User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Study launched to further evaluate the central vein sign in MS
DALLAS –
At the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis, Daniel Ontaneda, MD, said that up to 20% of individuals referred for a diagnosis of multiple sclerosis (MS) are incorrectly diagnosed with the disease, and about two-thirds of misdiagnosed patients are exposed to unnecessary and sometimes life-threatening risks associated with disease-modifying therapies. “MRI is a sensitive tool for diagnosis of MS and is an integral component of the diagnostic criteria for MS,” said Dr. Ontaneda, a neurologist at the Cleveland Clinic Mellen Center for Multiple Sclerosis Treatment and Research. “However, there are problems with its implementation. Approximately half of individuals referred to an MS clinic present with atypical symptoms [fatigue, cognitive disturbance, pain] and not typical syndromes [unilateral optic neuritis, brain stem syndromes, partial myelitis]. Increasing diagnostic sensitivity may have come at the price of decreased specificity. MRI criteria have a specificity of 32% for dissemination in space and 42% for dissemination in time.”
While misdiagnosis appears to be mainly caused by overinterpretation of abnormal MRI findings, the central vein sign (CVS) is an effective method to overcome such challenges. Recent studies have demonstrated that CVS may help to identify MS, as 85% of white matter lesions in MS have a central vein, compared with only 8% of small vessel ischemic disease, 34% of migraine, and 14% of other inflammatory or autoimmune diseases.
“We think there is a significant and unmet need for more specific and accurate diagnostic tests to facilitate early confirmation of a diagnosis of MS,” Dr. Ontaneda said. “We propose a prospective evaluation of the central vein sign, which we hypothesize will reduce misdiagnosis, hasten early diagnosis, and simplify clinical decision making.”
With funding from the Race to Erase MS Foundation, he and his associates have designed CAVS-MS (Central Vein Sign in MS), a multicenter, prospective, observational trial being conducted at 10 sites. The first phase of the study is a cross-sectional pilot at the 10 sites. The primary objective is to establish the contrast-to-noise ratio of lesion to normal-appearing white matter and central vein to lesion across the 10 sites using 3-tesla FLAIR imaging in subjects with a clinical or radiologic suspicion of MS. The secondary objectives are to investigate the difference in contrast-to-noise ratio identified in the primary objective between pre- and postcontrast FLAIR imaging to identify whether gadolinium injection improves central vein detection, to determine the reproducibility of different methods for detection of positive CVS across sites, and to determine the sensitivity and specificity of the different methods for the diagnosis of MS, compared with the McDonald 2010 MS criteria.
The study population will consist of 100 individuals referred to an MS center based on clinical or radiologic suspicion of MS; 30 participants are currently enrolled. The 10 sites include the Cleveland Clinic; Johns Hopkins University, Baltimore; the University of California, San Francisco; the University of Texas, Houston; the University of Toronto; the University of Vermont, Burlington; the University of Southern California, Los Angeles; Cedars-Sinai Medical Center, Los Angeles; Yale University, New Haven, Conn.; and the University of Pennsylvania, Philadelphia.
CAVS-MS includes development of a software platform for rating of central veins through an imaging software partner, QMENTA. “We are going to have the individual clinicians at each site rate the lesions, so we will have information from 10 different raters,” Dr. Ontaneda said. The study will be coordinated at the Cleveland Clinic, central image analysis will be conducted at the National Institutes of Health, and statistical analysis will be performed at the University of Pennsylvania.
The researchers also hope to perform a prospective study with three objectives. The first is to determine if incorporation of CVS for the diagnosis of MS improves diagnostic accuracy and hastens diagnosis in individuals presenting with typical first clinical events. The second objective “is to determine if incorporation of CVS for the diagnosis of MS improves specificity among individuals presenting with atypical syndromes,” Dr. Ontaneda said. “The third aim is to look at central vein volume as a predictor of clinical/MRI disease activity associated with disability in MS.”
He concluded his remarks by describing the CVS as “a tool that offers promise both for increasing specificity and perhaps enabling earlier diagnosis of MS. Studies will determine if the central vein sign can be incorporated into the diagnostic criteria. The NIH is working with MRI manufacturers to make sequences available for disseminated clinical use.”
Dr. Ontaneda reported that he has received grant support from the National Institutes of Health, the Race to Erase MS Foundation, the Patient-Centered Outcomes Research Institute, the National Multiple Sclerosis Society, Genentech, Genzyme, and Novartis. He has also received consulting fees from Biogen, Genentech, and Novartis.
DALLAS –
At the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis, Daniel Ontaneda, MD, said that up to 20% of individuals referred for a diagnosis of multiple sclerosis (MS) are incorrectly diagnosed with the disease, and about two-thirds of misdiagnosed patients are exposed to unnecessary and sometimes life-threatening risks associated with disease-modifying therapies. “MRI is a sensitive tool for diagnosis of MS and is an integral component of the diagnostic criteria for MS,” said Dr. Ontaneda, a neurologist at the Cleveland Clinic Mellen Center for Multiple Sclerosis Treatment and Research. “However, there are problems with its implementation. Approximately half of individuals referred to an MS clinic present with atypical symptoms [fatigue, cognitive disturbance, pain] and not typical syndromes [unilateral optic neuritis, brain stem syndromes, partial myelitis]. Increasing diagnostic sensitivity may have come at the price of decreased specificity. MRI criteria have a specificity of 32% for dissemination in space and 42% for dissemination in time.”
While misdiagnosis appears to be mainly caused by overinterpretation of abnormal MRI findings, the central vein sign (CVS) is an effective method to overcome such challenges. Recent studies have demonstrated that CVS may help to identify MS, as 85% of white matter lesions in MS have a central vein, compared with only 8% of small vessel ischemic disease, 34% of migraine, and 14% of other inflammatory or autoimmune diseases.
“We think there is a significant and unmet need for more specific and accurate diagnostic tests to facilitate early confirmation of a diagnosis of MS,” Dr. Ontaneda said. “We propose a prospective evaluation of the central vein sign, which we hypothesize will reduce misdiagnosis, hasten early diagnosis, and simplify clinical decision making.”
With funding from the Race to Erase MS Foundation, he and his associates have designed CAVS-MS (Central Vein Sign in MS), a multicenter, prospective, observational trial being conducted at 10 sites. The first phase of the study is a cross-sectional pilot at the 10 sites. The primary objective is to establish the contrast-to-noise ratio of lesion to normal-appearing white matter and central vein to lesion across the 10 sites using 3-tesla FLAIR imaging in subjects with a clinical or radiologic suspicion of MS. The secondary objectives are to investigate the difference in contrast-to-noise ratio identified in the primary objective between pre- and postcontrast FLAIR imaging to identify whether gadolinium injection improves central vein detection, to determine the reproducibility of different methods for detection of positive CVS across sites, and to determine the sensitivity and specificity of the different methods for the diagnosis of MS, compared with the McDonald 2010 MS criteria.
The study population will consist of 100 individuals referred to an MS center based on clinical or radiologic suspicion of MS; 30 participants are currently enrolled. The 10 sites include the Cleveland Clinic; Johns Hopkins University, Baltimore; the University of California, San Francisco; the University of Texas, Houston; the University of Toronto; the University of Vermont, Burlington; the University of Southern California, Los Angeles; Cedars-Sinai Medical Center, Los Angeles; Yale University, New Haven, Conn.; and the University of Pennsylvania, Philadelphia.
CAVS-MS includes development of a software platform for rating of central veins through an imaging software partner, QMENTA. “We are going to have the individual clinicians at each site rate the lesions, so we will have information from 10 different raters,” Dr. Ontaneda said. The study will be coordinated at the Cleveland Clinic, central image analysis will be conducted at the National Institutes of Health, and statistical analysis will be performed at the University of Pennsylvania.
The researchers also hope to perform a prospective study with three objectives. The first is to determine if incorporation of CVS for the diagnosis of MS improves diagnostic accuracy and hastens diagnosis in individuals presenting with typical first clinical events. The second objective “is to determine if incorporation of CVS for the diagnosis of MS improves specificity among individuals presenting with atypical syndromes,” Dr. Ontaneda said. “The third aim is to look at central vein volume as a predictor of clinical/MRI disease activity associated with disability in MS.”
He concluded his remarks by describing the CVS as “a tool that offers promise both for increasing specificity and perhaps enabling earlier diagnosis of MS. Studies will determine if the central vein sign can be incorporated into the diagnostic criteria. The NIH is working with MRI manufacturers to make sequences available for disseminated clinical use.”
Dr. Ontaneda reported that he has received grant support from the National Institutes of Health, the Race to Erase MS Foundation, the Patient-Centered Outcomes Research Institute, the National Multiple Sclerosis Society, Genentech, Genzyme, and Novartis. He has also received consulting fees from Biogen, Genentech, and Novartis.
DALLAS –
At the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis, Daniel Ontaneda, MD, said that up to 20% of individuals referred for a diagnosis of multiple sclerosis (MS) are incorrectly diagnosed with the disease, and about two-thirds of misdiagnosed patients are exposed to unnecessary and sometimes life-threatening risks associated with disease-modifying therapies. “MRI is a sensitive tool for diagnosis of MS and is an integral component of the diagnostic criteria for MS,” said Dr. Ontaneda, a neurologist at the Cleveland Clinic Mellen Center for Multiple Sclerosis Treatment and Research. “However, there are problems with its implementation. Approximately half of individuals referred to an MS clinic present with atypical symptoms [fatigue, cognitive disturbance, pain] and not typical syndromes [unilateral optic neuritis, brain stem syndromes, partial myelitis]. Increasing diagnostic sensitivity may have come at the price of decreased specificity. MRI criteria have a specificity of 32% for dissemination in space and 42% for dissemination in time.”
While misdiagnosis appears to be mainly caused by overinterpretation of abnormal MRI findings, the central vein sign (CVS) is an effective method to overcome such challenges. Recent studies have demonstrated that CVS may help to identify MS, as 85% of white matter lesions in MS have a central vein, compared with only 8% of small vessel ischemic disease, 34% of migraine, and 14% of other inflammatory or autoimmune diseases.
“We think there is a significant and unmet need for more specific and accurate diagnostic tests to facilitate early confirmation of a diagnosis of MS,” Dr. Ontaneda said. “We propose a prospective evaluation of the central vein sign, which we hypothesize will reduce misdiagnosis, hasten early diagnosis, and simplify clinical decision making.”
With funding from the Race to Erase MS Foundation, he and his associates have designed CAVS-MS (Central Vein Sign in MS), a multicenter, prospective, observational trial being conducted at 10 sites. The first phase of the study is a cross-sectional pilot at the 10 sites. The primary objective is to establish the contrast-to-noise ratio of lesion to normal-appearing white matter and central vein to lesion across the 10 sites using 3-tesla FLAIR imaging in subjects with a clinical or radiologic suspicion of MS. The secondary objectives are to investigate the difference in contrast-to-noise ratio identified in the primary objective between pre- and postcontrast FLAIR imaging to identify whether gadolinium injection improves central vein detection, to determine the reproducibility of different methods for detection of positive CVS across sites, and to determine the sensitivity and specificity of the different methods for the diagnosis of MS, compared with the McDonald 2010 MS criteria.
The study population will consist of 100 individuals referred to an MS center based on clinical or radiologic suspicion of MS; 30 participants are currently enrolled. The 10 sites include the Cleveland Clinic; Johns Hopkins University, Baltimore; the University of California, San Francisco; the University of Texas, Houston; the University of Toronto; the University of Vermont, Burlington; the University of Southern California, Los Angeles; Cedars-Sinai Medical Center, Los Angeles; Yale University, New Haven, Conn.; and the University of Pennsylvania, Philadelphia.
CAVS-MS includes development of a software platform for rating of central veins through an imaging software partner, QMENTA. “We are going to have the individual clinicians at each site rate the lesions, so we will have information from 10 different raters,” Dr. Ontaneda said. The study will be coordinated at the Cleveland Clinic, central image analysis will be conducted at the National Institutes of Health, and statistical analysis will be performed at the University of Pennsylvania.
The researchers also hope to perform a prospective study with three objectives. The first is to determine if incorporation of CVS for the diagnosis of MS improves diagnostic accuracy and hastens diagnosis in individuals presenting with typical first clinical events. The second objective “is to determine if incorporation of CVS for the diagnosis of MS improves specificity among individuals presenting with atypical syndromes,” Dr. Ontaneda said. “The third aim is to look at central vein volume as a predictor of clinical/MRI disease activity associated with disability in MS.”
He concluded his remarks by describing the CVS as “a tool that offers promise both for increasing specificity and perhaps enabling earlier diagnosis of MS. Studies will determine if the central vein sign can be incorporated into the diagnostic criteria. The NIH is working with MRI manufacturers to make sequences available for disseminated clinical use.”
Dr. Ontaneda reported that he has received grant support from the National Institutes of Health, the Race to Erase MS Foundation, the Patient-Centered Outcomes Research Institute, the National Multiple Sclerosis Society, Genentech, Genzyme, and Novartis. He has also received consulting fees from Biogen, Genentech, and Novartis.
EXPERT ANALYSIS FROM ACTRIMS FORUM 2019
Expert calls for more ‘ethnocentric’ research in MS
DALLAS – The way Lilyana Amezcua, MD, sees it, researchers should look beyond using race and ethnicity only as demographic variables when reporting results from multiple sclerosis studies.
“As a demographic variable we see it all the time: white versus non-white, and the methods to arrive at a category are seldom discussed,” Dr. Amezcua said at a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis. “We need to think about ethnocentric research, where the method for determination for race and ethnicity becomes important. This includes examining self-identity (ethnicity), along with physical characteristics and medical records, and confirming that beyond the individual.”
The goal, she continued, is to identify who is at risk for inferior health, such as trying to sort out biological and genetic explanations from non-biological explanations. Ethnocentric research also helps to address health care disparities. “But there’s a broad intersection between race and ethnicity, and depending on the question, genetic ancestry could help,” said Dr. Amezcua, a neurologist at the Keck School of Medicine at the University of Southern California, Los Angeles. “Race tries to infer biological differences, ethnicity infers societal differences, and ancestry infers genetic variations.”
While genetic and biologic features are often used to evaluate how race and ethnicity affects those with MS, Dr. Amezcua noted that several additional factors could influence outcomes. These include access to care as well as individual and community factors that relate to social determinants of health, such as poverty, exposures, and environmental stress. “These could be contributing to worse outcomes,” she said. “So could modifiable factors such as illness beliefs, health literacy, illness management, and acculturation.”
In terms of health literacy, there are reports suggesting that there is a general lack of adequate education and understanding about MS treatment and realistic expectations in African Americans and Hispanics, she said.
In addition, research has shown there is a lower probability of being under the care of a neurologist if you lack health insurance (odds ratio = 0.38) or are African American (OR = 0.52) or Hispanic (OR = 0.61), based on nationally representative data from the 2006-2013 Medical Expenditure Panel Survey (Neurology. 2017;88[24]:2268-75). “Just being African American or Hispanic lowered the probability of seeing a neurologist,” she said.
Published evidence also exists to suggest that illness beliefs drive some people away from MS treatment. “These are beliefs embedded in social and cultural factors known as cultural idioms,” Dr. Amezcua explained. “In a study that was able to capture qualitative and quantitative data, researchers found that social and cultural factors were more frequently reported in immigrant groups, alluding to the fact that we need to look beyond whether they are African American or Hispanic, and look at acculturation” (Int J MS Care. 2017;19[3]:131-9).
Then there’s the issue of Food and Drug Administration-approved disease-modifying therapies in MS and minorities. In an exploratory post hoc analysis of the Evidence of Interferon Dose-Response: European North American Comparative Efficacy (EVIDENCE) study, researchers found that African-American subjects experienced more exacerbations and were less likely to remain exacerbation free, compared with whites (Arch Neurol. 2005;62[11]:1681-3). The African-American subjects also developed more new MS lesions on T2-weighted brain MRI at 48 weeks (P = .04).
“There are a lot of unanswered questions, but understanding the effect of race/ethnicity is crucial to understanding MS disparities,” Dr. Amezcua said. “To better understand genetic variation in the context of health disparities, using ‘genetic ancestry’ could help with precision medicine. We must remember that minorities with MS face barriers related to access and education in MS care much more so than whites.”
She concluded her remarks by underscoring the importance of increasing minority participation in research and clinical trials. “But today, clinical trial participation by minorities is less than 10%. As we progress, and as we get closer to precision medicine, the health disparities will widen.”
She reported having no financial disclosures.
DALLAS – The way Lilyana Amezcua, MD, sees it, researchers should look beyond using race and ethnicity only as demographic variables when reporting results from multiple sclerosis studies.
“As a demographic variable we see it all the time: white versus non-white, and the methods to arrive at a category are seldom discussed,” Dr. Amezcua said at a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis. “We need to think about ethnocentric research, where the method for determination for race and ethnicity becomes important. This includes examining self-identity (ethnicity), along with physical characteristics and medical records, and confirming that beyond the individual.”
The goal, she continued, is to identify who is at risk for inferior health, such as trying to sort out biological and genetic explanations from non-biological explanations. Ethnocentric research also helps to address health care disparities. “But there’s a broad intersection between race and ethnicity, and depending on the question, genetic ancestry could help,” said Dr. Amezcua, a neurologist at the Keck School of Medicine at the University of Southern California, Los Angeles. “Race tries to infer biological differences, ethnicity infers societal differences, and ancestry infers genetic variations.”
While genetic and biologic features are often used to evaluate how race and ethnicity affects those with MS, Dr. Amezcua noted that several additional factors could influence outcomes. These include access to care as well as individual and community factors that relate to social determinants of health, such as poverty, exposures, and environmental stress. “These could be contributing to worse outcomes,” she said. “So could modifiable factors such as illness beliefs, health literacy, illness management, and acculturation.”
In terms of health literacy, there are reports suggesting that there is a general lack of adequate education and understanding about MS treatment and realistic expectations in African Americans and Hispanics, she said.
In addition, research has shown there is a lower probability of being under the care of a neurologist if you lack health insurance (odds ratio = 0.38) or are African American (OR = 0.52) or Hispanic (OR = 0.61), based on nationally representative data from the 2006-2013 Medical Expenditure Panel Survey (Neurology. 2017;88[24]:2268-75). “Just being African American or Hispanic lowered the probability of seeing a neurologist,” she said.
Published evidence also exists to suggest that illness beliefs drive some people away from MS treatment. “These are beliefs embedded in social and cultural factors known as cultural idioms,” Dr. Amezcua explained. “In a study that was able to capture qualitative and quantitative data, researchers found that social and cultural factors were more frequently reported in immigrant groups, alluding to the fact that we need to look beyond whether they are African American or Hispanic, and look at acculturation” (Int J MS Care. 2017;19[3]:131-9).
Then there’s the issue of Food and Drug Administration-approved disease-modifying therapies in MS and minorities. In an exploratory post hoc analysis of the Evidence of Interferon Dose-Response: European North American Comparative Efficacy (EVIDENCE) study, researchers found that African-American subjects experienced more exacerbations and were less likely to remain exacerbation free, compared with whites (Arch Neurol. 2005;62[11]:1681-3). The African-American subjects also developed more new MS lesions on T2-weighted brain MRI at 48 weeks (P = .04).
“There are a lot of unanswered questions, but understanding the effect of race/ethnicity is crucial to understanding MS disparities,” Dr. Amezcua said. “To better understand genetic variation in the context of health disparities, using ‘genetic ancestry’ could help with precision medicine. We must remember that minorities with MS face barriers related to access and education in MS care much more so than whites.”
She concluded her remarks by underscoring the importance of increasing minority participation in research and clinical trials. “But today, clinical trial participation by minorities is less than 10%. As we progress, and as we get closer to precision medicine, the health disparities will widen.”
She reported having no financial disclosures.
DALLAS – The way Lilyana Amezcua, MD, sees it, researchers should look beyond using race and ethnicity only as demographic variables when reporting results from multiple sclerosis studies.
“As a demographic variable we see it all the time: white versus non-white, and the methods to arrive at a category are seldom discussed,” Dr. Amezcua said at a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis. “We need to think about ethnocentric research, where the method for determination for race and ethnicity becomes important. This includes examining self-identity (ethnicity), along with physical characteristics and medical records, and confirming that beyond the individual.”
The goal, she continued, is to identify who is at risk for inferior health, such as trying to sort out biological and genetic explanations from non-biological explanations. Ethnocentric research also helps to address health care disparities. “But there’s a broad intersection between race and ethnicity, and depending on the question, genetic ancestry could help,” said Dr. Amezcua, a neurologist at the Keck School of Medicine at the University of Southern California, Los Angeles. “Race tries to infer biological differences, ethnicity infers societal differences, and ancestry infers genetic variations.”
While genetic and biologic features are often used to evaluate how race and ethnicity affects those with MS, Dr. Amezcua noted that several additional factors could influence outcomes. These include access to care as well as individual and community factors that relate to social determinants of health, such as poverty, exposures, and environmental stress. “These could be contributing to worse outcomes,” she said. “So could modifiable factors such as illness beliefs, health literacy, illness management, and acculturation.”
In terms of health literacy, there are reports suggesting that there is a general lack of adequate education and understanding about MS treatment and realistic expectations in African Americans and Hispanics, she said.
In addition, research has shown there is a lower probability of being under the care of a neurologist if you lack health insurance (odds ratio = 0.38) or are African American (OR = 0.52) or Hispanic (OR = 0.61), based on nationally representative data from the 2006-2013 Medical Expenditure Panel Survey (Neurology. 2017;88[24]:2268-75). “Just being African American or Hispanic lowered the probability of seeing a neurologist,” she said.
Published evidence also exists to suggest that illness beliefs drive some people away from MS treatment. “These are beliefs embedded in social and cultural factors known as cultural idioms,” Dr. Amezcua explained. “In a study that was able to capture qualitative and quantitative data, researchers found that social and cultural factors were more frequently reported in immigrant groups, alluding to the fact that we need to look beyond whether they are African American or Hispanic, and look at acculturation” (Int J MS Care. 2017;19[3]:131-9).
Then there’s the issue of Food and Drug Administration-approved disease-modifying therapies in MS and minorities. In an exploratory post hoc analysis of the Evidence of Interferon Dose-Response: European North American Comparative Efficacy (EVIDENCE) study, researchers found that African-American subjects experienced more exacerbations and were less likely to remain exacerbation free, compared with whites (Arch Neurol. 2005;62[11]:1681-3). The African-American subjects also developed more new MS lesions on T2-weighted brain MRI at 48 weeks (P = .04).
“There are a lot of unanswered questions, but understanding the effect of race/ethnicity is crucial to understanding MS disparities,” Dr. Amezcua said. “To better understand genetic variation in the context of health disparities, using ‘genetic ancestry’ could help with precision medicine. We must remember that minorities with MS face barriers related to access and education in MS care much more so than whites.”
She concluded her remarks by underscoring the importance of increasing minority participation in research and clinical trials. “But today, clinical trial participation by minorities is less than 10%. As we progress, and as we get closer to precision medicine, the health disparities will widen.”
She reported having no financial disclosures.
EXPERT ANALYSIS FROM ACTRIMS FORUM 2019
Smartphone technology helps to detect, track eye changes in MS
DALLAS – A battery of smartphone tests have been developed to help clinicians detect and monitor eye changes in MS patients.
At a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis, Randy H. Kardon, MD, PhD, said that there are two main high priority gaps to fill when it comes to better understanding the effects of MS on vision. “One, I think we need a way for early detection of visual pathway disturbances after either an acute clinical event or a subclinical event,” said Dr. Kardon, professor of neuro-ophthalmology at the University of Iowa, Iowa City. “Two, we need to monitor changes in the visual pathway over time in MS patients and capture variations due to changes in nerve conduction. The idea is, can we have a suite of smartphone tests that you can use in the clinic, but the patient can also use at home unsupervised, to get a time domain, so if there are fluctuations of core body temperature due to myelination, or subclinical changes going on, could we detect it earlier and monitor these patients? That’s the motivation.”
Although use of smartphone technology and mobile devices are emerging in health care settings, most of this technology is used sparingly in vision testing, mostly due to a lack of rigorous calibration of instruments and validation, said Dr. Kardon, who also directs the Iowa City VA Center for Prevention and Treatment of Visual Loss. To make a visual smartphone test viable, he continued, the visual output of the device must match the intended input in terms of multiple parameters (technical validation). Important parameters for vision tests include brightness, luminance, spatial resolution, and temporal resolution. Confounding variables include ambient lighting and viewing distance.
In his work with researchers from Aalborg University in Denmark, Dr. Kardon has developed four smartphone visual tests intended to be intuitive for patients. “We didn’t want something that was going to take more than 15 seconds,” he said. The visual tests include:
1. Critical flicker fusion, a test of optic nerve conduction. “This tests how well you can see a light flickering at a given temporal frequency at different levels of contrast, or how fast it can flicker before you don’t see a flicker anymore,” Dr. Kardon said. “The user sees spots that are flickering and just touches the ones they perceive to be flickering; they eliminate them by touching them.” When the test ends, the software “brackets what they did to a finer scale, and it finds the contrast at which that flicker wasn’t perceived anymore.”
2. The Landolt C visual acuity test. For this, the user must indicate the direction of the gap in the ring in a forced-choice task. “The user touches which arrow on the screen is pointing to where the location of the break in the Landolt C is perceived,” Dr. Kardon said. The Landolt C becomes progressively smaller until the location of the break can no longer be seen. “It’s pretty simple, and it finds the smallest size of the ‘C’ at which you’re making mistakes about 50% of the time, which is the threshold value for visual acuity,” he said.
3. Contrast sensitivity test at a fixed spatial frequency. “In this test, we fix the size of the letter to a large size, so spatial frequency is not at play, and we vary the contrast,” he said. “Users push the arrow wherever they see the break.” The contrast between the “C” and the background is sequentially reduced until a threshold is determined for the lowest contrast at which the location of the break in the “C” can still be observed.
4. Contrast sensitivity test at different spatial frequencies. This measure, also known as a vanishing optotype, is a line drawing of an object on a smooth, diffuse grayscale background. By altering the line properties used to define the shape of the vanishing optotype, one can vary its spatial frequency and contrast independent of target size. “This makes it an easy test because what the patient is asked to do is to touch wherever they see an object on the screen to eliminate it from the series of optotypes on the screen,” Dr. Kardon said. “The test is very fast, very intuitive.”
The researchers piloted use of these tests in a study of 104 age-matched control subjects and 117 MS patients. Of the 117 MS patients, 74 had a history of optic neuritis and 43 did not. The four tests were used in conjunction with standardized assessments, including the near-contrast acuity card test at 2.5%, the distant Early Treatment Diabetic Retinopathy Study (ETDRS) acuity test, as well as optical coherence tomography (OCT) of the retinal nerve fiber layer and ganglion cell layer thickness. Dr. Kardon and his colleagues found that when clinicians used a large target and varied the contrast, the test “did very well at differentiating normal from eyes with either previous optic neuritis or no previous optic neuritis,” he said. “It also differentiated eyes with previous optic neuritis and those with no optic neuritis. The visual acuity test didn’t perform as well because this is a near test. What we discovered afterward is that even at a fixed distance, many people who are presbyopic, or don’t have their optimal near correction, don’t do so well, because you’re testing spatial acuity. That’s a warning sign for future tests. You have to be careful as to how these are interpreted if they don’t have their best correction at near.”
Results from the critical flicker fusions tests were significant, except that they didn’t differentiate eyes affected by optic neuritis from those that weren’t. “The reason is that conduction was down in all of those eyes, so the combination of using contrast sensitivity and flicker fusion may not only help you diagnose MS, but whether that eye had been involved with optic neuritis before,” Dr. Kardon said. To date, he and his colleagues have completed technical validation of temporal frequency and contrast parameters. They’ve also completed preliminary investigations for determining test-retest variability, blurring effects, binocular summation effects, and quantification of normative ranges and abnormal subject data.
“A benefit of smartphone testing in MS is that visual dysfunction can be detected, leading to earlier interventions,” Dr. Kardon concluded. “We can study this on a time scale that wasn’t previously available. Wouldn’t you like to know on a daily or even a weekly basis what the fluctuations are in a home environment for MS patients? It’s low-cost, large-scale, and enables you to study genotype-phenotype comparisons.”
Going forward, Dr. Kardon and his colleagues have developed video cameras that go around the periphery of the iPad that can assess pupil and ocular motility, as well as eyelid and facial features in real time. He disclosed that he has received funding from the National Eye Institute, the Department of Defense, and from VA Rehabilitation Research and Development. He was also a member of the Novartis steering committee for the OCTiMS study and is a cofounder of MedFace and FaceX.
DALLAS – A battery of smartphone tests have been developed to help clinicians detect and monitor eye changes in MS patients.
At a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis, Randy H. Kardon, MD, PhD, said that there are two main high priority gaps to fill when it comes to better understanding the effects of MS on vision. “One, I think we need a way for early detection of visual pathway disturbances after either an acute clinical event or a subclinical event,” said Dr. Kardon, professor of neuro-ophthalmology at the University of Iowa, Iowa City. “Two, we need to monitor changes in the visual pathway over time in MS patients and capture variations due to changes in nerve conduction. The idea is, can we have a suite of smartphone tests that you can use in the clinic, but the patient can also use at home unsupervised, to get a time domain, so if there are fluctuations of core body temperature due to myelination, or subclinical changes going on, could we detect it earlier and monitor these patients? That’s the motivation.”
Although use of smartphone technology and mobile devices are emerging in health care settings, most of this technology is used sparingly in vision testing, mostly due to a lack of rigorous calibration of instruments and validation, said Dr. Kardon, who also directs the Iowa City VA Center for Prevention and Treatment of Visual Loss. To make a visual smartphone test viable, he continued, the visual output of the device must match the intended input in terms of multiple parameters (technical validation). Important parameters for vision tests include brightness, luminance, spatial resolution, and temporal resolution. Confounding variables include ambient lighting and viewing distance.
In his work with researchers from Aalborg University in Denmark, Dr. Kardon has developed four smartphone visual tests intended to be intuitive for patients. “We didn’t want something that was going to take more than 15 seconds,” he said. The visual tests include:
1. Critical flicker fusion, a test of optic nerve conduction. “This tests how well you can see a light flickering at a given temporal frequency at different levels of contrast, or how fast it can flicker before you don’t see a flicker anymore,” Dr. Kardon said. “The user sees spots that are flickering and just touches the ones they perceive to be flickering; they eliminate them by touching them.” When the test ends, the software “brackets what they did to a finer scale, and it finds the contrast at which that flicker wasn’t perceived anymore.”
2. The Landolt C visual acuity test. For this, the user must indicate the direction of the gap in the ring in a forced-choice task. “The user touches which arrow on the screen is pointing to where the location of the break in the Landolt C is perceived,” Dr. Kardon said. The Landolt C becomes progressively smaller until the location of the break can no longer be seen. “It’s pretty simple, and it finds the smallest size of the ‘C’ at which you’re making mistakes about 50% of the time, which is the threshold value for visual acuity,” he said.
3. Contrast sensitivity test at a fixed spatial frequency. “In this test, we fix the size of the letter to a large size, so spatial frequency is not at play, and we vary the contrast,” he said. “Users push the arrow wherever they see the break.” The contrast between the “C” and the background is sequentially reduced until a threshold is determined for the lowest contrast at which the location of the break in the “C” can still be observed.
4. Contrast sensitivity test at different spatial frequencies. This measure, also known as a vanishing optotype, is a line drawing of an object on a smooth, diffuse grayscale background. By altering the line properties used to define the shape of the vanishing optotype, one can vary its spatial frequency and contrast independent of target size. “This makes it an easy test because what the patient is asked to do is to touch wherever they see an object on the screen to eliminate it from the series of optotypes on the screen,” Dr. Kardon said. “The test is very fast, very intuitive.”
The researchers piloted use of these tests in a study of 104 age-matched control subjects and 117 MS patients. Of the 117 MS patients, 74 had a history of optic neuritis and 43 did not. The four tests were used in conjunction with standardized assessments, including the near-contrast acuity card test at 2.5%, the distant Early Treatment Diabetic Retinopathy Study (ETDRS) acuity test, as well as optical coherence tomography (OCT) of the retinal nerve fiber layer and ganglion cell layer thickness. Dr. Kardon and his colleagues found that when clinicians used a large target and varied the contrast, the test “did very well at differentiating normal from eyes with either previous optic neuritis or no previous optic neuritis,” he said. “It also differentiated eyes with previous optic neuritis and those with no optic neuritis. The visual acuity test didn’t perform as well because this is a near test. What we discovered afterward is that even at a fixed distance, many people who are presbyopic, or don’t have their optimal near correction, don’t do so well, because you’re testing spatial acuity. That’s a warning sign for future tests. You have to be careful as to how these are interpreted if they don’t have their best correction at near.”
Results from the critical flicker fusions tests were significant, except that they didn’t differentiate eyes affected by optic neuritis from those that weren’t. “The reason is that conduction was down in all of those eyes, so the combination of using contrast sensitivity and flicker fusion may not only help you diagnose MS, but whether that eye had been involved with optic neuritis before,” Dr. Kardon said. To date, he and his colleagues have completed technical validation of temporal frequency and contrast parameters. They’ve also completed preliminary investigations for determining test-retest variability, blurring effects, binocular summation effects, and quantification of normative ranges and abnormal subject data.
“A benefit of smartphone testing in MS is that visual dysfunction can be detected, leading to earlier interventions,” Dr. Kardon concluded. “We can study this on a time scale that wasn’t previously available. Wouldn’t you like to know on a daily or even a weekly basis what the fluctuations are in a home environment for MS patients? It’s low-cost, large-scale, and enables you to study genotype-phenotype comparisons.”
Going forward, Dr. Kardon and his colleagues have developed video cameras that go around the periphery of the iPad that can assess pupil and ocular motility, as well as eyelid and facial features in real time. He disclosed that he has received funding from the National Eye Institute, the Department of Defense, and from VA Rehabilitation Research and Development. He was also a member of the Novartis steering committee for the OCTiMS study and is a cofounder of MedFace and FaceX.
DALLAS – A battery of smartphone tests have been developed to help clinicians detect and monitor eye changes in MS patients.
At a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis, Randy H. Kardon, MD, PhD, said that there are two main high priority gaps to fill when it comes to better understanding the effects of MS on vision. “One, I think we need a way for early detection of visual pathway disturbances after either an acute clinical event or a subclinical event,” said Dr. Kardon, professor of neuro-ophthalmology at the University of Iowa, Iowa City. “Two, we need to monitor changes in the visual pathway over time in MS patients and capture variations due to changes in nerve conduction. The idea is, can we have a suite of smartphone tests that you can use in the clinic, but the patient can also use at home unsupervised, to get a time domain, so if there are fluctuations of core body temperature due to myelination, or subclinical changes going on, could we detect it earlier and monitor these patients? That’s the motivation.”
Although use of smartphone technology and mobile devices are emerging in health care settings, most of this technology is used sparingly in vision testing, mostly due to a lack of rigorous calibration of instruments and validation, said Dr. Kardon, who also directs the Iowa City VA Center for Prevention and Treatment of Visual Loss. To make a visual smartphone test viable, he continued, the visual output of the device must match the intended input in terms of multiple parameters (technical validation). Important parameters for vision tests include brightness, luminance, spatial resolution, and temporal resolution. Confounding variables include ambient lighting and viewing distance.
In his work with researchers from Aalborg University in Denmark, Dr. Kardon has developed four smartphone visual tests intended to be intuitive for patients. “We didn’t want something that was going to take more than 15 seconds,” he said. The visual tests include:
1. Critical flicker fusion, a test of optic nerve conduction. “This tests how well you can see a light flickering at a given temporal frequency at different levels of contrast, or how fast it can flicker before you don’t see a flicker anymore,” Dr. Kardon said. “The user sees spots that are flickering and just touches the ones they perceive to be flickering; they eliminate them by touching them.” When the test ends, the software “brackets what they did to a finer scale, and it finds the contrast at which that flicker wasn’t perceived anymore.”
2. The Landolt C visual acuity test. For this, the user must indicate the direction of the gap in the ring in a forced-choice task. “The user touches which arrow on the screen is pointing to where the location of the break in the Landolt C is perceived,” Dr. Kardon said. The Landolt C becomes progressively smaller until the location of the break can no longer be seen. “It’s pretty simple, and it finds the smallest size of the ‘C’ at which you’re making mistakes about 50% of the time, which is the threshold value for visual acuity,” he said.
3. Contrast sensitivity test at a fixed spatial frequency. “In this test, we fix the size of the letter to a large size, so spatial frequency is not at play, and we vary the contrast,” he said. “Users push the arrow wherever they see the break.” The contrast between the “C” and the background is sequentially reduced until a threshold is determined for the lowest contrast at which the location of the break in the “C” can still be observed.
4. Contrast sensitivity test at different spatial frequencies. This measure, also known as a vanishing optotype, is a line drawing of an object on a smooth, diffuse grayscale background. By altering the line properties used to define the shape of the vanishing optotype, one can vary its spatial frequency and contrast independent of target size. “This makes it an easy test because what the patient is asked to do is to touch wherever they see an object on the screen to eliminate it from the series of optotypes on the screen,” Dr. Kardon said. “The test is very fast, very intuitive.”
The researchers piloted use of these tests in a study of 104 age-matched control subjects and 117 MS patients. Of the 117 MS patients, 74 had a history of optic neuritis and 43 did not. The four tests were used in conjunction with standardized assessments, including the near-contrast acuity card test at 2.5%, the distant Early Treatment Diabetic Retinopathy Study (ETDRS) acuity test, as well as optical coherence tomography (OCT) of the retinal nerve fiber layer and ganglion cell layer thickness. Dr. Kardon and his colleagues found that when clinicians used a large target and varied the contrast, the test “did very well at differentiating normal from eyes with either previous optic neuritis or no previous optic neuritis,” he said. “It also differentiated eyes with previous optic neuritis and those with no optic neuritis. The visual acuity test didn’t perform as well because this is a near test. What we discovered afterward is that even at a fixed distance, many people who are presbyopic, or don’t have their optimal near correction, don’t do so well, because you’re testing spatial acuity. That’s a warning sign for future tests. You have to be careful as to how these are interpreted if they don’t have their best correction at near.”
Results from the critical flicker fusions tests were significant, except that they didn’t differentiate eyes affected by optic neuritis from those that weren’t. “The reason is that conduction was down in all of those eyes, so the combination of using contrast sensitivity and flicker fusion may not only help you diagnose MS, but whether that eye had been involved with optic neuritis before,” Dr. Kardon said. To date, he and his colleagues have completed technical validation of temporal frequency and contrast parameters. They’ve also completed preliminary investigations for determining test-retest variability, blurring effects, binocular summation effects, and quantification of normative ranges and abnormal subject data.
“A benefit of smartphone testing in MS is that visual dysfunction can be detected, leading to earlier interventions,” Dr. Kardon concluded. “We can study this on a time scale that wasn’t previously available. Wouldn’t you like to know on a daily or even a weekly basis what the fluctuations are in a home environment for MS patients? It’s low-cost, large-scale, and enables you to study genotype-phenotype comparisons.”
Going forward, Dr. Kardon and his colleagues have developed video cameras that go around the periphery of the iPad that can assess pupil and ocular motility, as well as eyelid and facial features in real time. He disclosed that he has received funding from the National Eye Institute, the Department of Defense, and from VA Rehabilitation Research and Development. He was also a member of the Novartis steering committee for the OCTiMS study and is a cofounder of MedFace and FaceX.
EXPERT ANALYSIS FROM ACTRIMS FORUM 2019
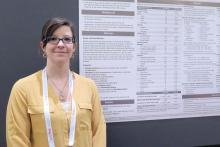
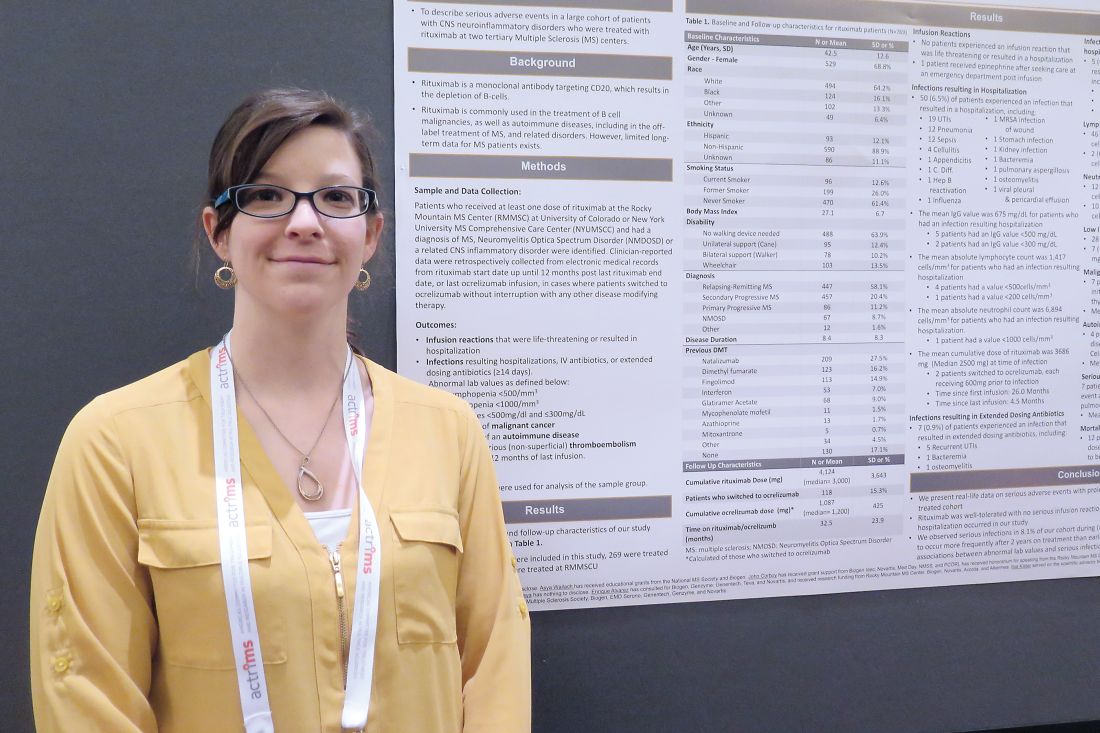
Study eyes serious adverse events from long-term rituximab use in MS
DALLAS – An analysis of two large cohorts treated with rituximab (Rituxan) showed that the rate of serious infections was 8.1%, yet no life-threatening infusion reactions occurred.
The finding comes from a retrospective chart review of 500 patients treated at the Rocky Mountain Multiple Sclerosis Center at the University of Colorado at Denver, Aurora, and 269 treated at the New York University Multiple Sclerosis Comprehensive Care Center.
At a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis, one of the study authors, Brandi L. Vollmer, MPH, noted that while rituximab is used off-label to treat multiple sclerosis (MS) and related disorders, limited long-term data for MS patients exist. Ms. Vollmer, a professional research assistant in the department of neurology in the division of neuroimmunology at the University of Colorado at Denver, and her associates identified all patients at the two MS centers who received at least one dose of rituximab. They reviewed patient charts from rituximab start date until 12 months after the last rituximab end date, or last ocrelizumab (Ocrevus) infusion in cases where patients switched to ocrelizumab without interruption with any other disease-modifying therapy. Data were abstracted from each chart using a case report form that systematically queried for demographic and clinical characteristics, serious adverse events, and significant laboratory abnormalities. The researchers used descriptive statistics to describe the sample group.
Key outcomes of interest were infusion reactions that were life-threatening or resulted in a hospitalization; infections that resulted in hospitalization, the need for IV antibiotics, or extended antibiotics; abnormal lab values; new diagnosis of malignant cancer; new diagnosis of autoimmune disease; diagnosis of serious thromboembolism; and mortality within 12 months of last infusion. At baseline, the mean age of the 769 patients was 43 years, 69% were female, 64% were white, and 16% were black. More than half (58%) had a diagnosis of relapsing-remitting MS, followed by secondary progressive MS (20%), primary progressive MS (11%), neuromyelitis optica spectrum disorder (9%), or other, and their mean disease duration was 8 years.
The researchers reported that the mean cumulative rituximab dose was 4,124 mg (median of 3,000 mg), the mean dose of ocrelizumab for ocrelizumab-switchers was 1,087 mg, and the mean time of follow-up was 33 months. Infections while on rituximab/ocrelizumab resulting in a hospitalization were observed in 50 patients (6.5%), which were primarily urinary tract infections (UTIs; 19 cases), pneumonia (12 cases), and sepsis (12 cases), while 7 patients (0.9%) experienced an infection that resulted in extended dosing antibiotics, including 5 recurrent UTIs, 1 case of bacteremia, and 1 case of osteomyelitis.
Ms. Vollmer and her colleagues also found that five patients (0.7%) experienced an infection that resulted in IV antibiotics without hospitalization, including one case each of pneumonia, cellulitis, UTI, infected wound, and aspiration pneumonia with respiratory syncytial virus. Serious de novo diagnoses while on rituximab were reported for 18 patients (2%), including autoimmune disease in 4, non-skin neoplasm in 7, and serious thromboembolic events in 7.
No patient experienced an infusion reaction requiring hospitalization. However, one patient received epinephrine after seeking care at an emergency department post infusion. Twelve patients (2%) died within 12 months of their last rituximab dose, although none were deemed by the treating clinician to be related to rituximab. Significant neutropenia was observed in 12 (2%), lymphopenia in 46 (6%), and IgG values below 500 mg/dL in 28 (4%).
“So far, this is just a descriptive analysis,” Ms. Vollmer said. “We want to look further into how abnormal lab values correlate with serious infections in particular.”
She acknowledged certain limitations of the study, including its retrospective design. Ms. Vollmer reported having no financial disclosures. Many of her coauthors reporting having numerous financial ties to the pharmaceutical industry.
SOURCE: Vollmer B et al. ACTRIMS Forum 2019, Poster 113
DALLAS – An analysis of two large cohorts treated with rituximab (Rituxan) showed that the rate of serious infections was 8.1%, yet no life-threatening infusion reactions occurred.
The finding comes from a retrospective chart review of 500 patients treated at the Rocky Mountain Multiple Sclerosis Center at the University of Colorado at Denver, Aurora, and 269 treated at the New York University Multiple Sclerosis Comprehensive Care Center.
At a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis, one of the study authors, Brandi L. Vollmer, MPH, noted that while rituximab is used off-label to treat multiple sclerosis (MS) and related disorders, limited long-term data for MS patients exist. Ms. Vollmer, a professional research assistant in the department of neurology in the division of neuroimmunology at the University of Colorado at Denver, and her associates identified all patients at the two MS centers who received at least one dose of rituximab. They reviewed patient charts from rituximab start date until 12 months after the last rituximab end date, or last ocrelizumab (Ocrevus) infusion in cases where patients switched to ocrelizumab without interruption with any other disease-modifying therapy. Data were abstracted from each chart using a case report form that systematically queried for demographic and clinical characteristics, serious adverse events, and significant laboratory abnormalities. The researchers used descriptive statistics to describe the sample group.
Key outcomes of interest were infusion reactions that were life-threatening or resulted in a hospitalization; infections that resulted in hospitalization, the need for IV antibiotics, or extended antibiotics; abnormal lab values; new diagnosis of malignant cancer; new diagnosis of autoimmune disease; diagnosis of serious thromboembolism; and mortality within 12 months of last infusion. At baseline, the mean age of the 769 patients was 43 years, 69% were female, 64% were white, and 16% were black. More than half (58%) had a diagnosis of relapsing-remitting MS, followed by secondary progressive MS (20%), primary progressive MS (11%), neuromyelitis optica spectrum disorder (9%), or other, and their mean disease duration was 8 years.
The researchers reported that the mean cumulative rituximab dose was 4,124 mg (median of 3,000 mg), the mean dose of ocrelizumab for ocrelizumab-switchers was 1,087 mg, and the mean time of follow-up was 33 months. Infections while on rituximab/ocrelizumab resulting in a hospitalization were observed in 50 patients (6.5%), which were primarily urinary tract infections (UTIs; 19 cases), pneumonia (12 cases), and sepsis (12 cases), while 7 patients (0.9%) experienced an infection that resulted in extended dosing antibiotics, including 5 recurrent UTIs, 1 case of bacteremia, and 1 case of osteomyelitis.
Ms. Vollmer and her colleagues also found that five patients (0.7%) experienced an infection that resulted in IV antibiotics without hospitalization, including one case each of pneumonia, cellulitis, UTI, infected wound, and aspiration pneumonia with respiratory syncytial virus. Serious de novo diagnoses while on rituximab were reported for 18 patients (2%), including autoimmune disease in 4, non-skin neoplasm in 7, and serious thromboembolic events in 7.
No patient experienced an infusion reaction requiring hospitalization. However, one patient received epinephrine after seeking care at an emergency department post infusion. Twelve patients (2%) died within 12 months of their last rituximab dose, although none were deemed by the treating clinician to be related to rituximab. Significant neutropenia was observed in 12 (2%), lymphopenia in 46 (6%), and IgG values below 500 mg/dL in 28 (4%).
“So far, this is just a descriptive analysis,” Ms. Vollmer said. “We want to look further into how abnormal lab values correlate with serious infections in particular.”
She acknowledged certain limitations of the study, including its retrospective design. Ms. Vollmer reported having no financial disclosures. Many of her coauthors reporting having numerous financial ties to the pharmaceutical industry.
SOURCE: Vollmer B et al. ACTRIMS Forum 2019, Poster 113
DALLAS – An analysis of two large cohorts treated with rituximab (Rituxan) showed that the rate of serious infections was 8.1%, yet no life-threatening infusion reactions occurred.
The finding comes from a retrospective chart review of 500 patients treated at the Rocky Mountain Multiple Sclerosis Center at the University of Colorado at Denver, Aurora, and 269 treated at the New York University Multiple Sclerosis Comprehensive Care Center.
At a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis, one of the study authors, Brandi L. Vollmer, MPH, noted that while rituximab is used off-label to treat multiple sclerosis (MS) and related disorders, limited long-term data for MS patients exist. Ms. Vollmer, a professional research assistant in the department of neurology in the division of neuroimmunology at the University of Colorado at Denver, and her associates identified all patients at the two MS centers who received at least one dose of rituximab. They reviewed patient charts from rituximab start date until 12 months after the last rituximab end date, or last ocrelizumab (Ocrevus) infusion in cases where patients switched to ocrelizumab without interruption with any other disease-modifying therapy. Data were abstracted from each chart using a case report form that systematically queried for demographic and clinical characteristics, serious adverse events, and significant laboratory abnormalities. The researchers used descriptive statistics to describe the sample group.
Key outcomes of interest were infusion reactions that were life-threatening or resulted in a hospitalization; infections that resulted in hospitalization, the need for IV antibiotics, or extended antibiotics; abnormal lab values; new diagnosis of malignant cancer; new diagnosis of autoimmune disease; diagnosis of serious thromboembolism; and mortality within 12 months of last infusion. At baseline, the mean age of the 769 patients was 43 years, 69% were female, 64% were white, and 16% were black. More than half (58%) had a diagnosis of relapsing-remitting MS, followed by secondary progressive MS (20%), primary progressive MS (11%), neuromyelitis optica spectrum disorder (9%), or other, and their mean disease duration was 8 years.
The researchers reported that the mean cumulative rituximab dose was 4,124 mg (median of 3,000 mg), the mean dose of ocrelizumab for ocrelizumab-switchers was 1,087 mg, and the mean time of follow-up was 33 months. Infections while on rituximab/ocrelizumab resulting in a hospitalization were observed in 50 patients (6.5%), which were primarily urinary tract infections (UTIs; 19 cases), pneumonia (12 cases), and sepsis (12 cases), while 7 patients (0.9%) experienced an infection that resulted in extended dosing antibiotics, including 5 recurrent UTIs, 1 case of bacteremia, and 1 case of osteomyelitis.
Ms. Vollmer and her colleagues also found that five patients (0.7%) experienced an infection that resulted in IV antibiotics without hospitalization, including one case each of pneumonia, cellulitis, UTI, infected wound, and aspiration pneumonia with respiratory syncytial virus. Serious de novo diagnoses while on rituximab were reported for 18 patients (2%), including autoimmune disease in 4, non-skin neoplasm in 7, and serious thromboembolic events in 7.
No patient experienced an infusion reaction requiring hospitalization. However, one patient received epinephrine after seeking care at an emergency department post infusion. Twelve patients (2%) died within 12 months of their last rituximab dose, although none were deemed by the treating clinician to be related to rituximab. Significant neutropenia was observed in 12 (2%), lymphopenia in 46 (6%), and IgG values below 500 mg/dL in 28 (4%).
“So far, this is just a descriptive analysis,” Ms. Vollmer said. “We want to look further into how abnormal lab values correlate with serious infections in particular.”
She acknowledged certain limitations of the study, including its retrospective design. Ms. Vollmer reported having no financial disclosures. Many of her coauthors reporting having numerous financial ties to the pharmaceutical industry.
SOURCE: Vollmer B et al. ACTRIMS Forum 2019, Poster 113
REPORTING FROM ACTRIMS 2019
Optical coherence tomography emerging as a promising biomarker for MS
DALLAS – Optical coherence tomography (OCT) has emerged as a promising biomarker in multiple sclerosis.
Thanks to OCT, clinicians are gaining an improved understanding of how MS affects certain eye structures. An optical analogue of ultrasound B mode imaging, OCT achieves a resolution of about 3-6 microns with commercially available devices. “That allows us to quantify the layers of the retina with quite a degree of accuracy,” Shiv Saidha, MD, said at ACTRIMS Forum 2019, the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
At postmortem, up to 99% of MS patients have demyelinated plaques in their optic nerves. “This implies that optic neuropathy is an ubiquitous phenomenon as part of the MS disease process,” said Dr. Saidha, a neurologist at Johns Hopkins University, Baltimore. “The prevailing hypothesis is that there is demyelination or axonal transection related to acute inflammation that occurs within the optic nerve. There’s a retrograde degeneration of its constituent axons, and that results in thinning of the inner retinal nerve fiber layer as well as the neuronal derivative of this layer called the ganglion cell layer. In addition to neurodegenerative mechanisms in the retina, there is also perivascular inflammation, called retinal periphlebitis, which we know occurs in about 20% of MS patients. At postmortem, there are also activate microglia present within the retina of MS patients.”
One of the principal findings of OCT in MS to date is that the retinal nerve fiber layer (RNFL) and ganglion cell plus inner plexiform layer (GCIP) thinning reflects MS-related optic nerve neurodegeneration. In addition, RNFL and GCIP thinning occur after optic neuritis and also as part of the MS disease course in eyes without a history of optic neuritis. “RNFL and GCIP thinning in MS are clinically relevant and correlate with visual function, global disability, and brain atrophy,” Dr. Saidha said. Researchers have also found that rates of GCIP thinning are accelerated in MS patients exhibiting clinical and/or radiological disease activity and are altered by disease-modifying therapies, and that increased inner nuclear layer (INL) thickness correlates with T2 lesion volume and predicts clinical and radiological disease activity. “In numerous trials of putatively neuroprotective and restorative treatments, we see OCT incorporated more and more, either as a secondary or a primary outcome,” he said.
Predicting disability and brain atrophy
In a study expected to be appear in a forthcoming issue of the Annals of Translational and Clinical Neurology, colleagues of Dr. Saidha found that OCT derived retinal layer measurements and visual function predict disability at 10 years in patients with MS. The researchers used an earlier generation, lower quality OCT device to examine tertiles of total macular volume, “an old, nonspecific composite measure of all of the retinal components,” he explained. “Even with inferior technology, a single measurement at a point in time not only could predict the change in EDSS [Expanded Disability Status Scale] scores from baseline to 10 years, but the accumulation of meaningful disability.”
In an earlier study, Dr. Saidha and his colleagues conducted a 4-year study of OCT and MRI in MS (Ann Neurol 2015; 78[5]:801-13). It consisted of six monthly spectral domain OCT scans (including automated intra-retinal segmentation) and baseline and annual 3 T brain MRI (including substructure volumetrics). Patients with ocular relapses (optic neuritis) during the study were excluded. The researchers correlated individual-specific rates of change in retinal and brain measurements, adjusting for age, sex, disease duration, and optic neuritis history. They found that cerebral volume fraction (analogous to whole brain volume) “had a decent correlation between rates of GCIP atrophy and rates of whole brain volume loss,” he said. “That was predominately driven by cortical gray matter atrophy.”
Measuring effects of disease-modifying therapies
What about the effects of disease-modifying therapies? According to Dr. Saidha, there has been a paucity of studies assessing the effects of DMTs on retinal layer thickness, and they are limited by small patient numbers, cross-sectional design, and/or short periods of observation. In a retrospective analysis, he and his associates examined the effects of treatments in relapsing-remitting MS patients at his center who underwent OCT (Neurology. 2017;88[6]:525-32). Over a mean 3 years of follow-up, they examined the effects of glatiramer acetate (Copaxone), natalizumab (Tysabri), and interferon beta-1a subcutaneously (Rebif) and intramuscularly (Avonex). They adjusted for gap time, which is the interval between when a patient started a treatment and when they started to undergo retinal observation with OCT. “This is to try to account for some of the biological changes that might have occurred during that period of time,” he explained. The researchers observed that rates of GCIP atrophy as well as other retinal measures were significantly lower in people treated with natalizumab, relative to all other DMTs. “What I found fascinating was the rate of GCIP atrophy of those on natalizumab was basically the same as healthy controls,” Dr. Saidha said. “It didn’t differ.”
Retinal inflammation and treatment’s impact
Significant inflammation in the unmyelinated retina may inform clinicians about other aspects of MS, he continued. For example, retinal periphlebitis occurs in about 20% of MS patients and may be a marker of CNS inflammation. In addition, intermediate uveitis occurs in about 16% of MS patients, and postmortem studies reveal retinal inflammation with microglia. Specifically, macular microcystoid changes occur in the eyes of about 5% of MS patients and may represent a breakdown of the blood-retinal barrier and inflammation. “Since it’s a dynamic process, increased thickness of the INL in the absence of visible microcystoid changes might occur,” Dr. Saidha said. “We found that baseline INL thickness is predictive of clinico-radiologic disease activity.”
In a separate analysis of 108 MS patients and 40 healthy controls, German researchers evaluated the impact of DMTs on INL volume (Brain. 2016;11[1]:2855-63). They found that higher baseline INL volume correlated with new T2 and GAD lesions over 1 year. The reduction in INL volume was significantly associated with reduced activity, and overall, DMTs reduced INL volume over 6 months. Patients who were not treated, or who were treated and did not achieve NEDA-3 (no evidence of disease activity) did not show reductions in INL volume. They concluded that INL volume might be a novel outcome of DMT treatment.
Finding prognostic and diagnostic biomarkers
In an ongoing multisite study, Dr. Saidha and his colleagues are assessing the use of OCT in patients with progressive MS (including 186 patients from Johns Hopkins), and also determining if OCT changes differ over time between relapsing-remitting MS and different subtypes of progressive MS. So far, they have found that progressive MS is associated with accelerated inner and in particular outer layer retinal atrophy. “Although this is a decent-sized cohort, at this stage I’m not sure I would definitively say that these novel retinal biomarkers have utility specific to progressive MS, but I’m very excited about it,” he said. “The goal is to take a much deeper look at this.”
Findings from a large collaborative IMSVISUAL inter-eye asymmetry study showed that peripapillary RNFL and ganglion cell–inner plexiform layer inter-eye differences of 5 microns, respectively, were optimal for identifying patients with prior unilateral optic neuritis in the MS cohort. “In the future, the possibility of using OCT to identify subclinical optic neuropathy so we can define when a lesion is present in the optic nerve has huge diagnostic implications for MS, because the optic nerve is not currently recognized as a lesion site in current MS diagnostic criteria,” Dr. Saidha said.
Dr. Saidha disclosed that he has served on scientific advisory boards for Biogen, Genzyme, Genentech, EMD Serono, and Novartis. He has also received consulting fees from JuneBrain LLC and is the site investigator of a trial sponsored by MedDay Pharmaceuticals.
DALLAS – Optical coherence tomography (OCT) has emerged as a promising biomarker in multiple sclerosis.
Thanks to OCT, clinicians are gaining an improved understanding of how MS affects certain eye structures. An optical analogue of ultrasound B mode imaging, OCT achieves a resolution of about 3-6 microns with commercially available devices. “That allows us to quantify the layers of the retina with quite a degree of accuracy,” Shiv Saidha, MD, said at ACTRIMS Forum 2019, the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
At postmortem, up to 99% of MS patients have demyelinated plaques in their optic nerves. “This implies that optic neuropathy is an ubiquitous phenomenon as part of the MS disease process,” said Dr. Saidha, a neurologist at Johns Hopkins University, Baltimore. “The prevailing hypothesis is that there is demyelination or axonal transection related to acute inflammation that occurs within the optic nerve. There’s a retrograde degeneration of its constituent axons, and that results in thinning of the inner retinal nerve fiber layer as well as the neuronal derivative of this layer called the ganglion cell layer. In addition to neurodegenerative mechanisms in the retina, there is also perivascular inflammation, called retinal periphlebitis, which we know occurs in about 20% of MS patients. At postmortem, there are also activate microglia present within the retina of MS patients.”
One of the principal findings of OCT in MS to date is that the retinal nerve fiber layer (RNFL) and ganglion cell plus inner plexiform layer (GCIP) thinning reflects MS-related optic nerve neurodegeneration. In addition, RNFL and GCIP thinning occur after optic neuritis and also as part of the MS disease course in eyes without a history of optic neuritis. “RNFL and GCIP thinning in MS are clinically relevant and correlate with visual function, global disability, and brain atrophy,” Dr. Saidha said. Researchers have also found that rates of GCIP thinning are accelerated in MS patients exhibiting clinical and/or radiological disease activity and are altered by disease-modifying therapies, and that increased inner nuclear layer (INL) thickness correlates with T2 lesion volume and predicts clinical and radiological disease activity. “In numerous trials of putatively neuroprotective and restorative treatments, we see OCT incorporated more and more, either as a secondary or a primary outcome,” he said.
Predicting disability and brain atrophy
In a study expected to be appear in a forthcoming issue of the Annals of Translational and Clinical Neurology, colleagues of Dr. Saidha found that OCT derived retinal layer measurements and visual function predict disability at 10 years in patients with MS. The researchers used an earlier generation, lower quality OCT device to examine tertiles of total macular volume, “an old, nonspecific composite measure of all of the retinal components,” he explained. “Even with inferior technology, a single measurement at a point in time not only could predict the change in EDSS [Expanded Disability Status Scale] scores from baseline to 10 years, but the accumulation of meaningful disability.”
In an earlier study, Dr. Saidha and his colleagues conducted a 4-year study of OCT and MRI in MS (Ann Neurol 2015; 78[5]:801-13). It consisted of six monthly spectral domain OCT scans (including automated intra-retinal segmentation) and baseline and annual 3 T brain MRI (including substructure volumetrics). Patients with ocular relapses (optic neuritis) during the study were excluded. The researchers correlated individual-specific rates of change in retinal and brain measurements, adjusting for age, sex, disease duration, and optic neuritis history. They found that cerebral volume fraction (analogous to whole brain volume) “had a decent correlation between rates of GCIP atrophy and rates of whole brain volume loss,” he said. “That was predominately driven by cortical gray matter atrophy.”
Measuring effects of disease-modifying therapies
What about the effects of disease-modifying therapies? According to Dr. Saidha, there has been a paucity of studies assessing the effects of DMTs on retinal layer thickness, and they are limited by small patient numbers, cross-sectional design, and/or short periods of observation. In a retrospective analysis, he and his associates examined the effects of treatments in relapsing-remitting MS patients at his center who underwent OCT (Neurology. 2017;88[6]:525-32). Over a mean 3 years of follow-up, they examined the effects of glatiramer acetate (Copaxone), natalizumab (Tysabri), and interferon beta-1a subcutaneously (Rebif) and intramuscularly (Avonex). They adjusted for gap time, which is the interval between when a patient started a treatment and when they started to undergo retinal observation with OCT. “This is to try to account for some of the biological changes that might have occurred during that period of time,” he explained. The researchers observed that rates of GCIP atrophy as well as other retinal measures were significantly lower in people treated with natalizumab, relative to all other DMTs. “What I found fascinating was the rate of GCIP atrophy of those on natalizumab was basically the same as healthy controls,” Dr. Saidha said. “It didn’t differ.”
Retinal inflammation and treatment’s impact
Significant inflammation in the unmyelinated retina may inform clinicians about other aspects of MS, he continued. For example, retinal periphlebitis occurs in about 20% of MS patients and may be a marker of CNS inflammation. In addition, intermediate uveitis occurs in about 16% of MS patients, and postmortem studies reveal retinal inflammation with microglia. Specifically, macular microcystoid changes occur in the eyes of about 5% of MS patients and may represent a breakdown of the blood-retinal barrier and inflammation. “Since it’s a dynamic process, increased thickness of the INL in the absence of visible microcystoid changes might occur,” Dr. Saidha said. “We found that baseline INL thickness is predictive of clinico-radiologic disease activity.”
In a separate analysis of 108 MS patients and 40 healthy controls, German researchers evaluated the impact of DMTs on INL volume (Brain. 2016;11[1]:2855-63). They found that higher baseline INL volume correlated with new T2 and GAD lesions over 1 year. The reduction in INL volume was significantly associated with reduced activity, and overall, DMTs reduced INL volume over 6 months. Patients who were not treated, or who were treated and did not achieve NEDA-3 (no evidence of disease activity) did not show reductions in INL volume. They concluded that INL volume might be a novel outcome of DMT treatment.
Finding prognostic and diagnostic biomarkers
In an ongoing multisite study, Dr. Saidha and his colleagues are assessing the use of OCT in patients with progressive MS (including 186 patients from Johns Hopkins), and also determining if OCT changes differ over time between relapsing-remitting MS and different subtypes of progressive MS. So far, they have found that progressive MS is associated with accelerated inner and in particular outer layer retinal atrophy. “Although this is a decent-sized cohort, at this stage I’m not sure I would definitively say that these novel retinal biomarkers have utility specific to progressive MS, but I’m very excited about it,” he said. “The goal is to take a much deeper look at this.”
Findings from a large collaborative IMSVISUAL inter-eye asymmetry study showed that peripapillary RNFL and ganglion cell–inner plexiform layer inter-eye differences of 5 microns, respectively, were optimal for identifying patients with prior unilateral optic neuritis in the MS cohort. “In the future, the possibility of using OCT to identify subclinical optic neuropathy so we can define when a lesion is present in the optic nerve has huge diagnostic implications for MS, because the optic nerve is not currently recognized as a lesion site in current MS diagnostic criteria,” Dr. Saidha said.
Dr. Saidha disclosed that he has served on scientific advisory boards for Biogen, Genzyme, Genentech, EMD Serono, and Novartis. He has also received consulting fees from JuneBrain LLC and is the site investigator of a trial sponsored by MedDay Pharmaceuticals.
DALLAS – Optical coherence tomography (OCT) has emerged as a promising biomarker in multiple sclerosis.
Thanks to OCT, clinicians are gaining an improved understanding of how MS affects certain eye structures. An optical analogue of ultrasound B mode imaging, OCT achieves a resolution of about 3-6 microns with commercially available devices. “That allows us to quantify the layers of the retina with quite a degree of accuracy,” Shiv Saidha, MD, said at ACTRIMS Forum 2019, the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
At postmortem, up to 99% of MS patients have demyelinated plaques in their optic nerves. “This implies that optic neuropathy is an ubiquitous phenomenon as part of the MS disease process,” said Dr. Saidha, a neurologist at Johns Hopkins University, Baltimore. “The prevailing hypothesis is that there is demyelination or axonal transection related to acute inflammation that occurs within the optic nerve. There’s a retrograde degeneration of its constituent axons, and that results in thinning of the inner retinal nerve fiber layer as well as the neuronal derivative of this layer called the ganglion cell layer. In addition to neurodegenerative mechanisms in the retina, there is also perivascular inflammation, called retinal periphlebitis, which we know occurs in about 20% of MS patients. At postmortem, there are also activate microglia present within the retina of MS patients.”
One of the principal findings of OCT in MS to date is that the retinal nerve fiber layer (RNFL) and ganglion cell plus inner plexiform layer (GCIP) thinning reflects MS-related optic nerve neurodegeneration. In addition, RNFL and GCIP thinning occur after optic neuritis and also as part of the MS disease course in eyes without a history of optic neuritis. “RNFL and GCIP thinning in MS are clinically relevant and correlate with visual function, global disability, and brain atrophy,” Dr. Saidha said. Researchers have also found that rates of GCIP thinning are accelerated in MS patients exhibiting clinical and/or radiological disease activity and are altered by disease-modifying therapies, and that increased inner nuclear layer (INL) thickness correlates with T2 lesion volume and predicts clinical and radiological disease activity. “In numerous trials of putatively neuroprotective and restorative treatments, we see OCT incorporated more and more, either as a secondary or a primary outcome,” he said.
Predicting disability and brain atrophy
In a study expected to be appear in a forthcoming issue of the Annals of Translational and Clinical Neurology, colleagues of Dr. Saidha found that OCT derived retinal layer measurements and visual function predict disability at 10 years in patients with MS. The researchers used an earlier generation, lower quality OCT device to examine tertiles of total macular volume, “an old, nonspecific composite measure of all of the retinal components,” he explained. “Even with inferior technology, a single measurement at a point in time not only could predict the change in EDSS [Expanded Disability Status Scale] scores from baseline to 10 years, but the accumulation of meaningful disability.”
In an earlier study, Dr. Saidha and his colleagues conducted a 4-year study of OCT and MRI in MS (Ann Neurol 2015; 78[5]:801-13). It consisted of six monthly spectral domain OCT scans (including automated intra-retinal segmentation) and baseline and annual 3 T brain MRI (including substructure volumetrics). Patients with ocular relapses (optic neuritis) during the study were excluded. The researchers correlated individual-specific rates of change in retinal and brain measurements, adjusting for age, sex, disease duration, and optic neuritis history. They found that cerebral volume fraction (analogous to whole brain volume) “had a decent correlation between rates of GCIP atrophy and rates of whole brain volume loss,” he said. “That was predominately driven by cortical gray matter atrophy.”
Measuring effects of disease-modifying therapies
What about the effects of disease-modifying therapies? According to Dr. Saidha, there has been a paucity of studies assessing the effects of DMTs on retinal layer thickness, and they are limited by small patient numbers, cross-sectional design, and/or short periods of observation. In a retrospective analysis, he and his associates examined the effects of treatments in relapsing-remitting MS patients at his center who underwent OCT (Neurology. 2017;88[6]:525-32). Over a mean 3 years of follow-up, they examined the effects of glatiramer acetate (Copaxone), natalizumab (Tysabri), and interferon beta-1a subcutaneously (Rebif) and intramuscularly (Avonex). They adjusted for gap time, which is the interval between when a patient started a treatment and when they started to undergo retinal observation with OCT. “This is to try to account for some of the biological changes that might have occurred during that period of time,” he explained. The researchers observed that rates of GCIP atrophy as well as other retinal measures were significantly lower in people treated with natalizumab, relative to all other DMTs. “What I found fascinating was the rate of GCIP atrophy of those on natalizumab was basically the same as healthy controls,” Dr. Saidha said. “It didn’t differ.”
Retinal inflammation and treatment’s impact
Significant inflammation in the unmyelinated retina may inform clinicians about other aspects of MS, he continued. For example, retinal periphlebitis occurs in about 20% of MS patients and may be a marker of CNS inflammation. In addition, intermediate uveitis occurs in about 16% of MS patients, and postmortem studies reveal retinal inflammation with microglia. Specifically, macular microcystoid changes occur in the eyes of about 5% of MS patients and may represent a breakdown of the blood-retinal barrier and inflammation. “Since it’s a dynamic process, increased thickness of the INL in the absence of visible microcystoid changes might occur,” Dr. Saidha said. “We found that baseline INL thickness is predictive of clinico-radiologic disease activity.”
In a separate analysis of 108 MS patients and 40 healthy controls, German researchers evaluated the impact of DMTs on INL volume (Brain. 2016;11[1]:2855-63). They found that higher baseline INL volume correlated with new T2 and GAD lesions over 1 year. The reduction in INL volume was significantly associated with reduced activity, and overall, DMTs reduced INL volume over 6 months. Patients who were not treated, or who were treated and did not achieve NEDA-3 (no evidence of disease activity) did not show reductions in INL volume. They concluded that INL volume might be a novel outcome of DMT treatment.
Finding prognostic and diagnostic biomarkers
In an ongoing multisite study, Dr. Saidha and his colleagues are assessing the use of OCT in patients with progressive MS (including 186 patients from Johns Hopkins), and also determining if OCT changes differ over time between relapsing-remitting MS and different subtypes of progressive MS. So far, they have found that progressive MS is associated with accelerated inner and in particular outer layer retinal atrophy. “Although this is a decent-sized cohort, at this stage I’m not sure I would definitively say that these novel retinal biomarkers have utility specific to progressive MS, but I’m very excited about it,” he said. “The goal is to take a much deeper look at this.”
Findings from a large collaborative IMSVISUAL inter-eye asymmetry study showed that peripapillary RNFL and ganglion cell–inner plexiform layer inter-eye differences of 5 microns, respectively, were optimal for identifying patients with prior unilateral optic neuritis in the MS cohort. “In the future, the possibility of using OCT to identify subclinical optic neuropathy so we can define when a lesion is present in the optic nerve has huge diagnostic implications for MS, because the optic nerve is not currently recognized as a lesion site in current MS diagnostic criteria,” Dr. Saidha said.
Dr. Saidha disclosed that he has served on scientific advisory boards for Biogen, Genzyme, Genentech, EMD Serono, and Novartis. He has also received consulting fees from JuneBrain LLC and is the site investigator of a trial sponsored by MedDay Pharmaceuticals.
EXPERT ANALYSIS FROM ACTRIMS FORUM 2019
Survey of MS patients reveals numerous pregnancy-related concerns
DALLAS – When it comes to family planning and pregnancy-related decisions such as breastfeeding and medication management, patients with multiple sclerosis (MS) receive a wide variety of advice, guidance, and engagement from their health care providers, results from a single-center survey demonstrated.
“We want our patients to feel comfortable when they come to us in their 20s or 30s and they get diagnosed, they’re scared, and it’s all new to them,” one of the study authors, Casey E. Engel said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We want them to know that family planning is something to consider and that they can proceed with having a family with our help and guidance.”
In an effort to collect patient-experience data around family planning, pregnancy, and breastfeeding post-MS diagnosis, Ms. Engel and senior author Myla D. Goldman, MD, mailed a survey to 1,000 women with confirmed MS diagnosis who had received care at the University of Virginia Medical Center in Charlottesville. The researchers reported findings from 173 respondents, of whom 70% were receiving specialty care for MS. Most of the survey participants (137) did not become pregnant following their diagnosis, while 36 did.
Of the 137 respondents who did not become pregnant following diagnosis, 22 (16%) indicated that their decision was driven by MS-related concerns, including MS worsening with pregnancy (64%), ability to care for child secondary to MS (46%), lack of knowledge about options for pregnancy and MS (18%), passing MS onto child (18%), and stopping disease-modifying therapy (DMT) to attempt pregnancy (9%).
Of the 36 women who had a pregnancy following diagnosis, 20% reported postpartum depression or anxiety, higher than the national average of 10%-15%. In addition, 79% reported not being on DMT at the time of conception, 9% were on either glatiramer acetate injection or interferon beta-1a at time of conception, and 3% were on fingolimod (Gilenya) at time of conception. The majority reported receiving inconsistent advice about when to discontinue DMT before attempting pregnancy (a range from 0 to 6 months).
“It’s also noteworthy that 20% took a year to achieve pregnancy,” said Dr. Goldman, a neurologist who directs the university’s MS clinic. “If these women stop [their DMT] 6 months in advance and they take a year to achieve pregnancy, that’s 18 months without therapeutic coverage. That’s a concern to bring to light.”
Breastfeeding was reported in 71% of mothers in postdiagnosis pregnancy with a range between 1 week and 10 months, driven in part by variable guidelines regarding DMT reinitiation. In the meantime, respondents who did not breastfeed made this decision due to fear of relapse, glucocorticoids, or desire to reinitiate medication.
“Though our study was limited by low survey response, we hope that our work may highlight the difficulty our patients face and foster discussions within the MS community around these issues to improve the individual patient experience,” the researchers wrote in their poster.
Ms. Engel worked on the study while an undergraduate at the University of Virginia. The study was supported by the ziMS Foundation.
SOURCE: Engel CE et al. ACTRIMS Forum 2019, Poster 307.
DALLAS – When it comes to family planning and pregnancy-related decisions such as breastfeeding and medication management, patients with multiple sclerosis (MS) receive a wide variety of advice, guidance, and engagement from their health care providers, results from a single-center survey demonstrated.
“We want our patients to feel comfortable when they come to us in their 20s or 30s and they get diagnosed, they’re scared, and it’s all new to them,” one of the study authors, Casey E. Engel said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We want them to know that family planning is something to consider and that they can proceed with having a family with our help and guidance.”
In an effort to collect patient-experience data around family planning, pregnancy, and breastfeeding post-MS diagnosis, Ms. Engel and senior author Myla D. Goldman, MD, mailed a survey to 1,000 women with confirmed MS diagnosis who had received care at the University of Virginia Medical Center in Charlottesville. The researchers reported findings from 173 respondents, of whom 70% were receiving specialty care for MS. Most of the survey participants (137) did not become pregnant following their diagnosis, while 36 did.
Of the 137 respondents who did not become pregnant following diagnosis, 22 (16%) indicated that their decision was driven by MS-related concerns, including MS worsening with pregnancy (64%), ability to care for child secondary to MS (46%), lack of knowledge about options for pregnancy and MS (18%), passing MS onto child (18%), and stopping disease-modifying therapy (DMT) to attempt pregnancy (9%).
Of the 36 women who had a pregnancy following diagnosis, 20% reported postpartum depression or anxiety, higher than the national average of 10%-15%. In addition, 79% reported not being on DMT at the time of conception, 9% were on either glatiramer acetate injection or interferon beta-1a at time of conception, and 3% were on fingolimod (Gilenya) at time of conception. The majority reported receiving inconsistent advice about when to discontinue DMT before attempting pregnancy (a range from 0 to 6 months).
“It’s also noteworthy that 20% took a year to achieve pregnancy,” said Dr. Goldman, a neurologist who directs the university’s MS clinic. “If these women stop [their DMT] 6 months in advance and they take a year to achieve pregnancy, that’s 18 months without therapeutic coverage. That’s a concern to bring to light.”
Breastfeeding was reported in 71% of mothers in postdiagnosis pregnancy with a range between 1 week and 10 months, driven in part by variable guidelines regarding DMT reinitiation. In the meantime, respondents who did not breastfeed made this decision due to fear of relapse, glucocorticoids, or desire to reinitiate medication.
“Though our study was limited by low survey response, we hope that our work may highlight the difficulty our patients face and foster discussions within the MS community around these issues to improve the individual patient experience,” the researchers wrote in their poster.
Ms. Engel worked on the study while an undergraduate at the University of Virginia. The study was supported by the ziMS Foundation.
SOURCE: Engel CE et al. ACTRIMS Forum 2019, Poster 307.
DALLAS – When it comes to family planning and pregnancy-related decisions such as breastfeeding and medication management, patients with multiple sclerosis (MS) receive a wide variety of advice, guidance, and engagement from their health care providers, results from a single-center survey demonstrated.
“We want our patients to feel comfortable when they come to us in their 20s or 30s and they get diagnosed, they’re scared, and it’s all new to them,” one of the study authors, Casey E. Engel said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We want them to know that family planning is something to consider and that they can proceed with having a family with our help and guidance.”
In an effort to collect patient-experience data around family planning, pregnancy, and breastfeeding post-MS diagnosis, Ms. Engel and senior author Myla D. Goldman, MD, mailed a survey to 1,000 women with confirmed MS diagnosis who had received care at the University of Virginia Medical Center in Charlottesville. The researchers reported findings from 173 respondents, of whom 70% were receiving specialty care for MS. Most of the survey participants (137) did not become pregnant following their diagnosis, while 36 did.
Of the 137 respondents who did not become pregnant following diagnosis, 22 (16%) indicated that their decision was driven by MS-related concerns, including MS worsening with pregnancy (64%), ability to care for child secondary to MS (46%), lack of knowledge about options for pregnancy and MS (18%), passing MS onto child (18%), and stopping disease-modifying therapy (DMT) to attempt pregnancy (9%).
Of the 36 women who had a pregnancy following diagnosis, 20% reported postpartum depression or anxiety, higher than the national average of 10%-15%. In addition, 79% reported not being on DMT at the time of conception, 9% were on either glatiramer acetate injection or interferon beta-1a at time of conception, and 3% were on fingolimod (Gilenya) at time of conception. The majority reported receiving inconsistent advice about when to discontinue DMT before attempting pregnancy (a range from 0 to 6 months).
“It’s also noteworthy that 20% took a year to achieve pregnancy,” said Dr. Goldman, a neurologist who directs the university’s MS clinic. “If these women stop [their DMT] 6 months in advance and they take a year to achieve pregnancy, that’s 18 months without therapeutic coverage. That’s a concern to bring to light.”
Breastfeeding was reported in 71% of mothers in postdiagnosis pregnancy with a range between 1 week and 10 months, driven in part by variable guidelines regarding DMT reinitiation. In the meantime, respondents who did not breastfeed made this decision due to fear of relapse, glucocorticoids, or desire to reinitiate medication.
“Though our study was limited by low survey response, we hope that our work may highlight the difficulty our patients face and foster discussions within the MS community around these issues to improve the individual patient experience,” the researchers wrote in their poster.
Ms. Engel worked on the study while an undergraduate at the University of Virginia. The study was supported by the ziMS Foundation.
SOURCE: Engel CE et al. ACTRIMS Forum 2019, Poster 307.
REPORTING FROM ACTRIMS FORUM 2019
Teriflunomide transmission can occur in female partners of men taking the drug
DALLAS – Low or undetectable levels of teriflunomide (Aubagio) occur in women who are sexually active with men taking the drug for relapsing multiple sclerosis, results from a small study demonstrated.
“One of the issues with this particular drug is that it carries a strong pregnancy warning because in animal studies the drug has been teratogenic,” Joseph B. Guarnaccia, MD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “The other issue is that it remains detectable in the body for some time. The issue of females taking this drug and conception are well known. There are strong warnings that, if a woman wants to become pregnant, the drug should be removed quickly from the system. But if their male partner is on the drug, does that pose a risk to their female partner? That question has never been addressed in a human study.”
The Food and Drug Administration prescribing information recommends that men wishing to father a child should discontinue use of teriflunomide and undergo the accelerated elimination procedure. It also recommends that female partners wishing to become pregnant should discontinue the drug and undergo an accelerated elimination procedure to verify that the plasma teriflunomide concentration is less than 0.020 mcg/mL.
In an effort to test the risk of female exposure to potentially teratogenic levels of teriflunomide through sexual intercourse, Dr. Guarnaccia, a neurologist with the Multiple Sclerosis Treatment Center at Griffin Hospital in Derby, Conn., and his colleagues recruited 10 couples and compared serum levels of teriflunomide in men with relapsing multiple sclerosis with those of their female partners. Enrollment criteria for men included a diagnosis of relapsing multiple sclerosis, age between 18 and 55 years, treatment with teriflunomide for at least 2 months prior to study entry, and frequency of sexual intercourse with their female partners at least twice a month. Pregnancy was excluded in females, and couples could not use barrier or withdrawal methods of contraception. The couples completed a brief questionnaire and underwent a one-time blood draw for teriflunomide levels either at the investigator’s office or at a LabCorp facility.
The mean age of study participants was 47 years and the mean frequency of intercourse was seven episodes per month. The mean teriflunomide concentration in men was 42.30 mcg/mL (ranged from 10.07 to 142.84 mcg/mL). Six women had teriflunomide below detection levels (0.020 mcg/mL). However, four women had detectable levels that averaged 0.045 mcg/mL (ranging from 0.022 to 0.077 mcg/mL).
“This small study demonstrates that low or undetectable levels of teriflunomide occur in females who are sexually active with males taking teriflunomide for relapsing multiple sclerosis,” the researchers wrote in their poster. They found that women who had low detectable levels of teriflunomide, compared with women with undetectable levels, did not engage in more frequent sexual intercourse nor were their levels associated with higher levels of teriflunomide in their male partners.
“Indeed, one might have expected a positive correlation between serum levels of teriflunomide in females and the frequency or concentration of inoculation in semen from their partners,” the researchers wrote. “While semen levels of teriflunomide were not measured in this study, it might be assumed that serum and semen concentrations of small molecules like teriflunomide are similar.”
The study was supported by a investigator-sponsored research grant from Sanofi-Genzyme. Dr. Guarnaccia reported that he has received speaking honoraria and educational grants from Sanofi-Genzyme, Biogen, Teva, Acorda Therapeutics, Bayer, EMD Serono, and Genentech.
SOURCE: Guarnaccia JB et al. ACTRIMS Forum 2019, Poster 115.
DALLAS – Low or undetectable levels of teriflunomide (Aubagio) occur in women who are sexually active with men taking the drug for relapsing multiple sclerosis, results from a small study demonstrated.
“One of the issues with this particular drug is that it carries a strong pregnancy warning because in animal studies the drug has been teratogenic,” Joseph B. Guarnaccia, MD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “The other issue is that it remains detectable in the body for some time. The issue of females taking this drug and conception are well known. There are strong warnings that, if a woman wants to become pregnant, the drug should be removed quickly from the system. But if their male partner is on the drug, does that pose a risk to their female partner? That question has never been addressed in a human study.”
The Food and Drug Administration prescribing information recommends that men wishing to father a child should discontinue use of teriflunomide and undergo the accelerated elimination procedure. It also recommends that female partners wishing to become pregnant should discontinue the drug and undergo an accelerated elimination procedure to verify that the plasma teriflunomide concentration is less than 0.020 mcg/mL.
In an effort to test the risk of female exposure to potentially teratogenic levels of teriflunomide through sexual intercourse, Dr. Guarnaccia, a neurologist with the Multiple Sclerosis Treatment Center at Griffin Hospital in Derby, Conn., and his colleagues recruited 10 couples and compared serum levels of teriflunomide in men with relapsing multiple sclerosis with those of their female partners. Enrollment criteria for men included a diagnosis of relapsing multiple sclerosis, age between 18 and 55 years, treatment with teriflunomide for at least 2 months prior to study entry, and frequency of sexual intercourse with their female partners at least twice a month. Pregnancy was excluded in females, and couples could not use barrier or withdrawal methods of contraception. The couples completed a brief questionnaire and underwent a one-time blood draw for teriflunomide levels either at the investigator’s office or at a LabCorp facility.
The mean age of study participants was 47 years and the mean frequency of intercourse was seven episodes per month. The mean teriflunomide concentration in men was 42.30 mcg/mL (ranged from 10.07 to 142.84 mcg/mL). Six women had teriflunomide below detection levels (0.020 mcg/mL). However, four women had detectable levels that averaged 0.045 mcg/mL (ranging from 0.022 to 0.077 mcg/mL).
“This small study demonstrates that low or undetectable levels of teriflunomide occur in females who are sexually active with males taking teriflunomide for relapsing multiple sclerosis,” the researchers wrote in their poster. They found that women who had low detectable levels of teriflunomide, compared with women with undetectable levels, did not engage in more frequent sexual intercourse nor were their levels associated with higher levels of teriflunomide in their male partners.
“Indeed, one might have expected a positive correlation between serum levels of teriflunomide in females and the frequency or concentration of inoculation in semen from their partners,” the researchers wrote. “While semen levels of teriflunomide were not measured in this study, it might be assumed that serum and semen concentrations of small molecules like teriflunomide are similar.”
The study was supported by a investigator-sponsored research grant from Sanofi-Genzyme. Dr. Guarnaccia reported that he has received speaking honoraria and educational grants from Sanofi-Genzyme, Biogen, Teva, Acorda Therapeutics, Bayer, EMD Serono, and Genentech.
SOURCE: Guarnaccia JB et al. ACTRIMS Forum 2019, Poster 115.
DALLAS – Low or undetectable levels of teriflunomide (Aubagio) occur in women who are sexually active with men taking the drug for relapsing multiple sclerosis, results from a small study demonstrated.
“One of the issues with this particular drug is that it carries a strong pregnancy warning because in animal studies the drug has been teratogenic,” Joseph B. Guarnaccia, MD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “The other issue is that it remains detectable in the body for some time. The issue of females taking this drug and conception are well known. There are strong warnings that, if a woman wants to become pregnant, the drug should be removed quickly from the system. But if their male partner is on the drug, does that pose a risk to their female partner? That question has never been addressed in a human study.”
The Food and Drug Administration prescribing information recommends that men wishing to father a child should discontinue use of teriflunomide and undergo the accelerated elimination procedure. It also recommends that female partners wishing to become pregnant should discontinue the drug and undergo an accelerated elimination procedure to verify that the plasma teriflunomide concentration is less than 0.020 mcg/mL.
In an effort to test the risk of female exposure to potentially teratogenic levels of teriflunomide through sexual intercourse, Dr. Guarnaccia, a neurologist with the Multiple Sclerosis Treatment Center at Griffin Hospital in Derby, Conn., and his colleagues recruited 10 couples and compared serum levels of teriflunomide in men with relapsing multiple sclerosis with those of their female partners. Enrollment criteria for men included a diagnosis of relapsing multiple sclerosis, age between 18 and 55 years, treatment with teriflunomide for at least 2 months prior to study entry, and frequency of sexual intercourse with their female partners at least twice a month. Pregnancy was excluded in females, and couples could not use barrier or withdrawal methods of contraception. The couples completed a brief questionnaire and underwent a one-time blood draw for teriflunomide levels either at the investigator’s office or at a LabCorp facility.
The mean age of study participants was 47 years and the mean frequency of intercourse was seven episodes per month. The mean teriflunomide concentration in men was 42.30 mcg/mL (ranged from 10.07 to 142.84 mcg/mL). Six women had teriflunomide below detection levels (0.020 mcg/mL). However, four women had detectable levels that averaged 0.045 mcg/mL (ranging from 0.022 to 0.077 mcg/mL).
“This small study demonstrates that low or undetectable levels of teriflunomide occur in females who are sexually active with males taking teriflunomide for relapsing multiple sclerosis,” the researchers wrote in their poster. They found that women who had low detectable levels of teriflunomide, compared with women with undetectable levels, did not engage in more frequent sexual intercourse nor were their levels associated with higher levels of teriflunomide in their male partners.
“Indeed, one might have expected a positive correlation between serum levels of teriflunomide in females and the frequency or concentration of inoculation in semen from their partners,” the researchers wrote. “While semen levels of teriflunomide were not measured in this study, it might be assumed that serum and semen concentrations of small molecules like teriflunomide are similar.”
The study was supported by a investigator-sponsored research grant from Sanofi-Genzyme. Dr. Guarnaccia reported that he has received speaking honoraria and educational grants from Sanofi-Genzyme, Biogen, Teva, Acorda Therapeutics, Bayer, EMD Serono, and Genentech.
SOURCE: Guarnaccia JB et al. ACTRIMS Forum 2019, Poster 115.
REPORTING FROM ACTRIMS FORUM 2019
Neurologists grappling with patients who embrace ‘stem cell tourism’
DALLAS – Stem cell tourism – the unethical practice of offering unproven cellular preparations to patients for a variety of conditions – is increasingly sought by patients with incurable conditions such as multiple sclerosis and amyotrophic lateral sclerosis, results from a novel survey suggest.
In fact, most academic neurologists have been approached by patients with incurable conditions who ask them about stem cell therapy, while about two-thirds have had at least one patient who has undergone stem cell therapy.
“It’s really scary,” Wijdan Rai, MBBS, the study’s first author, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “This is a more prevalent issue than we think, and the complication rates are higher than we think.”
According to the study’s senior author, Jaime Imitola, MD, who directs the Progressive Multiple Sclerosis Multidisciplinary Clinic and Translational Research Program at the Ohio State University Wexner Medical Center, Columbus, the results “call for the creation of a nationwide registry where neurologists can document adverse reactions to stem cell procedures and further support dedicated patient and neurologist education as we have proposed before” (See Semin Neurol. 2018; 38[2]:176-81 and JAMA Neurol. 2015;72[11]:1342-5).
In an effort to understand the experiences and attitudes of academic neurologists regarding stem cell tourism and patient-reported complications, the researchers developed a 25-question survey disseminated via Synapse, a web tool from the American Academy of Neurology. Respondents were asked about demographic information, frequency of patient questioning, perception of physician competence, patient complications and experiences, and attitudes toward increased physician education.
Dr. Rai, who is a senior neurology resident at the medical center, presented findings from 204 neurologist respondents, of whom 31% identified themselves as MS specialists. Nearly all respondents (91%) said they have been approached by patients with incurable conditions seeking information about stem cells (37% of whom had diagnosis of MS). In addition, 65% have had at least one patient that has undergone “stem cell therapy,” and 73% said it would be “helpful” or “very helpful” to have an evidence-based patient education tool on the topic. “Patients most often wanted general information,” Dr. Rai said. “However, 50% requested permission to undergo a stem cell procedure, and 31% approached their neurologist after the procedure.”
Survey respondents reported that 33% of the stem cell interventions were performed in the United States and 22% abroad, while 37% reported both in the U.S. and abroad. Patients underwent the procedures in China, Germany, the Bahamas, Mexico, Russia, and Costa Rica. Three-quarters of respondents (75%) indicated no patient experiencing complications from the stem cell interventions. However, 25% reported patients experiencing a variety of complications from the procedures, including strokes, meningoencephalitis, quadriparesis, MS deterioration, sepsis, hepatitis C, seizures, meningitis from intrathecal cell injections, infections, and spinal cord tumors. “At least three respondents had a patient who died as a direct complication from stem cell therapy,” Dr. Rai said.
In their poster, the researchers recommended a “multipronged approach to improve education of MS patients from exploitation and engaging multiple stakeholders in the field, including MS academic societies, licensing boards, and legislative bodies. Specifically, we call for creation of evidence-based education for both neurologists and patients, including physical resources that neurologists can use when discussing stem cell interventions with patients and videos on proper counseling during these visits.”
Colleagues from OSU’s Laboratory for Neural Stem Cells and Functional Neurogenetics contributed to this work. The researchers reported having no financial disclosures.
SOURCE: Rai W et al. ACTRIMS Forum 2019, Poster 237.
DALLAS – Stem cell tourism – the unethical practice of offering unproven cellular preparations to patients for a variety of conditions – is increasingly sought by patients with incurable conditions such as multiple sclerosis and amyotrophic lateral sclerosis, results from a novel survey suggest.
In fact, most academic neurologists have been approached by patients with incurable conditions who ask them about stem cell therapy, while about two-thirds have had at least one patient who has undergone stem cell therapy.
“It’s really scary,” Wijdan Rai, MBBS, the study’s first author, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “This is a more prevalent issue than we think, and the complication rates are higher than we think.”
According to the study’s senior author, Jaime Imitola, MD, who directs the Progressive Multiple Sclerosis Multidisciplinary Clinic and Translational Research Program at the Ohio State University Wexner Medical Center, Columbus, the results “call for the creation of a nationwide registry where neurologists can document adverse reactions to stem cell procedures and further support dedicated patient and neurologist education as we have proposed before” (See Semin Neurol. 2018; 38[2]:176-81 and JAMA Neurol. 2015;72[11]:1342-5).
In an effort to understand the experiences and attitudes of academic neurologists regarding stem cell tourism and patient-reported complications, the researchers developed a 25-question survey disseminated via Synapse, a web tool from the American Academy of Neurology. Respondents were asked about demographic information, frequency of patient questioning, perception of physician competence, patient complications and experiences, and attitudes toward increased physician education.
Dr. Rai, who is a senior neurology resident at the medical center, presented findings from 204 neurologist respondents, of whom 31% identified themselves as MS specialists. Nearly all respondents (91%) said they have been approached by patients with incurable conditions seeking information about stem cells (37% of whom had diagnosis of MS). In addition, 65% have had at least one patient that has undergone “stem cell therapy,” and 73% said it would be “helpful” or “very helpful” to have an evidence-based patient education tool on the topic. “Patients most often wanted general information,” Dr. Rai said. “However, 50% requested permission to undergo a stem cell procedure, and 31% approached their neurologist after the procedure.”
Survey respondents reported that 33% of the stem cell interventions were performed in the United States and 22% abroad, while 37% reported both in the U.S. and abroad. Patients underwent the procedures in China, Germany, the Bahamas, Mexico, Russia, and Costa Rica. Three-quarters of respondents (75%) indicated no patient experiencing complications from the stem cell interventions. However, 25% reported patients experiencing a variety of complications from the procedures, including strokes, meningoencephalitis, quadriparesis, MS deterioration, sepsis, hepatitis C, seizures, meningitis from intrathecal cell injections, infections, and spinal cord tumors. “At least three respondents had a patient who died as a direct complication from stem cell therapy,” Dr. Rai said.
In their poster, the researchers recommended a “multipronged approach to improve education of MS patients from exploitation and engaging multiple stakeholders in the field, including MS academic societies, licensing boards, and legislative bodies. Specifically, we call for creation of evidence-based education for both neurologists and patients, including physical resources that neurologists can use when discussing stem cell interventions with patients and videos on proper counseling during these visits.”
Colleagues from OSU’s Laboratory for Neural Stem Cells and Functional Neurogenetics contributed to this work. The researchers reported having no financial disclosures.
SOURCE: Rai W et al. ACTRIMS Forum 2019, Poster 237.
DALLAS – Stem cell tourism – the unethical practice of offering unproven cellular preparations to patients for a variety of conditions – is increasingly sought by patients with incurable conditions such as multiple sclerosis and amyotrophic lateral sclerosis, results from a novel survey suggest.
In fact, most academic neurologists have been approached by patients with incurable conditions who ask them about stem cell therapy, while about two-thirds have had at least one patient who has undergone stem cell therapy.
“It’s really scary,” Wijdan Rai, MBBS, the study’s first author, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “This is a more prevalent issue than we think, and the complication rates are higher than we think.”
According to the study’s senior author, Jaime Imitola, MD, who directs the Progressive Multiple Sclerosis Multidisciplinary Clinic and Translational Research Program at the Ohio State University Wexner Medical Center, Columbus, the results “call for the creation of a nationwide registry where neurologists can document adverse reactions to stem cell procedures and further support dedicated patient and neurologist education as we have proposed before” (See Semin Neurol. 2018; 38[2]:176-81 and JAMA Neurol. 2015;72[11]:1342-5).
In an effort to understand the experiences and attitudes of academic neurologists regarding stem cell tourism and patient-reported complications, the researchers developed a 25-question survey disseminated via Synapse, a web tool from the American Academy of Neurology. Respondents were asked about demographic information, frequency of patient questioning, perception of physician competence, patient complications and experiences, and attitudes toward increased physician education.
Dr. Rai, who is a senior neurology resident at the medical center, presented findings from 204 neurologist respondents, of whom 31% identified themselves as MS specialists. Nearly all respondents (91%) said they have been approached by patients with incurable conditions seeking information about stem cells (37% of whom had diagnosis of MS). In addition, 65% have had at least one patient that has undergone “stem cell therapy,” and 73% said it would be “helpful” or “very helpful” to have an evidence-based patient education tool on the topic. “Patients most often wanted general information,” Dr. Rai said. “However, 50% requested permission to undergo a stem cell procedure, and 31% approached their neurologist after the procedure.”
Survey respondents reported that 33% of the stem cell interventions were performed in the United States and 22% abroad, while 37% reported both in the U.S. and abroad. Patients underwent the procedures in China, Germany, the Bahamas, Mexico, Russia, and Costa Rica. Three-quarters of respondents (75%) indicated no patient experiencing complications from the stem cell interventions. However, 25% reported patients experiencing a variety of complications from the procedures, including strokes, meningoencephalitis, quadriparesis, MS deterioration, sepsis, hepatitis C, seizures, meningitis from intrathecal cell injections, infections, and spinal cord tumors. “At least three respondents had a patient who died as a direct complication from stem cell therapy,” Dr. Rai said.
In their poster, the researchers recommended a “multipronged approach to improve education of MS patients from exploitation and engaging multiple stakeholders in the field, including MS academic societies, licensing boards, and legislative bodies. Specifically, we call for creation of evidence-based education for both neurologists and patients, including physical resources that neurologists can use when discussing stem cell interventions with patients and videos on proper counseling during these visits.”
Colleagues from OSU’s Laboratory for Neural Stem Cells and Functional Neurogenetics contributed to this work. The researchers reported having no financial disclosures.
SOURCE: Rai W et al. ACTRIMS Forum 2019, Poster 237.
REPORTING FROM ACTRIMS FORUM 2019
Viewing childhood autism as a whole body disorder
Intestinal inflammation, oxidative stress, immune problems affect subsets of patients.
LAS VEGAS – When parents of children with autism ask their primary physicians about complementary and integrative medical treatments, they often get stonewalled, according to Robert L. Hendren, DO.
“They find [clinicians] usually say, ‘Don’t try that stuff. It doesn’t work,’” Dr. Hendren said at an annual psychopharmacology update held by the Nevada Psychiatric Association.
“Parents then go to two different sets of providers,” he said. One provider “tells them about complementary and integrative medicine, but is likely not a traditional physician who’s treating their autism. It’s somebody who knows about these biomedical interventions but when parents tell them that they’re using traditional interventions ... that person also says, ‘Don’t use that. That’s doesn’t work.’ Then they go see their traditional provider who might be thinking about traditional medications. But they’ve learned that they don’t want to tell them, ‘I’m considering using omega 3s or zinc.’ Regrettably, most times physicians don’t say, ‘Let’s examine that. Let’s look at the literature and see if that’s the right decision for you.’ By shutting a family down saying, ‘I don’t want to hear about that,’ it often leads the family to think: ‘How do I make a decision about this? How do I know what to do?’ ”
Dr. Hendren said clinicians are beginning to embrace the notion that autism is not just a brain disorder, but rather a whole body disorder. For example, he noted that significant subsets of people with autism have intestinal inflammation, digestive enzyme abnormalities, metabolic impairments, oxidative stress, mitochondrial dysfunction, and immunity problems that range from immune deficiency to hypersensitivity to autoimmunity. “,” said Dr. Hendren, professor of child and adolescent psychiatry at the University of California, San Francisco. “I hope that by thinking about making the body healthier, we can help kids have the very best outcomes.”
Several biomedical treatments have adequate evidence to use for many patients, he said, including melatonin, probiotics, omega 3s, and possibly vitamin D3, methyl B12, oxytocin, restrictive diets, digestive enzymes, and choline. “There are strong anecdotal reports of gluten-free diet benefits,” said Dr. Hendren, who also directs the UCSF Program for Research on Neurodevelopmental and Translational Outcomes. “Some parents I greatly respect tell me it’s the single most important thing they’ve done in their child’s health, that their GI symptoms have improved, and their overall health has improved.”
In a multisite trial called aViation, researchers are evaluating the effects of an investigational vasopressin antagonist in autistic patients aged 5-17 years. The drug works by blocking a brain receptor of the vasopressin receptor that is associated with control of stress, anxiety, affection, and aggression. “The first trial in adults showed potential benefit,” Dr. Hendren said.
No robust studies exist to suggest that medical marijuana makes a difference for patients with autism, he said, but he has several patients whose parents give their affected child medical marijuana or cannabidiol. “I have a number of families who say it’s really made a big difference for their children and for how they’re doing,” he said.
In Marin County, Calif., the Oak Hill School serves a heterogeneous population of children, adolescents, and young adults, all of whom have autism spectrum disorder (ASD) or other neurologically based disorders of relating and communicating. Students receive special education instruction and customized on-site clinical programs that might include speech/language pathology, occupational therapy, and group and individual psychotherapy. Some of the students have received recent functional behavior analyses from Dr. Hendren and his colleagues, with school staff implementing positive behavior intervention programs.
The researchers also are using metabolomics as a biomarker of outcome. “We’re using metabolomics from the urine, where we can look at these processes in different clusters and see whether our interventions make a difference or not,” said Dr. Hendren, who is a past president of the American Academy of Child and Adolescent Psychiatry. “We did one trial with sulforaphane, which is a concentrated broccoli sprout extract that helps with oxidative stress. It was initially developed to treat oxidative stress in cancer,” he said. Upcoming trials in this cohort include the use of folinic acid and CM-AT, a pancreatic digestive enzyme intended to increase levels of chymotrypsin.
“I think of autism as being a disorder where you have this person and there’s a veil of autism that comes over the top of them,” he said. “That veil is not the kid, although the kid becomes more and more expressed through that. If we can do something to lift that veil, we can do more and more to pull that child out.”
Dr. Hendren disclosed that he has received grants from Curemark, Roche, Shire, and Sunovion. He is a member of the advisory boards for Curemark, BioMarin, Janssen, and Axial Biotherapeutics.
Intestinal inflammation, oxidative stress, immune problems affect subsets of patients.
Intestinal inflammation, oxidative stress, immune problems affect subsets of patients.
LAS VEGAS – When parents of children with autism ask their primary physicians about complementary and integrative medical treatments, they often get stonewalled, according to Robert L. Hendren, DO.
“They find [clinicians] usually say, ‘Don’t try that stuff. It doesn’t work,’” Dr. Hendren said at an annual psychopharmacology update held by the Nevada Psychiatric Association.
“Parents then go to two different sets of providers,” he said. One provider “tells them about complementary and integrative medicine, but is likely not a traditional physician who’s treating their autism. It’s somebody who knows about these biomedical interventions but when parents tell them that they’re using traditional interventions ... that person also says, ‘Don’t use that. That’s doesn’t work.’ Then they go see their traditional provider who might be thinking about traditional medications. But they’ve learned that they don’t want to tell them, ‘I’m considering using omega 3s or zinc.’ Regrettably, most times physicians don’t say, ‘Let’s examine that. Let’s look at the literature and see if that’s the right decision for you.’ By shutting a family down saying, ‘I don’t want to hear about that,’ it often leads the family to think: ‘How do I make a decision about this? How do I know what to do?’ ”
Dr. Hendren said clinicians are beginning to embrace the notion that autism is not just a brain disorder, but rather a whole body disorder. For example, he noted that significant subsets of people with autism have intestinal inflammation, digestive enzyme abnormalities, metabolic impairments, oxidative stress, mitochondrial dysfunction, and immunity problems that range from immune deficiency to hypersensitivity to autoimmunity. “,” said Dr. Hendren, professor of child and adolescent psychiatry at the University of California, San Francisco. “I hope that by thinking about making the body healthier, we can help kids have the very best outcomes.”
Several biomedical treatments have adequate evidence to use for many patients, he said, including melatonin, probiotics, omega 3s, and possibly vitamin D3, methyl B12, oxytocin, restrictive diets, digestive enzymes, and choline. “There are strong anecdotal reports of gluten-free diet benefits,” said Dr. Hendren, who also directs the UCSF Program for Research on Neurodevelopmental and Translational Outcomes. “Some parents I greatly respect tell me it’s the single most important thing they’ve done in their child’s health, that their GI symptoms have improved, and their overall health has improved.”
In a multisite trial called aViation, researchers are evaluating the effects of an investigational vasopressin antagonist in autistic patients aged 5-17 years. The drug works by blocking a brain receptor of the vasopressin receptor that is associated with control of stress, anxiety, affection, and aggression. “The first trial in adults showed potential benefit,” Dr. Hendren said.
No robust studies exist to suggest that medical marijuana makes a difference for patients with autism, he said, but he has several patients whose parents give their affected child medical marijuana or cannabidiol. “I have a number of families who say it’s really made a big difference for their children and for how they’re doing,” he said.
In Marin County, Calif., the Oak Hill School serves a heterogeneous population of children, adolescents, and young adults, all of whom have autism spectrum disorder (ASD) or other neurologically based disorders of relating and communicating. Students receive special education instruction and customized on-site clinical programs that might include speech/language pathology, occupational therapy, and group and individual psychotherapy. Some of the students have received recent functional behavior analyses from Dr. Hendren and his colleagues, with school staff implementing positive behavior intervention programs.
The researchers also are using metabolomics as a biomarker of outcome. “We’re using metabolomics from the urine, where we can look at these processes in different clusters and see whether our interventions make a difference or not,” said Dr. Hendren, who is a past president of the American Academy of Child and Adolescent Psychiatry. “We did one trial with sulforaphane, which is a concentrated broccoli sprout extract that helps with oxidative stress. It was initially developed to treat oxidative stress in cancer,” he said. Upcoming trials in this cohort include the use of folinic acid and CM-AT, a pancreatic digestive enzyme intended to increase levels of chymotrypsin.
“I think of autism as being a disorder where you have this person and there’s a veil of autism that comes over the top of them,” he said. “That veil is not the kid, although the kid becomes more and more expressed through that. If we can do something to lift that veil, we can do more and more to pull that child out.”
Dr. Hendren disclosed that he has received grants from Curemark, Roche, Shire, and Sunovion. He is a member of the advisory boards for Curemark, BioMarin, Janssen, and Axial Biotherapeutics.
LAS VEGAS – When parents of children with autism ask their primary physicians about complementary and integrative medical treatments, they often get stonewalled, according to Robert L. Hendren, DO.
“They find [clinicians] usually say, ‘Don’t try that stuff. It doesn’t work,’” Dr. Hendren said at an annual psychopharmacology update held by the Nevada Psychiatric Association.
“Parents then go to two different sets of providers,” he said. One provider “tells them about complementary and integrative medicine, but is likely not a traditional physician who’s treating their autism. It’s somebody who knows about these biomedical interventions but when parents tell them that they’re using traditional interventions ... that person also says, ‘Don’t use that. That’s doesn’t work.’ Then they go see their traditional provider who might be thinking about traditional medications. But they’ve learned that they don’t want to tell them, ‘I’m considering using omega 3s or zinc.’ Regrettably, most times physicians don’t say, ‘Let’s examine that. Let’s look at the literature and see if that’s the right decision for you.’ By shutting a family down saying, ‘I don’t want to hear about that,’ it often leads the family to think: ‘How do I make a decision about this? How do I know what to do?’ ”
Dr. Hendren said clinicians are beginning to embrace the notion that autism is not just a brain disorder, but rather a whole body disorder. For example, he noted that significant subsets of people with autism have intestinal inflammation, digestive enzyme abnormalities, metabolic impairments, oxidative stress, mitochondrial dysfunction, and immunity problems that range from immune deficiency to hypersensitivity to autoimmunity. “,” said Dr. Hendren, professor of child and adolescent psychiatry at the University of California, San Francisco. “I hope that by thinking about making the body healthier, we can help kids have the very best outcomes.”
Several biomedical treatments have adequate evidence to use for many patients, he said, including melatonin, probiotics, omega 3s, and possibly vitamin D3, methyl B12, oxytocin, restrictive diets, digestive enzymes, and choline. “There are strong anecdotal reports of gluten-free diet benefits,” said Dr. Hendren, who also directs the UCSF Program for Research on Neurodevelopmental and Translational Outcomes. “Some parents I greatly respect tell me it’s the single most important thing they’ve done in their child’s health, that their GI symptoms have improved, and their overall health has improved.”
In a multisite trial called aViation, researchers are evaluating the effects of an investigational vasopressin antagonist in autistic patients aged 5-17 years. The drug works by blocking a brain receptor of the vasopressin receptor that is associated with control of stress, anxiety, affection, and aggression. “The first trial in adults showed potential benefit,” Dr. Hendren said.
No robust studies exist to suggest that medical marijuana makes a difference for patients with autism, he said, but he has several patients whose parents give their affected child medical marijuana or cannabidiol. “I have a number of families who say it’s really made a big difference for their children and for how they’re doing,” he said.
In Marin County, Calif., the Oak Hill School serves a heterogeneous population of children, adolescents, and young adults, all of whom have autism spectrum disorder (ASD) or other neurologically based disorders of relating and communicating. Students receive special education instruction and customized on-site clinical programs that might include speech/language pathology, occupational therapy, and group and individual psychotherapy. Some of the students have received recent functional behavior analyses from Dr. Hendren and his colleagues, with school staff implementing positive behavior intervention programs.
The researchers also are using metabolomics as a biomarker of outcome. “We’re using metabolomics from the urine, where we can look at these processes in different clusters and see whether our interventions make a difference or not,” said Dr. Hendren, who is a past president of the American Academy of Child and Adolescent Psychiatry. “We did one trial with sulforaphane, which is a concentrated broccoli sprout extract that helps with oxidative stress. It was initially developed to treat oxidative stress in cancer,” he said. Upcoming trials in this cohort include the use of folinic acid and CM-AT, a pancreatic digestive enzyme intended to increase levels of chymotrypsin.
“I think of autism as being a disorder where you have this person and there’s a veil of autism that comes over the top of them,” he said. “That veil is not the kid, although the kid becomes more and more expressed through that. If we can do something to lift that veil, we can do more and more to pull that child out.”
Dr. Hendren disclosed that he has received grants from Curemark, Roche, Shire, and Sunovion. He is a member of the advisory boards for Curemark, BioMarin, Janssen, and Axial Biotherapeutics.
EXPERT ANALYSIS FROM NPA 2019
What happens when RRMS patients discontinue their DMT?
DALLAS – results from a single-center study showed.
In addition, being over the age of 45 years was associated with a better disease course after treatment discontinuation.
“Being clinically and radiologically stable for more than 2 years can be a potential milestone to regard the discontinuation of DMT [disease-modifying therapy] as a reasonable option in a subset of patients, especially patients who are nondisabled,” lead study author Hajime Yano, MD, said in an interview at the Americas Committee for Treatment and Research in Multiple Sclerosis.
According to Dr. Yano, a research fellow at the Ann Romney Center for Neurologic Diseases and Partners Multiple Sclerosis Center in Boston, relapsing remitting multiple sclerosis (RRMS) patients without relapse for long periods on treatment may consider discontinuing DMT, but there is limited information regarding the impact of discontinuation, especially in terms of MRI activity.
In an effort to investigate the impact of DMT discontinuation on clinical and radiologic outcomes in RRMS patients, he and his colleagues identified 70 patients from the Comprehensive Longitudinal Investigation of Multiple Sclerosis at the Brigham and Women’s Hospital (CLIMB) study, which was initiated in 2000 and has enrolled more than 2,400 patients cared for at the Partners Multiple Sclerosis Center. Relapse date, symptoms, and Expanded Disability Status Scale (EDSS) were evaluated at 6-month intervals for each patient during the time of clinic visits by the treating neurologist. Additionally, brain MRIs were performed annually.
Next, the researchers matched the patients with 70 patients who remained on DMT identified by age, sex, treatment, treatment duration, disease duration, and EDSS. They used univariate and multivariable Cox proportional hazard models to test the differences between DMT discontinuation status with time to clinical relapse, MRI event, disability progression, and any inflammatory event (either clinical relapse or MRI event).
The mean age of patients was 45 years, 87% were female, their mean disease duration was about 13 years, and they had been receiving treatment for a mean of about 6 years. In adjusted analyses, the 70 pairs of patients who discontinued DMT and patients who continued DMT had similar outcomes in time to clinical relapse (hazard ratio, 0.93; P = .84), MRI event (HR, 1.01; P = .98), disability progression (HR, 1.33; P = .43), and any inflammatory event (HR, 0.93; P = .85). In a subgroup analysis, which compared the impact of DMT discontinuation between patients over the age of 45 years and those aged 45 years and younger, the researchers observed a statistically significant difference in effect of discontinuation on time to clinical relapse (P = .032), time to MRI event (P = .013), and time to any inflammatory event (P = .0005), all favoring patients over the age of 45 years.
“This finding makes sense since age has been reported as one of the factors that negatively impacts on the inflammatory activity in patients with RRMS,” Dr. Yano said. “However, our study is the first study [to find] that the impact of discontinuing DMT on RRMS patient prognosis may differ based on the age at the discontinuation. In short, stopping DMT at a younger age has a statistically significant higher risk on inflammatory activities, compared to [stopping DMT at an] older age.”
He acknowledged certain limitations of the study, including its small sample size and single-center design. However, Dr. Yano said that a key strength of the analysis was the inclusion of MRI activity prior to DMT as the definition of stable state, “which is an integral piece of information when physicians and patients consider DMT discontinuation in a ‘real world’ clinical setting. We also used MRI activity as an outcome measure, which is lacking in prior discontinuation studies.”
Dr. Yano reported that he has received a research grant from Yoshida Scholarship Foundation in Japan. His coauthors reported having numerous financial ties to industry.
SOURCE: Yano H et al. ACTRIMS Forum 2019, Poster 061.
DALLAS – results from a single-center study showed.
In addition, being over the age of 45 years was associated with a better disease course after treatment discontinuation.
“Being clinically and radiologically stable for more than 2 years can be a potential milestone to regard the discontinuation of DMT [disease-modifying therapy] as a reasonable option in a subset of patients, especially patients who are nondisabled,” lead study author Hajime Yano, MD, said in an interview at the Americas Committee for Treatment and Research in Multiple Sclerosis.
According to Dr. Yano, a research fellow at the Ann Romney Center for Neurologic Diseases and Partners Multiple Sclerosis Center in Boston, relapsing remitting multiple sclerosis (RRMS) patients without relapse for long periods on treatment may consider discontinuing DMT, but there is limited information regarding the impact of discontinuation, especially in terms of MRI activity.
In an effort to investigate the impact of DMT discontinuation on clinical and radiologic outcomes in RRMS patients, he and his colleagues identified 70 patients from the Comprehensive Longitudinal Investigation of Multiple Sclerosis at the Brigham and Women’s Hospital (CLIMB) study, which was initiated in 2000 and has enrolled more than 2,400 patients cared for at the Partners Multiple Sclerosis Center. Relapse date, symptoms, and Expanded Disability Status Scale (EDSS) were evaluated at 6-month intervals for each patient during the time of clinic visits by the treating neurologist. Additionally, brain MRIs were performed annually.
Next, the researchers matched the patients with 70 patients who remained on DMT identified by age, sex, treatment, treatment duration, disease duration, and EDSS. They used univariate and multivariable Cox proportional hazard models to test the differences between DMT discontinuation status with time to clinical relapse, MRI event, disability progression, and any inflammatory event (either clinical relapse or MRI event).
The mean age of patients was 45 years, 87% were female, their mean disease duration was about 13 years, and they had been receiving treatment for a mean of about 6 years. In adjusted analyses, the 70 pairs of patients who discontinued DMT and patients who continued DMT had similar outcomes in time to clinical relapse (hazard ratio, 0.93; P = .84), MRI event (HR, 1.01; P = .98), disability progression (HR, 1.33; P = .43), and any inflammatory event (HR, 0.93; P = .85). In a subgroup analysis, which compared the impact of DMT discontinuation between patients over the age of 45 years and those aged 45 years and younger, the researchers observed a statistically significant difference in effect of discontinuation on time to clinical relapse (P = .032), time to MRI event (P = .013), and time to any inflammatory event (P = .0005), all favoring patients over the age of 45 years.
“This finding makes sense since age has been reported as one of the factors that negatively impacts on the inflammatory activity in patients with RRMS,” Dr. Yano said. “However, our study is the first study [to find] that the impact of discontinuing DMT on RRMS patient prognosis may differ based on the age at the discontinuation. In short, stopping DMT at a younger age has a statistically significant higher risk on inflammatory activities, compared to [stopping DMT at an] older age.”
He acknowledged certain limitations of the study, including its small sample size and single-center design. However, Dr. Yano said that a key strength of the analysis was the inclusion of MRI activity prior to DMT as the definition of stable state, “which is an integral piece of information when physicians and patients consider DMT discontinuation in a ‘real world’ clinical setting. We also used MRI activity as an outcome measure, which is lacking in prior discontinuation studies.”
Dr. Yano reported that he has received a research grant from Yoshida Scholarship Foundation in Japan. His coauthors reported having numerous financial ties to industry.
SOURCE: Yano H et al. ACTRIMS Forum 2019, Poster 061.
DALLAS – results from a single-center study showed.
In addition, being over the age of 45 years was associated with a better disease course after treatment discontinuation.
“Being clinically and radiologically stable for more than 2 years can be a potential milestone to regard the discontinuation of DMT [disease-modifying therapy] as a reasonable option in a subset of patients, especially patients who are nondisabled,” lead study author Hajime Yano, MD, said in an interview at the Americas Committee for Treatment and Research in Multiple Sclerosis.
According to Dr. Yano, a research fellow at the Ann Romney Center for Neurologic Diseases and Partners Multiple Sclerosis Center in Boston, relapsing remitting multiple sclerosis (RRMS) patients without relapse for long periods on treatment may consider discontinuing DMT, but there is limited information regarding the impact of discontinuation, especially in terms of MRI activity.
In an effort to investigate the impact of DMT discontinuation on clinical and radiologic outcomes in RRMS patients, he and his colleagues identified 70 patients from the Comprehensive Longitudinal Investigation of Multiple Sclerosis at the Brigham and Women’s Hospital (CLIMB) study, which was initiated in 2000 and has enrolled more than 2,400 patients cared for at the Partners Multiple Sclerosis Center. Relapse date, symptoms, and Expanded Disability Status Scale (EDSS) were evaluated at 6-month intervals for each patient during the time of clinic visits by the treating neurologist. Additionally, brain MRIs were performed annually.
Next, the researchers matched the patients with 70 patients who remained on DMT identified by age, sex, treatment, treatment duration, disease duration, and EDSS. They used univariate and multivariable Cox proportional hazard models to test the differences between DMT discontinuation status with time to clinical relapse, MRI event, disability progression, and any inflammatory event (either clinical relapse or MRI event).
The mean age of patients was 45 years, 87% were female, their mean disease duration was about 13 years, and they had been receiving treatment for a mean of about 6 years. In adjusted analyses, the 70 pairs of patients who discontinued DMT and patients who continued DMT had similar outcomes in time to clinical relapse (hazard ratio, 0.93; P = .84), MRI event (HR, 1.01; P = .98), disability progression (HR, 1.33; P = .43), and any inflammatory event (HR, 0.93; P = .85). In a subgroup analysis, which compared the impact of DMT discontinuation between patients over the age of 45 years and those aged 45 years and younger, the researchers observed a statistically significant difference in effect of discontinuation on time to clinical relapse (P = .032), time to MRI event (P = .013), and time to any inflammatory event (P = .0005), all favoring patients over the age of 45 years.
“This finding makes sense since age has been reported as one of the factors that negatively impacts on the inflammatory activity in patients with RRMS,” Dr. Yano said. “However, our study is the first study [to find] that the impact of discontinuing DMT on RRMS patient prognosis may differ based on the age at the discontinuation. In short, stopping DMT at a younger age has a statistically significant higher risk on inflammatory activities, compared to [stopping DMT at an] older age.”
He acknowledged certain limitations of the study, including its small sample size and single-center design. However, Dr. Yano said that a key strength of the analysis was the inclusion of MRI activity prior to DMT as the definition of stable state, “which is an integral piece of information when physicians and patients consider DMT discontinuation in a ‘real world’ clinical setting. We also used MRI activity as an outcome measure, which is lacking in prior discontinuation studies.”
Dr. Yano reported that he has received a research grant from Yoshida Scholarship Foundation in Japan. His coauthors reported having numerous financial ties to industry.
SOURCE: Yano H et al. ACTRIMS Forum 2019, Poster 061.
REPORTING FROM ACTRIMS FORUM 2019
Key clinical point: Patients who discontinued disease-modifying therapy after a period of disease inactivity had a similar time to next event, compared with patients who remained on treatment.
Major finding: Compared with patients aged 45 years and younger, older patients who discontinued disease-modifying therapy had significantly favorable disease course in terms of time to clinical relapse (P = .032), time to MRI event (P = .013), and time to any inflammatory event (P = .0005).
Study details: A single-center study of 140 patients with relapsing remitting multiple sclerosis.
Disclosures: Dr. Yano reported that he has received a research grant from the Yoshida Scholarship Foundation in Japan. His coauthors reported having numerous financial ties to industry.Source: Yano H et al. ACTRIMS Forum 2019, Poster 061.