tam, 582 US 15 1293 (2017).
- Endrew F v Douglas County School District, RE-1, 580 US 15 827 (2017).
Summary of the Term
The Term was notable for the level of agreement. With 69 decided cases, 41 (69%) were unanimous. In 59 cases (85%), there was a strong consensus, with no more than 2 justices dissenting. Only 7 decisions (10%) were 5 to 4. Justice Kennedy was, as usual, the deciding vote in most of the close cases. He voted in the majority in 97% of the decisions. Justice Gorsuch took the place of Justice Scalia (who passed away in February 2016), so arguably the Court is ideologically close to where it has been for a number of years. Despite rumors that Justice Kennedy would announce his resignation from the Court, neither he nor any other justice has left. The Supreme Court began its new Term on October 2, 2017, with a full complement of 9 justices.
What’s to come
The Court will add cases through much of its new Term, but it has already accepted cases dealing with arbitration agreements (again); public employees’ union dues; immigration (again); the privacy of information held by mobile phone companies; a constitutional challenge to political gerrymandering; bakeries and gay-marriage ceremonies; whistleblowers and Dodd-Frank regulations; sports gambling and the NCAA; and more.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kindred Nursing Centers, LP v Clark, 581 US 16 32 (2017).
- Anderson L. Looking Ahead: Pharma Projections for 2016 - & Beyond. Perma.cc Website. . Reviewed March 30, 2017. Accessed November 2, 2017.
- Sandoz Inc v Amgen Inc, 581 US 15 1039 1195 (2017).
- Bristol-Myers Squibb Co v Superior Court of California, San Francisco County, 582 US 16 466 (2017).
- Trinity FR, Sterling AM, Rogaczewski JD, et al. Motion for Leave to File and Brief for the Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents. SCOTUSblog. http://www.scotusblog.com/wp-content/uploads/2017/06/16-1436-ac-AAMC-supporting-respondents.pdf. Accessed November 2, 2017.
- Donald J. Trump, President of the United States v International Refugee Assistance Project, 582 US 16 1436 (2017).
- Pavan v Smith, 582 US 16 992 (2017).
- Arkansas Code, §20 18 401(f)(1) (2014).
- Obergefell v Hodges, 576 US ___ (2015).
- NC Gen. Stat. Ann. §§14-202.5(a),(e).
- Packingham v North Carolina, 582 US 15 1194 (2017).
- Gloucester County School Board v G.G. SCOTUSblog. http://www.scotusblog.com/case-files/cases/gloucester-county-school-board-v-g-g/. Published March 6, 2017. Accessed November 2, 2017.
Despite being short-handed (there were only 8 justices for most of the Term), the United States Supreme Court decided a number of important cases during its most recent Term, which concluded on June 27, 2017. Among the 69 cases, several are of particular interest to ObGyns.
1. Arbitration in health care
In Kindred Nursing Centers v Clark, the Court decided an important case involving arbitration in health care.1
At stake. The families of 2 people who died after being in a long-term care facility filed lawsuits against the facility, claiming personal injury, violations of Kentucky statutes regarding long-term care facilities, and wrongful death. However, during admission to the facility, the patients (technically, their agents under a power of attorney) signed an agreement that any disputes would be taken to arbitration. The facility successfully had the lawsuits dismissed.
Final ruling. The Supreme Court agreed that the case had to go to arbitration rather than to court, even though the arbitration clause violated state law. The Federal Arbitration Act (FAA) preempts state law. The Court has been very aggressive in enforcing arbitration agreements and striking down state laws that are inconsistent with the FAA. This case emphasizes that the FAA applies in the health care context.
The case suggests both a warning and an opportunity for health care providers. The warning is that arbitration clauses will be enforced; thoughtlessly entering into arbitration for future disputes may be dangerous. Among other things, the decision of arbitrators is essentially unreviewable. Appellate courts review the decisions of lower courts, but there is no such review in arbitration. Furthermore, arbitration may be stacked in favor of commercial entities that often use arbitrators.
The opportunity for health care providers lies in that it may be possible to include arbitration clauses in agreements with patients. This should be considered only after obtaining legal advice. The agreements should, for example, be consistent with the obligations to patients (in the case of the Kentucky facility, it made clear that accepting the arbitration agreement was not necessary in order to receive care or be admitted to the facility). Because arbitration agreements are becoming ubiquitous and rigorously enforced by federal courts, arbitration is bound to have an important function in health care.
2. Pharmaceuticals
Biologics and biosimilars
Biologics play an important role in health care. Eight of the top 10 selling drugs in 2016 were biologics.2 The case of Sandoz v Amgen involved biosimilar pharmaceuticals, essentially the generics of biologic drugs.3
At stake. While biologics hold great promise in medicine, they are generally very expensive. Just as with generics, brand-name companies (generally referred to as “reference” biologics) want to keep biosimilars off the market for as long as possible, thereby extending the advantages of monopolistic pricing. This Term the Supreme Court considered the statutory rules for licensing biosimilar drugs.
Final ruling. The Court’s decision will allow biosimilar companies to speed up the licensing process by at least 180 days. This is a modest win for patients and their physicians, but the legal issues around biosimilars will need additional attention.
Class action suits
In another case, the Court made it more difficult to file class action suits against pharmaceutical companies in state courts.4 Although this is a fairly technical decision, it is likely to have a significant impact in pharmaceutical liability by limiting classactions.
3. The travel ban
The American College of Obstetricians and Gynecologists joined other medical organizations in an amicus curiae (friend of the court) brief to challenge President Trump’s “travel ban.”5
At stake. The brief argued that the United States “relies upon a significant number of health professionals and scientists who have entered the country through the immigration system.”5
Final ruling. The Court allowed most of the travel ban to stay in place, but did permit entry into the United States by foreign nationals “with a close familial relationship,” or pre-existing ties to US businesses or institutions (such as students who have been admitted to American colleges, workers who have accepted US employment, or lecturers invited to address American audiences).6 Following the Term, the Administration issued a different travel ban, so the issue was taken off the Court’s calendar for the moment. There undoubtedly will be additional chapters to come.
4. Birth certificates and same-sex marriage
In Pavan v Smith, the legal question concerned whether married same-sex couples may have both parents listed on the birth certificate of children born during the marriage.7 Two same-sex couples conceived children through anonymous sperm donation and gave birth in Arkansas. The Department of Health in Arkansas issued birth certificates listing the mother’s name, but refused to list the spouse on the birth certificate.
At stake. The couples brought suit claiming a constitutional right to have both parents listed. In particular, they noted that under Arkansas law, the woman who gives birth is deemed to be the mother. When the woman is married, the husband’s name is “entered on the certificate as the father of the child.”8 The same-sex parents argued that a 2015 decision of the Supreme Court, which held that the Constitution requires states to recognize same-sex marriages, made it clear that same-sex couples should have the benefits of marriage.9 Eventually the case wound its way to the Supreme Court.
Final ruling. The Court held that if the state ordinarily lists the names of both husband and wife on such certificates, then same-sex couples are entitled to have birth certificates listing both parents. The Court noted that laws are unconstitutional if they treat same-sex couples differently than opposite-sex couples. Based on this principle, the Court held that parental birth certificate registration is part of the “constellations of benefits” linked to marriage that the Constitution affords same-sex couples. This ruling applies as a matter of constitutional right in all states.
Read about more interesting Supreme Court decisions
5. Sexual offenders and social media
States struggle to protect children from convicted sex offenders. North Carolina, for example, made it a felony for sex offenders (who had completed their sentences) to use social media sites that “permit minor children to become members or create and maintain personal web pages.”10
At stake. In Packingham v North Carolina, the Court was asked to decide whether this statute violates the First Amendment (free speech) rights of sex offenders.11
Final ruling. The Court held that the North Carolina limitation on sex offenders’ use of social media was too broad. It noted the wide range of political, employment, news, personal, commercial, and religious websites that are off limits to sex offenders under the statute—hardly narrowly tailored. It suggested, however, that it probably would be constitutional for a state to prohibit sex offenders “from engaging in conduct that often presages a sexual crime, like contacting a minor or using a website to gather information about a minor.”11
It was important in this case that the defendant had already served his entire sentence and was “no longer subject to the supervision of the criminal justice system.”11 If he had still been in prison, the state could limit or prohibit his Internet use. Even if he had been on probation or parole (under the supervision of the criminal justice system) the restrictions may well have been permitted. In addition, the state could impose new, narrowly tailored restrictions.
This case is also a reminder that ObGyns are very important in the efforts to eliminate child sexual abuse. All states have laws that require the reporting of known or suspected sexual abuse. In addition to complying with the law, such reports are often critical to discovering and ending the abuse.
6. Transgender rights
The Court had accepted a “transgender bathroom case” in Gloucester County School Board v G.G.12
At stake. This case essentially challenged the Obama Administration’s requirement that schools allow transgender students to use the restrooms in which they feel most comfortable. It was one of the most anticipated cases of the Term, but it essentially disappeared. Following the presidential election, the Department of Education rescinded the earlier guidance on which the case was based.
Final ruling. The Court returned the case to the Fourth Circuit for reconsideration. This issue, however, may reappear before the Court in the form of a claim that the states must provide this accommodation as a matter of federal statutory right, or even Equal Protection.
- In an important First Amendment decision, the Court held that it is a violation of the Freedom of Religion to deny a church-related school access to generally available state grant funds solely because of its religious status (in this case the program funded playground surfacing grants).1
- In several cases, it was apparent that the Court is uncomfortable with the way death penalty cases are handled in some states.2
- Juries may be questioned about racial bias that was expressed during jury deliberations--a substantial change for many courts.3
- The failure of the Patent and Trademark Office (PTO) to register the trademark for the band "The Slants" was a First Amendment violation. One reason that this case was watched was because of the effort of the PTO to deregister the trademark of the Washington Redskins.4
- The Court considered 9 cases involving revoking citizenship, deportation, and cross-border liability (an extraordinary number). Two cases that could change the nature and process of deportation were held over to the next Term for reargument.
- Individualized educational plans under the federal Individuals with Disabilities Education Act (IDEA) must target more than trivial progress for the students.5
References
- Trinity Lutheran Church of Columbia, Inc. v Comer, 582 US 15 577 (2017).
- McAllister S. Death-penalty symposium: A court increasingly uncomfortable with the death penalty. SCOTUSblog.com. http://www.scotusblog.com/2017/06/death-penalty-symposium-court-increasingly-uncomfortable-death-penalty/. Published June 29, 2017. Accessed November 2, 2017.
- Pena-Rodriguez v Colorado, 580 US 15 606 (2017).
- Matal v Tam, 582 US 15 1293 (2017).
- Endrew F v Douglas County School District, RE-1, 580 US 15 827 (2017).
Summary of the Term
The Term was notable for the level of agreement. With 69 decided cases, 41 (69%) were unanimous. In 59 cases (85%), there was a strong consensus, with no more than 2 justices dissenting. Only 7 decisions (10%) were 5 to 4. Justice Kennedy was, as usual, the deciding vote in most of the close cases. He voted in the majority in 97% of the decisions. Justice Gorsuch took the place of Justice Scalia (who passed away in February 2016), so arguably the Court is ideologically close to where it has been for a number of years. Despite rumors that Justice Kennedy would announce his resignation from the Court, neither he nor any other justice has left. The Supreme Court began its new Term on October 2, 2017, with a full complement of 9 justices.
What’s to come
The Court will add cases through much of its new Term, but it has already accepted cases dealing with arbitration agreements (again); public employees’ union dues; immigration (again); the privacy of information held by mobile phone companies; a constitutional challenge to political gerrymandering; bakeries and gay-marriage ceremonies; whistleblowers and Dodd-Frank regulations; sports gambling and the NCAA; and more.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Despite being short-handed (there were only 8 justices for most of the Term), the United States Supreme Court decided a number of important cases during its most recent Term, which concluded on June 27, 2017. Among the 69 cases, several are of particular interest to ObGyns.
1. Arbitration in health care
In Kindred Nursing Centers v Clark, the Court decided an important case involving arbitration in health care.1
At stake. The families of 2 people who died after being in a long-term care facility filed lawsuits against the facility, claiming personal injury, violations of Kentucky statutes regarding long-term care facilities, and wrongful death. However, during admission to the facility, the patients (technically, their agents under a power of attorney) signed an agreement that any disputes would be taken to arbitration. The facility successfully had the lawsuits dismissed.
Final ruling. The Supreme Court agreed that the case had to go to arbitration rather than to court, even though the arbitration clause violated state law. The Federal Arbitration Act (FAA) preempts state law. The Court has been very aggressive in enforcing arbitration agreements and striking down state laws that are inconsistent with the FAA. This case emphasizes that the FAA applies in the health care context.
The case suggests both a warning and an opportunity for health care providers. The warning is that arbitration clauses will be enforced; thoughtlessly entering into arbitration for future disputes may be dangerous. Among other things, the decision of arbitrators is essentially unreviewable. Appellate courts review the decisions of lower courts, but there is no such review in arbitration. Furthermore, arbitration may be stacked in favor of commercial entities that often use arbitrators.
The opportunity for health care providers lies in that it may be possible to include arbitration clauses in agreements with patients. This should be considered only after obtaining legal advice. The agreements should, for example, be consistent with the obligations to patients (in the case of the Kentucky facility, it made clear that accepting the arbitration agreement was not necessary in order to receive care or be admitted to the facility). Because arbitration agreements are becoming ubiquitous and rigorously enforced by federal courts, arbitration is bound to have an important function in health care.
2. Pharmaceuticals
Biologics and biosimilars
Biologics play an important role in health care. Eight of the top 10 selling drugs in 2016 were biologics.2 The case of Sandoz v Amgen involved biosimilar pharmaceuticals, essentially the generics of biologic drugs.3
At stake. While biologics hold great promise in medicine, they are generally very expensive. Just as with generics, brand-name companies (generally referred to as “reference” biologics) want to keep biosimilars off the market for as long as possible, thereby extending the advantages of monopolistic pricing. This Term the Supreme Court considered the statutory rules for licensing biosimilar drugs.
Final ruling. The Court’s decision will allow biosimilar companies to speed up the licensing process by at least 180 days. This is a modest win for patients and their physicians, but the legal issues around biosimilars will need additional attention.
Class action suits
In another case, the Court made it more difficult to file class action suits against pharmaceutical companies in state courts.4 Although this is a fairly technical decision, it is likely to have a significant impact in pharmaceutical liability by limiting classactions.
3. The travel ban
The American College of Obstetricians and Gynecologists joined other medical organizations in an amicus curiae (friend of the court) brief to challenge President Trump’s “travel ban.”5
At stake. The brief argued that the United States “relies upon a significant number of health professionals and scientists who have entered the country through the immigration system.”5
Final ruling. The Court allowed most of the travel ban to stay in place, but did permit entry into the United States by foreign nationals “with a close familial relationship,” or pre-existing ties to US businesses or institutions (such as students who have been admitted to American colleges, workers who have accepted US employment, or lecturers invited to address American audiences).6 Following the Term, the Administration issued a different travel ban, so the issue was taken off the Court’s calendar for the moment. There undoubtedly will be additional chapters to come.
4. Birth certificates and same-sex marriage
In Pavan v Smith, the legal question concerned whether married same-sex couples may have both parents listed on the birth certificate of children born during the marriage.7 Two same-sex couples conceived children through anonymous sperm donation and gave birth in Arkansas. The Department of Health in Arkansas issued birth certificates listing the mother’s name, but refused to list the spouse on the birth certificate.
At stake. The couples brought suit claiming a constitutional right to have both parents listed. In particular, they noted that under Arkansas law, the woman who gives birth is deemed to be the mother. When the woman is married, the husband’s name is “entered on the certificate as the father of the child.”8 The same-sex parents argued that a 2015 decision of the Supreme Court, which held that the Constitution requires states to recognize same-sex marriages, made it clear that same-sex couples should have the benefits of marriage.9 Eventually the case wound its way to the Supreme Court.
Final ruling. The Court held that if the state ordinarily lists the names of both husband and wife on such certificates, then same-sex couples are entitled to have birth certificates listing both parents. The Court noted that laws are unconstitutional if they treat same-sex couples differently than opposite-sex couples. Based on this principle, the Court held that parental birth certificate registration is part of the “constellations of benefits” linked to marriage that the Constitution affords same-sex couples. This ruling applies as a matter of constitutional right in all states.
Read about more interesting Supreme Court decisions
5. Sexual offenders and social media
States struggle to protect children from convicted sex offenders. North Carolina, for example, made it a felony for sex offenders (who had completed their sentences) to use social media sites that “permit minor children to become members or create and maintain personal web pages.”10
At stake. In Packingham v North Carolina, the Court was asked to decide whether this statute violates the First Amendment (free speech) rights of sex offenders.11
Final ruling. The Court held that the North Carolina limitation on sex offenders’ use of social media was too broad. It noted the wide range of political, employment, news, personal, commercial, and religious websites that are off limits to sex offenders under the statute—hardly narrowly tailored. It suggested, however, that it probably would be constitutional for a state to prohibit sex offenders “from engaging in conduct that often presages a sexual crime, like contacting a minor or using a website to gather information about a minor.”11
It was important in this case that the defendant had already served his entire sentence and was “no longer subject to the supervision of the criminal justice system.”11 If he had still been in prison, the state could limit or prohibit his Internet use. Even if he had been on probation or parole (under the supervision of the criminal justice system) the restrictions may well have been permitted. In addition, the state could impose new, narrowly tailored restrictions.
This case is also a reminder that ObGyns are very important in the efforts to eliminate child sexual abuse. All states have laws that require the reporting of known or suspected sexual abuse. In addition to complying with the law, such reports are often critical to discovering and ending the abuse.
6. Transgender rights
The Court had accepted a “transgender bathroom case” in Gloucester County School Board v G.G.12
At stake. This case essentially challenged the Obama Administration’s requirement that schools allow transgender students to use the restrooms in which they feel most comfortable. It was one of the most anticipated cases of the Term, but it essentially disappeared. Following the presidential election, the Department of Education rescinded the earlier guidance on which the case was based.
Final ruling. The Court returned the case to the Fourth Circuit for reconsideration. This issue, however, may reappear before the Court in the form of a claim that the states must provide this accommodation as a matter of federal statutory right, or even Equal Protection.
- In an important First Amendment decision, the Court held that it is a violation of the Freedom of Religion to deny a church-related school access to generally available state grant funds solely because of its religious status (in this case the program funded playground surfacing grants).1
- In several cases, it was apparent that the Court is uncomfortable with the way death penalty cases are handled in some states.2
- Juries may be questioned about racial bias that was expressed during jury deliberations--a substantial change for many courts.3
- The failure of the Patent and Trademark Office (PTO) to register the trademark for the band "The Slants" was a First Amendment violation. One reason that this case was watched was because of the effort of the PTO to deregister the trademark of the Washington Redskins.4
- The Court considered 9 cases involving revoking citizenship, deportation, and cross-border liability (an extraordinary number). Two cases that could change the nature and process of deportation were held over to the next Term for reargument.
- Individualized educational plans under the federal Individuals with Disabilities Education Act (IDEA) must target more than trivial progress for the students.5
References
- Trinity Lutheran Church of Columbia, Inc. v Comer, 582 US 15 577 (2017).
- McAllister S. Death-penalty symposium: A court increasingly uncomfortable with the death penalty. SCOTUSblog.com. http://www.scotusblog.com/2017/06/death-penalty-symposium-court-increasingly-uncomfortable-death-penalty/. Published June 29, 2017. Accessed November 2, 2017.
- Pena-Rodriguez v Colorado, 580 US 15 606 (2017).
- Matal v Tam, 582 US 15 1293 (2017).
- Endrew F v Douglas County School District, RE-1, 580 US 15 827 (2017).
Summary of the Term
The Term was notable for the level of agreement. With 69 decided cases, 41 (69%) were unanimous. In 59 cases (85%), there was a strong consensus, with no more than 2 justices dissenting. Only 7 decisions (10%) were 5 to 4. Justice Kennedy was, as usual, the deciding vote in most of the close cases. He voted in the majority in 97% of the decisions. Justice Gorsuch took the place of Justice Scalia (who passed away in February 2016), so arguably the Court is ideologically close to where it has been for a number of years. Despite rumors that Justice Kennedy would announce his resignation from the Court, neither he nor any other justice has left. The Supreme Court began its new Term on October 2, 2017, with a full complement of 9 justices.
What’s to come
The Court will add cases through much of its new Term, but it has already accepted cases dealing with arbitration agreements (again); public employees’ union dues; immigration (again); the privacy of information held by mobile phone companies; a constitutional challenge to political gerrymandering; bakeries and gay-marriage ceremonies; whistleblowers and Dodd-Frank regulations; sports gambling and the NCAA; and more.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kindred Nursing Centers, LP v Clark, 581 US 16 32 (2017).
- Anderson L. Looking Ahead: Pharma Projections for 2016 - & Beyond. Perma.cc Website. . Reviewed March 30, 2017. Accessed November 2, 2017.
- Sandoz Inc v Amgen Inc, 581 US 15 1039 1195 (2017).
- Bristol-Myers Squibb Co v Superior Court of California, San Francisco County, 582 US 16 466 (2017).
- Trinity FR, Sterling AM, Rogaczewski JD, et al. Motion for Leave to File and Brief for the Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents. SCOTUSblog. http://www.scotusblog.com/wp-content/uploads/2017/06/16-1436-ac-AAMC-supporting-respondents.pdf. Accessed November 2, 2017.
- Donald J. Trump, President of the United States v International Refugee Assistance Project, 582 US 16 1436 (2017).
- Pavan v Smith, 582 US 16 992 (2017).
- Arkansas Code, §20 18 401(f)(1) (2014).
- Obergefell v Hodges, 576 US ___ (2015).
- NC Gen. Stat. Ann. §§14-202.5(a),(e).
- Packingham v North Carolina, 582 US 15 1194 (2017).
- Gloucester County School Board v G.G. SCOTUSblog. http://www.scotusblog.com/case-files/cases/gloucester-county-school-board-v-g-g/. Published March 6, 2017. Accessed November 2, 2017.
- Kindred Nursing Centers, LP v Clark, 581 US 16 32 (2017).
- Anderson L. Looking Ahead: Pharma Projections for 2016 - & Beyond. Perma.cc Website. . Reviewed March 30, 2017. Accessed November 2, 2017.
- Sandoz Inc v Amgen Inc, 581 US 15 1039 1195 (2017).
- Bristol-Myers Squibb Co v Superior Court of California, San Francisco County, 582 US 16 466 (2017).
- Trinity FR, Sterling AM, Rogaczewski JD, et al. Motion for Leave to File and Brief for the Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents. SCOTUSblog. http://www.scotusblog.com/wp-content/uploads/2017/06/16-1436-ac-AAMC-supporting-respondents.pdf. Accessed November 2, 2017.
- Donald J. Trump, President of the United States v International Refugee Assistance Project, 582 US 16 1436 (2017).
- Pavan v Smith, 582 US 16 992 (2017).
- Arkansas Code, §20 18 401(f)(1) (2014).
- Obergefell v Hodges, 576 US ___ (2015).
- NC Gen. Stat. Ann. §§14-202.5(a),(e).
- Packingham v North Carolina, 582 US 15 1194 (2017).
- Gloucester County School Board v G.G. SCOTUSblog. http://www.scotusblog.com/case-files/cases/gloucester-county-school-board-v-g-g/. Published March 6, 2017. Accessed November 2, 2017.
Reengineering your office to be perfect for your patients
Independent of the Affordable Care Act or any upcoming changes in health care, the focus of an ObGyn practice remains paramount: the patient comes first.
The “recipe” for creating patient satisfaction and service excellence is predicated upon the mission of your practice and creating a shared vision with your employees. An action plan that is created and “visited/revisited”on a regular basis will serve to keep all abreast of the latest information to enhance the quality of patient care. It goes without saying, the ObGyn must first “lead by example” and always strive for satisfied patients who will tell their friends about your practice.
Start with the right tools
To organize a practice well, you need the right tools, which ideally include mission and vision statements and an action plan with goals and objectives.
Mission statement
A mission statement can be developed by the ObGyn(s) in your office or in concert with your staff. It should include:
- the “here and now” focus on the current approach to patient care
- why the practice exists (Develop a brief description of your practice, including the desired patient population.)
- the products and services offered and why and how those services are provided.
Here is an example of a mission statement for an ObGyn practice: “Our mission is to provide excellent, exceptional, personalized care for women of all ages in a warm and friendly environment. We incorporate leading-edge technology in our practice and continue to be a leader in obstetrics and gynecology.”
Vision statement
A vision statement should be developed in concert with your staff. It should include:
- the “then and there” focus on the historic perspective of your practice
- the ObGyn(s) and staff vision of the future
- what the ObGyn(s) and staff want to create.
The vision statement should energize and excite your personnel, create a shared and meaningful purpose, inspire passion and interest, and convey the values you want to share in your practice.
Here is an example of a vision statement for an ObGyn practice: “We aim to become the premier obstetrics and gynecology pro-vider to residents of (location) community.”
Action plan: Setting goals
To succeed, an ObGyn practice needs to:
- develop targets and challenges reflecting periodic (quarterly) meetings with staff and new entity development in the practice
- establish benchmarks and measurable parameters (How do you compare with other local practices? Set criteria/metrics to assess your progress.)
- ensure that the objectives support the goals (Develop goals and objectives over a defined period of time.)
- revisit the goals (Have they have been met? Do they need revision?)
Goals and objectives are essential for the continued health of your practice. This is all predicated upon developing a competitive advantage and then maintaining it.
Read about how to make a positive first impression on a new patient.
Is the environment welcoming?
When we examine a practice from the patient’s point of view, a good starting place is with the front desk. Have you looked at your front desk “from the outside in?” In one sense, this is the showcase of your practice.
Related article:
Four pillars of a successful practice: 2. Attract new patients
The first impression: Appointment scheduling
The first impression a patient receives about your practice occurs when she attempts to set up an appointment. Perhaps you might ask someone to call in to schedule an appointment. Is the caller immediately put on hold? Are your personnel courteous on the phone? Can she be seen quickly if she has a problem? How long is the wait for an annual exam? A test run can be very revealing.
Walk in the front door
When a patient walks in the door, does the physical office space radiate a friendly, relaxed atmosphere? Walk through the waiting room, then consultation and exam rooms as if you are a patient seeing it for the first time. Have you created an environment in which patients sense a well-organized office and the esprit de corps of the personnel? Does it look and smell fresh and clean? This all sends a loud and clear positive message about your practice.1–3
Here are some suggestions for making a waiting room more inviting:
- Provide a seating arrangement that is “patient centered.” For example, semi- circular arrangements allow easy viewing of any monitors in the waiting room.
- WiFi is a great addition. Post several signs with the user name and password.
- Offer computers for patients to use to complete registration
- Set up a fish tank. If well-maintained, it can be soothing to many people.
- Display medical information pamphlets, even if they are rarely taken.
- Provide a big screen television that offers information about your practice, including personnel and procedures.
Streaming ads for physician offices are available. One platform, Outcome Health (https://www.outcomehealth.com), provides flat-screen TVs and tablets that show patient education videos.4 Another vendor, Patient Point (http://patientpoint.com), offers waiting room networks, editorials, and other communications designed to support “the goals of improving healthcare.”5 Other available media include channel news and music programming to relax patients.6
Wait times. A patient’s perceived wait time and the actual wait time are often quite different. How long she waits to see the ObGyn is “numero uno” with regard to patient satisfaction and can be a key source of annoyance, irritability, stress, and anger.
Does someone inform waiting patients that the ObGyn is running late? Does staff at the front desk or perhaps your medical assistant inquire, “Can I get you anything? The doctor is running late,” or “Dr. Jones has just finished delivering a baby. He’ll be here in 10 minutes. He’ll see you first.”
Consultation and exam rooms
Suggestions to develop a relaxing environment in your consultation and exam rooms are7:
- decorate the walls with soft, pastel colors
- use “spa aesthetics” to create a colorful atmosphere with appropriate lighting, artwork, and modern furnishings
- present a few magazines neatly and update them periodically
- stock and appropriately maintain the patients rooms with medical supplies
- remember, “Subjects perceive people more positively in beautiful rooms than in ugly rooms.”5
Read about how to keep your patients satisfied and your business stable.
Set the lead example
The need for open and supportive communication between you and your office staff cannot be overly emphasized. An ideal office staff member understands and shares in the vision, is aware of stated goals and objectives, is responsive to patient needs, and wants to create a win-win environment.
Frequently discuss your expectations with your staff. Expect them to be responsive, courteous, competent, have good communication skills, and be influenced by the appearance of the physical environ-ment. Provide support and educational tools to help them successfully perform their work.
Related article:
Four pillars of a successful practice: 1. Keep your current patients happy
Discover your patients’ vision of customer service
Formal measurement of patient satisfaction began with Professor Irwin Press at the University of Notre Dame. Rod Ganey, a sociologist and statistician, then developed the Press Ganey Patient Satisfaction Survey. These points earlier conveyed by Maslow and Mintz8 addressed the “effects of esthetic surroundings.” Color and art proved to be preferences in an esthetically pleasing environment. Additional historical information has been provided by Siegrist, who addressed “the patient experience.”9 He cites the myth that patients do not fill out satisfaction surveys. Indeed they do. Patient satisfaction is not a personality contest but rather a reflection of the health care provider’s investment of time and effort to offer patient-centered care. Siegrist also notes that the patient’s family plays a key role in how a patient perceives her experience with her health care professional.9
The federal government has been actively involved in assessing patient satisfaction in the hospital setting since 2002. This is reflected in the Centers for Medicare and Medicaid Services, the Agency for Healthcare Research and Quality, and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys. The HCAHPS is a 27-question survey randomly administered to adult inpatients after discharge.10–12
The following metrics are often included in patient satisfaction surveys9,10:
- rating of hospital care from 0 (lowest) to 10 (highest)
- percentage of patients who would recommend a practice to family and friends
- number of patients who say their health care providers always communicate well
- the number of patients who report that the office is always clean and friendly.
Use of search engines focused on health care patient surveys can provide a number of options for clinicians to use in their practice.
Tips on patient satisfaction
Several interesting tips from the busi-ness world can be applied to an ObGyn’s practice14:
- You will only hear from 4% of unhappy customers.
- One dissatisfied customer tells 9.
- 95% of customers with resolved issues will do business with you again.
- If a problem is not addressed, that patient will tell 10 others.
- Resolve the problem and 5 people will know about it.
- It costs 5 times as much effort to gain 1 new customer.
- Loyal customers in 1 area of service are good prospects for other (new) services.
Related article:
Using the Internet in your practice. Part 2: Generating new patients using social media
Tell stories about good, satisfied patients
Sharing the stories of satisfied patients motivates others to consider coming to your practice. To develop these stories, offer a “suggestion box” where patients can leave compliments or comments about their experiences. Ask patients to record their positive reviews (be sure to obtain written consent before recording and publishing). Show the videos on the big-screen TVs in your waiting room and include patient reviews (written, audio, and video) on your website.15
Related article:
Four pillars of a successful practice: 4. Motivate your staff
Reevaluate periodically
Encouraging team spirit makes good business sense. Offer staff members bonuses for coming up with improved processes. Provide educational programs for staff on patient care, technology, etc. If a difficult experience occurs, discuss it openly with staff members without accusing, asking them for suggestions to improve the situation.16
To assess the monetary value of your practice, you need to know what contributes to your profit margin and overhead. What investments are the most profitable? Then monitor each segment of the office practice.
Should you proceed with a purchase? Should you take on a new hire? Let's look at one excellent model from the Boston Consulting Group (FIGURE) that provides insight into "low and high performance" aspects of business or practice.1
In the matrix, Stars use large amounts of cash and are leaders in cash generation. Stars lead to development of a Cash Cow, which are entities that generate profits and cash with low investment prerequisites. Dogs are segments of product and service line(s) that should be carefully reevaluated. A decision must be made to liquidate if the problem cannot be corrected. Question Marks have the worst cash characteristics of all and are associated with high demands and low profit margin(s).1
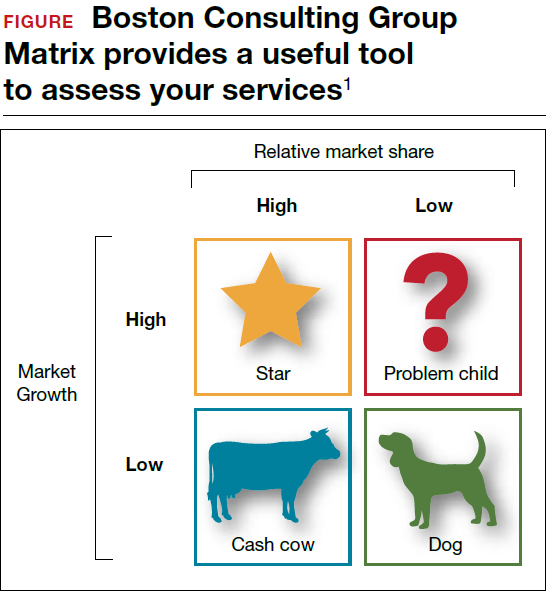
SWOT analysis
A SWOT analysis is most helpful when assessing a practice in real time. The basic tenets are2:
Strengths:
- prestigious reputation
- technological expertise
Weaknesses:
- antiquated computer system
- lack of experience in specific areas
Opportunities:
- growing market demand for a specific product or procedure
- provision of unique services
Threats:
- changing demographics
- competitive practices
- changes in health care third-party payers.
The American College of Obstetricians and Gynecologists (ACOG) has developed an "ACOG Medical Home Toolkit" to allow ObGyns to assess how significant the changes regarding payers will be to their practice. Sections include the patient/practice partnership support; clinical care information; community resources; care delivery management; performance measurement and improvement; and payment and finance.3 The toolkit is available for download from the ACOG website.
References
- Morrison A, Wensley R. Boxing up or boxed in? A short history of the Boston Consulting Group Share/Growth Matrix. J Market Manag. 1993;7(2):105-129. http://www.tandfonline.com/doi/abs/10.1080/0267257X.1991.9964145.
- Klasko SK, Toub DB. It's not a plan without a business plan. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:36-37.
- American Congress of Obstetricians and Gynecologists. ACOG Medical Home Toolkit. https://www.acog.org/About-ACOG/ACOG-Departments/Practice-Management-and-Managed-Care/ACOG-Medical-Home-Toolkit. Accessed August 14, 2017.
Bottom line
Ensuring that your patients have an outstanding experience is a smart business strategy. A unified approach that includes team members’ involvement to create a patient-centered environment will provide a quality experience and encourage patients to recommend your ObGyn practice to others.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Ulrich RS. Evidence-based environmental design for improving medical outcomes: Paper Delivered at a Conference Entitled Healing by Design: Building for Health Care in the 21st Century. Montreal: McGill University Health Centre; 2000. http://www.brikbase.org/sites/default/files/Evidence%20Based%20Environmental%20Design%20for%20Improving%20Medical.pdf. Accessed August 15, 2017.
- Becker F, Douglass S. The ecology of the patient visit: physical attractiveness, waiting times and perceived quality of care. J Ambul Care Manag. 2008;31(2):128–141.
- Becker F, Sweeney B, Parsons K. Ambulatory facility design and patients’ perceptions of healthcare quality. HERD. 2008;1(4):35–54.
- Outcome Health Website. https://www.outcomehealth.com/. Accessed August 14, 2017.
- Mazer SE. The waiting room: Where suffering begins. Healing Healthcare Systems website. http://www.healinghealth.com/waiting-room-suffering-begins/. Published November 7, 2014. Accessed August 14, 2017.
- Patient Point Programs Website. http://patientpoint.com/. Accessed August 14, 2017.
- Almquist J, Kelly C, Bromberg J, Bryant S, Christianson T, Montori V. Consultation room design and the clinical encounter: the space and interaction randomized trial. Health Environ Res Design. 2009;3(1):41–78.
- Maslow A, Mintz N. Effects of esthetic surroundings: I. Initial effects of three esthetic conditions upon perceiving “energy” and “well-being” in faces. J Psychology. 1956;41(2):247–254.
- Siegrist RB. The patient experience. In: Sanfilippo JS, Bieber E, Javich D, Siegrist R, eds. MBA for Healthcare. New York, NY: Oxford Press;2016:227–236.
- Press I. Patient satisfaction: Understanding and managing the experience of care. 2nd ed. Chicago, IL: Health Administration Press; 2005:66–78.
- Piper L, Tallman E. Hospital consumer assessment of healthcare providers and systems: An ethical leadership dilemma to satisfy patients. Health Care Manag (Frederick). 2016;35(2):151–155.
- Giordano L, Elliott M, Goldstein E, Lehrman W, Spencer P. Development, implementation and public reporting of HCAHPS survey. Med Care Res Rev. 2010;67(1):27–37.
- Jones KE. Helping the health profession help others: Applying business principles to the medical world. University of Tennessee, Knoxville Honors Thesis Projects. http://trace.tennessee.edu/cgi/viewcontent.cgi?article=1560&context=utk_chanhonoproj. Published 2002. Accessed August 14, 2017.
- Baum N. Marketing your practice: ethically, effectively and economically. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:123–154.
- Baum NH. Four pillars of a successful practice: 1. Keep your current patients happy. OBG Manag. 2013;25(3):49–56.
- Baum NH. Four pillars of a successful practice: 4. Motivate your staff. OBG Manag. 2013;25(8):29–33.
Independent of the Affordable Care Act or any upcoming changes in health care, the focus of an ObGyn practice remains paramount: the patient comes first.
The “recipe” for creating patient satisfaction and service excellence is predicated upon the mission of your practice and creating a shared vision with your employees. An action plan that is created and “visited/revisited”on a regular basis will serve to keep all abreast of the latest information to enhance the quality of patient care. It goes without saying, the ObGyn must first “lead by example” and always strive for satisfied patients who will tell their friends about your practice.
Start with the right tools
To organize a practice well, you need the right tools, which ideally include mission and vision statements and an action plan with goals and objectives.
Mission statement
A mission statement can be developed by the ObGyn(s) in your office or in concert with your staff. It should include:
- the “here and now” focus on the current approach to patient care
- why the practice exists (Develop a brief description of your practice, including the desired patient population.)
- the products and services offered and why and how those services are provided.
Here is an example of a mission statement for an ObGyn practice: “Our mission is to provide excellent, exceptional, personalized care for women of all ages in a warm and friendly environment. We incorporate leading-edge technology in our practice and continue to be a leader in obstetrics and gynecology.”
Vision statement
A vision statement should be developed in concert with your staff. It should include:
- the “then and there” focus on the historic perspective of your practice
- the ObGyn(s) and staff vision of the future
- what the ObGyn(s) and staff want to create.
The vision statement should energize and excite your personnel, create a shared and meaningful purpose, inspire passion and interest, and convey the values you want to share in your practice.
Here is an example of a vision statement for an ObGyn practice: “We aim to become the premier obstetrics and gynecology pro-vider to residents of (location) community.”
Action plan: Setting goals
To succeed, an ObGyn practice needs to:
- develop targets and challenges reflecting periodic (quarterly) meetings with staff and new entity development in the practice
- establish benchmarks and measurable parameters (How do you compare with other local practices? Set criteria/metrics to assess your progress.)
- ensure that the objectives support the goals (Develop goals and objectives over a defined period of time.)
- revisit the goals (Have they have been met? Do they need revision?)
Goals and objectives are essential for the continued health of your practice. This is all predicated upon developing a competitive advantage and then maintaining it.
Read about how to make a positive first impression on a new patient.
Is the environment welcoming?
When we examine a practice from the patient’s point of view, a good starting place is with the front desk. Have you looked at your front desk “from the outside in?” In one sense, this is the showcase of your practice.
Related article:
Four pillars of a successful practice: 2. Attract new patients
The first impression: Appointment scheduling
The first impression a patient receives about your practice occurs when she attempts to set up an appointment. Perhaps you might ask someone to call in to schedule an appointment. Is the caller immediately put on hold? Are your personnel courteous on the phone? Can she be seen quickly if she has a problem? How long is the wait for an annual exam? A test run can be very revealing.
Walk in the front door
When a patient walks in the door, does the physical office space radiate a friendly, relaxed atmosphere? Walk through the waiting room, then consultation and exam rooms as if you are a patient seeing it for the first time. Have you created an environment in which patients sense a well-organized office and the esprit de corps of the personnel? Does it look and smell fresh and clean? This all sends a loud and clear positive message about your practice.1–3
Here are some suggestions for making a waiting room more inviting:
- Provide a seating arrangement that is “patient centered.” For example, semi- circular arrangements allow easy viewing of any monitors in the waiting room.
- WiFi is a great addition. Post several signs with the user name and password.
- Offer computers for patients to use to complete registration
- Set up a fish tank. If well-maintained, it can be soothing to many people.
- Display medical information pamphlets, even if they are rarely taken.
- Provide a big screen television that offers information about your practice, including personnel and procedures.
Streaming ads for physician offices are available. One platform, Outcome Health (https://www.outcomehealth.com), provides flat-screen TVs and tablets that show patient education videos.4 Another vendor, Patient Point (http://patientpoint.com), offers waiting room networks, editorials, and other communications designed to support “the goals of improving healthcare.”5 Other available media include channel news and music programming to relax patients.6
Wait times. A patient’s perceived wait time and the actual wait time are often quite different. How long she waits to see the ObGyn is “numero uno” with regard to patient satisfaction and can be a key source of annoyance, irritability, stress, and anger.
Does someone inform waiting patients that the ObGyn is running late? Does staff at the front desk or perhaps your medical assistant inquire, “Can I get you anything? The doctor is running late,” or “Dr. Jones has just finished delivering a baby. He’ll be here in 10 minutes. He’ll see you first.”
Consultation and exam rooms
Suggestions to develop a relaxing environment in your consultation and exam rooms are7:
- decorate the walls with soft, pastel colors
- use “spa aesthetics” to create a colorful atmosphere with appropriate lighting, artwork, and modern furnishings
- present a few magazines neatly and update them periodically
- stock and appropriately maintain the patients rooms with medical supplies
- remember, “Subjects perceive people more positively in beautiful rooms than in ugly rooms.”5
Read about how to keep your patients satisfied and your business stable.
Set the lead example
The need for open and supportive communication between you and your office staff cannot be overly emphasized. An ideal office staff member understands and shares in the vision, is aware of stated goals and objectives, is responsive to patient needs, and wants to create a win-win environment.
Frequently discuss your expectations with your staff. Expect them to be responsive, courteous, competent, have good communication skills, and be influenced by the appearance of the physical environ-ment. Provide support and educational tools to help them successfully perform their work.
Related article:
Four pillars of a successful practice: 1. Keep your current patients happy
Discover your patients’ vision of customer service
Formal measurement of patient satisfaction began with Professor Irwin Press at the University of Notre Dame. Rod Ganey, a sociologist and statistician, then developed the Press Ganey Patient Satisfaction Survey. These points earlier conveyed by Maslow and Mintz8 addressed the “effects of esthetic surroundings.” Color and art proved to be preferences in an esthetically pleasing environment. Additional historical information has been provided by Siegrist, who addressed “the patient experience.”9 He cites the myth that patients do not fill out satisfaction surveys. Indeed they do. Patient satisfaction is not a personality contest but rather a reflection of the health care provider’s investment of time and effort to offer patient-centered care. Siegrist also notes that the patient’s family plays a key role in how a patient perceives her experience with her health care professional.9
The federal government has been actively involved in assessing patient satisfaction in the hospital setting since 2002. This is reflected in the Centers for Medicare and Medicaid Services, the Agency for Healthcare Research and Quality, and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys. The HCAHPS is a 27-question survey randomly administered to adult inpatients after discharge.10–12
The following metrics are often included in patient satisfaction surveys9,10:
- rating of hospital care from 0 (lowest) to 10 (highest)
- percentage of patients who would recommend a practice to family and friends
- number of patients who say their health care providers always communicate well
- the number of patients who report that the office is always clean and friendly.
Use of search engines focused on health care patient surveys can provide a number of options for clinicians to use in their practice.
Tips on patient satisfaction
Several interesting tips from the busi-ness world can be applied to an ObGyn’s practice14:
- You will only hear from 4% of unhappy customers.
- One dissatisfied customer tells 9.
- 95% of customers with resolved issues will do business with you again.
- If a problem is not addressed, that patient will tell 10 others.
- Resolve the problem and 5 people will know about it.
- It costs 5 times as much effort to gain 1 new customer.
- Loyal customers in 1 area of service are good prospects for other (new) services.
Related article:
Using the Internet in your practice. Part 2: Generating new patients using social media
Tell stories about good, satisfied patients
Sharing the stories of satisfied patients motivates others to consider coming to your practice. To develop these stories, offer a “suggestion box” where patients can leave compliments or comments about their experiences. Ask patients to record their positive reviews (be sure to obtain written consent before recording and publishing). Show the videos on the big-screen TVs in your waiting room and include patient reviews (written, audio, and video) on your website.15
Related article:
Four pillars of a successful practice: 4. Motivate your staff
Reevaluate periodically
Encouraging team spirit makes good business sense. Offer staff members bonuses for coming up with improved processes. Provide educational programs for staff on patient care, technology, etc. If a difficult experience occurs, discuss it openly with staff members without accusing, asking them for suggestions to improve the situation.16
To assess the monetary value of your practice, you need to know what contributes to your profit margin and overhead. What investments are the most profitable? Then monitor each segment of the office practice.
Should you proceed with a purchase? Should you take on a new hire? Let's look at one excellent model from the Boston Consulting Group (FIGURE) that provides insight into "low and high performance" aspects of business or practice.1
In the matrix, Stars use large amounts of cash and are leaders in cash generation. Stars lead to development of a Cash Cow, which are entities that generate profits and cash with low investment prerequisites. Dogs are segments of product and service line(s) that should be carefully reevaluated. A decision must be made to liquidate if the problem cannot be corrected. Question Marks have the worst cash characteristics of all and are associated with high demands and low profit margin(s).1
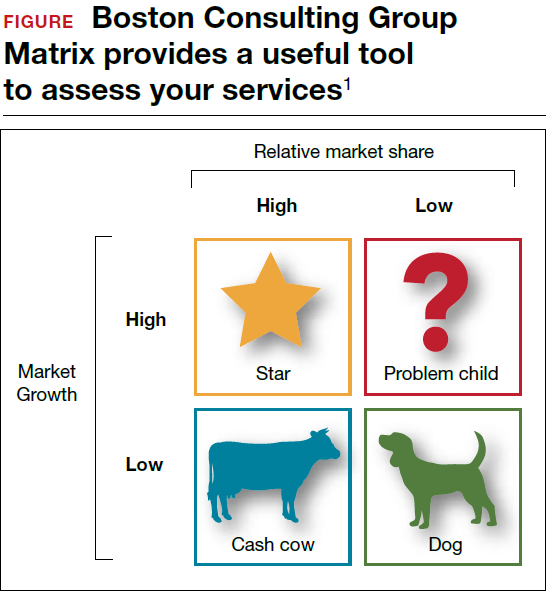
SWOT analysis
A SWOT analysis is most helpful when assessing a practice in real time. The basic tenets are2:
Strengths:
- prestigious reputation
- technological expertise
Weaknesses:
- antiquated computer system
- lack of experience in specific areas
Opportunities:
- growing market demand for a specific product or procedure
- provision of unique services
Threats:
- changing demographics
- competitive practices
- changes in health care third-party payers.
The American College of Obstetricians and Gynecologists (ACOG) has developed an "ACOG Medical Home Toolkit" to allow ObGyns to assess how significant the changes regarding payers will be to their practice. Sections include the patient/practice partnership support; clinical care information; community resources; care delivery management; performance measurement and improvement; and payment and finance.3 The toolkit is available for download from the ACOG website.
References
- Morrison A, Wensley R. Boxing up or boxed in? A short history of the Boston Consulting Group Share/Growth Matrix. J Market Manag. 1993;7(2):105-129. http://www.tandfonline.com/doi/abs/10.1080/0267257X.1991.9964145.
- Klasko SK, Toub DB. It's not a plan without a business plan. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:36-37.
- American Congress of Obstetricians and Gynecologists. ACOG Medical Home Toolkit. https://www.acog.org/About-ACOG/ACOG-Departments/Practice-Management-and-Managed-Care/ACOG-Medical-Home-Toolkit. Accessed August 14, 2017.
Bottom line
Ensuring that your patients have an outstanding experience is a smart business strategy. A unified approach that includes team members’ involvement to create a patient-centered environment will provide a quality experience and encourage patients to recommend your ObGyn practice to others.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Independent of the Affordable Care Act or any upcoming changes in health care, the focus of an ObGyn practice remains paramount: the patient comes first.
The “recipe” for creating patient satisfaction and service excellence is predicated upon the mission of your practice and creating a shared vision with your employees. An action plan that is created and “visited/revisited”on a regular basis will serve to keep all abreast of the latest information to enhance the quality of patient care. It goes without saying, the ObGyn must first “lead by example” and always strive for satisfied patients who will tell their friends about your practice.
Start with the right tools
To organize a practice well, you need the right tools, which ideally include mission and vision statements and an action plan with goals and objectives.
Mission statement
A mission statement can be developed by the ObGyn(s) in your office or in concert with your staff. It should include:
- the “here and now” focus on the current approach to patient care
- why the practice exists (Develop a brief description of your practice, including the desired patient population.)
- the products and services offered and why and how those services are provided.
Here is an example of a mission statement for an ObGyn practice: “Our mission is to provide excellent, exceptional, personalized care for women of all ages in a warm and friendly environment. We incorporate leading-edge technology in our practice and continue to be a leader in obstetrics and gynecology.”
Vision statement
A vision statement should be developed in concert with your staff. It should include:
- the “then and there” focus on the historic perspective of your practice
- the ObGyn(s) and staff vision of the future
- what the ObGyn(s) and staff want to create.
The vision statement should energize and excite your personnel, create a shared and meaningful purpose, inspire passion and interest, and convey the values you want to share in your practice.
Here is an example of a vision statement for an ObGyn practice: “We aim to become the premier obstetrics and gynecology pro-vider to residents of (location) community.”
Action plan: Setting goals
To succeed, an ObGyn practice needs to:
- develop targets and challenges reflecting periodic (quarterly) meetings with staff and new entity development in the practice
- establish benchmarks and measurable parameters (How do you compare with other local practices? Set criteria/metrics to assess your progress.)
- ensure that the objectives support the goals (Develop goals and objectives over a defined period of time.)
- revisit the goals (Have they have been met? Do they need revision?)
Goals and objectives are essential for the continued health of your practice. This is all predicated upon developing a competitive advantage and then maintaining it.
Read about how to make a positive first impression on a new patient.
Is the environment welcoming?
When we examine a practice from the patient’s point of view, a good starting place is with the front desk. Have you looked at your front desk “from the outside in?” In one sense, this is the showcase of your practice.
Related article:
Four pillars of a successful practice: 2. Attract new patients
The first impression: Appointment scheduling
The first impression a patient receives about your practice occurs when she attempts to set up an appointment. Perhaps you might ask someone to call in to schedule an appointment. Is the caller immediately put on hold? Are your personnel courteous on the phone? Can she be seen quickly if she has a problem? How long is the wait for an annual exam? A test run can be very revealing.
Walk in the front door
When a patient walks in the door, does the physical office space radiate a friendly, relaxed atmosphere? Walk through the waiting room, then consultation and exam rooms as if you are a patient seeing it for the first time. Have you created an environment in which patients sense a well-organized office and the esprit de corps of the personnel? Does it look and smell fresh and clean? This all sends a loud and clear positive message about your practice.1–3
Here are some suggestions for making a waiting room more inviting:
- Provide a seating arrangement that is “patient centered.” For example, semi- circular arrangements allow easy viewing of any monitors in the waiting room.
- WiFi is a great addition. Post several signs with the user name and password.
- Offer computers for patients to use to complete registration
- Set up a fish tank. If well-maintained, it can be soothing to many people.
- Display medical information pamphlets, even if they are rarely taken.
- Provide a big screen television that offers information about your practice, including personnel and procedures.
Streaming ads for physician offices are available. One platform, Outcome Health (https://www.outcomehealth.com), provides flat-screen TVs and tablets that show patient education videos.4 Another vendor, Patient Point (http://patientpoint.com), offers waiting room networks, editorials, and other communications designed to support “the goals of improving healthcare.”5 Other available media include channel news and music programming to relax patients.6
Wait times. A patient’s perceived wait time and the actual wait time are often quite different. How long she waits to see the ObGyn is “numero uno” with regard to patient satisfaction and can be a key source of annoyance, irritability, stress, and anger.
Does someone inform waiting patients that the ObGyn is running late? Does staff at the front desk or perhaps your medical assistant inquire, “Can I get you anything? The doctor is running late,” or “Dr. Jones has just finished delivering a baby. He’ll be here in 10 minutes. He’ll see you first.”
Consultation and exam rooms
Suggestions to develop a relaxing environment in your consultation and exam rooms are7:
- decorate the walls with soft, pastel colors
- use “spa aesthetics” to create a colorful atmosphere with appropriate lighting, artwork, and modern furnishings
- present a few magazines neatly and update them periodically
- stock and appropriately maintain the patients rooms with medical supplies
- remember, “Subjects perceive people more positively in beautiful rooms than in ugly rooms.”5
Read about how to keep your patients satisfied and your business stable.
Set the lead example
The need for open and supportive communication between you and your office staff cannot be overly emphasized. An ideal office staff member understands and shares in the vision, is aware of stated goals and objectives, is responsive to patient needs, and wants to create a win-win environment.
Frequently discuss your expectations with your staff. Expect them to be responsive, courteous, competent, have good communication skills, and be influenced by the appearance of the physical environ-ment. Provide support and educational tools to help them successfully perform their work.
Related article:
Four pillars of a successful practice: 1. Keep your current patients happy
Discover your patients’ vision of customer service
Formal measurement of patient satisfaction began with Professor Irwin Press at the University of Notre Dame. Rod Ganey, a sociologist and statistician, then developed the Press Ganey Patient Satisfaction Survey. These points earlier conveyed by Maslow and Mintz8 addressed the “effects of esthetic surroundings.” Color and art proved to be preferences in an esthetically pleasing environment. Additional historical information has been provided by Siegrist, who addressed “the patient experience.”9 He cites the myth that patients do not fill out satisfaction surveys. Indeed they do. Patient satisfaction is not a personality contest but rather a reflection of the health care provider’s investment of time and effort to offer patient-centered care. Siegrist also notes that the patient’s family plays a key role in how a patient perceives her experience with her health care professional.9
The federal government has been actively involved in assessing patient satisfaction in the hospital setting since 2002. This is reflected in the Centers for Medicare and Medicaid Services, the Agency for Healthcare Research and Quality, and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys. The HCAHPS is a 27-question survey randomly administered to adult inpatients after discharge.10–12
The following metrics are often included in patient satisfaction surveys9,10:
- rating of hospital care from 0 (lowest) to 10 (highest)
- percentage of patients who would recommend a practice to family and friends
- number of patients who say their health care providers always communicate well
- the number of patients who report that the office is always clean and friendly.
Use of search engines focused on health care patient surveys can provide a number of options for clinicians to use in their practice.
Tips on patient satisfaction
Several interesting tips from the busi-ness world can be applied to an ObGyn’s practice14:
- You will only hear from 4% of unhappy customers.
- One dissatisfied customer tells 9.
- 95% of customers with resolved issues will do business with you again.
- If a problem is not addressed, that patient will tell 10 others.
- Resolve the problem and 5 people will know about it.
- It costs 5 times as much effort to gain 1 new customer.
- Loyal customers in 1 area of service are good prospects for other (new) services.
Related article:
Using the Internet in your practice. Part 2: Generating new patients using social media
Tell stories about good, satisfied patients
Sharing the stories of satisfied patients motivates others to consider coming to your practice. To develop these stories, offer a “suggestion box” where patients can leave compliments or comments about their experiences. Ask patients to record their positive reviews (be sure to obtain written consent before recording and publishing). Show the videos on the big-screen TVs in your waiting room and include patient reviews (written, audio, and video) on your website.15
Related article:
Four pillars of a successful practice: 4. Motivate your staff
Reevaluate periodically
Encouraging team spirit makes good business sense. Offer staff members bonuses for coming up with improved processes. Provide educational programs for staff on patient care, technology, etc. If a difficult experience occurs, discuss it openly with staff members without accusing, asking them for suggestions to improve the situation.16
To assess the monetary value of your practice, you need to know what contributes to your profit margin and overhead. What investments are the most profitable? Then monitor each segment of the office practice.
Should you proceed with a purchase? Should you take on a new hire? Let's look at one excellent model from the Boston Consulting Group (FIGURE) that provides insight into "low and high performance" aspects of business or practice.1
In the matrix, Stars use large amounts of cash and are leaders in cash generation. Stars lead to development of a Cash Cow, which are entities that generate profits and cash with low investment prerequisites. Dogs are segments of product and service line(s) that should be carefully reevaluated. A decision must be made to liquidate if the problem cannot be corrected. Question Marks have the worst cash characteristics of all and are associated with high demands and low profit margin(s).1
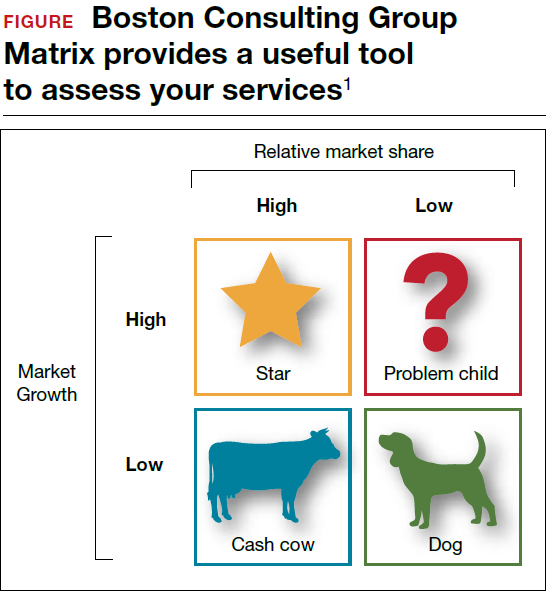
SWOT analysis
A SWOT analysis is most helpful when assessing a practice in real time. The basic tenets are2:
Strengths:
- prestigious reputation
- technological expertise
Weaknesses:
- antiquated computer system
- lack of experience in specific areas
Opportunities:
- growing market demand for a specific product or procedure
- provision of unique services
Threats:
- changing demographics
- competitive practices
- changes in health care third-party payers.
The American College of Obstetricians and Gynecologists (ACOG) has developed an "ACOG Medical Home Toolkit" to allow ObGyns to assess how significant the changes regarding payers will be to their practice. Sections include the patient/practice partnership support; clinical care information; community resources; care delivery management; performance measurement and improvement; and payment and finance.3 The toolkit is available for download from the ACOG website.
References
- Morrison A, Wensley R. Boxing up or boxed in? A short history of the Boston Consulting Group Share/Growth Matrix. J Market Manag. 1993;7(2):105-129. http://www.tandfonline.com/doi/abs/10.1080/0267257X.1991.9964145.
- Klasko SK, Toub DB. It's not a plan without a business plan. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:36-37.
- American Congress of Obstetricians and Gynecologists. ACOG Medical Home Toolkit. https://www.acog.org/About-ACOG/ACOG-Departments/Practice-Management-and-Managed-Care/ACOG-Medical-Home-Toolkit. Accessed August 14, 2017.
Bottom line
Ensuring that your patients have an outstanding experience is a smart business strategy. A unified approach that includes team members’ involvement to create a patient-centered environment will provide a quality experience and encourage patients to recommend your ObGyn practice to others.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Ulrich RS. Evidence-based environmental design for improving medical outcomes: Paper Delivered at a Conference Entitled Healing by Design: Building for Health Care in the 21st Century. Montreal: McGill University Health Centre; 2000. http://www.brikbase.org/sites/default/files/Evidence%20Based%20Environmental%20Design%20for%20Improving%20Medical.pdf. Accessed August 15, 2017.
- Becker F, Douglass S. The ecology of the patient visit: physical attractiveness, waiting times and perceived quality of care. J Ambul Care Manag. 2008;31(2):128–141.
- Becker F, Sweeney B, Parsons K. Ambulatory facility design and patients’ perceptions of healthcare quality. HERD. 2008;1(4):35–54.
- Outcome Health Website. https://www.outcomehealth.com/. Accessed August 14, 2017.
- Mazer SE. The waiting room: Where suffering begins. Healing Healthcare Systems website. http://www.healinghealth.com/waiting-room-suffering-begins/. Published November 7, 2014. Accessed August 14, 2017.
- Patient Point Programs Website. http://patientpoint.com/. Accessed August 14, 2017.
- Almquist J, Kelly C, Bromberg J, Bryant S, Christianson T, Montori V. Consultation room design and the clinical encounter: the space and interaction randomized trial. Health Environ Res Design. 2009;3(1):41–78.
- Maslow A, Mintz N. Effects of esthetic surroundings: I. Initial effects of three esthetic conditions upon perceiving “energy” and “well-being” in faces. J Psychology. 1956;41(2):247–254.
- Siegrist RB. The patient experience. In: Sanfilippo JS, Bieber E, Javich D, Siegrist R, eds. MBA for Healthcare. New York, NY: Oxford Press;2016:227–236.
- Press I. Patient satisfaction: Understanding and managing the experience of care. 2nd ed. Chicago, IL: Health Administration Press; 2005:66–78.
- Piper L, Tallman E. Hospital consumer assessment of healthcare providers and systems: An ethical leadership dilemma to satisfy patients. Health Care Manag (Frederick). 2016;35(2):151–155.
- Giordano L, Elliott M, Goldstein E, Lehrman W, Spencer P. Development, implementation and public reporting of HCAHPS survey. Med Care Res Rev. 2010;67(1):27–37.
- Jones KE. Helping the health profession help others: Applying business principles to the medical world. University of Tennessee, Knoxville Honors Thesis Projects. http://trace.tennessee.edu/cgi/viewcontent.cgi?article=1560&context=utk_chanhonoproj. Published 2002. Accessed August 14, 2017.
- Baum N. Marketing your practice: ethically, effectively and economically. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:123–154.
- Baum NH. Four pillars of a successful practice: 1. Keep your current patients happy. OBG Manag. 2013;25(3):49–56.
- Baum NH. Four pillars of a successful practice: 4. Motivate your staff. OBG Manag. 2013;25(8):29–33.
- Ulrich RS. Evidence-based environmental design for improving medical outcomes: Paper Delivered at a Conference Entitled Healing by Design: Building for Health Care in the 21st Century. Montreal: McGill University Health Centre; 2000. http://www.brikbase.org/sites/default/files/Evidence%20Based%20Environmental%20Design%20for%20Improving%20Medical.pdf. Accessed August 15, 2017.
- Becker F, Douglass S. The ecology of the patient visit: physical attractiveness, waiting times and perceived quality of care. J Ambul Care Manag. 2008;31(2):128–141.
- Becker F, Sweeney B, Parsons K. Ambulatory facility design and patients’ perceptions of healthcare quality. HERD. 2008;1(4):35–54.
- Outcome Health Website. https://www.outcomehealth.com/. Accessed August 14, 2017.
- Mazer SE. The waiting room: Where suffering begins. Healing Healthcare Systems website. http://www.healinghealth.com/waiting-room-suffering-begins/. Published November 7, 2014. Accessed August 14, 2017.
- Patient Point Programs Website. http://patientpoint.com/. Accessed August 14, 2017.
- Almquist J, Kelly C, Bromberg J, Bryant S, Christianson T, Montori V. Consultation room design and the clinical encounter: the space and interaction randomized trial. Health Environ Res Design. 2009;3(1):41–78.
- Maslow A, Mintz N. Effects of esthetic surroundings: I. Initial effects of three esthetic conditions upon perceiving “energy” and “well-being” in faces. J Psychology. 1956;41(2):247–254.
- Siegrist RB. The patient experience. In: Sanfilippo JS, Bieber E, Javich D, Siegrist R, eds. MBA for Healthcare. New York, NY: Oxford Press;2016:227–236.
- Press I. Patient satisfaction: Understanding and managing the experience of care. 2nd ed. Chicago, IL: Health Administration Press; 2005:66–78.
- Piper L, Tallman E. Hospital consumer assessment of healthcare providers and systems: An ethical leadership dilemma to satisfy patients. Health Care Manag (Frederick). 2016;35(2):151–155.
- Giordano L, Elliott M, Goldstein E, Lehrman W, Spencer P. Development, implementation and public reporting of HCAHPS survey. Med Care Res Rev. 2010;67(1):27–37.
- Jones KE. Helping the health profession help others: Applying business principles to the medical world. University of Tennessee, Knoxville Honors Thesis Projects. http://trace.tennessee.edu/cgi/viewcontent.cgi?article=1560&context=utk_chanhonoproj. Published 2002. Accessed August 14, 2017.
- Baum N. Marketing your practice: ethically, effectively and economically. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:123–154.
- Baum NH. Four pillars of a successful practice: 1. Keep your current patients happy. OBG Manag. 2013;25(3):49–56.
- Baum NH. Four pillars of a successful practice: 4. Motivate your staff. OBG Manag. 2013;25(8):29–33.
Pregnancy test missed before IUD placement? Your liability.
CASE: Gynecologist accused of placing an IUD without performing a pregnancy test
A 34-year-old woman (G4 P3013) presents to her gynecologist for planned placement of the Mirena Intrauterine System (Bayer HealthCare). She was divorced 2 months ago and is interested in birth control. She smokes 1.5 packs per day, and her history includes irregular menses, an earlier Pap smear result of atypical squamous cells of undetermined significance (ASCUS) with negative colposcopy results, polycystic ovary syndrome, obesity, migraine headaches with aura, bilateral carpel tunnel surgery, and a herniated L4.5 disc treated conservatively. She has no history of any psychiatric problems.
One week before intrauterine device (IUD) placement, she discussed the options with her gynecologist and received a Mirena patient brochure. At the office visit for IUD placement, the patient stated she had a negative home pregnancy test 1 week earlier. She did not tell the gynecologist that she had taken Plan B One-Step (levonorgestrel, 1.5 mg) emergency contraception 2 weeks prior to presenting to her gynecologist after receiving it from a Planned Parenthood office following condom breakage during coitus. IUD placement was uncomplicated.
After noting spotting several weeks later, she contacted her gynecologist’s office. Results of an office urine pregnancy test were positive; the serum human chorionic gonadotropin (hCG) level was reported at 65,000 mIU/mL.The results of a pelvic sonogram showed a 12 5/7-week intrauterine gestation. The gynecologist unsuccessfully tried to remove the IUD. Options for termination or continuation of the pregnancy were discussed. The patient felt the gynecologist strongly encouraged, “almost insisting on,” termination. Termination could not be performed locally as her state laws did not allow second trimester abortion; the gynecologist provided out-of-state clinic options.
The patient aborted the pregnancy in a neighboring state. She was opposed to the termination but decided it was not a good time for her to have a baby. She felt the staff at the facility were “cold” and had a “we got to get this done attitude.” As she left the clinic, she saw people picketing outside and found the whole process “psychologically traumatic.” When bleeding persisted, she sought care from another gynecologist. Pelvic sonography results showed retained products of conception (POC). The new gynecologist performed operative hysteroscopy to remove the POC. The patient became depressed and felt as if she was a victim of pain and suffering.
The patient’s attorney filed a medical malpractice claim against the gynecologist who inserted the IUD, accusing her of negligence for not performing a pregnancy test immediately before IUD insertion.
In a deposition, the patient stated she bought the home pregnancy test in a “dollar store” and was worried about its accuracy, but never told the gynecologist. Conception probably occurred 2 weeks prior to IUD insertion, correlating with the broken condom and taking of Plan B. She did not think the gynecologist needed to know this as it “would not have made any difference in her care.”
The gynecologist confirmed that the patient’s record included “Patient stated ‘pregnancy test negative within 1 week of IUD placement.’” The gynecologist did not feel that obtaining the date of the patient’s last menstrual period (LMP) was required since she asked if the patient had protected coitus since her LMP and the patient answered yes. The gynecologist thought that if a pregnancy were in utero, Mirena placement would prevent implantation. She believed that she had obtained proper informed consent and that the patient acknowledged receiving and reading the Mirena patient information prior to placement. The gynecologist stated she also provided other birth control options.
The patient’s expert witness testified that the gynecologist fell below the standard of care by not obtaining a pregnancy test prior to IUD insertion.
The gynecologist’s expert witness argued that the patient told the gynecologist that she did not have unprotected coitus. The patient herself withheld information from the gynecologist that she had taken Plan B due to condom breakage. The physician’s attorney also noted that the pelvic exam at time of IUD placement was normal.
What’s the verdict?
The patient has a fairly good case. The gynecologist may not have been sufficiently careful, given all of the facts in this case, to ensure that the patient was not pregnant. An expert is testifying that this fell below the acceptable level of care in the profession. At the same time, the failure of the patient to reveal some information may result in reduced damages through “comparative negligence.” Because there will be several questions of fact for a jury to decide, as well as some emotional elements in this case, the outcome of a trial is uncertain. This suggests that a negotiated settlement before trial should be considered.
Read about medical considerations of a pregnancy with an IUD.
Medical considerations
First, some background information on Mirena.
Indications for Mirena
Here are indications for Mirena1:
- intrauterine contraception for up to 5 years
- treatment of heavy menstrual bleeding for women who choose to use intrauterine contraception as their method of contraception.
Prior to insertion, the following are recommended2:
- a complete medical and social history should be obtained to determine conditions that might influence the selection of a levonorgestrel-releasing intrauterine system (LNG IUS) for contraception
- if indicated, perform a physical examination, and appropriate tests for any forms of genital or other sexually transmitted infections
- there is no requirement for prepregnancy test.
Contraindications for Mirena
Contraindications for Mirena include2:
- pregnancy or suspicion of pregnancy; cannot be used for postcoital contraception
- congenital or acquired uterine anomaly including fibroids if they distort the uterine cavity
- acute pelvic inflammatory disease or a history of pelvic inflammatory disease unless there has been a subsequent intrauterine pregnancy
- postpartum endometritis or infected abortion in the past 3 months
- known or suspected uterine or cervical neoplasia
- known or suspected breast cancer or other progestin-sensitive cancer, now or in the past
- uterine bleeding of unknown etiology
- untreated acute cervicitis or vaginitis, including bacterial vaginosis or other lower genital tract infections until infection is controlled
- acute liver disease or liver tumor (benign or malignant)
- conditions associated with increased susceptibility to pelvic infections
- a previously inserted IUD that has not been removed
- hypersensitivity to any component of this product.
Is Mirena a postcoital contraceptive?
The American College of Obstetricians and Gynecologists (ACOG) bulletin on long-acting reversible contraception states “the levonorgestrel intrauterine system has not been studied for emergency contraception.”3 Ongoing studies are comparing the levonor‑gestrel IUD to the copper IUD for emergency contraception.4
Related Article:
Webcast: Emergency contraception: How to choose the right one for your patient
Accuracy of home pregnancy tests
Although the first home pregnancy test was introduced in 1976,5 there are now several home pregnancy tests available over the counter, most designed to detect urinary levels of hCG at ≥25 mIU/mL. The tests identify hCG, hyperglycosylated hCG, and free Betasubunit hCG in urine. When Cole and colleagues evaluated the validity of urinary tests including assessment of 18 brands, results noted that sensitivity of 12.4 mIU/mL of hCG detected 95% of pregnancies at time of missed menses.6 Some brands required 100 mIU/mL levels of hCG for positive results. The authors concluded “the utility of home pregnancy tests is questioned.”6 For urinary levels of hCG, see TABLE.
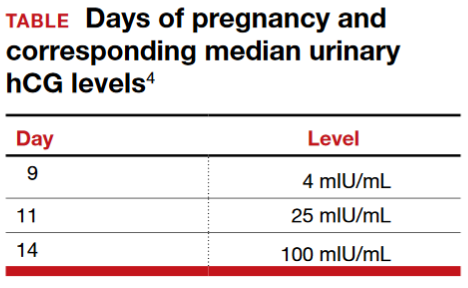
Pregnancy with an IUD
The gynecologist’s concern about pregnancy when an IUD is inserted was valid.
With regard to pregnancy with Mirena in place, the full prescribing information states2:
Intrauterine Pregnancy: If pregnancy occurs while using Mirena, remove Mirena because leaving it in place may increase the risk of spontaneous abortion and preterm labor. Removal of Mirena or probing of the uterus may also result in spontaneous abortion. In the event of an intrauterine pregnancy with Mirena, consider the following:
Septic abortion
In patients becoming pregnant with an IUD in place, septic abortion - with septicemia, septic shock, and death may occur.
Continuation of pregnancy
If a woman becomes pregnant with Mirena in place and if Mirena cannot be removed or the woman chooses not to have it removed, warn her that failure to remove Mirena increases the risk of miscarriage, sepsis, premature labor and premature delivery. Follow her pregnancy closely and advise her to report immediately any symptom that suggests complications of the pregnancy.
Concern for microbial invasion of the amniotic cavity must be considered. Kim and colleagues addressed pregnancy prognosis with an IUD in situ in a retrospective study of 12,297 pregnancies; 196 had an IUD with singleton gestation.7 The study revealed a higher incidence of histologic chorioamnionitis and/or funisitis when compared with those without an IUD (54.2% vs 14.7%, respectively; P<.001). The authors concluded that pregnant women with an IUD in utero are at very high risk for adverse pregnancy outcomes. Brahmi and colleagues8 reported similar risks with higher incidence of spontaneous abortion, preterm delivery, and septic abortion.
Related Article:
Overcoming LARC complications: 7 case challenges
Efficacy and safety concerns with emergency contraception
The efficacy and safety of emergency contraception using levonorgestrel oral tablets (Plan B One-Step; Duramed Pharmaceuticals) is another concern. Plan B One-Step should be taken orally as soon as possible within 72 hours after unprotected intercourse or a known or suspected contraceptive failure. Efficacy is better if Plan B is taken as soon as possible after unprotected intercourse. There are 2 dosages: 1 tablet of levonorgestrel 1.5 mg or 2 tablets of levonorgestrel 0.75 mg. The second 0.75-mg tablet should be taken 12 hours after the first dose.9
Plan B can be used at any time during the menstrual cycle. In a series of 2,445 women aged 15 to 48 years who took levonorgestrel tablets for emergency contraception (Phase IV clinical trial), 5 pregnancies occurred (0.2%).10
ACOG advises that emergency contraception using a pill or the copper IUD should be initiated as soon as possible (up to 5 days) after unprotected coitus or inadequately protected coitus.9
Retained products of contraception
ACOG Practice Bulletin No. 135 on complications associated with second trimesterabortion discusses retained POC.11 The approach to second trimester abortion includes dilation and evacuation (D&E) as well as medical therapy with mifepristone and misoprostol. D&E, a safe and effective approach with advantages over medical abortion, is associated with fewer complications (up to 4%) versus medical abortion (29%); the primary complication is retained POC (placenta).11
Read about the legal considerations of this case.
Legal considerations
The malpractice lawsuit filed in this case claims that the gynecologist failed to exercise the level of care of a reasonably prudent practitioner under the circumstances and was therefore negligent or in breach of a duty to the patient.
First, a lawyer would look for a medical error that was related to some harm. Keep in mind that not all medical errors are negligent or subject to liability. Many medical errors occur even though the physician has exercised all reasonable care and engaged in sound practice, given today’s medical knowledge and facilities. When harm is caused through medical error that was careless or otherwise does not meet the standard of care, financial recovery is possible for the patient through a malpractice claim.12
In this case, the expert witnesses’ statements focus on the issue of conducting a pregnancy test prior to IUD insertion. The patient’s expert testified that failure to perform a pregnancy test was below an acceptable standard of care. That opinion may have been based on the typical practice of gynecologists, widely accepted medical text books, and formal practice standards of professional organizations.13
Cost-benefit analysis. Additional support for the claim that not performing the pregnancy test is negligent comes from applying a cost-benefit analysis. In this analysis, the risks and costs of performing a pregnancy test are compared with the benefits of doing the test.
In this case, the cost of conducting the pregnancy test is very low: essentially risk-freeand relatively inexpensive. On the other hand, the harm that could be avoided would be significant. Kim and colleagues suggest that pregnant women with an IUD in utero are at very high risk for adverse pregnancy outcomes.7 Given that women receiving IUDs are candidates for pregnancy (and perhaps do not know they are pregnant), a simple, risk-free pregnancy test would seem to be an efficient way to avoid a nontrivial harm.14
Did she have unprotected sex? The gynecologist’s expert notes that the patient told the gynecologist that she did not have unprotected coitus. Furthermore, the patient withheld from the gynecologist the information that she had taken Plan B because of a broken condom. Is this a defense against the malpractice claim? The answer is “possibly no,” or “possibly somewhat.”
As for unprotected coitus, the patient could easily have misunderstood the question. Technically, the answer “no” was correct. She had not had unprotected sex—it is just that the protection (condom) failed. It does not appear from the facts that she disclosed or was asked about Plan B or other information related to possible failed contraception. As to whether the patient’s failure to provide that information could be a defense for the physician, the best answer is “possibly” and “somewhat.” (See below.)15
Withholding information. Patients, of course, have a responsibility to inform their physicians of information they know is relevant. Many patients, however, will not know what is relevant (or why), or will not be fully disclosing.
Professionals cannot ignore the fact that their patients and clients are often confused, do not understand what is important and relevant, and cannot always be relied upon. For that very reason, professionals generally are obliged to start with the proposition that they may not have all of the relevant information. In this case, this lack of information makes the cost-calculation of performing a pregnancy test that much more important. The risk of not knowing whether a patient is pregnant includes the fact that many patients just will not know or cannot say with assurance.16
A “somewhat” defense and comparative negligence
Earlier we referred to a “somewhat” defense. Almost all states now have some form of “comparative negligence,” meaning that the patient’s recovery is reduced by the proportion of the blame (negligence) that is attributed to the patient. The most common form of comparative negligence works this way: If there are damages of $100,000, and the jury finds that the fault is 20% the patient’s and 80% the physician’s, the patient would receive $80,000 recovery. (In the past, the concept of “contributory negligence” could result in the plaintiff being precluded from any recovery if the plaintiff was partially negligent—those days are mostly gone.)
Related Article:
Informed consent: The more you know, the more you and your patient are protected
Statement of risks, informed consent, and liability
The gynecologist must provide an adequate description of the IUD risks. The case facts indicate that appropriate risks were discussed and literature provided, so it appears there was probably appropriate informed consent in this case. If not true, this would provide another basis for recovery.
Two other aspects of this case could be the basis for liability. We can assume that the attempted removal of the IUD was performed competently.16 In addition, if the IUD was defective in terms of design, manufacture, or warnings, the manufacturer of the device could be subject to liability.17
Final verdict: Out of court settlement
Why would the gynecologist and the insurance company settle this case? After all, they have some arguments on their side, and physicians win the majority of malpractice cases that go to trial.18 On the other hand, the patient’s expert witness’ testimony and the cost-benefit analysis of the pregnancy test are strong, contrary claims.
Cases are settled for a variety of reasons. Litigation is inherently risky. In this case, we assume that the court denied a motion to dismiss the case before trial because there is a legitimate question of fact concerning what a reasonably prudent gynecologist would have done under the circumstances. That means a jury would probably decide the issue of medical judgment, which is generally disconcerting. Furthermore, the comparative negligence defense that the patient did not tell the gynecologist about the failed condom/Plan B would most likely reduce the amount of damages, but not eliminate liability. The questions regarding the pressure to terminate a second trimester pregnancy might well complicate a jury’s view.
Other considerations include the high costs in time, money, uncertainty, and disruption associated with litigation. The settlement amount was not stated, but the process of negotiating a settlement would allow factoring in the comparative negligence aspect of the case. It would be reasonable for this case to settle before trial.
Should the physician have apologized before trial? The gynecologist could have sent a statement of regret or apology to the patient before a lawsuit was filed. Most states now have statutes that preclude such statements of regret or apology from being used against the physician. Many experts now favor apology statements as a way to reduce the risk of malpractice suits being filed.19
Related Article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
Defensive medicine. There has been much discussion of “defensive medicine” in recent years.20 It is appropriately criticized when additional testing is solely used to protect the physician from liability. However, much of defensive medicine is not only to protect the physician but also to protect the patient from potential physical and mental harm. In this case, it would have been “careful medicine” in addition to “defensive medicine.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Heikinheimo O, Gemell-Danielsson K. Emerging indications for the levonorgestrel-releasing intrauterine system. ACTA Obstet Gynecol Scand. 2012;91(1):3–9.
- Mirena [prescribing information]. Whippany, NJ: Bayer HealthCare Pharmaceuticals Inc; 2000.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol. 2011;118(1):184–196.
- Rapid EC–Random clinical trial assessing pregnancy with intrauterine devices for emergency contraception. Clinical Trials Identifier: NCT02175030. https://www.clinicaltrials.gov/ct2/show/NCT02175030?term=NCT02175030&rank=1. Updated May 1, 2017. Accessed May 11, 2017.
- Gnoth C, Johnson S. Strips of hope: Accuracy of home pregnancy tests and new developments. Gerburtshilfe Frauenheilkd. 2014;74(7):661–669.
- Cole LA, Khanlian SA, Sutton JM, Davies S, Rayburn WF. Accuracy of home pregnancy tests at the time of missed menses. Am J Obstet Gynecol. 2004;190(1):100–105.
- Kim S, Romero R, Kusanovic J, et al. The prognosis of pregnancy conceived despite the presence of an intrauterine device (IUD). J Perinatal Med. 2010;38(1):45–53.
- Brahmi D, Steenland M, Renner R, Gaffield M, Curtis K. Pregnancy outcomes with an IUD in situ: a systematic review. Contraception. 2012;85(2):131–139.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 152: Emergency contraception. Obstet Gynecol. 2015;126(3):685–686.
- Chen Q, Xiang W, Zhang D, et al. Efficacy and safety of a levonorgestrel enteric-coated tablet as an over-the-counter drug for emergency contraception: a Phase IV clinical trial. Hum Reprod. 2011;26(9):2316–2321.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 135: Second-trimester abortion. Obstet Gynecol. 2013;121(6):1395–1406.
- White A, Pichert J, Bledsoe S, Irwin C, Entman S. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt1):1031–1038.
- Mehlman M. Professional power and the standard of care in medicine. Case Western Reserve University Scholarly Commons. 2012: Paper 574. http://scholarlycommons.law.case.edu/cgi/viewcontent.cgi?article=1576&context=faculty_publications. Accessed May 11, 2017.
- Klein D, Arnold J, Reese E. Provision of contraception: key recommendations from the CDC. Am Fam Physician. 2015;91(9);625–633.
- Reyes J, Reyes R. The effects of malpractice liability on obstetrics and gynecology: taking the measure of a crisis. N England Law Rev. 2012;47;315–348. https://www.scribd.com/document/136514285/Reyes-Reyes-The-Effect-of-Malpractice-Liability-on-Obstetrics-and -Gynecology#fullscreen&from_embed. Accessed May 11, 2017.
- Peckham C. Medscape Malpractice Report 2015: Why Ob/Gyns get sued. http://www.medscape.com/features/slideshow/malpractice-report-2015/obgyn#page=1. Published January 22, 2016. Accessed May 11. 2017.
- Rheingold P, Paris D. Contraceptives. In: Vargo JJ, ed. Products Liability Practice Guide New York, New York: Matthew Bender & Company; 2017;C:62.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
- Helmreich JS. Does sorry incriminate? Evidence, harm and the protection of apology. Cornell J Law Public Policy. 2012;21(3);567–609. http://scholarship.law.cornell.edu/cgi/viewcontent.cgi?article=1363&context=cjlpp.
- Baicker K, Wright B, Olson N. Reevaluating reports of defensive medicine. J Health Polit Policy Law. 2015;40(6);1157–1177.
CASE: Gynecologist accused of placing an IUD without performing a pregnancy test
A 34-year-old woman (G4 P3013) presents to her gynecologist for planned placement of the Mirena Intrauterine System (Bayer HealthCare). She was divorced 2 months ago and is interested in birth control. She smokes 1.5 packs per day, and her history includes irregular menses, an earlier Pap smear result of atypical squamous cells of undetermined significance (ASCUS) with negative colposcopy results, polycystic ovary syndrome, obesity, migraine headaches with aura, bilateral carpel tunnel surgery, and a herniated L4.5 disc treated conservatively. She has no history of any psychiatric problems.
One week before intrauterine device (IUD) placement, she discussed the options with her gynecologist and received a Mirena patient brochure. At the office visit for IUD placement, the patient stated she had a negative home pregnancy test 1 week earlier. She did not tell the gynecologist that she had taken Plan B One-Step (levonorgestrel, 1.5 mg) emergency contraception 2 weeks prior to presenting to her gynecologist after receiving it from a Planned Parenthood office following condom breakage during coitus. IUD placement was uncomplicated.
After noting spotting several weeks later, she contacted her gynecologist’s office. Results of an office urine pregnancy test were positive; the serum human chorionic gonadotropin (hCG) level was reported at 65,000 mIU/mL.The results of a pelvic sonogram showed a 12 5/7-week intrauterine gestation. The gynecologist unsuccessfully tried to remove the IUD. Options for termination or continuation of the pregnancy were discussed. The patient felt the gynecologist strongly encouraged, “almost insisting on,” termination. Termination could not be performed locally as her state laws did not allow second trimester abortion; the gynecologist provided out-of-state clinic options.
The patient aborted the pregnancy in a neighboring state. She was opposed to the termination but decided it was not a good time for her to have a baby. She felt the staff at the facility were “cold” and had a “we got to get this done attitude.” As she left the clinic, she saw people picketing outside and found the whole process “psychologically traumatic.” When bleeding persisted, she sought care from another gynecologist. Pelvic sonography results showed retained products of conception (POC). The new gynecologist performed operative hysteroscopy to remove the POC. The patient became depressed and felt as if she was a victim of pain and suffering.
The patient’s attorney filed a medical malpractice claim against the gynecologist who inserted the IUD, accusing her of negligence for not performing a pregnancy test immediately before IUD insertion.
In a deposition, the patient stated she bought the home pregnancy test in a “dollar store” and was worried about its accuracy, but never told the gynecologist. Conception probably occurred 2 weeks prior to IUD insertion, correlating with the broken condom and taking of Plan B. She did not think the gynecologist needed to know this as it “would not have made any difference in her care.”
The gynecologist confirmed that the patient’s record included “Patient stated ‘pregnancy test negative within 1 week of IUD placement.’” The gynecologist did not feel that obtaining the date of the patient’s last menstrual period (LMP) was required since she asked if the patient had protected coitus since her LMP and the patient answered yes. The gynecologist thought that if a pregnancy were in utero, Mirena placement would prevent implantation. She believed that she had obtained proper informed consent and that the patient acknowledged receiving and reading the Mirena patient information prior to placement. The gynecologist stated she also provided other birth control options.
The patient’s expert witness testified that the gynecologist fell below the standard of care by not obtaining a pregnancy test prior to IUD insertion.
The gynecologist’s expert witness argued that the patient told the gynecologist that she did not have unprotected coitus. The patient herself withheld information from the gynecologist that she had taken Plan B due to condom breakage. The physician’s attorney also noted that the pelvic exam at time of IUD placement was normal.
What’s the verdict?
The patient has a fairly good case. The gynecologist may not have been sufficiently careful, given all of the facts in this case, to ensure that the patient was not pregnant. An expert is testifying that this fell below the acceptable level of care in the profession. At the same time, the failure of the patient to reveal some information may result in reduced damages through “comparative negligence.” Because there will be several questions of fact for a jury to decide, as well as some emotional elements in this case, the outcome of a trial is uncertain. This suggests that a negotiated settlement before trial should be considered.
Read about medical considerations of a pregnancy with an IUD.
Medical considerations
First, some background information on Mirena.
Indications for Mirena
Here are indications for Mirena1:
- intrauterine contraception for up to 5 years
- treatment of heavy menstrual bleeding for women who choose to use intrauterine contraception as their method of contraception.
Prior to insertion, the following are recommended2:
- a complete medical and social history should be obtained to determine conditions that might influence the selection of a levonorgestrel-releasing intrauterine system (LNG IUS) for contraception
- if indicated, perform a physical examination, and appropriate tests for any forms of genital or other sexually transmitted infections
- there is no requirement for prepregnancy test.
Contraindications for Mirena
Contraindications for Mirena include2:
- pregnancy or suspicion of pregnancy; cannot be used for postcoital contraception
- congenital or acquired uterine anomaly including fibroids if they distort the uterine cavity
- acute pelvic inflammatory disease or a history of pelvic inflammatory disease unless there has been a subsequent intrauterine pregnancy
- postpartum endometritis or infected abortion in the past 3 months
- known or suspected uterine or cervical neoplasia
- known or suspected breast cancer or other progestin-sensitive cancer, now or in the past
- uterine bleeding of unknown etiology
- untreated acute cervicitis or vaginitis, including bacterial vaginosis or other lower genital tract infections until infection is controlled
- acute liver disease or liver tumor (benign or malignant)
- conditions associated with increased susceptibility to pelvic infections
- a previously inserted IUD that has not been removed
- hypersensitivity to any component of this product.
Is Mirena a postcoital contraceptive?
The American College of Obstetricians and Gynecologists (ACOG) bulletin on long-acting reversible contraception states “the levonorgestrel intrauterine system has not been studied for emergency contraception.”3 Ongoing studies are comparing the levonor‑gestrel IUD to the copper IUD for emergency contraception.4
Related Article:
Webcast: Emergency contraception: How to choose the right one for your patient
Accuracy of home pregnancy tests
Although the first home pregnancy test was introduced in 1976,5 there are now several home pregnancy tests available over the counter, most designed to detect urinary levels of hCG at ≥25 mIU/mL. The tests identify hCG, hyperglycosylated hCG, and free Betasubunit hCG in urine. When Cole and colleagues evaluated the validity of urinary tests including assessment of 18 brands, results noted that sensitivity of 12.4 mIU/mL of hCG detected 95% of pregnancies at time of missed menses.6 Some brands required 100 mIU/mL levels of hCG for positive results. The authors concluded “the utility of home pregnancy tests is questioned.”6 For urinary levels of hCG, see TABLE.
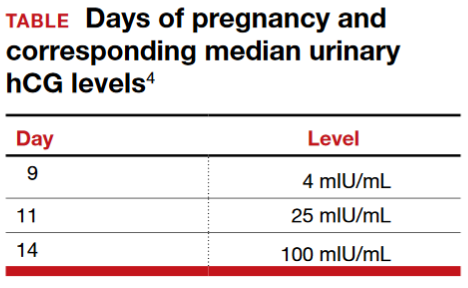
Pregnancy with an IUD
The gynecologist’s concern about pregnancy when an IUD is inserted was valid.
With regard to pregnancy with Mirena in place, the full prescribing information states2:
Intrauterine Pregnancy: If pregnancy occurs while using Mirena, remove Mirena because leaving it in place may increase the risk of spontaneous abortion and preterm labor. Removal of Mirena or probing of the uterus may also result in spontaneous abortion. In the event of an intrauterine pregnancy with Mirena, consider the following:
Septic abortion
In patients becoming pregnant with an IUD in place, septic abortion - with septicemia, septic shock, and death may occur.
Continuation of pregnancy
If a woman becomes pregnant with Mirena in place and if Mirena cannot be removed or the woman chooses not to have it removed, warn her that failure to remove Mirena increases the risk of miscarriage, sepsis, premature labor and premature delivery. Follow her pregnancy closely and advise her to report immediately any symptom that suggests complications of the pregnancy.
Concern for microbial invasion of the amniotic cavity must be considered. Kim and colleagues addressed pregnancy prognosis with an IUD in situ in a retrospective study of 12,297 pregnancies; 196 had an IUD with singleton gestation.7 The study revealed a higher incidence of histologic chorioamnionitis and/or funisitis when compared with those without an IUD (54.2% vs 14.7%, respectively; P<.001). The authors concluded that pregnant women with an IUD in utero are at very high risk for adverse pregnancy outcomes. Brahmi and colleagues8 reported similar risks with higher incidence of spontaneous abortion, preterm delivery, and septic abortion.
Related Article:
Overcoming LARC complications: 7 case challenges
Efficacy and safety concerns with emergency contraception
The efficacy and safety of emergency contraception using levonorgestrel oral tablets (Plan B One-Step; Duramed Pharmaceuticals) is another concern. Plan B One-Step should be taken orally as soon as possible within 72 hours after unprotected intercourse or a known or suspected contraceptive failure. Efficacy is better if Plan B is taken as soon as possible after unprotected intercourse. There are 2 dosages: 1 tablet of levonorgestrel 1.5 mg or 2 tablets of levonorgestrel 0.75 mg. The second 0.75-mg tablet should be taken 12 hours after the first dose.9
Plan B can be used at any time during the menstrual cycle. In a series of 2,445 women aged 15 to 48 years who took levonorgestrel tablets for emergency contraception (Phase IV clinical trial), 5 pregnancies occurred (0.2%).10
ACOG advises that emergency contraception using a pill or the copper IUD should be initiated as soon as possible (up to 5 days) after unprotected coitus or inadequately protected coitus.9
Retained products of contraception
ACOG Practice Bulletin No. 135 on complications associated with second trimesterabortion discusses retained POC.11 The approach to second trimester abortion includes dilation and evacuation (D&E) as well as medical therapy with mifepristone and misoprostol. D&E, a safe and effective approach with advantages over medical abortion, is associated with fewer complications (up to 4%) versus medical abortion (29%); the primary complication is retained POC (placenta).11
Read about the legal considerations of this case.
Legal considerations
The malpractice lawsuit filed in this case claims that the gynecologist failed to exercise the level of care of a reasonably prudent practitioner under the circumstances and was therefore negligent or in breach of a duty to the patient.
First, a lawyer would look for a medical error that was related to some harm. Keep in mind that not all medical errors are negligent or subject to liability. Many medical errors occur even though the physician has exercised all reasonable care and engaged in sound practice, given today’s medical knowledge and facilities. When harm is caused through medical error that was careless or otherwise does not meet the standard of care, financial recovery is possible for the patient through a malpractice claim.12
In this case, the expert witnesses’ statements focus on the issue of conducting a pregnancy test prior to IUD insertion. The patient’s expert testified that failure to perform a pregnancy test was below an acceptable standard of care. That opinion may have been based on the typical practice of gynecologists, widely accepted medical text books, and formal practice standards of professional organizations.13
Cost-benefit analysis. Additional support for the claim that not performing the pregnancy test is negligent comes from applying a cost-benefit analysis. In this analysis, the risks and costs of performing a pregnancy test are compared with the benefits of doing the test.
In this case, the cost of conducting the pregnancy test is very low: essentially risk-freeand relatively inexpensive. On the other hand, the harm that could be avoided would be significant. Kim and colleagues suggest that pregnant women with an IUD in utero are at very high risk for adverse pregnancy outcomes.7 Given that women receiving IUDs are candidates for pregnancy (and perhaps do not know they are pregnant), a simple, risk-free pregnancy test would seem to be an efficient way to avoid a nontrivial harm.14
Did she have unprotected sex? The gynecologist’s expert notes that the patient told the gynecologist that she did not have unprotected coitus. Furthermore, the patient withheld from the gynecologist the information that she had taken Plan B because of a broken condom. Is this a defense against the malpractice claim? The answer is “possibly no,” or “possibly somewhat.”
As for unprotected coitus, the patient could easily have misunderstood the question. Technically, the answer “no” was correct. She had not had unprotected sex—it is just that the protection (condom) failed. It does not appear from the facts that she disclosed or was asked about Plan B or other information related to possible failed contraception. As to whether the patient’s failure to provide that information could be a defense for the physician, the best answer is “possibly” and “somewhat.” (See below.)15
Withholding information. Patients, of course, have a responsibility to inform their physicians of information they know is relevant. Many patients, however, will not know what is relevant (or why), or will not be fully disclosing.
Professionals cannot ignore the fact that their patients and clients are often confused, do not understand what is important and relevant, and cannot always be relied upon. For that very reason, professionals generally are obliged to start with the proposition that they may not have all of the relevant information. In this case, this lack of information makes the cost-calculation of performing a pregnancy test that much more important. The risk of not knowing whether a patient is pregnant includes the fact that many patients just will not know or cannot say with assurance.16
A “somewhat” defense and comparative negligence
Earlier we referred to a “somewhat” defense. Almost all states now have some form of “comparative negligence,” meaning that the patient’s recovery is reduced by the proportion of the blame (negligence) that is attributed to the patient. The most common form of comparative negligence works this way: If there are damages of $100,000, and the jury finds that the fault is 20% the patient’s and 80% the physician’s, the patient would receive $80,000 recovery. (In the past, the concept of “contributory negligence” could result in the plaintiff being precluded from any recovery if the plaintiff was partially negligent—those days are mostly gone.)
Related Article:
Informed consent: The more you know, the more you and your patient are protected
Statement of risks, informed consent, and liability
The gynecologist must provide an adequate description of the IUD risks. The case facts indicate that appropriate risks were discussed and literature provided, so it appears there was probably appropriate informed consent in this case. If not true, this would provide another basis for recovery.
Two other aspects of this case could be the basis for liability. We can assume that the attempted removal of the IUD was performed competently.16 In addition, if the IUD was defective in terms of design, manufacture, or warnings, the manufacturer of the device could be subject to liability.17
Final verdict: Out of court settlement
Why would the gynecologist and the insurance company settle this case? After all, they have some arguments on their side, and physicians win the majority of malpractice cases that go to trial.18 On the other hand, the patient’s expert witness’ testimony and the cost-benefit analysis of the pregnancy test are strong, contrary claims.
Cases are settled for a variety of reasons. Litigation is inherently risky. In this case, we assume that the court denied a motion to dismiss the case before trial because there is a legitimate question of fact concerning what a reasonably prudent gynecologist would have done under the circumstances. That means a jury would probably decide the issue of medical judgment, which is generally disconcerting. Furthermore, the comparative negligence defense that the patient did not tell the gynecologist about the failed condom/Plan B would most likely reduce the amount of damages, but not eliminate liability. The questions regarding the pressure to terminate a second trimester pregnancy might well complicate a jury’s view.
Other considerations include the high costs in time, money, uncertainty, and disruption associated with litigation. The settlement amount was not stated, but the process of negotiating a settlement would allow factoring in the comparative negligence aspect of the case. It would be reasonable for this case to settle before trial.
Should the physician have apologized before trial? The gynecologist could have sent a statement of regret or apology to the patient before a lawsuit was filed. Most states now have statutes that preclude such statements of regret or apology from being used against the physician. Many experts now favor apology statements as a way to reduce the risk of malpractice suits being filed.19
Related Article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
Defensive medicine. There has been much discussion of “defensive medicine” in recent years.20 It is appropriately criticized when additional testing is solely used to protect the physician from liability. However, much of defensive medicine is not only to protect the physician but also to protect the patient from potential physical and mental harm. In this case, it would have been “careful medicine” in addition to “defensive medicine.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE: Gynecologist accused of placing an IUD without performing a pregnancy test
A 34-year-old woman (G4 P3013) presents to her gynecologist for planned placement of the Mirena Intrauterine System (Bayer HealthCare). She was divorced 2 months ago and is interested in birth control. She smokes 1.5 packs per day, and her history includes irregular menses, an earlier Pap smear result of atypical squamous cells of undetermined significance (ASCUS) with negative colposcopy results, polycystic ovary syndrome, obesity, migraine headaches with aura, bilateral carpel tunnel surgery, and a herniated L4.5 disc treated conservatively. She has no history of any psychiatric problems.
One week before intrauterine device (IUD) placement, she discussed the options with her gynecologist and received a Mirena patient brochure. At the office visit for IUD placement, the patient stated she had a negative home pregnancy test 1 week earlier. She did not tell the gynecologist that she had taken Plan B One-Step (levonorgestrel, 1.5 mg) emergency contraception 2 weeks prior to presenting to her gynecologist after receiving it from a Planned Parenthood office following condom breakage during coitus. IUD placement was uncomplicated.
After noting spotting several weeks later, she contacted her gynecologist’s office. Results of an office urine pregnancy test were positive; the serum human chorionic gonadotropin (hCG) level was reported at 65,000 mIU/mL.The results of a pelvic sonogram showed a 12 5/7-week intrauterine gestation. The gynecologist unsuccessfully tried to remove the IUD. Options for termination or continuation of the pregnancy were discussed. The patient felt the gynecologist strongly encouraged, “almost insisting on,” termination. Termination could not be performed locally as her state laws did not allow second trimester abortion; the gynecologist provided out-of-state clinic options.
The patient aborted the pregnancy in a neighboring state. She was opposed to the termination but decided it was not a good time for her to have a baby. She felt the staff at the facility were “cold” and had a “we got to get this done attitude.” As she left the clinic, she saw people picketing outside and found the whole process “psychologically traumatic.” When bleeding persisted, she sought care from another gynecologist. Pelvic sonography results showed retained products of conception (POC). The new gynecologist performed operative hysteroscopy to remove the POC. The patient became depressed and felt as if she was a victim of pain and suffering.
The patient’s attorney filed a medical malpractice claim against the gynecologist who inserted the IUD, accusing her of negligence for not performing a pregnancy test immediately before IUD insertion.
In a deposition, the patient stated she bought the home pregnancy test in a “dollar store” and was worried about its accuracy, but never told the gynecologist. Conception probably occurred 2 weeks prior to IUD insertion, correlating with the broken condom and taking of Plan B. She did not think the gynecologist needed to know this as it “would not have made any difference in her care.”
The gynecologist confirmed that the patient’s record included “Patient stated ‘pregnancy test negative within 1 week of IUD placement.’” The gynecologist did not feel that obtaining the date of the patient’s last menstrual period (LMP) was required since she asked if the patient had protected coitus since her LMP and the patient answered yes. The gynecologist thought that if a pregnancy were in utero, Mirena placement would prevent implantation. She believed that she had obtained proper informed consent and that the patient acknowledged receiving and reading the Mirena patient information prior to placement. The gynecologist stated she also provided other birth control options.
The patient’s expert witness testified that the gynecologist fell below the standard of care by not obtaining a pregnancy test prior to IUD insertion.
The gynecologist’s expert witness argued that the patient told the gynecologist that she did not have unprotected coitus. The patient herself withheld information from the gynecologist that she had taken Plan B due to condom breakage. The physician’s attorney also noted that the pelvic exam at time of IUD placement was normal.
What’s the verdict?
The patient has a fairly good case. The gynecologist may not have been sufficiently careful, given all of the facts in this case, to ensure that the patient was not pregnant. An expert is testifying that this fell below the acceptable level of care in the profession. At the same time, the failure of the patient to reveal some information may result in reduced damages through “comparative negligence.” Because there will be several questions of fact for a jury to decide, as well as some emotional elements in this case, the outcome of a trial is uncertain. This suggests that a negotiated settlement before trial should be considered.
Read about medical considerations of a pregnancy with an IUD.
Medical considerations
First, some background information on Mirena.
Indications for Mirena
Here are indications for Mirena1:
- intrauterine contraception for up to 5 years
- treatment of heavy menstrual bleeding for women who choose to use intrauterine contraception as their method of contraception.
Prior to insertion, the following are recommended2:
- a complete medical and social history should be obtained to determine conditions that might influence the selection of a levonorgestrel-releasing intrauterine system (LNG IUS) for contraception
- if indicated, perform a physical examination, and appropriate tests for any forms of genital or other sexually transmitted infections
- there is no requirement for prepregnancy test.
Contraindications for Mirena
Contraindications for Mirena include2:
- pregnancy or suspicion of pregnancy; cannot be used for postcoital contraception
- congenital or acquired uterine anomaly including fibroids if they distort the uterine cavity
- acute pelvic inflammatory disease or a history of pelvic inflammatory disease unless there has been a subsequent intrauterine pregnancy
- postpartum endometritis or infected abortion in the past 3 months
- known or suspected uterine or cervical neoplasia
- known or suspected breast cancer or other progestin-sensitive cancer, now or in the past
- uterine bleeding of unknown etiology
- untreated acute cervicitis or vaginitis, including bacterial vaginosis or other lower genital tract infections until infection is controlled
- acute liver disease or liver tumor (benign or malignant)
- conditions associated with increased susceptibility to pelvic infections
- a previously inserted IUD that has not been removed
- hypersensitivity to any component of this product.
Is Mirena a postcoital contraceptive?
The American College of Obstetricians and Gynecologists (ACOG) bulletin on long-acting reversible contraception states “the levonorgestrel intrauterine system has not been studied for emergency contraception.”3 Ongoing studies are comparing the levonor‑gestrel IUD to the copper IUD for emergency contraception.4
Related Article:
Webcast: Emergency contraception: How to choose the right one for your patient
Accuracy of home pregnancy tests
Although the first home pregnancy test was introduced in 1976,5 there are now several home pregnancy tests available over the counter, most designed to detect urinary levels of hCG at ≥25 mIU/mL. The tests identify hCG, hyperglycosylated hCG, and free Betasubunit hCG in urine. When Cole and colleagues evaluated the validity of urinary tests including assessment of 18 brands, results noted that sensitivity of 12.4 mIU/mL of hCG detected 95% of pregnancies at time of missed menses.6 Some brands required 100 mIU/mL levels of hCG for positive results. The authors concluded “the utility of home pregnancy tests is questioned.”6 For urinary levels of hCG, see TABLE.
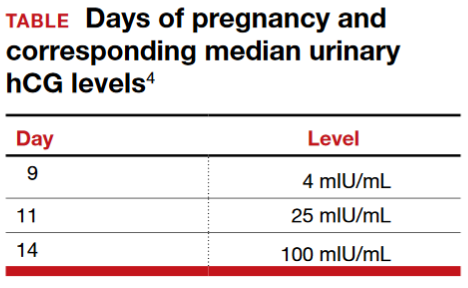
Pregnancy with an IUD
The gynecologist’s concern about pregnancy when an IUD is inserted was valid.
With regard to pregnancy with Mirena in place, the full prescribing information states2:
Intrauterine Pregnancy: If pregnancy occurs while using Mirena, remove Mirena because leaving it in place may increase the risk of spontaneous abortion and preterm labor. Removal of Mirena or probing of the uterus may also result in spontaneous abortion. In the event of an intrauterine pregnancy with Mirena, consider the following:
Septic abortion
In patients becoming pregnant with an IUD in place, septic abortion - with septicemia, septic shock, and death may occur.
Continuation of pregnancy
If a woman becomes pregnant with Mirena in place and if Mirena cannot be removed or the woman chooses not to have it removed, warn her that failure to remove Mirena increases the risk of miscarriage, sepsis, premature labor and premature delivery. Follow her pregnancy closely and advise her to report immediately any symptom that suggests complications of the pregnancy.
Concern for microbial invasion of the amniotic cavity must be considered. Kim and colleagues addressed pregnancy prognosis with an IUD in situ in a retrospective study of 12,297 pregnancies; 196 had an IUD with singleton gestation.7 The study revealed a higher incidence of histologic chorioamnionitis and/or funisitis when compared with those without an IUD (54.2% vs 14.7%, respectively; P<.001). The authors concluded that pregnant women with an IUD in utero are at very high risk for adverse pregnancy outcomes. Brahmi and colleagues8 reported similar risks with higher incidence of spontaneous abortion, preterm delivery, and septic abortion.
Related Article:
Overcoming LARC complications: 7 case challenges
Efficacy and safety concerns with emergency contraception
The efficacy and safety of emergency contraception using levonorgestrel oral tablets (Plan B One-Step; Duramed Pharmaceuticals) is another concern. Plan B One-Step should be taken orally as soon as possible within 72 hours after unprotected intercourse or a known or suspected contraceptive failure. Efficacy is better if Plan B is taken as soon as possible after unprotected intercourse. There are 2 dosages: 1 tablet of levonorgestrel 1.5 mg or 2 tablets of levonorgestrel 0.75 mg. The second 0.75-mg tablet should be taken 12 hours after the first dose.9
Plan B can be used at any time during the menstrual cycle. In a series of 2,445 women aged 15 to 48 years who took levonorgestrel tablets for emergency contraception (Phase IV clinical trial), 5 pregnancies occurred (0.2%).10
ACOG advises that emergency contraception using a pill or the copper IUD should be initiated as soon as possible (up to 5 days) after unprotected coitus or inadequately protected coitus.9
Retained products of contraception
ACOG Practice Bulletin No. 135 on complications associated with second trimesterabortion discusses retained POC.11 The approach to second trimester abortion includes dilation and evacuation (D&E) as well as medical therapy with mifepristone and misoprostol. D&E, a safe and effective approach with advantages over medical abortion, is associated with fewer complications (up to 4%) versus medical abortion (29%); the primary complication is retained POC (placenta).11
Read about the legal considerations of this case.
Legal considerations
The malpractice lawsuit filed in this case claims that the gynecologist failed to exercise the level of care of a reasonably prudent practitioner under the circumstances and was therefore negligent or in breach of a duty to the patient.
First, a lawyer would look for a medical error that was related to some harm. Keep in mind that not all medical errors are negligent or subject to liability. Many medical errors occur even though the physician has exercised all reasonable care and engaged in sound practice, given today’s medical knowledge and facilities. When harm is caused through medical error that was careless or otherwise does not meet the standard of care, financial recovery is possible for the patient through a malpractice claim.12
In this case, the expert witnesses’ statements focus on the issue of conducting a pregnancy test prior to IUD insertion. The patient’s expert testified that failure to perform a pregnancy test was below an acceptable standard of care. That opinion may have been based on the typical practice of gynecologists, widely accepted medical text books, and formal practice standards of professional organizations.13
Cost-benefit analysis. Additional support for the claim that not performing the pregnancy test is negligent comes from applying a cost-benefit analysis. In this analysis, the risks and costs of performing a pregnancy test are compared with the benefits of doing the test.
In this case, the cost of conducting the pregnancy test is very low: essentially risk-freeand relatively inexpensive. On the other hand, the harm that could be avoided would be significant. Kim and colleagues suggest that pregnant women with an IUD in utero are at very high risk for adverse pregnancy outcomes.7 Given that women receiving IUDs are candidates for pregnancy (and perhaps do not know they are pregnant), a simple, risk-free pregnancy test would seem to be an efficient way to avoid a nontrivial harm.14
Did she have unprotected sex? The gynecologist’s expert notes that the patient told the gynecologist that she did not have unprotected coitus. Furthermore, the patient withheld from the gynecologist the information that she had taken Plan B because of a broken condom. Is this a defense against the malpractice claim? The answer is “possibly no,” or “possibly somewhat.”
As for unprotected coitus, the patient could easily have misunderstood the question. Technically, the answer “no” was correct. She had not had unprotected sex—it is just that the protection (condom) failed. It does not appear from the facts that she disclosed or was asked about Plan B or other information related to possible failed contraception. As to whether the patient’s failure to provide that information could be a defense for the physician, the best answer is “possibly” and “somewhat.” (See below.)15
Withholding information. Patients, of course, have a responsibility to inform their physicians of information they know is relevant. Many patients, however, will not know what is relevant (or why), or will not be fully disclosing.
Professionals cannot ignore the fact that their patients and clients are often confused, do not understand what is important and relevant, and cannot always be relied upon. For that very reason, professionals generally are obliged to start with the proposition that they may not have all of the relevant information. In this case, this lack of information makes the cost-calculation of performing a pregnancy test that much more important. The risk of not knowing whether a patient is pregnant includes the fact that many patients just will not know or cannot say with assurance.16
A “somewhat” defense and comparative negligence
Earlier we referred to a “somewhat” defense. Almost all states now have some form of “comparative negligence,” meaning that the patient’s recovery is reduced by the proportion of the blame (negligence) that is attributed to the patient. The most common form of comparative negligence works this way: If there are damages of $100,000, and the jury finds that the fault is 20% the patient’s and 80% the physician’s, the patient would receive $80,000 recovery. (In the past, the concept of “contributory negligence” could result in the plaintiff being precluded from any recovery if the plaintiff was partially negligent—those days are mostly gone.)
Related Article:
Informed consent: The more you know, the more you and your patient are protected
Statement of risks, informed consent, and liability
The gynecologist must provide an adequate description of the IUD risks. The case facts indicate that appropriate risks were discussed and literature provided, so it appears there was probably appropriate informed consent in this case. If not true, this would provide another basis for recovery.
Two other aspects of this case could be the basis for liability. We can assume that the attempted removal of the IUD was performed competently.16 In addition, if the IUD was defective in terms of design, manufacture, or warnings, the manufacturer of the device could be subject to liability.17
Final verdict: Out of court settlement
Why would the gynecologist and the insurance company settle this case? After all, they have some arguments on their side, and physicians win the majority of malpractice cases that go to trial.18 On the other hand, the patient’s expert witness’ testimony and the cost-benefit analysis of the pregnancy test are strong, contrary claims.
Cases are settled for a variety of reasons. Litigation is inherently risky. In this case, we assume that the court denied a motion to dismiss the case before trial because there is a legitimate question of fact concerning what a reasonably prudent gynecologist would have done under the circumstances. That means a jury would probably decide the issue of medical judgment, which is generally disconcerting. Furthermore, the comparative negligence defense that the patient did not tell the gynecologist about the failed condom/Plan B would most likely reduce the amount of damages, but not eliminate liability. The questions regarding the pressure to terminate a second trimester pregnancy might well complicate a jury’s view.
Other considerations include the high costs in time, money, uncertainty, and disruption associated with litigation. The settlement amount was not stated, but the process of negotiating a settlement would allow factoring in the comparative negligence aspect of the case. It would be reasonable for this case to settle before trial.
Should the physician have apologized before trial? The gynecologist could have sent a statement of regret or apology to the patient before a lawsuit was filed. Most states now have statutes that preclude such statements of regret or apology from being used against the physician. Many experts now favor apology statements as a way to reduce the risk of malpractice suits being filed.19
Related Article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
Defensive medicine. There has been much discussion of “defensive medicine” in recent years.20 It is appropriately criticized when additional testing is solely used to protect the physician from liability. However, much of defensive medicine is not only to protect the physician but also to protect the patient from potential physical and mental harm. In this case, it would have been “careful medicine” in addition to “defensive medicine.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Heikinheimo O, Gemell-Danielsson K. Emerging indications for the levonorgestrel-releasing intrauterine system. ACTA Obstet Gynecol Scand. 2012;91(1):3–9.
- Mirena [prescribing information]. Whippany, NJ: Bayer HealthCare Pharmaceuticals Inc; 2000.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol. 2011;118(1):184–196.
- Rapid EC–Random clinical trial assessing pregnancy with intrauterine devices for emergency contraception. Clinical Trials Identifier: NCT02175030. https://www.clinicaltrials.gov/ct2/show/NCT02175030?term=NCT02175030&rank=1. Updated May 1, 2017. Accessed May 11, 2017.
- Gnoth C, Johnson S. Strips of hope: Accuracy of home pregnancy tests and new developments. Gerburtshilfe Frauenheilkd. 2014;74(7):661–669.
- Cole LA, Khanlian SA, Sutton JM, Davies S, Rayburn WF. Accuracy of home pregnancy tests at the time of missed menses. Am J Obstet Gynecol. 2004;190(1):100–105.
- Kim S, Romero R, Kusanovic J, et al. The prognosis of pregnancy conceived despite the presence of an intrauterine device (IUD). J Perinatal Med. 2010;38(1):45–53.
- Brahmi D, Steenland M, Renner R, Gaffield M, Curtis K. Pregnancy outcomes with an IUD in situ: a systematic review. Contraception. 2012;85(2):131–139.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 152: Emergency contraception. Obstet Gynecol. 2015;126(3):685–686.
- Chen Q, Xiang W, Zhang D, et al. Efficacy and safety of a levonorgestrel enteric-coated tablet as an over-the-counter drug for emergency contraception: a Phase IV clinical trial. Hum Reprod. 2011;26(9):2316–2321.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 135: Second-trimester abortion. Obstet Gynecol. 2013;121(6):1395–1406.
- White A, Pichert J, Bledsoe S, Irwin C, Entman S. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt1):1031–1038.
- Mehlman M. Professional power and the standard of care in medicine. Case Western Reserve University Scholarly Commons. 2012: Paper 574. http://scholarlycommons.law.case.edu/cgi/viewcontent.cgi?article=1576&context=faculty_publications. Accessed May 11, 2017.
- Klein D, Arnold J, Reese E. Provision of contraception: key recommendations from the CDC. Am Fam Physician. 2015;91(9);625–633.
- Reyes J, Reyes R. The effects of malpractice liability on obstetrics and gynecology: taking the measure of a crisis. N England Law Rev. 2012;47;315–348. https://www.scribd.com/document/136514285/Reyes-Reyes-The-Effect-of-Malpractice-Liability-on-Obstetrics-and -Gynecology#fullscreen&from_embed. Accessed May 11, 2017.
- Peckham C. Medscape Malpractice Report 2015: Why Ob/Gyns get sued. http://www.medscape.com/features/slideshow/malpractice-report-2015/obgyn#page=1. Published January 22, 2016. Accessed May 11. 2017.
- Rheingold P, Paris D. Contraceptives. In: Vargo JJ, ed. Products Liability Practice Guide New York, New York: Matthew Bender & Company; 2017;C:62.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
- Helmreich JS. Does sorry incriminate? Evidence, harm and the protection of apology. Cornell J Law Public Policy. 2012;21(3);567–609. http://scholarship.law.cornell.edu/cgi/viewcontent.cgi?article=1363&context=cjlpp.
- Baicker K, Wright B, Olson N. Reevaluating reports of defensive medicine. J Health Polit Policy Law. 2015;40(6);1157–1177.
- Heikinheimo O, Gemell-Danielsson K. Emerging indications for the levonorgestrel-releasing intrauterine system. ACTA Obstet Gynecol Scand. 2012;91(1):3–9.
- Mirena [prescribing information]. Whippany, NJ: Bayer HealthCare Pharmaceuticals Inc; 2000.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol. 2011;118(1):184–196.
- Rapid EC–Random clinical trial assessing pregnancy with intrauterine devices for emergency contraception. Clinical Trials Identifier: NCT02175030. https://www.clinicaltrials.gov/ct2/show/NCT02175030?term=NCT02175030&rank=1. Updated May 1, 2017. Accessed May 11, 2017.
- Gnoth C, Johnson S. Strips of hope: Accuracy of home pregnancy tests and new developments. Gerburtshilfe Frauenheilkd. 2014;74(7):661–669.
- Cole LA, Khanlian SA, Sutton JM, Davies S, Rayburn WF. Accuracy of home pregnancy tests at the time of missed menses. Am J Obstet Gynecol. 2004;190(1):100–105.
- Kim S, Romero R, Kusanovic J, et al. The prognosis of pregnancy conceived despite the presence of an intrauterine device (IUD). J Perinatal Med. 2010;38(1):45–53.
- Brahmi D, Steenland M, Renner R, Gaffield M, Curtis K. Pregnancy outcomes with an IUD in situ: a systematic review. Contraception. 2012;85(2):131–139.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 152: Emergency contraception. Obstet Gynecol. 2015;126(3):685–686.
- Chen Q, Xiang W, Zhang D, et al. Efficacy and safety of a levonorgestrel enteric-coated tablet as an over-the-counter drug for emergency contraception: a Phase IV clinical trial. Hum Reprod. 2011;26(9):2316–2321.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 135: Second-trimester abortion. Obstet Gynecol. 2013;121(6):1395–1406.
- White A, Pichert J, Bledsoe S, Irwin C, Entman S. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt1):1031–1038.
- Mehlman M. Professional power and the standard of care in medicine. Case Western Reserve University Scholarly Commons. 2012: Paper 574. http://scholarlycommons.law.case.edu/cgi/viewcontent.cgi?article=1576&context=faculty_publications. Accessed May 11, 2017.
- Klein D, Arnold J, Reese E. Provision of contraception: key recommendations from the CDC. Am Fam Physician. 2015;91(9);625–633.
- Reyes J, Reyes R. The effects of malpractice liability on obstetrics and gynecology: taking the measure of a crisis. N England Law Rev. 2012;47;315–348. https://www.scribd.com/document/136514285/Reyes-Reyes-The-Effect-of-Malpractice-Liability-on-Obstetrics-and -Gynecology#fullscreen&from_embed. Accessed May 11, 2017.
- Peckham C. Medscape Malpractice Report 2015: Why Ob/Gyns get sued. http://www.medscape.com/features/slideshow/malpractice-report-2015/obgyn#page=1. Published January 22, 2016. Accessed May 11. 2017.
- Rheingold P, Paris D. Contraceptives. In: Vargo JJ, ed. Products Liability Practice Guide New York, New York: Matthew Bender & Company; 2017;C:62.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
- Helmreich JS. Does sorry incriminate? Evidence, harm and the protection of apology. Cornell J Law Public Policy. 2012;21(3);567–609. http://scholarship.law.cornell.edu/cgi/viewcontent.cgi?article=1363&context=cjlpp.
- Baicker K, Wright B, Olson N. Reevaluating reports of defensive medicine. J Health Polit Policy Law. 2015;40(6);1157–1177.
Informed consent: The more you know, the more you and your patient are protected
CASE: Surgeon accused of performing tubal ligation without consent
A patient was scheduled for an elective cesarean delivery to be performed by her ObGyn (Dr. Surgeon) at the nearby medical center. The patient was asked to sign an electronic signature pad in her ObGyn’s office, which transposed her signature onto an electronic form that she could not see at the time. She signed it. The consent was not printed out in the office but was added to her electronic medical record, and a copy was sent to her via email. Among other things, the consent included, “[Name] hereby agrees that all appropriate medical and surgical procedures as determined by the physicians and others in this hospital are in my best interest. No further consent is required to any of the treatment in this hospital.”
In the hospital, Dr. Surgeon spoke preoper- atively with the patient about cesarean delivery, the various risks and benefits, and the possibility and risks of an alternative trial of labor. Dr. Surgeon noted the conversation in the patient’s chart.
A nurse brought a standard hard copy “Zee Hospital Surgical Consent Form” to the patient. In a relevant part it provided, “I hereby consent to the surgical procedure Dr. Surgeon has discussed with me: _______” (the blank was filled in with “cesarean delivery”). The form continued: “He/She has explained the risks and benefits. I also authorize Dr. Surgeon, and such assistants as he/she may select, to perform this procedure. In his/her medical judgment, if additional procedures are appropriate, I hereby consent to their performance, in addition to the procedures listed in this form.” The patient signed the form.
While Dr. Surgeon was scrubbing for the delivery, the patient’s husband (also a surgeon at the hospital; Dr. Husband), stopped by, thanked Dr. Surgeon, and said, “Oh, by the way, my wife would like you to do a tubal ligation as well—she really wants it for health reasons. Her chronic hypertension skyrocketed during this pregnancy, and we don’t want any more children.”
“She didn’t mention that a little earlier while I was talking with her,” replied Dr. Surgeon, “but I can see how it would have slipped her mind.”
Dr. Surgeon performed the cesarean delivery and tubal ligation. All went well, with a healthy baby and mother. Several months later, the patient and Dr. Husband separated and sought divorce.
The patient, surprised by the cost of the hospital bill (Dr. Surgeon did not bill for his surgical services as a professional courtesy), was astonished to see a charge related to tubal ligation. Knowing how common billing mistakes were at Zee Hospital, she called to have the bill corrected. The clerk informed her that her medical record showed that a tubal ligation had been performed and that the bill was correct.
The patient sued Dr. Surgeon, Zee Hospital, and her (now former) husband, Dr. Husband, both for the cesarean delivery and the tubal ligation. Her claims are primarily based on the lack of informed consent.
What’s the verdict?
The patient likely has a strong case regarding the tubal ligation claim, but a weak case related to the cesarean delivery claim.
Read the ethical, medical, and legal implications of this case
Ethical and medical considerations
Although this case seems too strange for fiction, the basic facts are taken from events that did occur at a major institution. The puzzling features of this case are meant to be a cautionary tale: it is easy in the rush with the pressure of clinical practice to view informed consent as a bothersome technical detail. Yet as the following discussion suggests, adhering closely to the tenets of informed consent protects not only the fundamental interests of the patient but also the physicians and medical institutions.
Informed consent serves as protective communication
Informed consent at its core is a “process of communication” that involves you as the health care provider and the patient. It provides authority for an activity based upon an understanding of what that activity entails.1,2 Aspects of informed consent, from the physician−patient perspective, include the following:
- disclosure
- comprehension
- voluntary choice
- authorization.
In one other sense, informed consent is based on a fiduciary relationship between the ObGyn and patient.3 Overall, the process consists of an educational communication by the physician to the patient. Ideally, providers perceive the process from an ethical point of view that has been formalized by cases and statutes.4
Informed consent protects one of the most basic values of medicine and society: autonomy. From the perspective of moral philosophers, the principle of autonomy establishes the moral right to choose and follow one’s own plan for life and action.5,6 For ObGyns, the patient’s autonomy and her ability to participate in the medical decision-making process is of paramount importance. Informed consent is also a reflection of trust inherent to the physician−patient relationship.4
Informed consent is too often viewed as a mere legal formality. In truth, it melds legal and ethical values and concerns. The President’s Commission reflected this, noting that informed consent is rooted in “the fundamental recognition that adults are entitled to accept or reject health care intervention(s) on the basis of their own personal values and in furtherance of their own personal goals.”7
The historic perspective of informed consent dates back to Egyptian, Greek, and Roman eras. Dhar and Dhar suggest that the concept of “physicians’ love for humanity—philantropia” dates back to Plato and is complemented by the term “philotechnia” (love of medicine), all of which have evolved into today’s use of the terms “risks, benefits, and alternatives.”8
We emphasize that informed consent is much more than a legal concept. It has strong clinical roots because it provides an opportunity for physicians to improve communication with their patients. Informed consent is not a form; it is a process to be taken seriously.
Legal principles of informed consent
The famous New York case of Mary Schloendorff v. Society of New York Hospital, in 1914, heralded a principle that remains central in American law. Justice Benjamin Cardozo, writing for the majority, held that, “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent commits an assault for which he is liable in damages.”9 The surgeon in the Schloendorff case had undertaken a gynecologic procedure—removal of a fibroid tumor—without patient consent. (In that case the hospital rather than the physician was sued, but the principle clearly applied to the physician.)
Over the last century, the American law of informed consent has developed in a number of ways.10 Lack of informed consent is now almost always considered a form of negligence rather than an intentional tort of battery. The details of the legal requirements vary from state to state as a result of statutory changes and court decisions. But in one way or another, to be “informed,” consent generally must include 4 things:
- a description of the procedure or intervention that is proposed
- the risks and benefits of the proposal—the focus here is generally on the risks of the treatment
- alternatives, if there are any (eg, pharmacologic vs surgical treatment)
- the consequences of not undertaking the proposed treatment (eg, the refusal to have a Papanicolaou smear).
A fifth point might be added—the offer to answer any questions or provide additional information.
These 4 or 5 basic items and the expanded list are efforts to simply describe the information that a reasonable person would need in order to make a decision that represents the patient’s values, personality, and preferences. (Informed consent is in some ways an ongoing process—since a patient may withdraw his/her consent.)
Exceptions to the informed consent requirement
Before turning to the facts in the hypothetical case, it is worth noting that there are 2 common exceptions to the informed consent requirement. The first is an emergency exception. When someone requires immediate attention and the patient is not conscious or capable of consent (nor is a “next of kin” available), treatment may proceed.
The second is therapeutic exception. Its designation is narrow, and it is risky to rely on it except in extreme circumstances. But when the very process of informing the patient of all the risks of a proposed treatment would create significant additional risks for the patient, the consent process may be modified. For example, for an extremely suggestable patient, describing certain risks might, in a psychosomatic way, cause the risk to be realized. In such cases, the record must be clearly documented. It is generally best to discuss the matter with a family member or other surrogate decision maker.
Read what went wrong in this case
What went wrong with consent in this case?
Our case illustrates a number of problems that occur when informed consent is not properly completed.
The electronic signature on the broadly stated consent form the patient initially signed in the office was nearly useless. She did not know what she was signing, did not have any chance to read it before signing, and was provided no help with any of the information factors of informed consent.
The surgical consent form is among the most interesting elements of this case. The form itself was seriously flawed because it contained no real evidence that the patient received information about the risks and alternatives. If the form is all there was, it would be a problem. But the conversation that Dr. Surgeon documented with the patient seemed to provide the basic elements of informed consent, including discussion of risks and benefits.
Oral informed consent is recognized in most states. To his credit, Dr. Surgeon appropriately recorded the conversation in the record. The risk of oral informed consent not backed up by text signature is that, if a dispute arises about the consent, it is difficult to prove details of what was said. (There was, of course, no such dispute about the cesarean delivery as it turned out in this case.)
Technological add-ons to consent: Pros and cons
Video and computer software are increasingly becoming an integral part of the informed consent process, and may improve comprehension by patients.11 Electronic consent may be helpful in proving what the patient was told during the consent process. A difficulty can result from overreliance on the electronic aspect and forgetting the human part of the informed consent equation. The health care team often can be productive parts of the informed consent process, but the surgeon must take ultimate responsibility for the informed consent.12
Was there informed consent for the tubal ligation?
The major problem in this case, of course, was the tubal ligation. It does not take much of an understanding of the legal niceties of informed consent to know that there was no real consent to this procedure. Dr. Husband did not have authority to consent, and his comment to Dr. Surgeon did not qualify as consent.
The hospital consent form may appear to provide some legal protection (“In his medical judgment, if additional procedures are appropriate, I hereby consent to doing those….”). Such language was once common in informed consent forms, but it offered little real consent except for trivial incidental processes (removal of an appendix) or where there was a real medical necessity for doing an expanded procedure (removal of a previously unknown cancerous growth).
Thus, Dr. Surgeon performed the sterilization without consent and may well be liable for that part of the surgery even though it did not turn out badly in a medical sense. If not for the tubal ligation, the damages would probably have been trivial. The real loss here is not a medical injury; it is the loss of reproductive capacity.
Protecting reproductive capacity. Modern law has been especially sensitive to protecting decisions regarding reproductive capacity. Therefore, the absence of clear consent to permanent sterilization is legally problematic. Dr. Surgeon may claim that he reasonably believed that the husband could give surrogate consent and it was too late to check with the patient herself. This situation does not fit well with the emergency exception, and it appears from the facts that Dr. Surgeon acted without informed consent to the sterilization.
Was it negligence or battery?
Dr. Surgeon. The most likely basis for liability for Dr. Surgeon is negligence. There is some argument that the tort of battery is a possibility because there was no consent at all for the sterilization. The claim would be that it was not the “information” that was lacking; it was the consent itself. The fact that Dr. Surgeon did not charge for his services would not absolve him of liability.
Dr. Husband. The potential liability of Dr. Husband is complicated by questions of whether he was acting in the capacity of a physician (which would likely involve the question of whether his malpractice insurance would be available), the degree to which he was acting in good faith, and facts we do not have in this case. If Dr. Husband gave consent (and thereby “caused”) the sterilization knowing that his wife did not want to have it or because of animus toward her (they were about to be separated and divorced, after all), there is the possibility of liability. (In some states a form of interspousal liability might complicate some of these claims—but that is a topic for another day.) He essentially took action for the purpose of wrongly causing the sterilization—which may be a battery (an intentional offensive or harmful touching). The legal rules around battery allow punitive damages as well as compensatory damages. In addition, many malpractice insurance policies provide limited coverage for intentional torts. To complicate matters further, it is not clear that Dr. Husband’s actions were related to his practice of medicine in any event (although Dr. Surgeon might claim that Dr. Husband’s expressed concern about his wife’s hypertension was enough to create a malpractice issue if Dr. Surgeon did not perform the verbally requested tubal ligation).
If, as we have speculated, Dr. Husband’s actions were motivated by improper personal considerations at the expense of a patient, he may also face medical board complaints from the patient. It is plausible that a state law makes it a criminal offense to wrongfully (or fraudulently) consent to medical treatment, particularly if related to reproductive capacity.
The hospital may face liability on several grounds, depending in part on the relationships between the hospital, Dr. Surgeon, and Dr. Husband. If Dr. Surgeon is an employee or agent of the hospital, he would be liable for his negligence. Even if Dr. Surgeon is technically an independent contractor, the failure of the hospital to offer more oversight concerning the surgical procedures in its facilities could give rise to a claim of negligence.
As to Dr. Husband, many of the same considerations are present. In addition, even if he is an agent of the hospital, the hospital may claim that his actions (especially if motivated by personal considerations) were a “lark of his own” and not in the course of his employment by the hospital.
Read about the clinical opportunity of informed consent
The clinical opportunity of informed consent
More than a technical legal doctrine, informed consent provides ObGyns an important opportunity for better communications with patients, and is a chance to create reasonable expectations and a more therapeutic relationship that involves the patient in care and decision making. It is likely that engaging the patient in good informed consent processes can set the stage for improved outcomes.
Interactive dialogue with the patient is one advised approach.10 This undertaking in part reflects that, as patients have more ready access to information in the digital age, they are positioned to play a more active role in health care decision making.
The benefits of informed consent are likely to be greatest if you view the process not as a technical legal requirement but as an excellent opportunity to engage the patient in her own care and treatment. Planning, intervention, and evaluation of care options as well as education regarding the medical problem at hand are integral to the informed consent process. And, of course, the right to consent is a “basic patient right” that in a sense guarantees that he/she has the right to make informed decisions regarding one’s care.6
Special considerations
Informed consent most often is associated with but not limited to surgical procedures (often performed with the use of surgical instruments and/or devices). It applies to diagnostic interventions as well as treatment. The more invasive or risky an intervention, the more important it is that the information is thorough.14,15
Pharmaceuticals have informed consent issues. The theory has been that pharmaceutical companies inform physicians of the risks and instructions for the use of pharmaceuticals and the physicians inform the patients. Indeed, traditionally pharmaceutical companies have gained immunity for “failure to warn” patients because the physicians were the “learned intermediaries” providing information to the public. Patient package inserts and pharmacists have taken over the informational role, but informed consent does apply to pharmaceuticals.
It is also worth noting that informed consent in any formal research study or the trial of new techniques, compounds, or devices requires a special process of approval by an institutional review board.
Set the stage for best outcomes
The main objective of informed consent is promoting the autonomy of your patient. That requires that she understand the risks, benefits, and alternatives associated with the procedure and the risks associated with a refusal of treatment. Done properly, this can result in your patient gaining confidence and trust in you as her provider.
Informed consent is a process that reflects our interactions with our patients. It is part of the broader commitment by the medical profession to “first do no harm.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Grady C. Enduring and emerging challenges of informed consent. N Engl J Med. 2015;372(22):855–862.
- Faden RR, Beauchamp TL. History and theory of informed consent. New York, New York: Oxford University Press; 1986.
- Paterick TJ, Carson G, Allen M, Paterick TE. Medical informed consent: general considerations for physicians. Mayo Clin Proc. 2008;83(3):313–319.
- American College of Obstetricians and Gynecologists Committee on Ethics. ACOG Committee Opinion No. 439: Informed consent (reaffirmed 2015). Obstet Gynecol. 2009;114(2 pt 1):401–408.
- Jonsen A, Siegler M, Winslade W. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. New York, New York: McGraw Hill; 2010.
- Menendez J. Informed consent: essential legal and ethical principles for nurses. JONAS Healthc Law Ethics Regul. 2013;15(4):140–144.
- Abram MB, Ballantine HT, Dunlop GR, et al; President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Making Health Care Decisions: The Ethical and Legal Implications of Informed Consent in the Patient-Practitioner Relationship. Volume One: Report. https://repository.library.georgetown.edu/bitstream/handle/10822/559354/making_health_care_decisions.pdf?sequence=1. Published October 1982. Accessed January 9, 2017.
- Dhar H, Dhar D. Informed consent in clinical practice and literature overview. Arch Gynecol Obstet. 2012;286(3):649–651.
- NE Schloendorff v Society of New York Hospital, 211 NY 125, 106 NE 93 1914.
- Avery D. Summary of informed consent and refusal. Am J Clinical Med. 2009;6(3):28–29.
- Pallett A, Phippen N, Miller C, Barnett J. Informed consent for hysterectomy: Does a video presentation improve patient comprehension? [poster 17F]. Obstet Gynecol. 2016;127(suppl):55S.
- Cainzos M, Gonzalez-Vinagre S. Informed consent in surgery. World J Surg. 2014;38(7):1587–1593.
- Weaver J. A problem with informed consent. J Am Coll Surg. 2009;209(2):286–287.
- Bunch W. Informed consent. Clin Orthop Relat Res. 2000;378:71–77.
- Peltier LF. Orthopedics: a history and iconography (Norman Orthopedic, No. 3). San Francisco, California: Jeremy Norman Co; 1993.
CASE: Surgeon accused of performing tubal ligation without consent
A patient was scheduled for an elective cesarean delivery to be performed by her ObGyn (Dr. Surgeon) at the nearby medical center. The patient was asked to sign an electronic signature pad in her ObGyn’s office, which transposed her signature onto an electronic form that she could not see at the time. She signed it. The consent was not printed out in the office but was added to her electronic medical record, and a copy was sent to her via email. Among other things, the consent included, “[Name] hereby agrees that all appropriate medical and surgical procedures as determined by the physicians and others in this hospital are in my best interest. No further consent is required to any of the treatment in this hospital.”
In the hospital, Dr. Surgeon spoke preoper- atively with the patient about cesarean delivery, the various risks and benefits, and the possibility and risks of an alternative trial of labor. Dr. Surgeon noted the conversation in the patient’s chart.
A nurse brought a standard hard copy “Zee Hospital Surgical Consent Form” to the patient. In a relevant part it provided, “I hereby consent to the surgical procedure Dr. Surgeon has discussed with me: _______” (the blank was filled in with “cesarean delivery”). The form continued: “He/She has explained the risks and benefits. I also authorize Dr. Surgeon, and such assistants as he/she may select, to perform this procedure. In his/her medical judgment, if additional procedures are appropriate, I hereby consent to their performance, in addition to the procedures listed in this form.” The patient signed the form.
While Dr. Surgeon was scrubbing for the delivery, the patient’s husband (also a surgeon at the hospital; Dr. Husband), stopped by, thanked Dr. Surgeon, and said, “Oh, by the way, my wife would like you to do a tubal ligation as well—she really wants it for health reasons. Her chronic hypertension skyrocketed during this pregnancy, and we don’t want any more children.”
“She didn’t mention that a little earlier while I was talking with her,” replied Dr. Surgeon, “but I can see how it would have slipped her mind.”
Dr. Surgeon performed the cesarean delivery and tubal ligation. All went well, with a healthy baby and mother. Several months later, the patient and Dr. Husband separated and sought divorce.
The patient, surprised by the cost of the hospital bill (Dr. Surgeon did not bill for his surgical services as a professional courtesy), was astonished to see a charge related to tubal ligation. Knowing how common billing mistakes were at Zee Hospital, she called to have the bill corrected. The clerk informed her that her medical record showed that a tubal ligation had been performed and that the bill was correct.
The patient sued Dr. Surgeon, Zee Hospital, and her (now former) husband, Dr. Husband, both for the cesarean delivery and the tubal ligation. Her claims are primarily based on the lack of informed consent.
What’s the verdict?
The patient likely has a strong case regarding the tubal ligation claim, but a weak case related to the cesarean delivery claim.
Read the ethical, medical, and legal implications of this case
Ethical and medical considerations
Although this case seems too strange for fiction, the basic facts are taken from events that did occur at a major institution. The puzzling features of this case are meant to be a cautionary tale: it is easy in the rush with the pressure of clinical practice to view informed consent as a bothersome technical detail. Yet as the following discussion suggests, adhering closely to the tenets of informed consent protects not only the fundamental interests of the patient but also the physicians and medical institutions.
Informed consent serves as protective communication
Informed consent at its core is a “process of communication” that involves you as the health care provider and the patient. It provides authority for an activity based upon an understanding of what that activity entails.1,2 Aspects of informed consent, from the physician−patient perspective, include the following:
- disclosure
- comprehension
- voluntary choice
- authorization.
In one other sense, informed consent is based on a fiduciary relationship between the ObGyn and patient.3 Overall, the process consists of an educational communication by the physician to the patient. Ideally, providers perceive the process from an ethical point of view that has been formalized by cases and statutes.4
Informed consent protects one of the most basic values of medicine and society: autonomy. From the perspective of moral philosophers, the principle of autonomy establishes the moral right to choose and follow one’s own plan for life and action.5,6 For ObGyns, the patient’s autonomy and her ability to participate in the medical decision-making process is of paramount importance. Informed consent is also a reflection of trust inherent to the physician−patient relationship.4
Informed consent is too often viewed as a mere legal formality. In truth, it melds legal and ethical values and concerns. The President’s Commission reflected this, noting that informed consent is rooted in “the fundamental recognition that adults are entitled to accept or reject health care intervention(s) on the basis of their own personal values and in furtherance of their own personal goals.”7
The historic perspective of informed consent dates back to Egyptian, Greek, and Roman eras. Dhar and Dhar suggest that the concept of “physicians’ love for humanity—philantropia” dates back to Plato and is complemented by the term “philotechnia” (love of medicine), all of which have evolved into today’s use of the terms “risks, benefits, and alternatives.”8
We emphasize that informed consent is much more than a legal concept. It has strong clinical roots because it provides an opportunity for physicians to improve communication with their patients. Informed consent is not a form; it is a process to be taken seriously.
Legal principles of informed consent
The famous New York case of Mary Schloendorff v. Society of New York Hospital, in 1914, heralded a principle that remains central in American law. Justice Benjamin Cardozo, writing for the majority, held that, “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent commits an assault for which he is liable in damages.”9 The surgeon in the Schloendorff case had undertaken a gynecologic procedure—removal of a fibroid tumor—without patient consent. (In that case the hospital rather than the physician was sued, but the principle clearly applied to the physician.)
Over the last century, the American law of informed consent has developed in a number of ways.10 Lack of informed consent is now almost always considered a form of negligence rather than an intentional tort of battery. The details of the legal requirements vary from state to state as a result of statutory changes and court decisions. But in one way or another, to be “informed,” consent generally must include 4 things:
- a description of the procedure or intervention that is proposed
- the risks and benefits of the proposal—the focus here is generally on the risks of the treatment
- alternatives, if there are any (eg, pharmacologic vs surgical treatment)
- the consequences of not undertaking the proposed treatment (eg, the refusal to have a Papanicolaou smear).
A fifth point might be added—the offer to answer any questions or provide additional information.
These 4 or 5 basic items and the expanded list are efforts to simply describe the information that a reasonable person would need in order to make a decision that represents the patient’s values, personality, and preferences. (Informed consent is in some ways an ongoing process—since a patient may withdraw his/her consent.)
Exceptions to the informed consent requirement
Before turning to the facts in the hypothetical case, it is worth noting that there are 2 common exceptions to the informed consent requirement. The first is an emergency exception. When someone requires immediate attention and the patient is not conscious or capable of consent (nor is a “next of kin” available), treatment may proceed.
The second is therapeutic exception. Its designation is narrow, and it is risky to rely on it except in extreme circumstances. But when the very process of informing the patient of all the risks of a proposed treatment would create significant additional risks for the patient, the consent process may be modified. For example, for an extremely suggestable patient, describing certain risks might, in a psychosomatic way, cause the risk to be realized. In such cases, the record must be clearly documented. It is generally best to discuss the matter with a family member or other surrogate decision maker.
Read what went wrong in this case
What went wrong with consent in this case?
Our case illustrates a number of problems that occur when informed consent is not properly completed.
The electronic signature on the broadly stated consent form the patient initially signed in the office was nearly useless. She did not know what she was signing, did not have any chance to read it before signing, and was provided no help with any of the information factors of informed consent.
The surgical consent form is among the most interesting elements of this case. The form itself was seriously flawed because it contained no real evidence that the patient received information about the risks and alternatives. If the form is all there was, it would be a problem. But the conversation that Dr. Surgeon documented with the patient seemed to provide the basic elements of informed consent, including discussion of risks and benefits.
Oral informed consent is recognized in most states. To his credit, Dr. Surgeon appropriately recorded the conversation in the record. The risk of oral informed consent not backed up by text signature is that, if a dispute arises about the consent, it is difficult to prove details of what was said. (There was, of course, no such dispute about the cesarean delivery as it turned out in this case.)
Technological add-ons to consent: Pros and cons
Video and computer software are increasingly becoming an integral part of the informed consent process, and may improve comprehension by patients.11 Electronic consent may be helpful in proving what the patient was told during the consent process. A difficulty can result from overreliance on the electronic aspect and forgetting the human part of the informed consent equation. The health care team often can be productive parts of the informed consent process, but the surgeon must take ultimate responsibility for the informed consent.12
Was there informed consent for the tubal ligation?
The major problem in this case, of course, was the tubal ligation. It does not take much of an understanding of the legal niceties of informed consent to know that there was no real consent to this procedure. Dr. Husband did not have authority to consent, and his comment to Dr. Surgeon did not qualify as consent.
The hospital consent form may appear to provide some legal protection (“In his medical judgment, if additional procedures are appropriate, I hereby consent to doing those….”). Such language was once common in informed consent forms, but it offered little real consent except for trivial incidental processes (removal of an appendix) or where there was a real medical necessity for doing an expanded procedure (removal of a previously unknown cancerous growth).
Thus, Dr. Surgeon performed the sterilization without consent and may well be liable for that part of the surgery even though it did not turn out badly in a medical sense. If not for the tubal ligation, the damages would probably have been trivial. The real loss here is not a medical injury; it is the loss of reproductive capacity.
Protecting reproductive capacity. Modern law has been especially sensitive to protecting decisions regarding reproductive capacity. Therefore, the absence of clear consent to permanent sterilization is legally problematic. Dr. Surgeon may claim that he reasonably believed that the husband could give surrogate consent and it was too late to check with the patient herself. This situation does not fit well with the emergency exception, and it appears from the facts that Dr. Surgeon acted without informed consent to the sterilization.
Was it negligence or battery?
Dr. Surgeon. The most likely basis for liability for Dr. Surgeon is negligence. There is some argument that the tort of battery is a possibility because there was no consent at all for the sterilization. The claim would be that it was not the “information” that was lacking; it was the consent itself. The fact that Dr. Surgeon did not charge for his services would not absolve him of liability.
Dr. Husband. The potential liability of Dr. Husband is complicated by questions of whether he was acting in the capacity of a physician (which would likely involve the question of whether his malpractice insurance would be available), the degree to which he was acting in good faith, and facts we do not have in this case. If Dr. Husband gave consent (and thereby “caused”) the sterilization knowing that his wife did not want to have it or because of animus toward her (they were about to be separated and divorced, after all), there is the possibility of liability. (In some states a form of interspousal liability might complicate some of these claims—but that is a topic for another day.) He essentially took action for the purpose of wrongly causing the sterilization—which may be a battery (an intentional offensive or harmful touching). The legal rules around battery allow punitive damages as well as compensatory damages. In addition, many malpractice insurance policies provide limited coverage for intentional torts. To complicate matters further, it is not clear that Dr. Husband’s actions were related to his practice of medicine in any event (although Dr. Surgeon might claim that Dr. Husband’s expressed concern about his wife’s hypertension was enough to create a malpractice issue if Dr. Surgeon did not perform the verbally requested tubal ligation).
If, as we have speculated, Dr. Husband’s actions were motivated by improper personal considerations at the expense of a patient, he may also face medical board complaints from the patient. It is plausible that a state law makes it a criminal offense to wrongfully (or fraudulently) consent to medical treatment, particularly if related to reproductive capacity.
The hospital may face liability on several grounds, depending in part on the relationships between the hospital, Dr. Surgeon, and Dr. Husband. If Dr. Surgeon is an employee or agent of the hospital, he would be liable for his negligence. Even if Dr. Surgeon is technically an independent contractor, the failure of the hospital to offer more oversight concerning the surgical procedures in its facilities could give rise to a claim of negligence.
As to Dr. Husband, many of the same considerations are present. In addition, even if he is an agent of the hospital, the hospital may claim that his actions (especially if motivated by personal considerations) were a “lark of his own” and not in the course of his employment by the hospital.
Read about the clinical opportunity of informed consent
The clinical opportunity of informed consent
More than a technical legal doctrine, informed consent provides ObGyns an important opportunity for better communications with patients, and is a chance to create reasonable expectations and a more therapeutic relationship that involves the patient in care and decision making. It is likely that engaging the patient in good informed consent processes can set the stage for improved outcomes.
Interactive dialogue with the patient is one advised approach.10 This undertaking in part reflects that, as patients have more ready access to information in the digital age, they are positioned to play a more active role in health care decision making.
The benefits of informed consent are likely to be greatest if you view the process not as a technical legal requirement but as an excellent opportunity to engage the patient in her own care and treatment. Planning, intervention, and evaluation of care options as well as education regarding the medical problem at hand are integral to the informed consent process. And, of course, the right to consent is a “basic patient right” that in a sense guarantees that he/she has the right to make informed decisions regarding one’s care.6
Special considerations
Informed consent most often is associated with but not limited to surgical procedures (often performed with the use of surgical instruments and/or devices). It applies to diagnostic interventions as well as treatment. The more invasive or risky an intervention, the more important it is that the information is thorough.14,15
Pharmaceuticals have informed consent issues. The theory has been that pharmaceutical companies inform physicians of the risks and instructions for the use of pharmaceuticals and the physicians inform the patients. Indeed, traditionally pharmaceutical companies have gained immunity for “failure to warn” patients because the physicians were the “learned intermediaries” providing information to the public. Patient package inserts and pharmacists have taken over the informational role, but informed consent does apply to pharmaceuticals.
It is also worth noting that informed consent in any formal research study or the trial of new techniques, compounds, or devices requires a special process of approval by an institutional review board.
Set the stage for best outcomes
The main objective of informed consent is promoting the autonomy of your patient. That requires that she understand the risks, benefits, and alternatives associated with the procedure and the risks associated with a refusal of treatment. Done properly, this can result in your patient gaining confidence and trust in you as her provider.
Informed consent is a process that reflects our interactions with our patients. It is part of the broader commitment by the medical profession to “first do no harm.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE: Surgeon accused of performing tubal ligation without consent
A patient was scheduled for an elective cesarean delivery to be performed by her ObGyn (Dr. Surgeon) at the nearby medical center. The patient was asked to sign an electronic signature pad in her ObGyn’s office, which transposed her signature onto an electronic form that she could not see at the time. She signed it. The consent was not printed out in the office but was added to her electronic medical record, and a copy was sent to her via email. Among other things, the consent included, “[Name] hereby agrees that all appropriate medical and surgical procedures as determined by the physicians and others in this hospital are in my best interest. No further consent is required to any of the treatment in this hospital.”
In the hospital, Dr. Surgeon spoke preoper- atively with the patient about cesarean delivery, the various risks and benefits, and the possibility and risks of an alternative trial of labor. Dr. Surgeon noted the conversation in the patient’s chart.
A nurse brought a standard hard copy “Zee Hospital Surgical Consent Form” to the patient. In a relevant part it provided, “I hereby consent to the surgical procedure Dr. Surgeon has discussed with me: _______” (the blank was filled in with “cesarean delivery”). The form continued: “He/She has explained the risks and benefits. I also authorize Dr. Surgeon, and such assistants as he/she may select, to perform this procedure. In his/her medical judgment, if additional procedures are appropriate, I hereby consent to their performance, in addition to the procedures listed in this form.” The patient signed the form.
While Dr. Surgeon was scrubbing for the delivery, the patient’s husband (also a surgeon at the hospital; Dr. Husband), stopped by, thanked Dr. Surgeon, and said, “Oh, by the way, my wife would like you to do a tubal ligation as well—she really wants it for health reasons. Her chronic hypertension skyrocketed during this pregnancy, and we don’t want any more children.”
“She didn’t mention that a little earlier while I was talking with her,” replied Dr. Surgeon, “but I can see how it would have slipped her mind.”
Dr. Surgeon performed the cesarean delivery and tubal ligation. All went well, with a healthy baby and mother. Several months later, the patient and Dr. Husband separated and sought divorce.
The patient, surprised by the cost of the hospital bill (Dr. Surgeon did not bill for his surgical services as a professional courtesy), was astonished to see a charge related to tubal ligation. Knowing how common billing mistakes were at Zee Hospital, she called to have the bill corrected. The clerk informed her that her medical record showed that a tubal ligation had been performed and that the bill was correct.
The patient sued Dr. Surgeon, Zee Hospital, and her (now former) husband, Dr. Husband, both for the cesarean delivery and the tubal ligation. Her claims are primarily based on the lack of informed consent.
What’s the verdict?
The patient likely has a strong case regarding the tubal ligation claim, but a weak case related to the cesarean delivery claim.
Read the ethical, medical, and legal implications of this case
Ethical and medical considerations
Although this case seems too strange for fiction, the basic facts are taken from events that did occur at a major institution. The puzzling features of this case are meant to be a cautionary tale: it is easy in the rush with the pressure of clinical practice to view informed consent as a bothersome technical detail. Yet as the following discussion suggests, adhering closely to the tenets of informed consent protects not only the fundamental interests of the patient but also the physicians and medical institutions.
Informed consent serves as protective communication
Informed consent at its core is a “process of communication” that involves you as the health care provider and the patient. It provides authority for an activity based upon an understanding of what that activity entails.1,2 Aspects of informed consent, from the physician−patient perspective, include the following:
- disclosure
- comprehension
- voluntary choice
- authorization.
In one other sense, informed consent is based on a fiduciary relationship between the ObGyn and patient.3 Overall, the process consists of an educational communication by the physician to the patient. Ideally, providers perceive the process from an ethical point of view that has been formalized by cases and statutes.4
Informed consent protects one of the most basic values of medicine and society: autonomy. From the perspective of moral philosophers, the principle of autonomy establishes the moral right to choose and follow one’s own plan for life and action.5,6 For ObGyns, the patient’s autonomy and her ability to participate in the medical decision-making process is of paramount importance. Informed consent is also a reflection of trust inherent to the physician−patient relationship.4
Informed consent is too often viewed as a mere legal formality. In truth, it melds legal and ethical values and concerns. The President’s Commission reflected this, noting that informed consent is rooted in “the fundamental recognition that adults are entitled to accept or reject health care intervention(s) on the basis of their own personal values and in furtherance of their own personal goals.”7
The historic perspective of informed consent dates back to Egyptian, Greek, and Roman eras. Dhar and Dhar suggest that the concept of “physicians’ love for humanity—philantropia” dates back to Plato and is complemented by the term “philotechnia” (love of medicine), all of which have evolved into today’s use of the terms “risks, benefits, and alternatives.”8
We emphasize that informed consent is much more than a legal concept. It has strong clinical roots because it provides an opportunity for physicians to improve communication with their patients. Informed consent is not a form; it is a process to be taken seriously.
Legal principles of informed consent
The famous New York case of Mary Schloendorff v. Society of New York Hospital, in 1914, heralded a principle that remains central in American law. Justice Benjamin Cardozo, writing for the majority, held that, “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent commits an assault for which he is liable in damages.”9 The surgeon in the Schloendorff case had undertaken a gynecologic procedure—removal of a fibroid tumor—without patient consent. (In that case the hospital rather than the physician was sued, but the principle clearly applied to the physician.)
Over the last century, the American law of informed consent has developed in a number of ways.10 Lack of informed consent is now almost always considered a form of negligence rather than an intentional tort of battery. The details of the legal requirements vary from state to state as a result of statutory changes and court decisions. But in one way or another, to be “informed,” consent generally must include 4 things:
- a description of the procedure or intervention that is proposed
- the risks and benefits of the proposal—the focus here is generally on the risks of the treatment
- alternatives, if there are any (eg, pharmacologic vs surgical treatment)
- the consequences of not undertaking the proposed treatment (eg, the refusal to have a Papanicolaou smear).
A fifth point might be added—the offer to answer any questions or provide additional information.
These 4 or 5 basic items and the expanded list are efforts to simply describe the information that a reasonable person would need in order to make a decision that represents the patient’s values, personality, and preferences. (Informed consent is in some ways an ongoing process—since a patient may withdraw his/her consent.)
Exceptions to the informed consent requirement
Before turning to the facts in the hypothetical case, it is worth noting that there are 2 common exceptions to the informed consent requirement. The first is an emergency exception. When someone requires immediate attention and the patient is not conscious or capable of consent (nor is a “next of kin” available), treatment may proceed.
The second is therapeutic exception. Its designation is narrow, and it is risky to rely on it except in extreme circumstances. But when the very process of informing the patient of all the risks of a proposed treatment would create significant additional risks for the patient, the consent process may be modified. For example, for an extremely suggestable patient, describing certain risks might, in a psychosomatic way, cause the risk to be realized. In such cases, the record must be clearly documented. It is generally best to discuss the matter with a family member or other surrogate decision maker.
Read what went wrong in this case
What went wrong with consent in this case?
Our case illustrates a number of problems that occur when informed consent is not properly completed.
The electronic signature on the broadly stated consent form the patient initially signed in the office was nearly useless. She did not know what she was signing, did not have any chance to read it before signing, and was provided no help with any of the information factors of informed consent.
The surgical consent form is among the most interesting elements of this case. The form itself was seriously flawed because it contained no real evidence that the patient received information about the risks and alternatives. If the form is all there was, it would be a problem. But the conversation that Dr. Surgeon documented with the patient seemed to provide the basic elements of informed consent, including discussion of risks and benefits.
Oral informed consent is recognized in most states. To his credit, Dr. Surgeon appropriately recorded the conversation in the record. The risk of oral informed consent not backed up by text signature is that, if a dispute arises about the consent, it is difficult to prove details of what was said. (There was, of course, no such dispute about the cesarean delivery as it turned out in this case.)
Technological add-ons to consent: Pros and cons
Video and computer software are increasingly becoming an integral part of the informed consent process, and may improve comprehension by patients.11 Electronic consent may be helpful in proving what the patient was told during the consent process. A difficulty can result from overreliance on the electronic aspect and forgetting the human part of the informed consent equation. The health care team often can be productive parts of the informed consent process, but the surgeon must take ultimate responsibility for the informed consent.12
Was there informed consent for the tubal ligation?
The major problem in this case, of course, was the tubal ligation. It does not take much of an understanding of the legal niceties of informed consent to know that there was no real consent to this procedure. Dr. Husband did not have authority to consent, and his comment to Dr. Surgeon did not qualify as consent.
The hospital consent form may appear to provide some legal protection (“In his medical judgment, if additional procedures are appropriate, I hereby consent to doing those….”). Such language was once common in informed consent forms, but it offered little real consent except for trivial incidental processes (removal of an appendix) or where there was a real medical necessity for doing an expanded procedure (removal of a previously unknown cancerous growth).
Thus, Dr. Surgeon performed the sterilization without consent and may well be liable for that part of the surgery even though it did not turn out badly in a medical sense. If not for the tubal ligation, the damages would probably have been trivial. The real loss here is not a medical injury; it is the loss of reproductive capacity.
Protecting reproductive capacity. Modern law has been especially sensitive to protecting decisions regarding reproductive capacity. Therefore, the absence of clear consent to permanent sterilization is legally problematic. Dr. Surgeon may claim that he reasonably believed that the husband could give surrogate consent and it was too late to check with the patient herself. This situation does not fit well with the emergency exception, and it appears from the facts that Dr. Surgeon acted without informed consent to the sterilization.
Was it negligence or battery?
Dr. Surgeon. The most likely basis for liability for Dr. Surgeon is negligence. There is some argument that the tort of battery is a possibility because there was no consent at all for the sterilization. The claim would be that it was not the “information” that was lacking; it was the consent itself. The fact that Dr. Surgeon did not charge for his services would not absolve him of liability.
Dr. Husband. The potential liability of Dr. Husband is complicated by questions of whether he was acting in the capacity of a physician (which would likely involve the question of whether his malpractice insurance would be available), the degree to which he was acting in good faith, and facts we do not have in this case. If Dr. Husband gave consent (and thereby “caused”) the sterilization knowing that his wife did not want to have it or because of animus toward her (they were about to be separated and divorced, after all), there is the possibility of liability. (In some states a form of interspousal liability might complicate some of these claims—but that is a topic for another day.) He essentially took action for the purpose of wrongly causing the sterilization—which may be a battery (an intentional offensive or harmful touching). The legal rules around battery allow punitive damages as well as compensatory damages. In addition, many malpractice insurance policies provide limited coverage for intentional torts. To complicate matters further, it is not clear that Dr. Husband’s actions were related to his practice of medicine in any event (although Dr. Surgeon might claim that Dr. Husband’s expressed concern about his wife’s hypertension was enough to create a malpractice issue if Dr. Surgeon did not perform the verbally requested tubal ligation).
If, as we have speculated, Dr. Husband’s actions were motivated by improper personal considerations at the expense of a patient, he may also face medical board complaints from the patient. It is plausible that a state law makes it a criminal offense to wrongfully (or fraudulently) consent to medical treatment, particularly if related to reproductive capacity.
The hospital may face liability on several grounds, depending in part on the relationships between the hospital, Dr. Surgeon, and Dr. Husband. If Dr. Surgeon is an employee or agent of the hospital, he would be liable for his negligence. Even if Dr. Surgeon is technically an independent contractor, the failure of the hospital to offer more oversight concerning the surgical procedures in its facilities could give rise to a claim of negligence.
As to Dr. Husband, many of the same considerations are present. In addition, even if he is an agent of the hospital, the hospital may claim that his actions (especially if motivated by personal considerations) were a “lark of his own” and not in the course of his employment by the hospital.
Read about the clinical opportunity of informed consent
The clinical opportunity of informed consent
More than a technical legal doctrine, informed consent provides ObGyns an important opportunity for better communications with patients, and is a chance to create reasonable expectations and a more therapeutic relationship that involves the patient in care and decision making. It is likely that engaging the patient in good informed consent processes can set the stage for improved outcomes.
Interactive dialogue with the patient is one advised approach.10 This undertaking in part reflects that, as patients have more ready access to information in the digital age, they are positioned to play a more active role in health care decision making.
The benefits of informed consent are likely to be greatest if you view the process not as a technical legal requirement but as an excellent opportunity to engage the patient in her own care and treatment. Planning, intervention, and evaluation of care options as well as education regarding the medical problem at hand are integral to the informed consent process. And, of course, the right to consent is a “basic patient right” that in a sense guarantees that he/she has the right to make informed decisions regarding one’s care.6
Special considerations
Informed consent most often is associated with but not limited to surgical procedures (often performed with the use of surgical instruments and/or devices). It applies to diagnostic interventions as well as treatment. The more invasive or risky an intervention, the more important it is that the information is thorough.14,15
Pharmaceuticals have informed consent issues. The theory has been that pharmaceutical companies inform physicians of the risks and instructions for the use of pharmaceuticals and the physicians inform the patients. Indeed, traditionally pharmaceutical companies have gained immunity for “failure to warn” patients because the physicians were the “learned intermediaries” providing information to the public. Patient package inserts and pharmacists have taken over the informational role, but informed consent does apply to pharmaceuticals.
It is also worth noting that informed consent in any formal research study or the trial of new techniques, compounds, or devices requires a special process of approval by an institutional review board.
Set the stage for best outcomes
The main objective of informed consent is promoting the autonomy of your patient. That requires that she understand the risks, benefits, and alternatives associated with the procedure and the risks associated with a refusal of treatment. Done properly, this can result in your patient gaining confidence and trust in you as her provider.
Informed consent is a process that reflects our interactions with our patients. It is part of the broader commitment by the medical profession to “first do no harm.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Grady C. Enduring and emerging challenges of informed consent. N Engl J Med. 2015;372(22):855–862.
- Faden RR, Beauchamp TL. History and theory of informed consent. New York, New York: Oxford University Press; 1986.
- Paterick TJ, Carson G, Allen M, Paterick TE. Medical informed consent: general considerations for physicians. Mayo Clin Proc. 2008;83(3):313–319.
- American College of Obstetricians and Gynecologists Committee on Ethics. ACOG Committee Opinion No. 439: Informed consent (reaffirmed 2015). Obstet Gynecol. 2009;114(2 pt 1):401–408.
- Jonsen A, Siegler M, Winslade W. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. New York, New York: McGraw Hill; 2010.
- Menendez J. Informed consent: essential legal and ethical principles for nurses. JONAS Healthc Law Ethics Regul. 2013;15(4):140–144.
- Abram MB, Ballantine HT, Dunlop GR, et al; President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Making Health Care Decisions: The Ethical and Legal Implications of Informed Consent in the Patient-Practitioner Relationship. Volume One: Report. https://repository.library.georgetown.edu/bitstream/handle/10822/559354/making_health_care_decisions.pdf?sequence=1. Published October 1982. Accessed January 9, 2017.
- Dhar H, Dhar D. Informed consent in clinical practice and literature overview. Arch Gynecol Obstet. 2012;286(3):649–651.
- NE Schloendorff v Society of New York Hospital, 211 NY 125, 106 NE 93 1914.
- Avery D. Summary of informed consent and refusal. Am J Clinical Med. 2009;6(3):28–29.
- Pallett A, Phippen N, Miller C, Barnett J. Informed consent for hysterectomy: Does a video presentation improve patient comprehension? [poster 17F]. Obstet Gynecol. 2016;127(suppl):55S.
- Cainzos M, Gonzalez-Vinagre S. Informed consent in surgery. World J Surg. 2014;38(7):1587–1593.
- Weaver J. A problem with informed consent. J Am Coll Surg. 2009;209(2):286–287.
- Bunch W. Informed consent. Clin Orthop Relat Res. 2000;378:71–77.
- Peltier LF. Orthopedics: a history and iconography (Norman Orthopedic, No. 3). San Francisco, California: Jeremy Norman Co; 1993.
- Grady C. Enduring and emerging challenges of informed consent. N Engl J Med. 2015;372(22):855–862.
- Faden RR, Beauchamp TL. History and theory of informed consent. New York, New York: Oxford University Press; 1986.
- Paterick TJ, Carson G, Allen M, Paterick TE. Medical informed consent: general considerations for physicians. Mayo Clin Proc. 2008;83(3):313–319.
- American College of Obstetricians and Gynecologists Committee on Ethics. ACOG Committee Opinion No. 439: Informed consent (reaffirmed 2015). Obstet Gynecol. 2009;114(2 pt 1):401–408.
- Jonsen A, Siegler M, Winslade W. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. New York, New York: McGraw Hill; 2010.
- Menendez J. Informed consent: essential legal and ethical principles for nurses. JONAS Healthc Law Ethics Regul. 2013;15(4):140–144.
- Abram MB, Ballantine HT, Dunlop GR, et al; President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Making Health Care Decisions: The Ethical and Legal Implications of Informed Consent in the Patient-Practitioner Relationship. Volume One: Report. https://repository.library.georgetown.edu/bitstream/handle/10822/559354/making_health_care_decisions.pdf?sequence=1. Published October 1982. Accessed January 9, 2017.
- Dhar H, Dhar D. Informed consent in clinical practice and literature overview. Arch Gynecol Obstet. 2012;286(3):649–651.
- NE Schloendorff v Society of New York Hospital, 211 NY 125, 106 NE 93 1914.
- Avery D. Summary of informed consent and refusal. Am J Clinical Med. 2009;6(3):28–29.
- Pallett A, Phippen N, Miller C, Barnett J. Informed consent for hysterectomy: Does a video presentation improve patient comprehension? [poster 17F]. Obstet Gynecol. 2016;127(suppl):55S.
- Cainzos M, Gonzalez-Vinagre S. Informed consent in surgery. World J Surg. 2014;38(7):1587–1593.
- Weaver J. A problem with informed consent. J Am Coll Surg. 2009;209(2):286–287.
- Bunch W. Informed consent. Clin Orthop Relat Res. 2000;378:71–77.
- Peltier LF. Orthopedics: a history and iconography (Norman Orthopedic, No. 3). San Francisco, California: Jeremy Norman Co; 1993.
Patient with a breast mass: Why did she pursue litigation?
CASE: After routine mammography results, DCIS found
A 49-year-old woman (G2 P2002) with a history of fibrocystic breast disease presented with a left breast mass that she found a month ago on self-examination. The patient faithfully had obtained routine mammograms since age 40. This year, after reporting the mass and with spot films obtained as recommended by the radiologist, a new cluster of microcalcifications was identified on the report: “spot compression” assessment identified a 3-cm mass and noted “s/p breast augmentation.”
The radiologist interpreted the spot films to be benign. His report stated that “15% of breast cancers are not detected by mammogram and breast self-exam is recommended monthly from 40 years of age.”
The gynecologist recommended a 6-month follow up. When the patient complied, the radiologist’s report again noted calcifications believed to be nonmalignant. Six months later, the patient presented with bloody nipple discharge from her left breast with apparent “eczema-like” lesions on the areola. The patient noted that her “left implant felt different.”
The patient’s surgical history included breast augmentation “years ago.” Her family history was negative for breast cancer. Her medications included hormone therapy (conjugated estrogens 0.625 mg with medroxyprogesterone acetate 2.5 mg daily) for vaginal atrophy. Other medical conditions included irritable bowel syndrome (managed with diet), anxiety and mood swings (for which she was taking sertraline), decreased libido, and irregular vaginal bleeding (after the patient refused endometrial sampling, she was switched to oral contraceptives to address the problem). In addition, her hypertension was being treated with hydrochlorothiazide.
At the gynecologist’s suggestion, a dermatology consultation was obtained.
The dermatologist gave a diagnosis of Paget disease with high-grade ductal carcinoma-in-situ (DCIS). The interval from screening mammogram to DCIS diagnosis had been 8 months. The dermatologist referred the patient to a breast surgeon. A discussion ensued between the breast surgeon and the dermatologist concerning the difficulty of making a diagnosis of breast cancer in a woman with breast augmentation.
The patient underwent modified radical mastectomy, and histopathology revealed DCIS with clear margins; lymph nodes were negative.
The patient filed a malpractice suit against the gynecologist related to the delayed breast mass evaluation and management. She remained upset that when she called the gynecologist’s office to convey her concerns regarding the left nipple discharge and implant concerns, “she was blown off.” She felt there was a clear “failure to communicate on critical matters of her health.” She alleged that the gynecologist, not the dermatologist, should have referred her to a breast surgeon.
WHAT 'S THE VERDICT?
In the end, the patient decided not to pursue the lawsuit.
Related article:
Who is liable when a surgical error occurs?
Medical considerations
Breast cancer is the most common female malignancy, with 232,340 cases occurring annually in the United States. It is the second leading cause of cancer-related death in US women.1 For this case discussion, we review the role of breast cancer screening, including breast self-examination and mammography.
Is breast self-examination recommended?
Recently, medical care has evolved from “breast self-examination” (BSE) to “breast self-awareness.”2 The concept of BSE and concerns about it stem in part from “the Shanghai study.”3 In this prospective randomized trial, 266,064 female textile workers were randomly assigned to “rigorous and repetitive training in BSE” versus no instruction and no BSE performance. The former group had twice as many breast biopsies than the latter group (2,761 biopsies in the BSE group vs 1,505 in the control group). There was no difference in the number of breast cancers diagnosed among the groups—864 in the BSE group and 896 in the control group (relative risk [RR], 0.97; 95% confidence interval [CI], 0.88–1.06; P = .47). Other studies also support lack of efficacy regarding BSE.4
The potential for psychological harm, unnecessary biopsy, and additional imaging in association with false-positive findings is a concern2 (TABLE). The American College of Obstetricians and Gynecologists (ACOG) states, “breast self-examination may be appropriate for certain high-risk populations and for other women who chose to follow this approach.”2,5,6 The US Preventive Services Task Force (USPSTF) guidelines say that there is “insufficient evidence to assess risks vs benefits, including harms,” and recommends against teaching BSE.7 The American Cancer Society puts BSE in the “optional” category.2,8
Is there a middle of the road strategy? Perhaps. The concept of breast-awareness was developed so that women understand how their breasts look and feel.2,5 The concept does not advocate monthly BSE. The Mayo Clinic reported that, of 592 breast cancers, 57% were detected following abnormal screening mammography, 30% by BSE and 14% by clinical examination by a clinician. Furthermore, 38% of women with a palpable abnormality had a normal mammogram within the preceding 13 months.9 McBride and colleagues aptly addressed this: “Healthcare providers can educate their patients that breast awareness, in essence, is a two-step process. First, it requires that women be familiar with their breasts and aware of new changes and, second, have an understanding of the implications of these changes which includes informing their health care provider promptly.”10 The concept of “know what is normal for you” as conveyed by The Susan G. Komen Foundation succinctly encourages communication with patients.2,11
Mammography
The latest technique in mammography is digital or 3D mammography, also known as tomosynthesis. The technique is similar to 2D mammography with the addition of digital cameras. A study published in the radiology literature noted that the 2 methods were equivalent.12 One possible advantage of 3D mammography is that the 3D images are stored in computer files and are more easily incorporated into the electronic medical record.
What about mammography after breast augmentation?
While breast augmentation is not associated with an increase in breast cancer,13 mammography following breast augmentation can be more difficult to interpret and may result in a delay in diagnosis. In a prospective study of asymptomatic women who were diagnosed with breast cancer, 137 had augmentation and 685 did not. Miglioretti and colleagues noted that the sensitivity of screening mammography was lower in the augmentation cohort.14 To enhance accuracy, breast implant displacement views (in which the breast tissue is pulled forward and the implant is displaced posteriorly to improve visualization) have been recommended.15 A retrospective review provides data reporting no effect on interpretation of mammograms following augmentation.16 The American Cancer Society recommends the same screening for women with implants as without implants, starting at age 40 years.17
Paget disease of the breast
Paget disease of the breast was first described by Sir James Paget in 1874. He also defined Paget disease of extramammary tissue, bone, vulva, and penis. Paget disease of the breast is a rare type of cancer in which the skin and nipple are involved frequently in association with DCIS or invasive breast cancer. The skin has an eczema-like appearance. Characteristic Paget (malignant) cells are large with clear cytoplasm (clear halo) and eccentric, hyperchromatic nuclei throughout the dermis. Assessment includes mammography and biopsy with immunohistochemical staining. Treatment varies by case and can include lumpectomy or mastectomy and chemotherapy and/or radiation therapy. Medications, including tamoxifen and anastrazole, have been recommended. Prognosis depends on nodal involvement. The disease is more common in women older than age 50.18
Related article:
The medicolegal considerations of interacting with your patients online
Legal issues: What was the gynecologist’s obligation?
The question remains, did the gynecologist have an obligation to obtain diagnostic mammography and ultrasound of the breast? Would it have been prudent for immediate referral to a breast surgeon? These are critical questions.
Negligence and the standard of care
The malpractice lawsuit against this gynecologist is based on negligence. In essence, it is a claim that the management provided fell below a standard of care that would be given by a reasonably careful and prudent gynecologist under the circumstances. This generally means that the care was less than the profession itself would find acceptable. Here the claim is essentially a diagnostic error claim, a common basis of malpractice.19 The delay in diagnosing breast cancer is a leading cause of malpractice claims against gynecologists.20,21
It is axiomatic that not all bad outcomes are the result of error, and not all errors are a result of an unacceptable standard of care. It is only bad outcomes resulting from careless or negligent errors that give rise to malpractice. But malpractice claims are often filed without knowing whether or not there was negligence—and, as we will see, many of those claims are without merit.
Was there negligence?
Ordinarily the plaintiff/patient must demonstrate that the care by the physician fell below the standard of care and, as a result, the patient suffered an injury. Stated another way, the plaintiff must show that the physician’s actions were unreasonable given all of the circumstances. In this case, the plaintiff must demonstrate that the gynecologist’s care was not appropriate. Failure to refer to another physician or provide additional testing is likely to be the major claim for negligence or inappropriate care.
Did that negligence cause injury?
Even if the plaintiff can demonstrate that the care was negligent, to prevail the plaintiff must also demonstrate that that negligence caused the injury—and that might be difficult.
What injury was caused by the delay in discovering the cancer? It did not apparently lead to the patient’s death. Can it be proven that the delay clearly shortened the patient’s life expectancy or required additional expensive and painful treatment? That may be difficult to demonstrate.
Causation. The causation factor could appear in many cancer or similar medical cases. On one hand, causation is a critical matter, but on the other hand, delay in treating cancer might have a very adverse effect on patients.
In recent years, about half the states have solved this dilemma by recognizing the concept of “loss of chance.”22 Essentially, this means that the health care provider, by delaying treatment, diminished the possibility that the patient would survive or recover fully.
There are significant variations among states in the loss-of-chance concept, many being quite technical.22 Thus, it is possible that a delay that reduced the chance of recovery or survival could be the injury and causal connection between the injury and the negligence. Even in states that recognize the loss-of-chance concept, the patient still must prove loss of chance.
Lessons learned from this case study
- Breast self-awareness has replaced (substituted) breast self-examination
- ACOG recommends breast mammography beginning at age 40 years
- Breast augmentation affects mammographic interpretation
- Prehaps if better communication had been provided initially, the patient would not have sought legal counsel or filed a weak suit
Related article:
Is the smartphone recording while the patient is under anesthesia?
Is this a strong malpractice case?
In the case presented here, it is not clear that the patient could show a meaningful loss of chance. If there is a delay in the breast cancer diagnosis, tumor doubling time would be an issue. While it is impossible to assess growth rate when a breast cancer is in its preclinical microscopic stage, doubling time can be 100 to 200 days. Therefore, it would take 20 years for the tumor to reach a 1- to 2-cm diameter. A log-normal distribution has been suggested for determining tumor growth.23
Although the facts in this case are sketchy, this does not look like a strong malpractice case. Given the expense, difficulty, and length of time it takes to pursue a malpractice case (especially for someone battling cancer), an obvious question is: Why would a patient file a lawsuit in these circumstances? There is no single answer to that, but the hope of getting rich is unlikely a primary motivation. Ironically, many malpractice cases are filed in which there was no error (or at least no negligent error).24
The search for what really happened, or why the bad event happened, is key. In other circumstances, it may be a desire for revenge or to protect other patients from similar bad results. Studies repeatedly have shown a somewhat limited correlation between negligent error and the decision to file a malpractice claim.24–26 In this case, the patient’s sense of being “blown off” during a particularly difficult time may represent the reason why she filed a malpractice lawsuit. Communication gaffes and poor physician-patient relationships undoubtedly contribute to medical malpractice claims.27,28 Improving communication with patients probably improves care, but it also almost certainly reduces the risk of a malpractice claim.29
Why a lawyer would accept this case is also unclear, but that is an issue for another day. Also for another day is the issue of product liability concerning breast implants. Those legal issues and related liability, primarily directed to the manufacturers of the implants, are interesting topics. They are also complex and will be the subject of a future article.
Finally, the patient’s decision to not pursue her lawsuit does not come as a surprise. A relatively small percentage of malpractice claims result in any meaningful financial recovery for the plaintiff. Few cases go to trial, and of those that do result in a verdict, about 75% of the verdicts are in favor of the physician.25,30 Many cases just fade away, either because the plaintiff never pursues them or because they are dismissed by a court at an early stage. Nonetheless, for the physician, even winning a malpractice case is disruptive and difficult. So in addition to ensuring careful, quality, and up-to-date care, a physician should seek to maintain good relationships and communication with patients to reduce the probability of even weak lawsuits being filed.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
- Mark K, Temkin S, Terplan M. Breast self-awareness: the evidence behind the euphemism. Obstet Gynecol. 2014;123(4):734–745.
- Thomas D, Gao D, Self S, et al. Randomized trial of breast self-examination in Shanghai: methodology and preliminary results. J Natl Cancer Inst. 1997;89(5):355–365.
- Jones S. Regular self-examination or clinical examination for early detection of breast cancer. Int J Epidemiol. 2008;37(6):1219.
- ACOG Committee on Practice Bulletins–Gynecology. ACOG Practice Bulletin No. 122. American College of Obstetricians and Gynecologists website. http://www.acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Breast-Cancer-Screening. Published August 2011; reaffirmed 2014. Accessed November 10, 2016.
- ACOG Statement on breast cancer screening guidelines. American College of Obstetricians and Gynecologists website. http://www.acog.org/About-ACOG/News-Room/Statements/2016/ACOG-Statement-on-Breast-Cancer-Screening-Guidelines. Published January 11, 2016. Accessed November 10, 2016.
- Final Recommendation Statement: Breast Cancer: Screening. U.S. Preventive Services Task Force web site. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1. Published September 2016. Accessed November 10, 2016.
- American Cancer Society recommendations for early breast cancer detection in women without breast symptoms. American Cancer Society website. http://www.cancer.org/cancer/breastcancer/moreinformation/breastcancerearlydetection/breast-cancer-early-detection-acs-recs. Updated October 20, 2015. Accessed November 10, 2016.
- Mathis K, Hoskin T, Boughey J, et al. Palpable presentation of breast cancer persists in the era of screening mammography. J Am Coll Surg. 2010;210(3):314–318.
- MacBride M, Pruthi S, Bevers T. The evolution of breast self-examination to breast awareness. Breast J. 2012;18(6):641–643.
- Susan G. Komen Foundation. Breast self-awareness messages. http://ww5.komen.org/Breastcancer/Breastselfawareness.html. Accessed November 10, 2016.
- DelTurco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR. 2007;189(4):860–866.
- Susan G. Koman Foundation. Factors that do not increase breast cancer risk: Breast implants. https://ww5.komen.org/BreastCancer/FactorsThatDoNotIncreaseRisk.html. Updated October 28, 2016. Accessed November 10, 2016.
- Miglioretti D, Rutter, C, Geller B, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004;291(4):442–450.
- Eklund GW, Busby RC, Miller SH, Job JS. Improved imaging of the augmented breast. Am J Roentgenol. 1988;151(3):469–473.
- Kam K, Lee E, Pairwan S, et al. The effect of breast implants on mammogram outcomes. Am Surg. 2015;81(10):1053–1056.
- American Cancer Society. Mammograms and other imaging tests. http://www.cancer.org/acs/groups/cid/documents/webcontent/003178-pdf.pdf. Revised April 25, 2016. Accessed November 10, 2016.
- Dalberg K, Hellborg H, Warnberg F. Paget’s disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2008;111(2):313–319.
- Saber Tehrani A, Lee H, Mathews S, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- White AA, Pichert JW, Bledsoe SH, Irwin C, Entman SS. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt 1):1031–1038.
- Ward CJ, Green VL. Risk management and medico-legal issues in breast cancer. Clin Obstet Gynecol. 2016;59(2):439–446.
- Guest L, Schap D, Tran T. The “Loss of Chance” rule as a special category of damages in medical malpractice: a state-by-state analysis. J Legal Econ. 2015;21(2):53–107.
- Kuroishi T, Tominaga S, Morimoto T, et al. Tumor growth rate and prognosis of breast cancer mainly detected by mass screening. Jpn J Cancer Res. 1990;81(5):454–462.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence: results of the Harvard Medical Practice Study III. N Engl J Medicine. 1991;325(4):245–251.
- Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145(7):488–496.
- Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024–2033.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157–161.
- Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- Hickson GB, Jenkins AD. Identifying and addressing communication failures as a means of reducing unnecessary malpractice claims. NC Med J. 2007;68(5):362–364.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
CASE: After routine mammography results, DCIS found
A 49-year-old woman (G2 P2002) with a history of fibrocystic breast disease presented with a left breast mass that she found a month ago on self-examination. The patient faithfully had obtained routine mammograms since age 40. This year, after reporting the mass and with spot films obtained as recommended by the radiologist, a new cluster of microcalcifications was identified on the report: “spot compression” assessment identified a 3-cm mass and noted “s/p breast augmentation.”
The radiologist interpreted the spot films to be benign. His report stated that “15% of breast cancers are not detected by mammogram and breast self-exam is recommended monthly from 40 years of age.”
The gynecologist recommended a 6-month follow up. When the patient complied, the radiologist’s report again noted calcifications believed to be nonmalignant. Six months later, the patient presented with bloody nipple discharge from her left breast with apparent “eczema-like” lesions on the areola. The patient noted that her “left implant felt different.”
The patient’s surgical history included breast augmentation “years ago.” Her family history was negative for breast cancer. Her medications included hormone therapy (conjugated estrogens 0.625 mg with medroxyprogesterone acetate 2.5 mg daily) for vaginal atrophy. Other medical conditions included irritable bowel syndrome (managed with diet), anxiety and mood swings (for which she was taking sertraline), decreased libido, and irregular vaginal bleeding (after the patient refused endometrial sampling, she was switched to oral contraceptives to address the problem). In addition, her hypertension was being treated with hydrochlorothiazide.
At the gynecologist’s suggestion, a dermatology consultation was obtained.
The dermatologist gave a diagnosis of Paget disease with high-grade ductal carcinoma-in-situ (DCIS). The interval from screening mammogram to DCIS diagnosis had been 8 months. The dermatologist referred the patient to a breast surgeon. A discussion ensued between the breast surgeon and the dermatologist concerning the difficulty of making a diagnosis of breast cancer in a woman with breast augmentation.
The patient underwent modified radical mastectomy, and histopathology revealed DCIS with clear margins; lymph nodes were negative.
The patient filed a malpractice suit against the gynecologist related to the delayed breast mass evaluation and management. She remained upset that when she called the gynecologist’s office to convey her concerns regarding the left nipple discharge and implant concerns, “she was blown off.” She felt there was a clear “failure to communicate on critical matters of her health.” She alleged that the gynecologist, not the dermatologist, should have referred her to a breast surgeon.
WHAT 'S THE VERDICT?
In the end, the patient decided not to pursue the lawsuit.
Related article:
Who is liable when a surgical error occurs?
Medical considerations
Breast cancer is the most common female malignancy, with 232,340 cases occurring annually in the United States. It is the second leading cause of cancer-related death in US women.1 For this case discussion, we review the role of breast cancer screening, including breast self-examination and mammography.
Is breast self-examination recommended?
Recently, medical care has evolved from “breast self-examination” (BSE) to “breast self-awareness.”2 The concept of BSE and concerns about it stem in part from “the Shanghai study.”3 In this prospective randomized trial, 266,064 female textile workers were randomly assigned to “rigorous and repetitive training in BSE” versus no instruction and no BSE performance. The former group had twice as many breast biopsies than the latter group (2,761 biopsies in the BSE group vs 1,505 in the control group). There was no difference in the number of breast cancers diagnosed among the groups—864 in the BSE group and 896 in the control group (relative risk [RR], 0.97; 95% confidence interval [CI], 0.88–1.06; P = .47). Other studies also support lack of efficacy regarding BSE.4
The potential for psychological harm, unnecessary biopsy, and additional imaging in association with false-positive findings is a concern2 (TABLE). The American College of Obstetricians and Gynecologists (ACOG) states, “breast self-examination may be appropriate for certain high-risk populations and for other women who chose to follow this approach.”2,5,6 The US Preventive Services Task Force (USPSTF) guidelines say that there is “insufficient evidence to assess risks vs benefits, including harms,” and recommends against teaching BSE.7 The American Cancer Society puts BSE in the “optional” category.2,8
Is there a middle of the road strategy? Perhaps. The concept of breast-awareness was developed so that women understand how their breasts look and feel.2,5 The concept does not advocate monthly BSE. The Mayo Clinic reported that, of 592 breast cancers, 57% were detected following abnormal screening mammography, 30% by BSE and 14% by clinical examination by a clinician. Furthermore, 38% of women with a palpable abnormality had a normal mammogram within the preceding 13 months.9 McBride and colleagues aptly addressed this: “Healthcare providers can educate their patients that breast awareness, in essence, is a two-step process. First, it requires that women be familiar with their breasts and aware of new changes and, second, have an understanding of the implications of these changes which includes informing their health care provider promptly.”10 The concept of “know what is normal for you” as conveyed by The Susan G. Komen Foundation succinctly encourages communication with patients.2,11
Mammography
The latest technique in mammography is digital or 3D mammography, also known as tomosynthesis. The technique is similar to 2D mammography with the addition of digital cameras. A study published in the radiology literature noted that the 2 methods were equivalent.12 One possible advantage of 3D mammography is that the 3D images are stored in computer files and are more easily incorporated into the electronic medical record.
What about mammography after breast augmentation?
While breast augmentation is not associated with an increase in breast cancer,13 mammography following breast augmentation can be more difficult to interpret and may result in a delay in diagnosis. In a prospective study of asymptomatic women who were diagnosed with breast cancer, 137 had augmentation and 685 did not. Miglioretti and colleagues noted that the sensitivity of screening mammography was lower in the augmentation cohort.14 To enhance accuracy, breast implant displacement views (in which the breast tissue is pulled forward and the implant is displaced posteriorly to improve visualization) have been recommended.15 A retrospective review provides data reporting no effect on interpretation of mammograms following augmentation.16 The American Cancer Society recommends the same screening for women with implants as without implants, starting at age 40 years.17
Paget disease of the breast
Paget disease of the breast was first described by Sir James Paget in 1874. He also defined Paget disease of extramammary tissue, bone, vulva, and penis. Paget disease of the breast is a rare type of cancer in which the skin and nipple are involved frequently in association with DCIS or invasive breast cancer. The skin has an eczema-like appearance. Characteristic Paget (malignant) cells are large with clear cytoplasm (clear halo) and eccentric, hyperchromatic nuclei throughout the dermis. Assessment includes mammography and biopsy with immunohistochemical staining. Treatment varies by case and can include lumpectomy or mastectomy and chemotherapy and/or radiation therapy. Medications, including tamoxifen and anastrazole, have been recommended. Prognosis depends on nodal involvement. The disease is more common in women older than age 50.18
Related article:
The medicolegal considerations of interacting with your patients online
Legal issues: What was the gynecologist’s obligation?
The question remains, did the gynecologist have an obligation to obtain diagnostic mammography and ultrasound of the breast? Would it have been prudent for immediate referral to a breast surgeon? These are critical questions.
Negligence and the standard of care
The malpractice lawsuit against this gynecologist is based on negligence. In essence, it is a claim that the management provided fell below a standard of care that would be given by a reasonably careful and prudent gynecologist under the circumstances. This generally means that the care was less than the profession itself would find acceptable. Here the claim is essentially a diagnostic error claim, a common basis of malpractice.19 The delay in diagnosing breast cancer is a leading cause of malpractice claims against gynecologists.20,21
It is axiomatic that not all bad outcomes are the result of error, and not all errors are a result of an unacceptable standard of care. It is only bad outcomes resulting from careless or negligent errors that give rise to malpractice. But malpractice claims are often filed without knowing whether or not there was negligence—and, as we will see, many of those claims are without merit.
Was there negligence?
Ordinarily the plaintiff/patient must demonstrate that the care by the physician fell below the standard of care and, as a result, the patient suffered an injury. Stated another way, the plaintiff must show that the physician’s actions were unreasonable given all of the circumstances. In this case, the plaintiff must demonstrate that the gynecologist’s care was not appropriate. Failure to refer to another physician or provide additional testing is likely to be the major claim for negligence or inappropriate care.
Did that negligence cause injury?
Even if the plaintiff can demonstrate that the care was negligent, to prevail the plaintiff must also demonstrate that that negligence caused the injury—and that might be difficult.
What injury was caused by the delay in discovering the cancer? It did not apparently lead to the patient’s death. Can it be proven that the delay clearly shortened the patient’s life expectancy or required additional expensive and painful treatment? That may be difficult to demonstrate.
Causation. The causation factor could appear in many cancer or similar medical cases. On one hand, causation is a critical matter, but on the other hand, delay in treating cancer might have a very adverse effect on patients.
In recent years, about half the states have solved this dilemma by recognizing the concept of “loss of chance.”22 Essentially, this means that the health care provider, by delaying treatment, diminished the possibility that the patient would survive or recover fully.
There are significant variations among states in the loss-of-chance concept, many being quite technical.22 Thus, it is possible that a delay that reduced the chance of recovery or survival could be the injury and causal connection between the injury and the negligence. Even in states that recognize the loss-of-chance concept, the patient still must prove loss of chance.
Lessons learned from this case study
- Breast self-awareness has replaced (substituted) breast self-examination
- ACOG recommends breast mammography beginning at age 40 years
- Breast augmentation affects mammographic interpretation
- Prehaps if better communication had been provided initially, the patient would not have sought legal counsel or filed a weak suit
Related article:
Is the smartphone recording while the patient is under anesthesia?
Is this a strong malpractice case?
In the case presented here, it is not clear that the patient could show a meaningful loss of chance. If there is a delay in the breast cancer diagnosis, tumor doubling time would be an issue. While it is impossible to assess growth rate when a breast cancer is in its preclinical microscopic stage, doubling time can be 100 to 200 days. Therefore, it would take 20 years for the tumor to reach a 1- to 2-cm diameter. A log-normal distribution has been suggested for determining tumor growth.23
Although the facts in this case are sketchy, this does not look like a strong malpractice case. Given the expense, difficulty, and length of time it takes to pursue a malpractice case (especially for someone battling cancer), an obvious question is: Why would a patient file a lawsuit in these circumstances? There is no single answer to that, but the hope of getting rich is unlikely a primary motivation. Ironically, many malpractice cases are filed in which there was no error (or at least no negligent error).24
The search for what really happened, or why the bad event happened, is key. In other circumstances, it may be a desire for revenge or to protect other patients from similar bad results. Studies repeatedly have shown a somewhat limited correlation between negligent error and the decision to file a malpractice claim.24–26 In this case, the patient’s sense of being “blown off” during a particularly difficult time may represent the reason why she filed a malpractice lawsuit. Communication gaffes and poor physician-patient relationships undoubtedly contribute to medical malpractice claims.27,28 Improving communication with patients probably improves care, but it also almost certainly reduces the risk of a malpractice claim.29
Why a lawyer would accept this case is also unclear, but that is an issue for another day. Also for another day is the issue of product liability concerning breast implants. Those legal issues and related liability, primarily directed to the manufacturers of the implants, are interesting topics. They are also complex and will be the subject of a future article.
Finally, the patient’s decision to not pursue her lawsuit does not come as a surprise. A relatively small percentage of malpractice claims result in any meaningful financial recovery for the plaintiff. Few cases go to trial, and of those that do result in a verdict, about 75% of the verdicts are in favor of the physician.25,30 Many cases just fade away, either because the plaintiff never pursues them or because they are dismissed by a court at an early stage. Nonetheless, for the physician, even winning a malpractice case is disruptive and difficult. So in addition to ensuring careful, quality, and up-to-date care, a physician should seek to maintain good relationships and communication with patients to reduce the probability of even weak lawsuits being filed.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE: After routine mammography results, DCIS found
A 49-year-old woman (G2 P2002) with a history of fibrocystic breast disease presented with a left breast mass that she found a month ago on self-examination. The patient faithfully had obtained routine mammograms since age 40. This year, after reporting the mass and with spot films obtained as recommended by the radiologist, a new cluster of microcalcifications was identified on the report: “spot compression” assessment identified a 3-cm mass and noted “s/p breast augmentation.”
The radiologist interpreted the spot films to be benign. His report stated that “15% of breast cancers are not detected by mammogram and breast self-exam is recommended monthly from 40 years of age.”
The gynecologist recommended a 6-month follow up. When the patient complied, the radiologist’s report again noted calcifications believed to be nonmalignant. Six months later, the patient presented with bloody nipple discharge from her left breast with apparent “eczema-like” lesions on the areola. The patient noted that her “left implant felt different.”
The patient’s surgical history included breast augmentation “years ago.” Her family history was negative for breast cancer. Her medications included hormone therapy (conjugated estrogens 0.625 mg with medroxyprogesterone acetate 2.5 mg daily) for vaginal atrophy. Other medical conditions included irritable bowel syndrome (managed with diet), anxiety and mood swings (for which she was taking sertraline), decreased libido, and irregular vaginal bleeding (after the patient refused endometrial sampling, she was switched to oral contraceptives to address the problem). In addition, her hypertension was being treated with hydrochlorothiazide.
At the gynecologist’s suggestion, a dermatology consultation was obtained.
The dermatologist gave a diagnosis of Paget disease with high-grade ductal carcinoma-in-situ (DCIS). The interval from screening mammogram to DCIS diagnosis had been 8 months. The dermatologist referred the patient to a breast surgeon. A discussion ensued between the breast surgeon and the dermatologist concerning the difficulty of making a diagnosis of breast cancer in a woman with breast augmentation.
The patient underwent modified radical mastectomy, and histopathology revealed DCIS with clear margins; lymph nodes were negative.
The patient filed a malpractice suit against the gynecologist related to the delayed breast mass evaluation and management. She remained upset that when she called the gynecologist’s office to convey her concerns regarding the left nipple discharge and implant concerns, “she was blown off.” She felt there was a clear “failure to communicate on critical matters of her health.” She alleged that the gynecologist, not the dermatologist, should have referred her to a breast surgeon.
WHAT 'S THE VERDICT?
In the end, the patient decided not to pursue the lawsuit.
Related article:
Who is liable when a surgical error occurs?
Medical considerations
Breast cancer is the most common female malignancy, with 232,340 cases occurring annually in the United States. It is the second leading cause of cancer-related death in US women.1 For this case discussion, we review the role of breast cancer screening, including breast self-examination and mammography.
Is breast self-examination recommended?
Recently, medical care has evolved from “breast self-examination” (BSE) to “breast self-awareness.”2 The concept of BSE and concerns about it stem in part from “the Shanghai study.”3 In this prospective randomized trial, 266,064 female textile workers were randomly assigned to “rigorous and repetitive training in BSE” versus no instruction and no BSE performance. The former group had twice as many breast biopsies than the latter group (2,761 biopsies in the BSE group vs 1,505 in the control group). There was no difference in the number of breast cancers diagnosed among the groups—864 in the BSE group and 896 in the control group (relative risk [RR], 0.97; 95% confidence interval [CI], 0.88–1.06; P = .47). Other studies also support lack of efficacy regarding BSE.4
The potential for psychological harm, unnecessary biopsy, and additional imaging in association with false-positive findings is a concern2 (TABLE). The American College of Obstetricians and Gynecologists (ACOG) states, “breast self-examination may be appropriate for certain high-risk populations and for other women who chose to follow this approach.”2,5,6 The US Preventive Services Task Force (USPSTF) guidelines say that there is “insufficient evidence to assess risks vs benefits, including harms,” and recommends against teaching BSE.7 The American Cancer Society puts BSE in the “optional” category.2,8
Is there a middle of the road strategy? Perhaps. The concept of breast-awareness was developed so that women understand how their breasts look and feel.2,5 The concept does not advocate monthly BSE. The Mayo Clinic reported that, of 592 breast cancers, 57% were detected following abnormal screening mammography, 30% by BSE and 14% by clinical examination by a clinician. Furthermore, 38% of women with a palpable abnormality had a normal mammogram within the preceding 13 months.9 McBride and colleagues aptly addressed this: “Healthcare providers can educate their patients that breast awareness, in essence, is a two-step process. First, it requires that women be familiar with their breasts and aware of new changes and, second, have an understanding of the implications of these changes which includes informing their health care provider promptly.”10 The concept of “know what is normal for you” as conveyed by The Susan G. Komen Foundation succinctly encourages communication with patients.2,11
Mammography
The latest technique in mammography is digital or 3D mammography, also known as tomosynthesis. The technique is similar to 2D mammography with the addition of digital cameras. A study published in the radiology literature noted that the 2 methods were equivalent.12 One possible advantage of 3D mammography is that the 3D images are stored in computer files and are more easily incorporated into the electronic medical record.
What about mammography after breast augmentation?
While breast augmentation is not associated with an increase in breast cancer,13 mammography following breast augmentation can be more difficult to interpret and may result in a delay in diagnosis. In a prospective study of asymptomatic women who were diagnosed with breast cancer, 137 had augmentation and 685 did not. Miglioretti and colleagues noted that the sensitivity of screening mammography was lower in the augmentation cohort.14 To enhance accuracy, breast implant displacement views (in which the breast tissue is pulled forward and the implant is displaced posteriorly to improve visualization) have been recommended.15 A retrospective review provides data reporting no effect on interpretation of mammograms following augmentation.16 The American Cancer Society recommends the same screening for women with implants as without implants, starting at age 40 years.17
Paget disease of the breast
Paget disease of the breast was first described by Sir James Paget in 1874. He also defined Paget disease of extramammary tissue, bone, vulva, and penis. Paget disease of the breast is a rare type of cancer in which the skin and nipple are involved frequently in association with DCIS or invasive breast cancer. The skin has an eczema-like appearance. Characteristic Paget (malignant) cells are large with clear cytoplasm (clear halo) and eccentric, hyperchromatic nuclei throughout the dermis. Assessment includes mammography and biopsy with immunohistochemical staining. Treatment varies by case and can include lumpectomy or mastectomy and chemotherapy and/or radiation therapy. Medications, including tamoxifen and anastrazole, have been recommended. Prognosis depends on nodal involvement. The disease is more common in women older than age 50.18
Related article:
The medicolegal considerations of interacting with your patients online
Legal issues: What was the gynecologist’s obligation?
The question remains, did the gynecologist have an obligation to obtain diagnostic mammography and ultrasound of the breast? Would it have been prudent for immediate referral to a breast surgeon? These are critical questions.
Negligence and the standard of care
The malpractice lawsuit against this gynecologist is based on negligence. In essence, it is a claim that the management provided fell below a standard of care that would be given by a reasonably careful and prudent gynecologist under the circumstances. This generally means that the care was less than the profession itself would find acceptable. Here the claim is essentially a diagnostic error claim, a common basis of malpractice.19 The delay in diagnosing breast cancer is a leading cause of malpractice claims against gynecologists.20,21
It is axiomatic that not all bad outcomes are the result of error, and not all errors are a result of an unacceptable standard of care. It is only bad outcomes resulting from careless or negligent errors that give rise to malpractice. But malpractice claims are often filed without knowing whether or not there was negligence—and, as we will see, many of those claims are without merit.
Was there negligence?
Ordinarily the plaintiff/patient must demonstrate that the care by the physician fell below the standard of care and, as a result, the patient suffered an injury. Stated another way, the plaintiff must show that the physician’s actions were unreasonable given all of the circumstances. In this case, the plaintiff must demonstrate that the gynecologist’s care was not appropriate. Failure to refer to another physician or provide additional testing is likely to be the major claim for negligence or inappropriate care.
Did that negligence cause injury?
Even if the plaintiff can demonstrate that the care was negligent, to prevail the plaintiff must also demonstrate that that negligence caused the injury—and that might be difficult.
What injury was caused by the delay in discovering the cancer? It did not apparently lead to the patient’s death. Can it be proven that the delay clearly shortened the patient’s life expectancy or required additional expensive and painful treatment? That may be difficult to demonstrate.
Causation. The causation factor could appear in many cancer or similar medical cases. On one hand, causation is a critical matter, but on the other hand, delay in treating cancer might have a very adverse effect on patients.
In recent years, about half the states have solved this dilemma by recognizing the concept of “loss of chance.”22 Essentially, this means that the health care provider, by delaying treatment, diminished the possibility that the patient would survive or recover fully.
There are significant variations among states in the loss-of-chance concept, many being quite technical.22 Thus, it is possible that a delay that reduced the chance of recovery or survival could be the injury and causal connection between the injury and the negligence. Even in states that recognize the loss-of-chance concept, the patient still must prove loss of chance.
Lessons learned from this case study
- Breast self-awareness has replaced (substituted) breast self-examination
- ACOG recommends breast mammography beginning at age 40 years
- Breast augmentation affects mammographic interpretation
- Prehaps if better communication had been provided initially, the patient would not have sought legal counsel or filed a weak suit
Related article:
Is the smartphone recording while the patient is under anesthesia?
Is this a strong malpractice case?
In the case presented here, it is not clear that the patient could show a meaningful loss of chance. If there is a delay in the breast cancer diagnosis, tumor doubling time would be an issue. While it is impossible to assess growth rate when a breast cancer is in its preclinical microscopic stage, doubling time can be 100 to 200 days. Therefore, it would take 20 years for the tumor to reach a 1- to 2-cm diameter. A log-normal distribution has been suggested for determining tumor growth.23
Although the facts in this case are sketchy, this does not look like a strong malpractice case. Given the expense, difficulty, and length of time it takes to pursue a malpractice case (especially for someone battling cancer), an obvious question is: Why would a patient file a lawsuit in these circumstances? There is no single answer to that, but the hope of getting rich is unlikely a primary motivation. Ironically, many malpractice cases are filed in which there was no error (or at least no negligent error).24
The search for what really happened, or why the bad event happened, is key. In other circumstances, it may be a desire for revenge or to protect other patients from similar bad results. Studies repeatedly have shown a somewhat limited correlation between negligent error and the decision to file a malpractice claim.24–26 In this case, the patient’s sense of being “blown off” during a particularly difficult time may represent the reason why she filed a malpractice lawsuit. Communication gaffes and poor physician-patient relationships undoubtedly contribute to medical malpractice claims.27,28 Improving communication with patients probably improves care, but it also almost certainly reduces the risk of a malpractice claim.29
Why a lawyer would accept this case is also unclear, but that is an issue for another day. Also for another day is the issue of product liability concerning breast implants. Those legal issues and related liability, primarily directed to the manufacturers of the implants, are interesting topics. They are also complex and will be the subject of a future article.
Finally, the patient’s decision to not pursue her lawsuit does not come as a surprise. A relatively small percentage of malpractice claims result in any meaningful financial recovery for the plaintiff. Few cases go to trial, and of those that do result in a verdict, about 75% of the verdicts are in favor of the physician.25,30 Many cases just fade away, either because the plaintiff never pursues them or because they are dismissed by a court at an early stage. Nonetheless, for the physician, even winning a malpractice case is disruptive and difficult. So in addition to ensuring careful, quality, and up-to-date care, a physician should seek to maintain good relationships and communication with patients to reduce the probability of even weak lawsuits being filed.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
- Mark K, Temkin S, Terplan M. Breast self-awareness: the evidence behind the euphemism. Obstet Gynecol. 2014;123(4):734–745.
- Thomas D, Gao D, Self S, et al. Randomized trial of breast self-examination in Shanghai: methodology and preliminary results. J Natl Cancer Inst. 1997;89(5):355–365.
- Jones S. Regular self-examination or clinical examination for early detection of breast cancer. Int J Epidemiol. 2008;37(6):1219.
- ACOG Committee on Practice Bulletins–Gynecology. ACOG Practice Bulletin No. 122. American College of Obstetricians and Gynecologists website. http://www.acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Breast-Cancer-Screening. Published August 2011; reaffirmed 2014. Accessed November 10, 2016.
- ACOG Statement on breast cancer screening guidelines. American College of Obstetricians and Gynecologists website. http://www.acog.org/About-ACOG/News-Room/Statements/2016/ACOG-Statement-on-Breast-Cancer-Screening-Guidelines. Published January 11, 2016. Accessed November 10, 2016.
- Final Recommendation Statement: Breast Cancer: Screening. U.S. Preventive Services Task Force web site. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1. Published September 2016. Accessed November 10, 2016.
- American Cancer Society recommendations for early breast cancer detection in women without breast symptoms. American Cancer Society website. http://www.cancer.org/cancer/breastcancer/moreinformation/breastcancerearlydetection/breast-cancer-early-detection-acs-recs. Updated October 20, 2015. Accessed November 10, 2016.
- Mathis K, Hoskin T, Boughey J, et al. Palpable presentation of breast cancer persists in the era of screening mammography. J Am Coll Surg. 2010;210(3):314–318.
- MacBride M, Pruthi S, Bevers T. The evolution of breast self-examination to breast awareness. Breast J. 2012;18(6):641–643.
- Susan G. Komen Foundation. Breast self-awareness messages. http://ww5.komen.org/Breastcancer/Breastselfawareness.html. Accessed November 10, 2016.
- DelTurco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR. 2007;189(4):860–866.
- Susan G. Koman Foundation. Factors that do not increase breast cancer risk: Breast implants. https://ww5.komen.org/BreastCancer/FactorsThatDoNotIncreaseRisk.html. Updated October 28, 2016. Accessed November 10, 2016.
- Miglioretti D, Rutter, C, Geller B, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004;291(4):442–450.
- Eklund GW, Busby RC, Miller SH, Job JS. Improved imaging of the augmented breast. Am J Roentgenol. 1988;151(3):469–473.
- Kam K, Lee E, Pairwan S, et al. The effect of breast implants on mammogram outcomes. Am Surg. 2015;81(10):1053–1056.
- American Cancer Society. Mammograms and other imaging tests. http://www.cancer.org/acs/groups/cid/documents/webcontent/003178-pdf.pdf. Revised April 25, 2016. Accessed November 10, 2016.
- Dalberg K, Hellborg H, Warnberg F. Paget’s disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2008;111(2):313–319.
- Saber Tehrani A, Lee H, Mathews S, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- White AA, Pichert JW, Bledsoe SH, Irwin C, Entman SS. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt 1):1031–1038.
- Ward CJ, Green VL. Risk management and medico-legal issues in breast cancer. Clin Obstet Gynecol. 2016;59(2):439–446.
- Guest L, Schap D, Tran T. The “Loss of Chance” rule as a special category of damages in medical malpractice: a state-by-state analysis. J Legal Econ. 2015;21(2):53–107.
- Kuroishi T, Tominaga S, Morimoto T, et al. Tumor growth rate and prognosis of breast cancer mainly detected by mass screening. Jpn J Cancer Res. 1990;81(5):454–462.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence: results of the Harvard Medical Practice Study III. N Engl J Medicine. 1991;325(4):245–251.
- Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145(7):488–496.
- Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024–2033.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157–161.
- Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- Hickson GB, Jenkins AD. Identifying and addressing communication failures as a means of reducing unnecessary malpractice claims. NC Med J. 2007;68(5):362–364.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
- Mark K, Temkin S, Terplan M. Breast self-awareness: the evidence behind the euphemism. Obstet Gynecol. 2014;123(4):734–745.
- Thomas D, Gao D, Self S, et al. Randomized trial of breast self-examination in Shanghai: methodology and preliminary results. J Natl Cancer Inst. 1997;89(5):355–365.
- Jones S. Regular self-examination or clinical examination for early detection of breast cancer. Int J Epidemiol. 2008;37(6):1219.
- ACOG Committee on Practice Bulletins–Gynecology. ACOG Practice Bulletin No. 122. American College of Obstetricians and Gynecologists website. http://www.acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Breast-Cancer-Screening. Published August 2011; reaffirmed 2014. Accessed November 10, 2016.
- ACOG Statement on breast cancer screening guidelines. American College of Obstetricians and Gynecologists website. http://www.acog.org/About-ACOG/News-Room/Statements/2016/ACOG-Statement-on-Breast-Cancer-Screening-Guidelines. Published January 11, 2016. Accessed November 10, 2016.
- Final Recommendation Statement: Breast Cancer: Screening. U.S. Preventive Services Task Force web site. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1. Published September 2016. Accessed November 10, 2016.
- American Cancer Society recommendations for early breast cancer detection in women without breast symptoms. American Cancer Society website. http://www.cancer.org/cancer/breastcancer/moreinformation/breastcancerearlydetection/breast-cancer-early-detection-acs-recs. Updated October 20, 2015. Accessed November 10, 2016.
- Mathis K, Hoskin T, Boughey J, et al. Palpable presentation of breast cancer persists in the era of screening mammography. J Am Coll Surg. 2010;210(3):314–318.
- MacBride M, Pruthi S, Bevers T. The evolution of breast self-examination to breast awareness. Breast J. 2012;18(6):641–643.
- Susan G. Komen Foundation. Breast self-awareness messages. http://ww5.komen.org/Breastcancer/Breastselfawareness.html. Accessed November 10, 2016.
- DelTurco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR. 2007;189(4):860–866.
- Susan G. Koman Foundation. Factors that do not increase breast cancer risk: Breast implants. https://ww5.komen.org/BreastCancer/FactorsThatDoNotIncreaseRisk.html. Updated October 28, 2016. Accessed November 10, 2016.
- Miglioretti D, Rutter, C, Geller B, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004;291(4):442–450.
- Eklund GW, Busby RC, Miller SH, Job JS. Improved imaging of the augmented breast. Am J Roentgenol. 1988;151(3):469–473.
- Kam K, Lee E, Pairwan S, et al. The effect of breast implants on mammogram outcomes. Am Surg. 2015;81(10):1053–1056.
- American Cancer Society. Mammograms and other imaging tests. http://www.cancer.org/acs/groups/cid/documents/webcontent/003178-pdf.pdf. Revised April 25, 2016. Accessed November 10, 2016.
- Dalberg K, Hellborg H, Warnberg F. Paget’s disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2008;111(2):313–319.
- Saber Tehrani A, Lee H, Mathews S, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- White AA, Pichert JW, Bledsoe SH, Irwin C, Entman SS. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt 1):1031–1038.
- Ward CJ, Green VL. Risk management and medico-legal issues in breast cancer. Clin Obstet Gynecol. 2016;59(2):439–446.
- Guest L, Schap D, Tran T. The “Loss of Chance” rule as a special category of damages in medical malpractice: a state-by-state analysis. J Legal Econ. 2015;21(2):53–107.
- Kuroishi T, Tominaga S, Morimoto T, et al. Tumor growth rate and prognosis of breast cancer mainly detected by mass screening. Jpn J Cancer Res. 1990;81(5):454–462.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence: results of the Harvard Medical Practice Study III. N Engl J Medicine. 1991;325(4):245–251.
- Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145(7):488–496.
- Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024–2033.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157–161.
- Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- Hickson GB, Jenkins AD. Identifying and addressing communication failures as a means of reducing unnecessary malpractice claims. NC Med J. 2007;68(5):362–364.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
4 Supreme Court decisions important to ObGyns from the 2015−2016 term
Each year, the decisions of the Supreme Court have a significant impact on ObGyn practice. During the 2015–2016 term, which ended in June, the Court issued important rulings on abortion facilities, Affordable Care Act (ACA) contraception coverage, health care False Claims Act (FCA) liability, and state health care data collection. The American Medical Association (AMA), the Association of American Medical Colleges (AAMC), the American College of Obstetricians and Gynecologists (ACOG), and other organizations that represent health care professionals play an important role in health-related Supreme Court cases. For example, amicus curiae (“friend of the Court”) briefs are filed not by parties to a case but by organizations that have a special insight into or interest in a case. Although the extent to which amicus briefs influence cases is often unclear, organization representatives think their briefs make a difference, and briefs undoubtedly do in some cases.
The 2016 presidential election will determine the Supreme Court make-up for the next term, but in this article we consider recent cases that affect ObGyns’ practice in particular. We start with the cases in which professional organizations filed amicus briefs and then turn to other notable cases.
1. Abortion access in Texas and other states
The most important ObGyn case of the 2015–2016 term was Whole Woman’s Health v Hellerstedt.1
At stake. Texas adopted a statute requiring 1) that physicians who perform abortions have admitting privileges at a hospital within 30 miles of the clinic and 2) that abortion clinics meet the state’s standards for ambulatory surgical centers. The current law, upheld by the Court some years ago, is that state laws affecting abortion are unconstitutional if they “unduly burden” the right to abortion. By undue burden, the Court meant, “Regulations that have the purpose or effect of presenting a substantial obstacle to a woman seeking an abortion impose an undue burden on the right.” The question in the Texas case was whether the statute’s 2 requirements were undue.
ACOG, AMA, and other groups filed a brief stating that the Texas law did not promote the welfare of women but instead was unnecessary and not “supported by accepted medical practice or scientific evidence.”2 In another brief the Society of Hospital Medicine and the Society of ObGyn Hospitalists also indicated that having admitting privileges is appropriate only for physicians who regularly admit patients to a hospital.3
A brief filed by the American Association of Pro-Life Obstetricians and Gynecologists and several other organizations argued the other side: “The surgical center and admitting privileges requirements imposed by the Act reflect the professional standard of practice for outpatient gynecological and similar surgery.”4
Final ruling. In a 5−3 decision, the Court struck down the Texas law for providing little or no health benefits while significantly burdening abortion facility access. Many clinics had closed or were in plans to because of the difficulty and expense of complying with the law. This case has national implications. Similar laws, either in place or being considered in other states, will almost certainly be ruled unconstitutional.
2. Contraceptive coverage
The case of Zubik v Burwell was closely watched this past year.
At stake. Under the ACA, a nonprofit religious organization may certify its objection to its insurance plan’s contraception coverage, at which point other arrangements are made to provide contraceptive coverage through the same plan. Religious organizations objected to the certification requirement.
A brief filed by ACOG, Physicians for Reproductive Health, and other groups emphasized the importance of providing contraceptives and contraceptive counseling as part of regular health care and suggested that the current accommodation for religious organizations is appropriate.5
After hearing the formal oral arguments, the Court asked for additional briefs on “whether contraceptive coverage could be provided to petitioners’ employees, through petitioners’ insurance companies, without any such notice from petitioners.”6
Final ruling. The parties agreed such a system would resolve the issue, so the Court sent the case back to the lower court to work out the details. In effect, the case was mediated—an unusual if not unique action for the Court. The resolution probably will achieve what the briefs sought—access to contraceptives and continuity of care.
3. Fraud and abuse litigation
The FCA, which provides for triple damages (3 times actual damages) and stiff civil penalties for anyone who presents the federal government (Medicare, Medicaid) with false claims for goods or services, is a major means of uncovering and punishing health care fraud and abuse. In health care, this law has been used to prosecute cases involving services paid for but not provided, unnecessary services, and off-label pharmaceutical promotion.
An important part of the FCA is that it allows a private intervenor (whistleblower) to initiate an action against a health care provider. The government may then take up the case. If not, the intervenor may pursue it; the incentive is 15% to 30% of the damages the government is awarded.
At stake. The Court was asked if “implied certification” applies to FCA cases.7 Implied certification means that requesting a payment from Medicare or Medicaid implies that the provider is not knowingly withholding information material to the government’s decision to pay the claim. In separately filed briefs, AMA et al8 and American Hospital Association (AHA) et al9 argued that applying implied certification to FCA cases would expand FCA litigation (particularly by intervenors), which is already expensive for health care institutions.
Final ruling. The Court unanimously adopted implied certification but noted that nondisclosure of information must be shown to be a material misrepresentation rather than a trivial regulatory or contractual violation. Furthermore, the Court emphasized that the basis for a claim must be an allegation of fraud, not of malpractice. These findings, which certainly are not what the health care organizations had hoped for, likely will lead to an increase in FCA cases.
4. Collection of state health care data
In Vermont, and about 20 other states that collect data on health care utilization and costs, health insurers and other entities are required to submit detailed reports about health care claims.10 Some insurers objected to this requirement.
At stake. An AHA–AAMC brief noted the importance of health care data and of Vermont’s collecting these data as contributing to better, more efficient health care delivery.11 Another brief, filed by AMA and the Vermont Medical Society, presented more legal or statutory arguments.12
Final ruling. The Court held that the Vermont plan and similar plans violate the federal Employee Retirement Income Security Act of 1974. As health insurance companies and other entities already provide detailed utilization and cost data to the federal government, producing up to 50 additional reports for state governments would be burdensome. Any state that wants the information, the Court said, should obtain it from the federal government.
More notable 2015-2016 Supreme Court decisions.
The Court:
- permitted limited consideration of race in university admissions. ACOG, AAMC, and AMA with many other groups filed an amicus brief supporting medical school and university affirmative action programs.1
- held that a state must give full faith and credit to the adoption orders of the courts of other states (this case involved an LGBT couple).2
- held that states may require (without a search warrant) a breathalyzer test, but not a blood test, for a driver suspected of drinking.3
- narrowed the ability of the federal government to seize or restrain (before trial) the assets of a person charged with criminal health care offenses.4
- temporarily stayed the August 2016 US Department of Education order to schools to allow transgender students to use the facilities in which they feel "most comfortable." The Court likely will take up this case very soon.5
- Fisher v University of Texas at Austin et al, No. 14-981 (2016). https://www.supremecourt.gov/opinions/15pdf/14-981_4g15.pdf. Accessed August 30, 2016.
- V.L. v E.L. et al, No. 15-648 (2016). https://www.supremecourt.gov/opinions/15pdf/15-648_d18e.pdf. Accessed August 30, 2016.
- Birchfield v North Dakota, No. 14-1468 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1468_8n59.pdf. Accessed August 30, 2016.
- Luis v United States, No. 14-419 (2016). https://www.supremecourt.gov/opinions/15pdf/14-419_nmip.pdf. Accessed August 30, 2016.
- Gloucester County School Board v G.G., by his next friend and mother, Deidre Grimm, No. 16A52 (2016). https://www.supremecourt.gov/opinions/15pdf/16a52_8759.pdf. Accessed August 30, 2016.
What’s to come
The Court’s recent decisions on access to abortion services and contraceptives were good for patients of ObGyns, but its decisions on health care FCA liability and state health care data collection were, arguably, not as good for ObGyn business practices.
The Court itself had an unusual year. Justice Scalia died in February, and Congress’s inaction on seating a replacement meant that most of the term’s cases were decided by an 8-member Court. Nevertheless, the Court was deadlocked 4−4 on only 4 of the 80 cases it heard. In addition, it was relatively agreed on outcomes; in only about one-third of cases were there more than 2 justices disagreeing with the outcome.
It is unlikely that a replacement for Justice Scalia will be confirmed before the Court begins its new term in October. The need to replace Justice Scalia and the potential turnover of other Court members—Justice Ginsburg is 83, Justice Kennedy is 80, and Justice Breyer is 78—are reminders of the importance of this year’s presidential election. In the meantime, the Court is accepting the cases that will make up the coming term’s docket, and ObGyns undoubtedly will play a role in cases that involve health care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). https://www.supremecourt.gov/opinions/15pdf/15-274_new_e18f.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, American Medical Association, American Academy of Family Physicians, American Osteopathic Association, and American Academy of Pediatrics in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/ACOG-WilmerHale.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by Society of Hospital Medicine and Society of Ob/Gyn Hospitalists in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/Society-of-Hospital-Medicine-Crowell.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Association of Pro-Life Obstetricians and Gynecologists, American College of Pediatricians, Christian Medical & Dental Association, Catholic Medical Association, and Physicians for Life in support of respondents. Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al. http://www.scotusblog.com/wp-content/uploads/2016/02/15-274-bsac-American-Association-of-Pro-Life-Obstetricians-and-Gynecolog....pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, Physicians for Reproductive Health, American Academy of Family Physicians, American Nurses Association, et al in support of the government and affirmance. Zubik et al v Burwell, Secretary of Health and Human Services, et al, Nos. 14-1418, 14-1458, 14-1505, 15-35, 15-105, 15-119, and 15-191. http://www.scotusblog.com/wp-content/uploads/2016/02/Docfoc.com-Amicus-Brief-Zubik-v.-Burwell.pdf. Accessed August 30, 2016.
- Zubik et al v Burwell, Secretary of Health and Human Services, et al, No. 14-1418 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1418_8758.pdf. Accessed August 30, 2016.
- Universal Health Services, Inc v United States et al ex rel. Escobar et al, No. 15-7 (2016). https://www.supremecourt.gov/opinions/15pdf/15-7_a074.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association, National Association of Chain Drug Stores, National Association of Manufacturers, American Tort Reform Association and NFIB Small Business Legal Center in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7-tsac-American-Medical-Association.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association, Federation of American Hospitals, and Association of American Medical Colleges in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7tsacAHAFAHAAMC.pdf. Accessed August 30, 2016.
- Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). https://www.supremecourt.gov/opinions/15pdf/14-181_5426.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association and Association of American Medical Colleges in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/150904-amicus-gobeille-liberty.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association and Vermont Medical Society in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/VHCURES-Amicus-Brief-of-American-Medical-Association.pdf. Accessed August 30, 2016.
Each year, the decisions of the Supreme Court have a significant impact on ObGyn practice. During the 2015–2016 term, which ended in June, the Court issued important rulings on abortion facilities, Affordable Care Act (ACA) contraception coverage, health care False Claims Act (FCA) liability, and state health care data collection. The American Medical Association (AMA), the Association of American Medical Colleges (AAMC), the American College of Obstetricians and Gynecologists (ACOG), and other organizations that represent health care professionals play an important role in health-related Supreme Court cases. For example, amicus curiae (“friend of the Court”) briefs are filed not by parties to a case but by organizations that have a special insight into or interest in a case. Although the extent to which amicus briefs influence cases is often unclear, organization representatives think their briefs make a difference, and briefs undoubtedly do in some cases.
The 2016 presidential election will determine the Supreme Court make-up for the next term, but in this article we consider recent cases that affect ObGyns’ practice in particular. We start with the cases in which professional organizations filed amicus briefs and then turn to other notable cases.
1. Abortion access in Texas and other states
The most important ObGyn case of the 2015–2016 term was Whole Woman’s Health v Hellerstedt.1
At stake. Texas adopted a statute requiring 1) that physicians who perform abortions have admitting privileges at a hospital within 30 miles of the clinic and 2) that abortion clinics meet the state’s standards for ambulatory surgical centers. The current law, upheld by the Court some years ago, is that state laws affecting abortion are unconstitutional if they “unduly burden” the right to abortion. By undue burden, the Court meant, “Regulations that have the purpose or effect of presenting a substantial obstacle to a woman seeking an abortion impose an undue burden on the right.” The question in the Texas case was whether the statute’s 2 requirements were undue.
ACOG, AMA, and other groups filed a brief stating that the Texas law did not promote the welfare of women but instead was unnecessary and not “supported by accepted medical practice or scientific evidence.”2 In another brief the Society of Hospital Medicine and the Society of ObGyn Hospitalists also indicated that having admitting privileges is appropriate only for physicians who regularly admit patients to a hospital.3
A brief filed by the American Association of Pro-Life Obstetricians and Gynecologists and several other organizations argued the other side: “The surgical center and admitting privileges requirements imposed by the Act reflect the professional standard of practice for outpatient gynecological and similar surgery.”4
Final ruling. In a 5−3 decision, the Court struck down the Texas law for providing little or no health benefits while significantly burdening abortion facility access. Many clinics had closed or were in plans to because of the difficulty and expense of complying with the law. This case has national implications. Similar laws, either in place or being considered in other states, will almost certainly be ruled unconstitutional.
2. Contraceptive coverage
The case of Zubik v Burwell was closely watched this past year.
At stake. Under the ACA, a nonprofit religious organization may certify its objection to its insurance plan’s contraception coverage, at which point other arrangements are made to provide contraceptive coverage through the same plan. Religious organizations objected to the certification requirement.
A brief filed by ACOG, Physicians for Reproductive Health, and other groups emphasized the importance of providing contraceptives and contraceptive counseling as part of regular health care and suggested that the current accommodation for religious organizations is appropriate.5
After hearing the formal oral arguments, the Court asked for additional briefs on “whether contraceptive coverage could be provided to petitioners’ employees, through petitioners’ insurance companies, without any such notice from petitioners.”6
Final ruling. The parties agreed such a system would resolve the issue, so the Court sent the case back to the lower court to work out the details. In effect, the case was mediated—an unusual if not unique action for the Court. The resolution probably will achieve what the briefs sought—access to contraceptives and continuity of care.
3. Fraud and abuse litigation
The FCA, which provides for triple damages (3 times actual damages) and stiff civil penalties for anyone who presents the federal government (Medicare, Medicaid) with false claims for goods or services, is a major means of uncovering and punishing health care fraud and abuse. In health care, this law has been used to prosecute cases involving services paid for but not provided, unnecessary services, and off-label pharmaceutical promotion.
An important part of the FCA is that it allows a private intervenor (whistleblower) to initiate an action against a health care provider. The government may then take up the case. If not, the intervenor may pursue it; the incentive is 15% to 30% of the damages the government is awarded.
At stake. The Court was asked if “implied certification” applies to FCA cases.7 Implied certification means that requesting a payment from Medicare or Medicaid implies that the provider is not knowingly withholding information material to the government’s decision to pay the claim. In separately filed briefs, AMA et al8 and American Hospital Association (AHA) et al9 argued that applying implied certification to FCA cases would expand FCA litigation (particularly by intervenors), which is already expensive for health care institutions.
Final ruling. The Court unanimously adopted implied certification but noted that nondisclosure of information must be shown to be a material misrepresentation rather than a trivial regulatory or contractual violation. Furthermore, the Court emphasized that the basis for a claim must be an allegation of fraud, not of malpractice. These findings, which certainly are not what the health care organizations had hoped for, likely will lead to an increase in FCA cases.
4. Collection of state health care data
In Vermont, and about 20 other states that collect data on health care utilization and costs, health insurers and other entities are required to submit detailed reports about health care claims.10 Some insurers objected to this requirement.
At stake. An AHA–AAMC brief noted the importance of health care data and of Vermont’s collecting these data as contributing to better, more efficient health care delivery.11 Another brief, filed by AMA and the Vermont Medical Society, presented more legal or statutory arguments.12
Final ruling. The Court held that the Vermont plan and similar plans violate the federal Employee Retirement Income Security Act of 1974. As health insurance companies and other entities already provide detailed utilization and cost data to the federal government, producing up to 50 additional reports for state governments would be burdensome. Any state that wants the information, the Court said, should obtain it from the federal government.
More notable 2015-2016 Supreme Court decisions.
The Court:
- permitted limited consideration of race in university admissions. ACOG, AAMC, and AMA with many other groups filed an amicus brief supporting medical school and university affirmative action programs.1
- held that a state must give full faith and credit to the adoption orders of the courts of other states (this case involved an LGBT couple).2
- held that states may require (without a search warrant) a breathalyzer test, but not a blood test, for a driver suspected of drinking.3
- narrowed the ability of the federal government to seize or restrain (before trial) the assets of a person charged with criminal health care offenses.4
- temporarily stayed the August 2016 US Department of Education order to schools to allow transgender students to use the facilities in which they feel "most comfortable." The Court likely will take up this case very soon.5
- Fisher v University of Texas at Austin et al, No. 14-981 (2016). https://www.supremecourt.gov/opinions/15pdf/14-981_4g15.pdf. Accessed August 30, 2016.
- V.L. v E.L. et al, No. 15-648 (2016). https://www.supremecourt.gov/opinions/15pdf/15-648_d18e.pdf. Accessed August 30, 2016.
- Birchfield v North Dakota, No. 14-1468 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1468_8n59.pdf. Accessed August 30, 2016.
- Luis v United States, No. 14-419 (2016). https://www.supremecourt.gov/opinions/15pdf/14-419_nmip.pdf. Accessed August 30, 2016.
- Gloucester County School Board v G.G., by his next friend and mother, Deidre Grimm, No. 16A52 (2016). https://www.supremecourt.gov/opinions/15pdf/16a52_8759.pdf. Accessed August 30, 2016.
What’s to come
The Court’s recent decisions on access to abortion services and contraceptives were good for patients of ObGyns, but its decisions on health care FCA liability and state health care data collection were, arguably, not as good for ObGyn business practices.
The Court itself had an unusual year. Justice Scalia died in February, and Congress’s inaction on seating a replacement meant that most of the term’s cases were decided by an 8-member Court. Nevertheless, the Court was deadlocked 4−4 on only 4 of the 80 cases it heard. In addition, it was relatively agreed on outcomes; in only about one-third of cases were there more than 2 justices disagreeing with the outcome.
It is unlikely that a replacement for Justice Scalia will be confirmed before the Court begins its new term in October. The need to replace Justice Scalia and the potential turnover of other Court members—Justice Ginsburg is 83, Justice Kennedy is 80, and Justice Breyer is 78—are reminders of the importance of this year’s presidential election. In the meantime, the Court is accepting the cases that will make up the coming term’s docket, and ObGyns undoubtedly will play a role in cases that involve health care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Each year, the decisions of the Supreme Court have a significant impact on ObGyn practice. During the 2015–2016 term, which ended in June, the Court issued important rulings on abortion facilities, Affordable Care Act (ACA) contraception coverage, health care False Claims Act (FCA) liability, and state health care data collection. The American Medical Association (AMA), the Association of American Medical Colleges (AAMC), the American College of Obstetricians and Gynecologists (ACOG), and other organizations that represent health care professionals play an important role in health-related Supreme Court cases. For example, amicus curiae (“friend of the Court”) briefs are filed not by parties to a case but by organizations that have a special insight into or interest in a case. Although the extent to which amicus briefs influence cases is often unclear, organization representatives think their briefs make a difference, and briefs undoubtedly do in some cases.
The 2016 presidential election will determine the Supreme Court make-up for the next term, but in this article we consider recent cases that affect ObGyns’ practice in particular. We start with the cases in which professional organizations filed amicus briefs and then turn to other notable cases.
1. Abortion access in Texas and other states
The most important ObGyn case of the 2015–2016 term was Whole Woman’s Health v Hellerstedt.1
At stake. Texas adopted a statute requiring 1) that physicians who perform abortions have admitting privileges at a hospital within 30 miles of the clinic and 2) that abortion clinics meet the state’s standards for ambulatory surgical centers. The current law, upheld by the Court some years ago, is that state laws affecting abortion are unconstitutional if they “unduly burden” the right to abortion. By undue burden, the Court meant, “Regulations that have the purpose or effect of presenting a substantial obstacle to a woman seeking an abortion impose an undue burden on the right.” The question in the Texas case was whether the statute’s 2 requirements were undue.
ACOG, AMA, and other groups filed a brief stating that the Texas law did not promote the welfare of women but instead was unnecessary and not “supported by accepted medical practice or scientific evidence.”2 In another brief the Society of Hospital Medicine and the Society of ObGyn Hospitalists also indicated that having admitting privileges is appropriate only for physicians who regularly admit patients to a hospital.3
A brief filed by the American Association of Pro-Life Obstetricians and Gynecologists and several other organizations argued the other side: “The surgical center and admitting privileges requirements imposed by the Act reflect the professional standard of practice for outpatient gynecological and similar surgery.”4
Final ruling. In a 5−3 decision, the Court struck down the Texas law for providing little or no health benefits while significantly burdening abortion facility access. Many clinics had closed or were in plans to because of the difficulty and expense of complying with the law. This case has national implications. Similar laws, either in place or being considered in other states, will almost certainly be ruled unconstitutional.
2. Contraceptive coverage
The case of Zubik v Burwell was closely watched this past year.
At stake. Under the ACA, a nonprofit religious organization may certify its objection to its insurance plan’s contraception coverage, at which point other arrangements are made to provide contraceptive coverage through the same plan. Religious organizations objected to the certification requirement.
A brief filed by ACOG, Physicians for Reproductive Health, and other groups emphasized the importance of providing contraceptives and contraceptive counseling as part of regular health care and suggested that the current accommodation for religious organizations is appropriate.5
After hearing the formal oral arguments, the Court asked for additional briefs on “whether contraceptive coverage could be provided to petitioners’ employees, through petitioners’ insurance companies, without any such notice from petitioners.”6
Final ruling. The parties agreed such a system would resolve the issue, so the Court sent the case back to the lower court to work out the details. In effect, the case was mediated—an unusual if not unique action for the Court. The resolution probably will achieve what the briefs sought—access to contraceptives and continuity of care.
3. Fraud and abuse litigation
The FCA, which provides for triple damages (3 times actual damages) and stiff civil penalties for anyone who presents the federal government (Medicare, Medicaid) with false claims for goods or services, is a major means of uncovering and punishing health care fraud and abuse. In health care, this law has been used to prosecute cases involving services paid for but not provided, unnecessary services, and off-label pharmaceutical promotion.
An important part of the FCA is that it allows a private intervenor (whistleblower) to initiate an action against a health care provider. The government may then take up the case. If not, the intervenor may pursue it; the incentive is 15% to 30% of the damages the government is awarded.
At stake. The Court was asked if “implied certification” applies to FCA cases.7 Implied certification means that requesting a payment from Medicare or Medicaid implies that the provider is not knowingly withholding information material to the government’s decision to pay the claim. In separately filed briefs, AMA et al8 and American Hospital Association (AHA) et al9 argued that applying implied certification to FCA cases would expand FCA litigation (particularly by intervenors), which is already expensive for health care institutions.
Final ruling. The Court unanimously adopted implied certification but noted that nondisclosure of information must be shown to be a material misrepresentation rather than a trivial regulatory or contractual violation. Furthermore, the Court emphasized that the basis for a claim must be an allegation of fraud, not of malpractice. These findings, which certainly are not what the health care organizations had hoped for, likely will lead to an increase in FCA cases.
4. Collection of state health care data
In Vermont, and about 20 other states that collect data on health care utilization and costs, health insurers and other entities are required to submit detailed reports about health care claims.10 Some insurers objected to this requirement.
At stake. An AHA–AAMC brief noted the importance of health care data and of Vermont’s collecting these data as contributing to better, more efficient health care delivery.11 Another brief, filed by AMA and the Vermont Medical Society, presented more legal or statutory arguments.12
Final ruling. The Court held that the Vermont plan and similar plans violate the federal Employee Retirement Income Security Act of 1974. As health insurance companies and other entities already provide detailed utilization and cost data to the federal government, producing up to 50 additional reports for state governments would be burdensome. Any state that wants the information, the Court said, should obtain it from the federal government.
More notable 2015-2016 Supreme Court decisions.
The Court:
- permitted limited consideration of race in university admissions. ACOG, AAMC, and AMA with many other groups filed an amicus brief supporting medical school and university affirmative action programs.1
- held that a state must give full faith and credit to the adoption orders of the courts of other states (this case involved an LGBT couple).2
- held that states may require (without a search warrant) a breathalyzer test, but not a blood test, for a driver suspected of drinking.3
- narrowed the ability of the federal government to seize or restrain (before trial) the assets of a person charged with criminal health care offenses.4
- temporarily stayed the August 2016 US Department of Education order to schools to allow transgender students to use the facilities in which they feel "most comfortable." The Court likely will take up this case very soon.5
- Fisher v University of Texas at Austin et al, No. 14-981 (2016). https://www.supremecourt.gov/opinions/15pdf/14-981_4g15.pdf. Accessed August 30, 2016.
- V.L. v E.L. et al, No. 15-648 (2016). https://www.supremecourt.gov/opinions/15pdf/15-648_d18e.pdf. Accessed August 30, 2016.
- Birchfield v North Dakota, No. 14-1468 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1468_8n59.pdf. Accessed August 30, 2016.
- Luis v United States, No. 14-419 (2016). https://www.supremecourt.gov/opinions/15pdf/14-419_nmip.pdf. Accessed August 30, 2016.
- Gloucester County School Board v G.G., by his next friend and mother, Deidre Grimm, No. 16A52 (2016). https://www.supremecourt.gov/opinions/15pdf/16a52_8759.pdf. Accessed August 30, 2016.
What’s to come
The Court’s recent decisions on access to abortion services and contraceptives were good for patients of ObGyns, but its decisions on health care FCA liability and state health care data collection were, arguably, not as good for ObGyn business practices.
The Court itself had an unusual year. Justice Scalia died in February, and Congress’s inaction on seating a replacement meant that most of the term’s cases were decided by an 8-member Court. Nevertheless, the Court was deadlocked 4−4 on only 4 of the 80 cases it heard. In addition, it was relatively agreed on outcomes; in only about one-third of cases were there more than 2 justices disagreeing with the outcome.
It is unlikely that a replacement for Justice Scalia will be confirmed before the Court begins its new term in October. The need to replace Justice Scalia and the potential turnover of other Court members—Justice Ginsburg is 83, Justice Kennedy is 80, and Justice Breyer is 78—are reminders of the importance of this year’s presidential election. In the meantime, the Court is accepting the cases that will make up the coming term’s docket, and ObGyns undoubtedly will play a role in cases that involve health care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). https://www.supremecourt.gov/opinions/15pdf/15-274_new_e18f.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, American Medical Association, American Academy of Family Physicians, American Osteopathic Association, and American Academy of Pediatrics in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/ACOG-WilmerHale.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by Society of Hospital Medicine and Society of Ob/Gyn Hospitalists in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/Society-of-Hospital-Medicine-Crowell.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Association of Pro-Life Obstetricians and Gynecologists, American College of Pediatricians, Christian Medical & Dental Association, Catholic Medical Association, and Physicians for Life in support of respondents. Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al. http://www.scotusblog.com/wp-content/uploads/2016/02/15-274-bsac-American-Association-of-Pro-Life-Obstetricians-and-Gynecolog....pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, Physicians for Reproductive Health, American Academy of Family Physicians, American Nurses Association, et al in support of the government and affirmance. Zubik et al v Burwell, Secretary of Health and Human Services, et al, Nos. 14-1418, 14-1458, 14-1505, 15-35, 15-105, 15-119, and 15-191. http://www.scotusblog.com/wp-content/uploads/2016/02/Docfoc.com-Amicus-Brief-Zubik-v.-Burwell.pdf. Accessed August 30, 2016.
- Zubik et al v Burwell, Secretary of Health and Human Services, et al, No. 14-1418 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1418_8758.pdf. Accessed August 30, 2016.
- Universal Health Services, Inc v United States et al ex rel. Escobar et al, No. 15-7 (2016). https://www.supremecourt.gov/opinions/15pdf/15-7_a074.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association, National Association of Chain Drug Stores, National Association of Manufacturers, American Tort Reform Association and NFIB Small Business Legal Center in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7-tsac-American-Medical-Association.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association, Federation of American Hospitals, and Association of American Medical Colleges in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7tsacAHAFAHAAMC.pdf. Accessed August 30, 2016.
- Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). https://www.supremecourt.gov/opinions/15pdf/14-181_5426.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association and Association of American Medical Colleges in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/150904-amicus-gobeille-liberty.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association and Vermont Medical Society in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/VHCURES-Amicus-Brief-of-American-Medical-Association.pdf. Accessed August 30, 2016.
- Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). https://www.supremecourt.gov/opinions/15pdf/15-274_new_e18f.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, American Medical Association, American Academy of Family Physicians, American Osteopathic Association, and American Academy of Pediatrics in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/ACOG-WilmerHale.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by Society of Hospital Medicine and Society of Ob/Gyn Hospitalists in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/Society-of-Hospital-Medicine-Crowell.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Association of Pro-Life Obstetricians and Gynecologists, American College of Pediatricians, Christian Medical & Dental Association, Catholic Medical Association, and Physicians for Life in support of respondents. Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al. http://www.scotusblog.com/wp-content/uploads/2016/02/15-274-bsac-American-Association-of-Pro-Life-Obstetricians-and-Gynecolog....pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, Physicians for Reproductive Health, American Academy of Family Physicians, American Nurses Association, et al in support of the government and affirmance. Zubik et al v Burwell, Secretary of Health and Human Services, et al, Nos. 14-1418, 14-1458, 14-1505, 15-35, 15-105, 15-119, and 15-191. http://www.scotusblog.com/wp-content/uploads/2016/02/Docfoc.com-Amicus-Brief-Zubik-v.-Burwell.pdf. Accessed August 30, 2016.
- Zubik et al v Burwell, Secretary of Health and Human Services, et al, No. 14-1418 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1418_8758.pdf. Accessed August 30, 2016.
- Universal Health Services, Inc v United States et al ex rel. Escobar et al, No. 15-7 (2016). https://www.supremecourt.gov/opinions/15pdf/15-7_a074.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association, National Association of Chain Drug Stores, National Association of Manufacturers, American Tort Reform Association and NFIB Small Business Legal Center in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7-tsac-American-Medical-Association.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association, Federation of American Hospitals, and Association of American Medical Colleges in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7tsacAHAFAHAAMC.pdf. Accessed August 30, 2016.
- Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). https://www.supremecourt.gov/opinions/15pdf/14-181_5426.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association and Association of American Medical Colleges in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/150904-amicus-gobeille-liberty.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association and Vermont Medical Society in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/VHCURES-Amicus-Brief-of-American-Medical-Association.pdf. Accessed August 30, 2016.
In this Article
- Whole Woman’s Health v Hellerstedt
- Fraud and abuse litigation
- What’s to come